First Clinical Experience with a Carbon Fibre Reinforced PEEK Composite Plating System for Anterior Cervical Discectomy and Fusion
Abstract
1. Introduction
2. Materials and Methods
2.1. Clinical and Radiological Outcome Measures
2.2. Statistical Analysis
3. Results
3.1. Clinical Outcomes
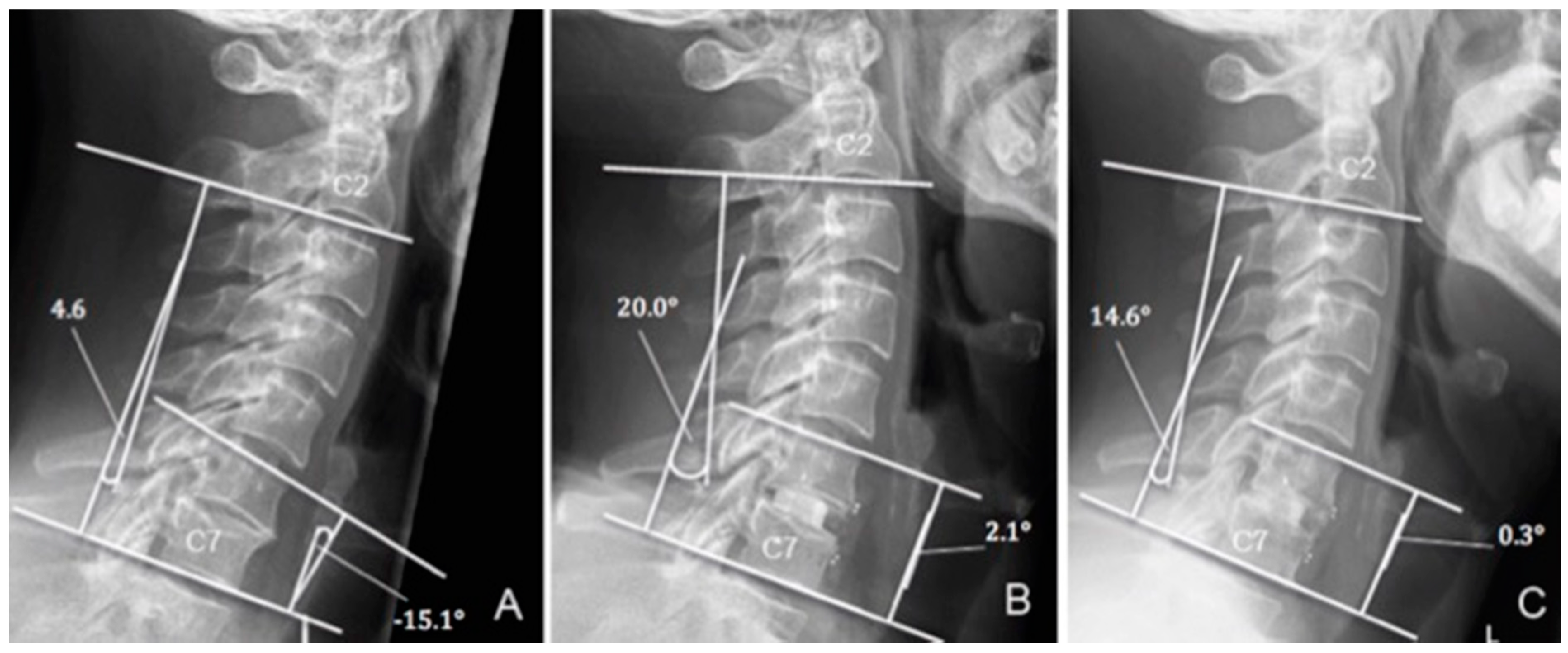
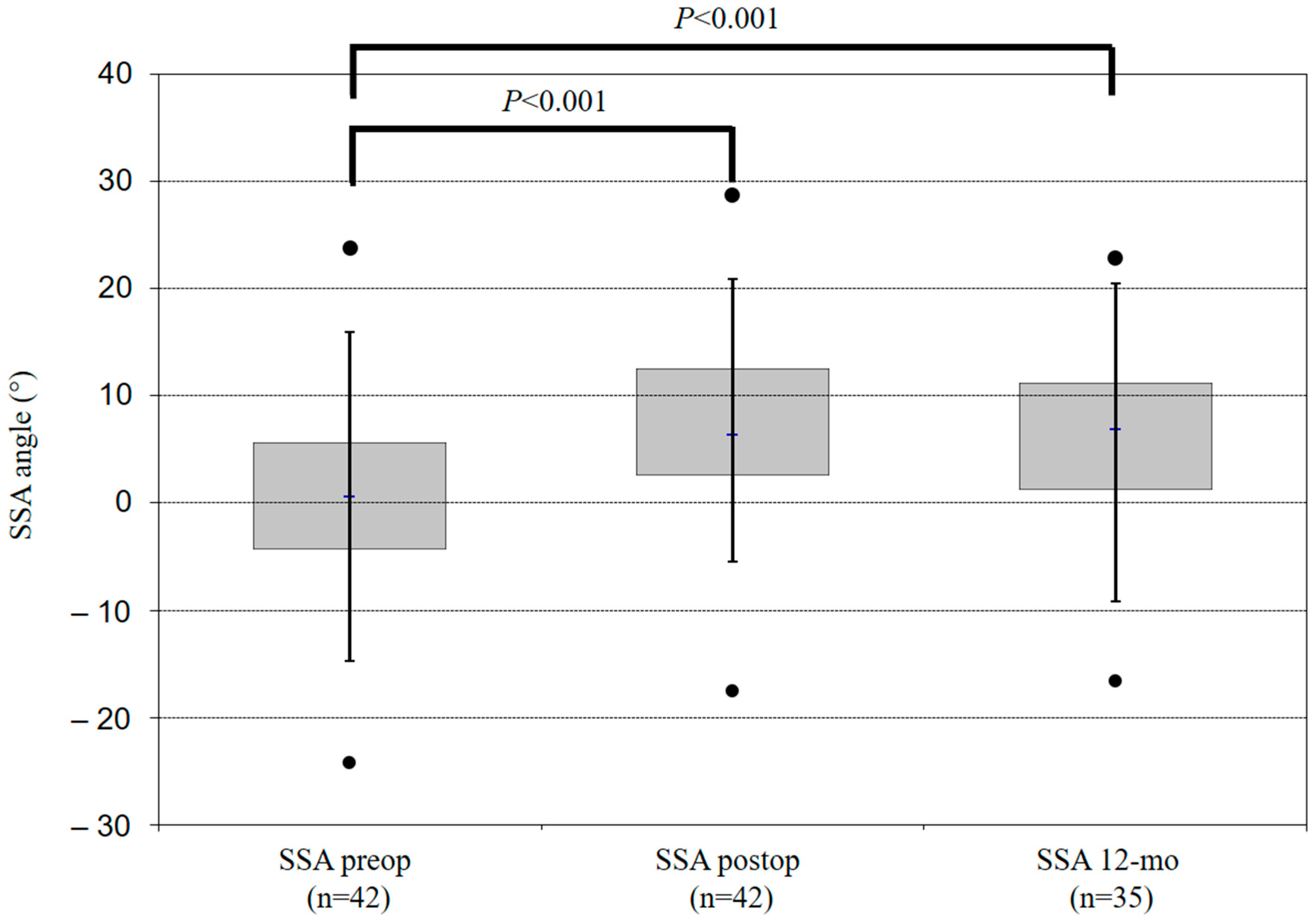
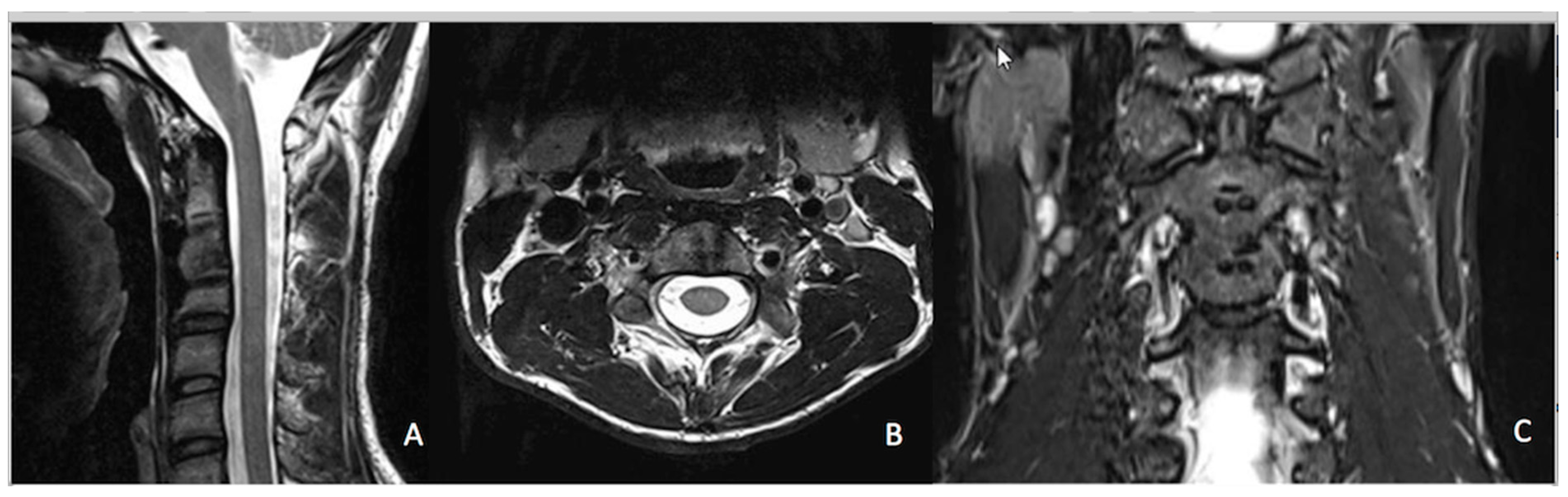
3.2. Radiological Outcomes
3.3. Complications
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gao, Y.; Liu, M.; Li, T.; Huang, F.; Tang, T.; Xiang, Z. A meta-analysis comparing the results of cervical disc arthroplasty with anterior cervical discectomy and fusion (ACDF) for the treatment of symptomatic cervical disc disease. J. Bone Jt. Surg. Am. 2013, 95, 555–561. [Google Scholar] [CrossRef] [PubMed]
- Villavicencio, A.T.; Babuska, J.M.; Ashton, A.; Busch, E.; Roeca, C.; Nelson, E.L.; Mason, A.; Burneikiene, S. Prospective, randomized, double-blind clinical study evaluating the correlation of clinical outcomes and cervical sagittal alignment. Neurosurgery 2011, 68, 1309–1316. [Google Scholar] [CrossRef] [PubMed]
- Park, M.S.; Kelly, M.P.; Lee, D.-H.; Min, W.K.; Rahman, R.K.; Riew, K.D. Sagittal alignment as a predictor of clinical adjacent segment pathology requiring surgery after anterior cervical arthrodesis. Spine J. 2014, 14, 1228–1234. [Google Scholar] [CrossRef] [PubMed]
- Burkhardt, B.W.; Simgen, A.; Dehnen, M.; Wagenpfeil, G.; Reith, W.; Oertel, J.M. Is there an impact of cervical plating on the development of adjacent segment degeneration following Smith-Robinson procedure? A magnetic resonance imaging study of 84 patients with a 24-year follow-up. Spine J. 2018, 19, 587–596. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Xu, M.; Zhang, W.; Kwok, D.T.; Jiang, J.; Wu, Z.; Chu, P.K. Mechanical and biological characteristics of diamond-like carbon coated poly aryl-ether-ether-ketone. Biomaterials 2010, 31, 8181–8187. [Google Scholar] [CrossRef] [PubMed]
- Kurtz, S.M.; Devine, J.N. PEEK biomaterials in trauma, orthopedic, and spinal implants. Biomaterials 2007, 28, 4845–4869. [Google Scholar] [CrossRef] [PubMed]
- Devine, D.M.; Hahn, J.; Richards, R.G.; Gruner, H.; Wieling, R.; Pearce, S.G. Coating of carbon fiber-reinforced polyetheretherketone implants with titanium to improve bone apposition. J. Biomed. Mater. Res. B Appl. Biomater. 2013, 101, 591–598. [Google Scholar] [CrossRef]
- Li, C.S.; Vannabouathong, C.; Sprague, S.; Bhandari, M. The use of carbon-fiber-reinforced (CFR) PEEK material in orthopedic implants: A systematic review. Clin. Med. Insights Arthritis Musculoskelet. Disord. 2015, 8, 33–45. [Google Scholar] [CrossRef]
- Jackson, J.B., III; Crimaldi, A.J.; Peindl, R.; Norton, H.J.; Anderson, W.E.; Patt, J.C. Effect of polyether ether ketone on therapeutic radiation to the spine: A pilot study. Spine 2017, 42, E1–E7. [Google Scholar] [CrossRef]
- Tedesco, G.; Gasbarrini, A.; Bandiera, S.; Ghermandi, R.; Boriani, S. Composite PEEK/Carbon fiber implants can increase the effectiveness of radiotherapy in the management of spine tumors. J. Spine Surg. 2017, 3, 323–329. [Google Scholar] [CrossRef]
- Haid, R.W.; Foley, K.T.; Rodts, G.E.; Barnes, B. The cervical spine study group anterior cervical plate nomenclature. Neurosurg. Focus 2002, 12, 1–6. [Google Scholar] [CrossRef]
- Odom, G.L.; Finney, W.; Woodhall, B. Cervical disk lesions. J. Am. Med. Assoc. 1958, 166, 23–28. [Google Scholar] [CrossRef] [PubMed]
- Faldini, C.; Leonetti, D.; Nanni, M.; Di Martino, A.; Denaro, L.; Denaro, V.; Giannini, S. Cervical disc herniation and cervical spondylosis surgically treated by Cloward procedure: A 10-year-minimum follow-up study. J. Orthop. Traumatol. 2010, 11, 99–103. [Google Scholar] [CrossRef] [PubMed]
- Gum, J.L.; Glassman, S.D.; Douglas, L.R.; Carreon, L.Y. Correlation between cervical spine sagittal alignment and clinical outcomes after ACDF. Spine J. 2010, 10, S2–S3. [Google Scholar] [CrossRef]
- Aghayev, E.; Zullig, N.; Diel, P.; Dietrich, D.; Benneker, L.M. Development and validation of a quantitative method to assess pedicle screw loosening in posterior spine instrumentation on plain radiographs. Eur. Spine J. 2014, 23, 689–694. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Benneker, L.M.; Heini, P.F.; Anderson, S.E.; Alini, M.; Ito, K. Correlation of radiographic and MRI parameters to morphological and biochemical assessment of intervertebral disc degeneration. Eur. Spine J. 2005, 14, 27–35. [Google Scholar] [CrossRef]
- Bridwell, K.H.; Lenke, L.G.; McEnery, K.W.; Baldus, C.; Blanke, K. Anterior fresh frozen structural allografts in the thoracic and lumbar spine. Do they work if combined with posterior fusion and instrumentation in adult patients with kyphosis or anterior column defects? Spine 1995, 20, 1410–1418. [Google Scholar] [CrossRef]
- Schemper, M.; Smith, T.L. A note on quantifying follow-up in studies of failure time. Control. Clin. Trials 1996, 17, 343–346. [Google Scholar] [CrossRef]
- Moftakhar, R.; Trost, G.R. Anterior cervical plates: A historical perspective. Neurosurg. Focus 2004, 16, 1–5. [Google Scholar] [CrossRef]
- Boriani, S.; Tedesco, G.; Ming, L.; Ghermandi, R.; Amichetti, M.; Fossati, P.; Krengli, M.; Mavilla, L.; Gasbarrini, A. Carbon-fiber-reinforced PEEK fixation system in the treatment of spine tumors: A pre-liminary report. Eur. Spine J. 2018, 27, 874–881. [Google Scholar] [CrossRef]
- Miller, L.E.; Block, J.E. Safety and effectiveness of bone allografts in anterior cervical discectomy and fusion surgery. Spine 2011, 36, 2045–2050. [Google Scholar] [CrossRef] [PubMed]
- Oshina, M.; Oshima, Y.; Tanaka, S.; Riew, K.D. Radiological fusion criteria of postoperative anterior cervical discectomy and fusion: A systematic review. Glob. Spine J. 2018, 8, 739–750. [Google Scholar] [CrossRef] [PubMed]
- Shriver, M.F.; Lewis, D.J.; Kshettry, V.R.; Rosenbaum, B.P.; Benzel, E.C.; Mroz, T.E. Pseudoarthrosis rates in anterior cervical discectomy and fusion: A meta-analysis. Spine J. 2015, 15, 2016–2027. [Google Scholar] [CrossRef] [PubMed]
- Skolasky, R.L.; Maggard, A.M.; Hilibrand, A.S.; Northrup,, B.E.; Ullrich, C.G.; Albert, T.J.; Coe, J.D.; Riley, L.H., 3rd. Agreement between surgeons and an independent panel with respect to surgical site fusion after single-level anterior cervical spine surgery: A prospective, multicenter study. Spine (Phila Pa 1976) 2006, 31, E503–E506. [Google Scholar]
- Kreitz, T.M.; Hollern, D.A.; Padegimas, E.M.; Schroeder, G.D.; Kepler, C.K.; Vaccaro, A.R.; Hilibrand, A.S. Clinical outcomes after four-level anterior cervical discectomy and fusion. Glob. Spine J. 2018, 8, 776–783. [Google Scholar] [CrossRef] [PubMed]
- Laratta, J.L.; Reddy, H.P.; Bratcher, K.R.; McGraw, K.E.; Carreon, L.Y.; Owens, R.K., 2nd. Outcomes and revision rates following multilevel anterior cervical discectomy and fusion. J. Spine Surg. 2018, 4, 496–500. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.H.; Cho, J.H.; Hwang, C.J.; Lee, C.S.; Cho, S.K.; Kim, C.; Ha, J.K. What is the fate of pseudarthrosis detected 1 year after anterior cervical discectomy and fusion? Spine (Phila Pa 1976) 2018, 43, E23–E28. [Google Scholar] [CrossRef] [PubMed]
- Hilibrand, A.S.; Carlson, G.D.; Palumbo, M.A.; Jones, P.K.; Bohlman, H.H. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J. Bone Jt. Surg. Am. 1999, 81, 519–528. [Google Scholar] [CrossRef] [PubMed]
- Shriver, M.F.; Lubelski, D.; Sharma, A.M.; Steinmetz, M.P.; Benzel, E.C.; Mroz, T.E. Adjacent segment degeneration and disease following cervical arthroplasty: A systematic review and meta-analysis. Spine J. 2016, 16, 168–181. [Google Scholar] [CrossRef] [PubMed]
- Buttermann, G.R. Anterior cervical discectomy and fusion outcomes over 10 years. Spine 2018, 43, 207–214. [Google Scholar] [CrossRef]
- Fountas, K.N.; Kapsalaki, E.Z.; Nikolakakos, L.G.; Smisson, H.F.; Johnston, K.W.; Grigorian, A.A.; Lee, G.P.; Robinson, J.S., Jr. Anterior cervical discectomy and fusion associated complications. Spine 2007, 32, 2310–2317. [Google Scholar] [CrossRef] [PubMed]
- Shriver, M.F.; Lewis, D.J.; Kshettry, V.R.; Rosenbaum, B.P.; Benzel, E.C.; Mroz, T.E. Dysphagia rates after anterior cervical Diskectomy and fusion: A systematic review and meta-analysis. Glob. Spine J. 2017, 7, 95–103. [Google Scholar] [CrossRef] [PubMed]
- Zhong, Z.-M.; Zhu, S.-Y.; Zhuang, J.-S.; Wu, Q.; Chen, J.T. Reoperation after cervical disc arthroplasty versus anterior cervical discectomy and fusion: A meta-analysis. Clin. Orthop. Relat. Res. 2016, 474, 1307–1316. [Google Scholar] [CrossRef] [PubMed]



| Age (Median (IQR)) | Gender (M:F) | Indication | Number of Cases Undergoing ACDF (%) |
|---|---|---|---|
| 51.9 (44.5 to 58.6) | 36:6 | Trauma | 23 (54.8%) |
| Degeneration | 16 (38.1%) | ||
| Tumour | 3 (7.1%) | ||
| Total | 42 (100%) |
| Complications | Number of Cases (%) |
|---|---|
| Dysphagia | 2 (5.7%) |
| Screw loosening | 1 (2.9%) |
| Cage subsidence | 1 (2.9%) |
| Infections | 0 (0.0%) |
| Recurrent nerve palsy | 0 (0.0%) |
| Hardware failure | 0 (0.0%) |
| Death related to procedure | 0 (0.0%) |
| Group | Angle | Time Point of Measurement | Mean Change of SSA and SACS Between Two Measurements | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Preop (n = 42) (±SD) | Preop (n = 35) (±SD) | Postop (n = 42) (±SD) | Postop (n = 35) (±D) | 12-Mo (±SD) | Preop to Post Op (Degrees) (±SD) | p-Value | Preop to 12-Mo (Degrees) (±SD) | p-Value | Postop to 12-Mo (Degrees) (±SD) | p-Value | ||
| Overall | SACS | 13.5 (±11.7) | 14.1 (±12.3) | 19.6 (±11.7) | 20.8 (±11.3) | 21.5 (±12.3) | +6.1 (±9.1) | <0.001 | +7.4 (±10.1) | <0.001 | +0.7 (±8.4) | 0.643 |
| SSA | 0.5 (±8.9) | 1.1 (±9.4) | 7.1 (±7.7) | 7.8 (±7.9) | 6.7 (±7.8) | +6.6 (±6.1) | <0.001 | +5.6 (±7.1) | <0.001 | −1.1 (±3.9) | 0.094 | |
| Trauma | SACS | 12.7 (±11.5) | 12.9 (±12.2) | 20.1 (±10.1) | 20.5 (±10.9) | 20.6 (±11.9) | +7.4 (±8.5) | <0.001 | +7.7 (±12.5) | <0.05 | +0.1 (±7.9) | 0.945 |
| SSA | −2.6 (±9.5) | −2.5 (±10.3) | 5.3 (±6.8) | 5.2 (±7.3) | 4.0 (±7.2) | +7.9 (±6.8) | <0.001 | +6.5 (±8.6) | <0.05 | −1.2 (±4.3) | 0.249 | |
| Degeneration | SACS | 14.3 (±13.4) | 15.4 (±13.1) | 18.6 (±14.3) | 20.6 (±12.2) | 21.4 (±12.7) | +4.3 (±10.0) | 0.111 | +6.0 (±5.6) | <0.05 | +0.8 (±9.3) | 0.728 |
| SSA | 5.4 (±6.0) | 5.8 (±6.1) | 10.6 (±7.9) | 11.3 (±7.7) | 10.1 (±7.5) | +5.2 (±5.3) | <0.05 | +4.3 (±4.8) | <0.05 | −1.2 (±3.5) | 0.202 | |
| Monosegmental | SACS | 11.8 (±12.9) | 12.5 (±13.4) | 18.1 (±13.1) | 19.7 (±12.6) | 20.7 (±13.4) | +6.3 (±9.7) | <0.05 | +8.2 (±10.4) | <0.05 | +1.0 (±7.6) | 0.553 |
| SSA | −0.9 (±9.4) | −0.6 (±10.1) | 5.2 (±7.0) | 5.4 (±7.6) | 4.3 (±7.4) | +6.1 (±6.9) | <0.05 | +4.9 (±8.3) | <0.05 | −1.1 (±4.2) | 0.247 | |
| Bi-/Trisegmental | SACS | 15.8 (±10.1) | 16.3 (±10.7) | 21.7 (±9.5) | 22.4 (±9.55) | 22.6 (±11.1) | +5.9 (±8.5) | <0.05 | +6.3 (±10.1) | <0.05 | +0.2 (±9.6) | 0.943 |
| SSA | 2.5 (±8.3) | 3.4 (±8.2) | 9.7 (±8.1) | 11.2 (±7.1) | 10.1 (±7.3) | +7.2 (±4.9) | <0.001 | +6.7 (±5.1) | <0.001 | −1.1 (±3.5) | 0.234 | |
| Groups | Angle | Preoperative to Postoperative | Postoperative to 12-Month Follow Up |
|---|---|---|---|
| p-Values | p-Values | ||
| Trauma vs. Degeneration | SACS | 0.302 | 0.808 |
| SSA | 0.185 | 0.991 | |
| Monosegmental vs. Bi-/trisegmental | SACS | 0.857 | 0.773 |
| SSA | 0.612 | 0.990 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Milavec, H.; Kellner, C.; Ravikumar, N.; Albers, C.E.; Lerch, T.; Hoppe, S.; Deml, M.C.; Bigdon, S.F.; Kumar, N.; Benneker, L.M. First Clinical Experience with a Carbon Fibre Reinforced PEEK Composite Plating System for Anterior Cervical Discectomy and Fusion. J. Funct. Biomater. 2019, 10, 29. https://doi.org/10.3390/jfb10030029
Milavec H, Kellner C, Ravikumar N, Albers CE, Lerch T, Hoppe S, Deml MC, Bigdon SF, Kumar N, Benneker LM. First Clinical Experience with a Carbon Fibre Reinforced PEEK Composite Plating System for Anterior Cervical Discectomy and Fusion. Journal of Functional Biomaterials. 2019; 10(3):29. https://doi.org/10.3390/jfb10030029
Chicago/Turabian StyleMilavec, Helena, Christoph Kellner, Nivetha Ravikumar, Christoph E. Albers, Till Lerch, Sven Hoppe, Moritz C. Deml, Sebastian F. Bigdon, Naresh Kumar, and Lorin M. Benneker. 2019. "First Clinical Experience with a Carbon Fibre Reinforced PEEK Composite Plating System for Anterior Cervical Discectomy and Fusion" Journal of Functional Biomaterials 10, no. 3: 29. https://doi.org/10.3390/jfb10030029
APA StyleMilavec, H., Kellner, C., Ravikumar, N., Albers, C. E., Lerch, T., Hoppe, S., Deml, M. C., Bigdon, S. F., Kumar, N., & Benneker, L. M. (2019). First Clinical Experience with a Carbon Fibre Reinforced PEEK Composite Plating System for Anterior Cervical Discectomy and Fusion. Journal of Functional Biomaterials, 10(3), 29. https://doi.org/10.3390/jfb10030029





