Abstract
Childbearing and infant care practices have dramatically evolved since the 15th century. Shifting away from traditional home-based experiences, with the emergence of the microbial aware era and the hospital as a quintessential sanitizing machine, early life has now long been characterized as a condition to be medically managed. Paradoxically, this ‘germ-free’ march towards a healthier early life environment has opened the door to greater microbial susceptibility and dysbiosis. Many studies have now established that infant exposure to excessive sanitation and hygiene regimens are associated with an increased risk for and onset of childhood immune system diseases. In this paper, we explore the ways in which biomedical-centered efforts to enhance early life have come at a cost to planetary health, in relation to infant microbial succession. We examine three major areas of early life that have been subject to the ‘ripple effect’ of hygiene and sanitation concerns—childbirth, home environment, and breastfeeding.
1. Introduction
Traditional practices of childbearing and infant care have long been replaced by modern science and medical technology in the western world today. While this transition to a biomedical model, where birth is ‘medicalized’ such that it is perceived to be a condition that requires medical management [1], has enhanced the probability of survival, it has also introduced much controversy. From a planetary health perspective, whether the medicalization of early childhood is an environmentally sustainable approach in which our present and future generation can flourish is a concern [2,3]. Research evidence has demonstrated that biomedical-centered efforts to improve childbirth processes has come at the cost of downstream adverse events, such as greater susceptibility to nosocomial infection [4] and increased burden of immunological diseases [5]. Grounded on historical trends and recent research findings, this paper highlights key areas in which early life has been medicalized in the context of planetary health, i.e., infant microbial succession, which is important for development of the immune system and affects the likelihood of developing childhood and adult diseases [6]. Specifically, we present an argument which suggests the ‘ripple effect’ of hygiene and sanitation concerns (see Figure 1), which have underpinned the medicalization of childbirth and early infant care practices over time.
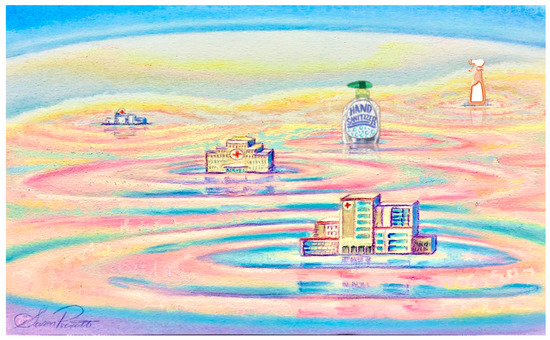
Figure 1.
Ripple effect of the medicalization of childbirth and early infant care practices.
2. The Modern Hospital
The concept of the ‘modern’ hospital as an instrument for therapeutic intervention and healing of disease began in late 15th century Europe [7]. Evolving through movements in social and societal norms, key reformations to health care included the consolidation of diverse health centres in Spain to economize delivery of care, the medicalization of hospitals in England, and the emergence of the hospital as the quintessential sanitizing machine in the US.
Microbes and their infection of humans have played a fundamental role in modern hospital practices. For instance, the theory and understanding of microbes led to the development of isolated pavilions to prevent transmission of hospital-acquired infections and the introduction of laboratories in hospitals. Disciplines of bacteriology and chemistry in the late 19th century further added to the reputation of the hospital as a site for infection control. Reaching beyond the surgical operating room, the battle against microbes became one of the earliest pillars of modern medicine and sought to pervade every single practice and specialty. Inevitably, birth practices and early childhood care were subjected to the transformational shifts associated with widespread medicalization and sanitization practices in this microbe aware era.
3. Medicalization of Birth: Home to Hospital
In almost all industrialized countries, birth in the modern hospital is deemed to be the safest and most comfortable place to give birth; however, before the 20th century, most women gave birth at home [8]. Surrounded by friends and family, and attended to by midwives and physicians, the home bed was viewed as a more desirable, comfortable, and safe birth setting. As the number of physicians specializing in obstetrics grew in the 20th century, home birth came under scrutiny. New knowledge about bacteriology and germ transmission also made home delivery difficult to manage from the infection control perspective. Despite these feelings of uneasiness about the cleanliness of home birth, ironically, it was maternal mortality from childbirth or ‘puerperal fever’ in the hospital that led to the discovery of the ‘germ theory’ [9]. Although microbes had already been discovered in 1674, little was known regarding their roles, especially in relation to infection. As such, it was not uncommon for physicians to perform autopsies and directly transition to delivering newborns without taking proper sanitation measures in between. However, such practices were no longer tolerated with the establishment of hospital infection control in the 1900s. At this time, the desire and demand for safe and controlled hospital births increased among both childbearing women and physicians. In the US alone, the proportion of home births declined from more than 50% to only about 12% between 1930 to 1950 [8].
Today, despite the continued trend towards hospital births, an exception known as the ’Dutch way of birth’ exists, where the home is still considered the proper place for birth, and midwives the preferred caregivers. Compared to a mere 3% in other industrialized countries, in the Netherlands, almost one-third of births occur at home. In fact, the Netherlands has the lowest caesarean and infant mortality rates in the world, and evidence suggests that home births attended by midwives is as safe as hospital births [10]. Further evidence has demonstrated that in industrialized countries, hospital birth can be detrimental due to a relation with greater risk for unnecessary medical intervention [11]. As such, the medicalization of birth has been put into question, with studies now suggesting that the safety paradox of institutionalized birth has introduced new areas of risk. One ethnographic study of an obstetric hospital unit by Newnham et al. illustrated how women in labour are often pushed through the system and propelled into interventions to keep up with the pace of the hospital rather than being allowed to have a physiologic, naturally progressing birth [12].
4. Sanitization of Birth: Caesarean Delivery
A further development in the delivery of infants—caesarean section—has resulted in birth becoming an even more sanitized situation. The first successful caesarean section was performed by Mary Donally in the British Isles in 1738 [13]. By the twentieth century, medicalization of birth resulted in a significant reduction in the number of newborn and maternal deaths during birth in industrialized countries. Arguably, the most beneficial of interventions for birth have been the use of soap to stop the spread of infectious diseases, infant heart rate monitoring, and the use of aseptic protocols, including maternal antibiotic prophylaxis prior to caesarean section, and anesthesia. The latter allowed for the widespread introduction of caesarean section delivery. Current standard practice is for Canadian women who undergo caesarean section to receive antibiotic prophylaxis [14].
Over the past 150 years, caesarean rates have surged, doubling over the past decade to an alarming global rate of 21.1% [15]. In some countries such as Brazil, 80 to 90% of babies are born by caesarean in private hospitals, which, in comparison to public sector rates of 40 to 50%, introduces financial incentives for hospitals, often persuading women to believe caesarean delivery is the safest option [15]. In North America, caesarean rates have reached up to 32% [16], with Canadian rates following close behind at 28% [17]. Despite its often discussed medical and economic benefits, caesarean section is not a risk-free endeavour. Both elective and emergency caesarean section have been found to increase the risk of maternal morbidity and mortality, and fetal and neonatal morbidity when the recommended rates set by WHO of 10 to 15% are exceeded [18]. Of concern, caesarean section rates are mainly driven by repeat caesarean delivery, elective caesarean delivery, and caesarean delivery after failed induction, of which medical indication is often absent [19]. In one Canadian city (Edmonton, AB), caesarean section rates range by neighbourhood of residence, between 20 to 31% [20]. These rates are suggested to fluctuate depending on hospital proximity.
Caesarean section has both auxiliary psychosocial and physical health consequences [21]. Maternal–infant bonding can be delayed in caesarean section birth, which can delay neurodevelopment and impede breastfeeding. As a result, infants born by caesarean section are less likely to be breastfed in the hospital, a known factor in supporting a healthy infant gut microbiome and reducing childhood obesity [22]. Further, maternal postpartum depression appears to be increased by caesarean section, a consequence which is often overlooked in prominent reviews on the topic [23].
Putatively, the greatest impact of caesarean birth is its effects on maternal–infant transmission of the microbiome during birth. The revolution in human microbiome research has brought to the forefront of health research both the immediate and long-term outcomes of the interruption of physiologic, naturally progressing birth. Maternal intergenerational transmission is not unique to humans. Millions of years of evolution has perfected this inoculation of microbes at birth [24], laying the foundation for microbial succession and stimulation of the infant immune system. Any disturbances during this critical period pose threats to the vulnerable infant while altering the course of development. Over the course of pregnancy, the mother’s vaginal and gut microbiome undergo a cascade of specific changes ensuring the transmission of ancestral microbes [25]. Early pioneer bacteria such as Enterobacteriaceae and lactic acid bacteria [26], which coincidently are increased during pregnancy, are crucial during transmission at birth to allow initial and subsequent microbial succession of beneficial bacteria. Most notably, in infants born by caesarean section is the depletion of Bacteroidetes at three months [27], which is acquired from the maternal gut microbiota during delivery, and is the result of this disrupted and delayed assembly of pioneer bacteria at birth. Modern day birth practices, such as caesarean delivery, deprive infants of this natural system of maternal inheritance which has undoubtedly coincided with increases in metabolic and immune disorders later in life [21,28].
5. Sanitization of Birth: Antibiotics during Vaginal Birth
Antibiotics are used as a standard of practice not only for caesarean births, but notably for vaginal deliveries as well. Newborns may acquire group B Streptococcus (GBS) from their mother during vaginal delivery, and although it is not very common, GBS infection may be seriously life-threatening to neonates. To prevent this, it is the standard of care in most countries to provide intrapartum antibiotic prophylaxis (IAP) to GBS-positive women [29]. Preventive measures with the use of IAP started gaining momentum in the 1900s; however, disagreements as to which strategies should be employed existed. By 1996, the first consensus guideline for IAP was established by joint efforts from members of the American Academy of Pediatrics (AAP), American College of Obstetricians and Gynaecologists (ACOG), and Centers for Disease Control and Prevention (CDC). With this new guideline, before 2000, almost all hospitals and obstetricians in North America had adopted and shared similar practices for maternal IAP [30]. However, today, there is a global disparity in IAP guidelines. In the United Kingdom and Netherlands, IAP administration is based on a progressive clinical risk assessment procedure. In contrast, in North America, including Canada, women are routinely given IAP if they are GBS positive [31,32]. As such, North American neonates are substantially more likely to be exposed to antibiotics during vaginal delivery. Without IAP, the risk of acquiring GBS infection in neonates is fairly small [32]. Yet, in most North American countries, most women are given these antibiotics, which unnecessarily exposes both mother and child to antibiotic-induced gut dysbiosis and antimicrobial resistance.
Infants are particularly susceptible soon after birth to changes in their microbiome. Maternal IAP not only targets the GBS but also other beneficial bacteria, which thereby has the ability to affect initial colonization of the newborn gut and natural succession of gut microbiota throughout infancy. It also has the capacity to result in the emergence of antibiotic resistance genes. Azad et al. reported gut dysbiosis following maternal IAP administration up to three months of infant age, with reductions in Bacteroidaceae, as also seen following caesarean birth [33]. Similar evidence of infant gut dysbiosis post IAP was reported by Nogacka and colleagues, as well as the enrichment of beta-lactamase resistant genes [34]. In another study, differing succession of bacterial community was observed between IAP exposed and control full-term infants [35]. In fact, women who are to receive IAP are indicated to have at-risk pregnancies and more likely to undergo a series of interventions such as increased hospitalization [36].
6. Sanitization in the Home after Childbirth
Sanitization can extend from the hospital to the home environment after childbirth. Since home hygiene and housework go hand in hand, the degree of sanitization often reflects pre-birth practices of parents. As evident in household production studies and discourse analyses of advertisements aimed at women in industrialized countries [37,38], housework and use of cleaning products has declined steadily in industrialized countries since the 1950s. In the 1950s, portrayal of the ‘domestic mother’ frequently placed her in the kitchen or living room holding a cleaning product [37]. Cleaning products were somewhat less frequently advertised in the 1970s at a time when packaged food products were promoted for the ‘efficient mother’. They were shelved in the 1980s in adverts of child products targeting the ‘nurturing mother’ but made a resurgence in the 1990’s in adverts of the ‘expertise-guided’ mother.
In current times, many parents in industrialized countries understand that a newborn’s immune system is immature, are concerned about the impact of household ‘germs’ on the infant’s immune system, and will increase their efforts to hand wash with soap after diaper changes and to regularly use antibacterial cleaning products to prevent the transfer of germs. These beliefs have been nicely captured in the qualitative component of the Curtis et al. multi-method study [39]. This UK study conducted in the early 2000s also revealed that the birth of a child may motivate mothers to use antibacterial agents for the first time. In contrast, it has been documented that mothers in some non-industrialized countries do not regard child excreta as dangerous [40]. Diaper changes mainly took place in the living room in the UK study, a common gathering place for children and parents in the US as well, and the likely focus of cleaning for outwards appearances [39,41]. Indeed, using excretion of the polio vaccine virus as a clever marker to trace household deposition of infant feces, Curtis et al. found evidence of fecal contamination in 12% of living room samples [39].
Medical opinion has been gaining influence since the 1980s in the use of many childhood products [37]. With the rising rates of preterm birth, parents are increasingly at the receiving end of hospital practices and recommendations to create a sanitary home environment post-birth [42]. It is noteworthy that in the CHILD birth cohort study, household disinfectants were used more frequently after the delivery of an infant by caesarean section than by vaginal birth [43]. Hand sanitizers, which made their appearance in hospitals first [44], make this portable hygiene method convenient for families as they spend more time on recreational activities [38]. They are now recommended in the WHO Multi-modal Hand Hygiene Improvement Strategy [44]. Coupled with common general knowledge about bacteria and concern over infection in young infants [39], evidence is already emerging that widespread availability of inexpensive and easy-to-use multi-surface cleaners and hand sanitizers can alter infant gut microbiota and increase risk for non-communicable disease [43].
7. Sanitization of Breastfeeding in Canada
Breastfeeding practices are shaped by several multifaceted factors, from socioeconomic and health related influences to societal expectations. Consequently, the understanding of current breastfeeding practices takes a multi-disciplinary approach that must consider both biological and sociological determinants. Recommendations surrounding infant feeding have gone back and forth between formula use and breastfeeding over the years, thus complicating the situation further [45]. Before the 1890s, the use of formula was discouraged because of an apparent association with infant mortality. Ultimately, this association was caused by improper storage, thus spoilage of the bottled milk. Shortly after, a greater understanding and study of microbes led to the development of germ theory, creating radical changes in cleanliness and pasteurization, making formula appear to be the superior method of infant feeding. Most recently in the 2000s, when the field of microbiology was further revolutionized with the discovery of the microbiome and its importance in many health outcomes, there has been a re-evaluation of the importance of breastfeeding. This evolution in practice coincides with modern culture in Canada and most other countries, where medical norms such as caesarean section delivery and hospitalization makes early breastfeeding more challenging for new mothers. In fact, when modern day women are asked to express their perceptions of breastfeeding, their response has largely been one of confusion and misinformation, especially for those of lower socioeconomic status [46]. These women may lack support and education surrounding breastfeeding, feel pressured to breastfeed but are unable to due to exhaustion (i.e., after a caesarean section surgery, work, or colicky behaviour), feel their milk is inadequate due to diet and habits (i.e., smoking), feel burdened by the stigma around breastfeeding in public, and face difficulties learning to breastfeed while in hospital. Efforts to raise an awareness about the current breastfeeding guidelines and to ensure that all women are educated, empowered, and supported to breastfeed are needed.
Early infant feeding practices have profound impacts on the gut microbiome of infants. Breast milk is exceptionally complex in that it contains particular nutrients such as milk sugars that are of utmost importance in the development of the infant gut microbiome. In addition to promoting skin-to-skin contact between the mother and the infant, breastfeeding encourages key bacteria to thrive as a result of specific breast milk components (i.e., cells, proteins, enzymes, and antibodies). As such, the gut microbial profiles of breastfed and formula-fed infants are undoubtedly unique [47]. Formula feeding, partial breastfeeding, and donor milk feeding have not demonstrated the same benefits in terms of the maturation of the gut microbiota as has breastfeeding. While one might consider formula feeding a more ‘sanitary’ practice, the hygiene hypothesis suggests that these feeding practices may hinder immune maturation in infants with lack of early microbial exposure [48]. Thus, it is not surprising that many of the beneficial health outcomes attributed to breastfeeding are now also associated with early microbial seeding, both from the bacteria directly within breast milk and also the select groups of bacteria that thrive on this natural and nutritious food source [49].
Early introduction and maintenance of breastfeeding until at least six months are now the central components in current guidelines for mothers and their newborns [50]. Still yet, despite this resurgence in appreciation for breastfeeding, factors such as medical interventions, modernization of birth and short maternity leaves can discourage families from adhering to breastfeeding guidelines. Rather, families may opt for shorter breastfeeding periods and supplementation with formula. Further, tube feeding rates are on the rise, even though there are contentions of its ability to provide proper nutrition and its downstream effects on chronic disease [51]. Tube feeding may also prevent skin-to-skin contact, the lack of which has been widely understood to inhibit proper neurodevelopment and maternal attachment. While this is without a doubt a barrier to optimal infant health and development, some research suggests that it may even be beneficial for families to choose partial breastfeeding with addition of complementary foods for up to two years. The arguments for the beneficial effects of prolonged breastfeeding are largely a result of the current microbiome-related research, particularly in relation to atopic disease [48].
8. The Clean Road Ahead?
The medicalization and sanitization of birth and early infant care is considered the norm in much of the developed world. However, using the Netherlands as an example, small pockets still exist where an effort to reduce the amount of medical intervention in birth has been made. Given the evidence on higher maternal satisfaction with childbirth for planned home births compared to hospital births, such resistive efforts hold reasonable ground [52]. In fact, with recent discoveries demonstrating the integral role of maternal–infant transmission at birth in the ecological succession of infant microbes, modern day birth practices are becoming increasingly scrutinized. For instance, due to potential microbiome-related adverse effects [33,53] and subsequent long-term consequences of childhood atopic dermatitis and asthma [54,55], efforts to minimize antibiotic use in early life are now growing. In regards to maternal breastfeeding, while the decision to formula feed or breastfeed remains with the mother, clinicians now have the responsibility to promote infant care practices which may not necessarily align with the popularized biomedical model. Whilst on this march towards creating a ‘germ-free’ early life environment, we have come full circle to understanding its cost to planetary health.
Author Contributions
All authors contributed substantially to this work. Conceptualization, S.J. and A.K.; Writing—Original Draft Preparation, S.J., K.D., B.M., C.M., C.N., C.V.O., A.v.d.L., and A.K.; Writing—Review and Editing, S.J., C.N., A.v.d.L., and A.K.; Supervision, A.K.; Project Administration, S.J.
Acknowledgments
The authors would like to acknowledge Dr. Susan Prescott for her creative and artistic contributions to Figure 1.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Parry, D.C. “We wanted a birth experience, not a medical experience”: Exploring Canadian women’s use of midwifery. Health Care Women Int. 2008, 29, 784–806. [Google Scholar] [CrossRef] [PubMed]
- Lerner, H.; Berg, C. A Comparison of Three Holistic Approaches to Health: One Health, EcoHealth, and Planetary Health. Front. Vet. Sci. 2017, 4, 163. [Google Scholar] [CrossRef] [PubMed]
- Whitmee, S.; Haines, A.; Beyrer, C.; Boltz, F.; Capon, A.G.; de Souza Dias, B.F.; Ezeh, A.; Frumkin, H.; Gong, P.; Head, P.; et al. Safeguarding human health in the Anthropocene epoch: Report of the Rockefeller Foundation-Lancet Commission on planetary health. Lancet 2015, 386, 1973–2028. [Google Scholar] [CrossRef]
- Zafar, N.; Wallace, C.M.; Kieffer, P.; Schroeder, P.; Schootman, M.; Hamvas, A. Improving survival of vulnerable infants increases neonatal intensive care unit nosocomial infection rate. Arch. Pediatr. Adolesc. Med. 2001, 155, 1098–1104. [Google Scholar] [CrossRef] [PubMed]
- Sevelsted, A.; Stokholm, J.; Bonnelykke, K.; Bisgaard, H. Cesarean section and chronic immune disorders. Pediatrics 2015, 135, e92–e98. [Google Scholar] [CrossRef] [PubMed]
- Houghteling, P.D.; Walker, W.A. Why is initial bacterial colonization of the intestine important to infants’ and children’s health? J. Pediatr. Gastroenterol. Nutr. 2015, 60, 294–307. [Google Scholar] [CrossRef] [PubMed]
- Gomez Pineda, F.H. Incorporation of the health care system in the west. Colomb. Med. 2015, 46, 144–149. [Google Scholar] [PubMed]
- Leavitt, J.W. What do men have to do with it? Fathers and mid-twentieth-century childbirth. Bull. Hist. Med. 2003, 77, 235–262. [Google Scholar] [CrossRef] [PubMed]
- Carter, K.C. Ignaz Semmelweis, Carl Mayrhofer, and the rise of germ theory. Med. Hist. 1985, 29, 33–53. [Google Scholar] [CrossRef] [PubMed]
- De Vries, R.; Lemmens, T. The social and cultural shaping of medical evidence: Case studies from pharmaceutical research and obstetric science. Soc. Sci. Med. 2006, 62, 2694–2706. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Townend, J.; Rowe, R.; Brocklehurst, P.; Knight, M.; Linsell, L.; Macfarlane, A.; McCourt, C.; Newburn, M.; Marlow, N.; et al. Perinatal and maternal outcomes in planned home and obstetric unit births in women at ‘higher risk’ of complications: Secondary analysis of the Birthplace national prospective cohort study. BJOG 2015, 122, 741–753. [Google Scholar] [CrossRef] [PubMed]
- Newnham, E.C.; McKellar, L.V.; Pincombe, J.I. Paradox of the institution: Findings from a hospital labour ward ethnography. BMC Pregnancy Childbirth 2017, 17, 2. [Google Scholar] [CrossRef] [PubMed]
- Drife, J. The start of life: A history of obstetrics. Postgrad. Med. J. 2002, 78, 311–315. [Google Scholar] [CrossRef] [PubMed]
- Van Schalkwyk, J.; Van Eyk, N.; Infectious Diseases Committee. Antibiotic prophylaxis in obstetric procedures. J. Obstet. Gynaecol. Can. 2010, 32, 878–884. [Google Scholar] [CrossRef]
- Betran, A.P.; Temmerman, M.; Kingdon, C.; Mohiddin, A.; Opiyo, N.; Torloni, M.R.; Zhang, J.; Musana, O.; Wanyonyi, S.Z.; Gulmezoglu, A.M.; et al. Interventions to reduce unnecessary caesarean sections in healthy women and babies. Lancet 2018, 392, 1358–1368. [Google Scholar] [CrossRef]
- Boerma, T.; Ronsmans, C.; Melesse, D.Y.; Barros, A.J.D.; Barros, F.C.; Juan, L.; Moller, A.B.; Say, L.; Hosseinpoor, A.R.; Yi, M.; et al. Global epidemiology of use of and disparities in caesarean sections. Lancet 2018, 392, 1341–1348. [Google Scholar] [CrossRef]
- Betrán, A.P.; Ye, J.; Moller, A.B.; Zhang, J.; Gülmezoglu, A.M.; Torloni, M.R. The increasing trend in caesarean section rates: Global, regional and national estimates: 1990–2014. PLoS ONE 2016. [Google Scholar] [CrossRef] [PubMed]
- Betran, A.P.; Torloni, M.R.; Zhang, J.; Ye, J.; Mikolajczyk, R.; Deneux-Tharaux, C.; Oladapo, O.T.; Souza, J.P.; Tunçalp, O.Z.; Vogel, J.P.; et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod. Health 2015, 12, 57. [Google Scholar] [CrossRef] [PubMed]
- Kelly, S.; Sprague, A.; Fell, D.B.; Murphy, P.; Aelicks, N.; Guo, Y.; Fahey, J.; Lauzon, L.; Scott, H.; Lee, L.; et al. Examining caesarean section rates in Canada using the Robson classification system. J. Obstet. Gynaecol. Can. 2013, 35, 206–214. [Google Scholar] [CrossRef]
- Alberta Health. Hospital Delivery Method Age-Standardized Percent—by Geography, 1997–2014 [Digital Data]. Available online: http://www.ahw.gov.ab.ca/IHDA_Retrieval/redirectToURL.do?cat=4&subCat=767 (accessed on 12 December 2018).
- Keag, O.E.; Norman, J.E.; Stock, S.J. Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: Systematic review and meta-analysis. PLoS Med. 2018, 15, e1002494. [Google Scholar] [CrossRef] [PubMed]
- Forbes, J.D.; Azad, M.B.; Vehling, L.; Tun, H.M.; Konya, T.B.; Guttman, D.S.; Field, C.J.; Lefebvre, D.; Sears, M.R.; Becker, A.B.; et al. Association of Exposure to Formula in the Hospital and Subsequent Infant Feeding Practices with Gut Microbiota and Risk of Overweight in the First Year of Life. JAMA Pediatr. 2018, 172, e181161. [Google Scholar] [CrossRef] [PubMed]
- Carter, F.A.; Frampton, C.M.; Mulder, R.T. Cesarean section and postpartum depression: A review of the evidence examining the link. Psychosom. Med. 2006, 68, 321–330. [Google Scholar] [CrossRef] [PubMed]
- Blaser, M.J.; Dominguez-Bello, M.G. The Human Microbiome before Birth. Cell Host Microbe 2016, 20, 558–560. [Google Scholar] [CrossRef] [PubMed]
- Koren, O.; Goodrich, J.K.; Cullender, T.C.; Spor, A.; Laitinen, K.; Backhed, H.K.; Gonzalez, A.; Werner, J.J.; Angenent, L.T.; Knight, R.; et al. Host remodeling of the gut microbiome and metabolic changes during pregnancy. Cell 2012, 150, 470–480. [Google Scholar] [CrossRef] [PubMed]
- Koleva, P.T.; Kim, J.S.; Scott, J.A.; Kozyrskyj, A.L. Microbial programming of health and disease starts during fetal life. Birth Defects Res C Embryo Today 2015, 105, 265–277. [Google Scholar] [CrossRef] [PubMed]
- Ho, N.T.; Li, F.; Lee-Sarwar, K.A.; Tun, H.M.; Brown, B.P.; Pannaraj, P.S.; Bender, J.M.; Azad, M.B.; Thompson, A.L.; Weiss, S.T.; et al. Meta-analysis of effects of exclusive breastfeeding on infant gut microbiota across populations. Nat. Commun. 2018, 9, 4169. [Google Scholar] [CrossRef] [PubMed]
- Tun, H.M.; Bridgman, S.L.; Chari, R.; Field, C.J.; Guttman, D.S.; Becker, A.B.; Mandhane, P.J.; Turvey, S.E.; Subbarao, P.; Sears, M.R.; et al. Roles of Birth Mode and Infant Gut Microbiota in Intergenerational Transmission of Overweight and Obesity from Mother to Offspring. JAMA Pediatr. 2018, 172, 368–377. [Google Scholar] [CrossRef] [PubMed]
- Homer, C.S.; Scarf, V.; Catling, C.; Davis, D. Culture-based versus risk-based screening for the prevention of group B streptococcal disease in newborns: A review of national guidelines. Women Birth 2014, 27, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Tumbaga, P.F.; Philip, A.G.S. Perinatal Group B Streptococcal Infections: Past, Present, and Future. NeoReviews 2003, 4, e65–e72. [Google Scholar] [CrossRef]
- Le Doare, K.; O’Driscoll, M.; Turner, K.; Seedat, F.; Russell, N.J.; Seale, A.C.; Heath, P.T.; Lawn, J.E.; Baker, C.J.; Bartlett, L.; et al. Intrapartum Antibiotic Chemoprophylaxis Policies for the Prevention of Group B Streptococcal Disease Worldwide: Systematic Review. Clin. Infect. Dis. 2017, 65, S143–S151. [Google Scholar] [CrossRef] [PubMed]
- Jefferies, A.L. Management of term infants at increased risk for early-onset bacterial sepsis. Paediatr. Child Health 2017, 22, 223–228. [Google Scholar] [CrossRef] [PubMed]
- Azad, M.B.; Konya, T.; Persaud, R.R.; Guttman, D.S.; Chari, R.S.; Field, C.J.; Sears, M.R.; Mandhane, P.J.; Turvey, S.E.; Subbarao, P.; et al. Impact of maternal intrapartum antibiotics, method of birth and breastfeeding on gut microbiota during the first year of life: A prospective cohort study. BJOG 2016, 123, 983–993. [Google Scholar] [CrossRef] [PubMed]
- Nogacka, A.; Salazar, N.; Suarez, M.; Milani, C.; Arboleya, S.; Solis, G.; Fernandez, N.; Alaez, L.; Hernandez-Barranco, A.M.; de Los Reyes-Gavilan, C.G.; et al. Impact of intrapartum antimicrobial prophylaxis upon the intestinal microbiota and the prevalence of antibiotic resistance genes in vaginally delivered full-term neonates. Microbiome 2017, 5, 93. [Google Scholar] [CrossRef] [PubMed]
- Stearns, J.C.; Simioni, J.; Gunn, E.; McDonald, H.; Holloway, A.C.; Thabane, L.; Mousseau, A.; Schertzer, J.D.; Ratcliffe, E.M.; Rossi, L.; et al. Intrapartum antibiotics for GBS prophylaxis alter colonization patterns in the early infant gut microbiome of low risk infants. Sci. Rep. 2017, 7, 16527. [Google Scholar] [CrossRef] [PubMed]
- Kurz, E.; Davis, D. Routine culture-based screening versus risk-based management for the prevention of early-onset group B streptococcus disease in the neonate: A systematic review. JBI Database Syst. Rev. Implement. Rep. 2015, 13, 206–246. [Google Scholar] [CrossRef] [PubMed]
- Lynch, K.D. Advertising Motherhood: Image, Ideology, and Consumption. Berkeley J. Sociol. 2005, 49, 32–57. [Google Scholar]
- Huffman, W. Household Production and the Demand for Food and Other Inputs: US Evidence. J. Agric. Resour. Econ. 2011, 36, 465–487. [Google Scholar]
- Curtis, V.; Biran, A.; Deverell, K.; Hughes, C.; Bellamy, K.; Drasar, B. Hygiene in the home: Relating bugs and behaviour. Soc. Sci. Med. 2003, 57, 657–672. [Google Scholar] [CrossRef]
- Kanki, B.; Curtis, V.; Mertens, T.; Cousens, S.; Traoré, E. Measuring Hygiene Behaviours: Experiences of a Comprehensive approach in Burkina Faso. In Studying Hygiene Behaviour: Issues and Experiences; Cairnross, S., Kochar, V., Eds.; Sage Publications: London, UK, 1994. [Google Scholar]
- Broege, N.; Owens, A.; Graesch, A.P.; Arnold, J.E.; Schneider, B. Calibrating measures of family activities between large- and small-scale data sets. Sociol. Methodol. 2007, 37, 119–149. [Google Scholar] [CrossRef]
- Hobbs, J.E.; Tschudy, M.; Hussey-Gardner, B.; Jennings, J.; Boss, R.D. “I Don’t Know What I Was Expecting”: Home Visit. By Neonatol. Fellows Infants Discharged NICU. Birth 2017, 44. [Google Scholar] [CrossRef] [PubMed]
- Tun, M.H.; Tun, H.M.; Mahoney, J.J.; Konya, T.B.; Guttman, D.S.; Becker, A.B.; Mandhane, P.J.; Turvey, S.E.; Subbarao, P.; Sears, M.R.; et al. Postnatal exposure to household disinfectants, infant gut microbiota and subsequent risk of overweight in children. CMAJ 2018, 190, E1097–E1107. [Google Scholar] [CrossRef] [PubMed]
- Vermeil, T.; Peters, A.; Kilpatrick, C.; Pires, D.; Allegranzi, B.; Pittet, D. Hand hygiene in hospitals: Anatomy of a revolution. J. Hosp. Infect. 2018. [Google Scholar] [CrossRef] [PubMed]
- Stevens, E.E.; Patrick, T.E.; Pickler, R. A history of infant feeding. J. Périnat. Educ. 2009, 18, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Newhook, J.T.; Ludlow, V.; Newhook, L.A.; Bonia, K.; Goodridge, J.M.; Twells, L. Infant-feeding among low-income women: The social context that shapes their perspectives and experiences. Can. J. Nurs. Res. 2013, 45, 28–49. [Google Scholar] [CrossRef] [PubMed]
- Azad, M.B.; Konya, T.; Maughan, H.; Guttman, D.S.; Field, C.J.; Chari, R.S.; Sears, M.R.; Becker, A.B.; Scott, J.A.; Kozyrskyj, A.L.; et al. Gut microbiota of healthy Canadian infants: Profiles by mode of delivery and infant diet at 4 months. Can. Med. Assoc. J. 2013, 185, 385–394. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, S.; Friedberg, I.; Ivanov, I.V.; Davidson, L.A.; Goldsby, J.S.; Dahl, D.B.; Herman, D.; Wang, M.; Donovan, S.M.; Chapkin, R.S. A metagenomic study of diet-dependent interaction between gut microbiota and host in infants reveals differences in immune response. Genome Biol. 2012, 13, r32. [Google Scholar] [CrossRef] [PubMed]
- Pannaraj, P.S.; Li, F.; Cerini, C.; Bender, J.M.; Yang, S.; Rollie, A.; Adisetiyo, H.; Zabih, S.; Lincez, P.J.; Bittinger, K.; et al. Association Between Breast Milk Bacterial Communities and Establishment and Development of the Infant Gut Microbiome. JAMA Pediatr. 2017, 171, 647–654. [Google Scholar] [CrossRef] [PubMed]
- Eidelman, A.I.; Schanler, R.J.; Johnston, M.; Landers, S.; Noble, L.; Szucs, K.; Viehmann, L.; Feldman-Winter, L.; Lawrence, R.; Kim, S.; et al. Breastfeeding and the use of human milk. Pediatrics 2012, 129, e827–e841. [Google Scholar] [CrossRef]
- Spagnuolo, M.I.; Chiatto, F.; Buccigrossi, V.; Morlando, A.; Mambretti, D.; Aceto, B.; Laudiero, F.; Giordano, F.; Guarino, A. P154 Analysis of the pediatric home enteral nutrition in Campania region: Implementation rates and observed trends during the past 10 years. Dig. Liver Dis. 2018, 50, e412. [Google Scholar] [CrossRef]
- Christiaens, W.; Bracke, P. Place of birth and satisfaction with childbirth in Belgium and The Netherlands. Midwifery 2009, 25, e11–e19. [Google Scholar] [CrossRef] [PubMed]
- Ohlsson, A.; Shah, V.S. Intrapartum antibiotics for known maternal Group B streptococcal colonization. Cochrane Database Syst. Rev. 2014. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Feldman, A.S.; Rosas-Salazar, C.; James, K.; Escobar, G.; Gebretsadik, T.; Li, S.X.; Carroll, K.N.; Walsh, E.; Mitchel, E.; et al. Relative importance and additive effects of maternal and infant risk factors on childhood asthma. PLoS ONE 2016, 11, e0151705. [Google Scholar] [CrossRef] [PubMed]
- Wohl, D.L.; Curry, W.J.; Mauger, D.; Miller, J.; Tyrie, K. Intrapartum Antibiotics and Childhood Atopic Dermatitis. J. Am. Board Fam. Med. 2015, 28, 82–89. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).