Phosphatidylethanol for Monitoring Alcohol Use in Liver Transplant Candidates: An Observational Study
Abstract
:1. Introduction
2. Methods
2.1. Study Design
2.2. Study Population and Procedure
2.3. Biomarker Assessment
2.4. Statistical Analysis
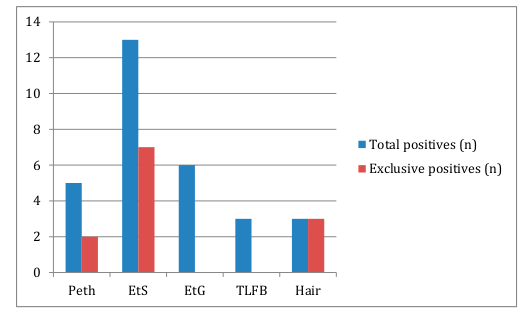
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Burra, P.; Senzolo, M.; Adam, R.; Delvart, V.; Karam, V.; Germani, G.; Neuberger, J.; ELITA; ELTR Liver Transplant Centers. Liver Transplantation for Alcoholic Liver Disease in Europe: A Study from the ELTR (European Liver Transplant Registry). Am. J. Transpl. 2010, 10, 138–148. [Google Scholar] [CrossRef] [PubMed]
- Burroughs, A.-K.; Sabin, C.; Rolles, K.; Delvart, V.; Karam, V.; Buckels, J.; O’Grady, J.G.; Castaing, D.; Klempnauer, J.; Jamieson, N.V.; et al. 3-month and 12-month mortality after first liver transplant in adults in Europe: Predictive models for outcome. Lancet 2006, 367, 225–232. [Google Scholar] [CrossRef] [Green Version]
- Marroni, N.P.; Fleck, A.M., Jr.; Fernandes, S.A.; Galant, L.H.; Mucenic, M.; Meine, M.H.D.M.; Mariante-Neto, G.; Brandão, A.B.D.M. Liver transplantation and alcoholic liver disease: History, controversies, and considerations. World J. Gastroenterol. 2018, 24, 2785–2805. [Google Scholar] [CrossRef] [PubMed]
- Kotlyar, D.S.; Burke, A.; Campbell, M.S.; Weinrieb, R.M. A Critical Review of Candidacy for Orthotopic Liver Transplantation in Alcoholic Liver Disease. Am. J. Gastroenterol. 2008, 103, 734–743. [Google Scholar] [CrossRef] [PubMed]
- Testino, G.; Leone, S. Acute alcoholic hepatitis: A literature review and proposal of treatment. Minerva Med. 2017, 109, 290–299. [Google Scholar]
- Frazier, T.H.; Stocker, A.M.; Kershner, N.A.; Marsano, L.S.; McClain, C.J. Treatment of alcoholic liver disease. Adv. Gastroenterol. 2010, 4, 63–81. [Google Scholar] [CrossRef] [Green Version]
- Jaurigue, M.M.; Cappell, M.S. Therapy for alcoholic liver disease. World J. Gastroenterol. 2014, 20, 2143–2158. [Google Scholar] [CrossRef]
- Marroni, N.P. Management of alcohol recurrence before and after liver transplantation. Clin. Res. Hepatol. Gastroenterol. 2015, 39, S109–S114. [Google Scholar] [CrossRef]
- Dew, M.A.; DiMartini, A.F.; Steel, J.; Dabbs, A.D.V.; Myaskovsky, L.; Unruh, M.; Greenhouse, J. Meta-analysis of risk for relapse to substance use after transplantation of the liver or other solid organs. Liver Transpl. 2008, 14, 159–172. [Google Scholar] [CrossRef] [Green Version]
- Testino, G. Alcohol and liver transplantation: The six-month abstinence rule is not a dogma. Transpl. Int. 2016, 29, 953–954. [Google Scholar] [CrossRef] [Green Version]
- Testino, G.; Burra, P.; Bonino, F.; Piani, F.; Sumberaz, A.; Peressutti, R.; Castiglione, A.G.; Patussi, V.; Fanucchi, T.; Ancarani, O.; et al. Acute alcoholic hepatitis, end stage alcoholic liver disease and liver transplantation: An Italian position statement. World J. Gastroenterol. 2014, 20, 14642–14651. [Google Scholar] [CrossRef]
- Saunders, J.B.; Whitfield, J.B.; Conigrave, K. Diagnostic tests for alcohol consumption. Alcohol Alcohol. 1995, 30, 13–26. [Google Scholar]
- Hock, B.; Schwarz, M.; Domke, I.; Grunert, V.P.; Wuertemberger, M.; Schiemann, U.; Horster, S.; Limmer, C.; Stecker, G.; Soyka, M. Validity of carbohydrate-deficient transferrin (%CDT), γ-glutamyltransferase (γ-GT) and mean corpuscular erythrocyte volume (MCV) as biomarkers for chronic alcohol abuse: A study in patients with alcohol dependence and liver disorders of non-alcoholic and alcoholic origin. Addiction 2005, 100, 1477–1486. [Google Scholar] [PubMed]
- Conigrave, K.M.; Degenhardt, L.J.; Whitfield, J.B.; Saunders, J.B.; Helander, A.; Tabakoff, B.; WHO/ISBRA Study Group. CDT, GGT, and AST as markers of alcohol use: The WHO/ISBRA collaborative project. Alcohol. Clin. Exp. Res. 2002, 26, 332–339. [Google Scholar] [CrossRef] [PubMed]
- Barrio, P.; Teixidor, L.; Rico, N.; Bruguera, P.; Ortega, L.; Bedini, J.L.; Gual, A. Urine Ethyl Glucuronide Unraveling the Reality of Abstinence Monitoring in a Routine Outpatient Setting: A Cross-Sectional Comparison with Ethanol, Self Report and Clinical Judgment. Eur. Addict. Res. 2016, 22, 243–248. [Google Scholar] [CrossRef] [PubMed]
- Staufer, K.; Andresen, H.; Vettorazzi, E.; Tobias, N.; Nashan, B.; Sterneck, M. Urinary ethyl glucuronide as a novel screening tool in patients pre- and post-liver transplantation improves detection of alcohol consumption. Hepatology 2011, 54, 1640–1649. [Google Scholar] [CrossRef] [PubMed]
- Stewart, S.H.; Koch, D.G.; Burgess, D.M.; Willner, I.R.; Reuben, A. Sensitivity and specificity of urinary ethyl glucuronide and ethyl sulfate in liver disease patients. Alcohol. Clin. Exp. Res. 2012, 37, 150–155. [Google Scholar] [CrossRef] [PubMed]
- Simons, J.S.; Wills, T.A.; Emery, N.N.; Marks, R.M. Quantifying alcohol consumption: Self-report, transdermal assessment, and prediction of dependence symptoms. Addict. Behav. 2015, 50, 205–212. [Google Scholar] [CrossRef] [Green Version]
- Wurst, F.M.; Thon, N.; Yegles, M.; Schrück, A.; Preuss, U.W.; Weinmann, W. Ethanol metabolites: Their role in the assessment of alcohol intake. Alcohol. Clin. Exp. Res. 2015, 39, 2060–2072. [Google Scholar] [CrossRef] [Green Version]
- Allen, J.P.; Wurst, F.M.; Thon, N.; Litten, R.Z. Assessing the drinking status of liver transplant patients with alcoholic liver disease. Liver Transpl. 2013, 19, 369–376. [Google Scholar] [CrossRef]
- Stewart, S.H.; Reuben, A.; Brzezinski, W.A.; Koch, D.G.; Basile, J.; Randall, P.K.; Miller, P.M. Preliminary Evaluation of Phosphatidylethanol and Alcohol Consumption in Patients with Liver Disease and Hypertension. Alcohol Alcohol. 2009, 44, 464–467. [Google Scholar] [CrossRef] [PubMed]
- Stewart, S.H.; Koch, D.G.; Willner, I.R.; Anton, R.F.; Reuben, A. Validation of Blood Phosphatidylethanol as an Alcohol Consumption Biomarker in Patients with Chronic Liver Disease. Alcohol. Clin. Exp. Res. 2014, 38, 1706–1711. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Andresen-Streichert, H.; Beres, Y.; Weinmann, W.; Schröck, A.; Müller, A.; Skopp, G.; Pischke, S.; Vettorazzi, E.; Lohse, A.; Nashan, B.; et al. Improved detection of alcohol consumption using the novel marker phosphatidylethanol in the transplant setting: Results of a prospective study. Transpl. Int. 2017, 30, 611–620. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fleming, M.F.; Smith, M.J.; Oslakovic, E.; Lucey, M.R.; Vue, J.X.; Al-Saden, P.; Levitsky, J. Phosphatidylethanol Detects Moderate-to-Heavy Alcohol Use in Liver Transplant Recipients. Alcohol. Clin. Exp. Res. 2017, 41, 857–862. [Google Scholar] [CrossRef] [PubMed]
- Bohn, M.J.; Babor, T.F.; Kranzler, H.R. The Alcohol Use Disorders Identification Test (AUDIT): Validation of a screening instrument for use in medical settings. J. Stud. Alcohol 1995, 56, 423–432. [Google Scholar] [CrossRef] [PubMed]
- Sobell, L.C.; Sobell, M.B. Timeline Follow-Back. In Measuring Alcohol Consumption; Humana Press: Totowa, NJ, USA, 1992; pp. 41–72. [Google Scholar]
- Barrio, P.; Wurst, F.M.; Gual, A. New Alcohol Biomarkers. New challenges. Alcohol Alcohol. 2018, 53, 762–763. [Google Scholar] [CrossRef] [Green Version]
- Reisfield, G.M.; Teitelbaum, S.A.; Large, S.O.; Jones, J.; Morrison, D.G.; Lewis, B. The roles of phosphatidylethanol (PEth), ethyl glucuronide (EtG), and ethyl sulfate (EtS) in identifying alcohol consumption among participants in professionals’ health programs. Drug Test. Anal. 2020, 12, 1102–1108. [Google Scholar] [CrossRef]
- Musshoff, F.; Albermann, E.; Madea, B. Ethyl glucuronide and ethyl sulfate in urine after consumption of various beverages and foods—Misleading results? Int. J. Leg. Med. 2010, 124, 623–630. [Google Scholar] [CrossRef]
- Stachel, N.; Skopp, G. Formation and inhibition of ethyl glucuronide and ethyl sulfate. Forensic Sci. Int. 2016, 265, 61–64. [Google Scholar] [CrossRef]
- Lindenger, C.; Castedal, M.; Schult, A.; Åberg, F. Long-term survival and predictors of relapse and survival after liver transplantation for alcoholic liver disease. Scand. J. Gastroenterol. 2018, 53, 1553–1561. [Google Scholar] [CrossRef]
- Rice, J.P.; Eickhoff, J.; Agni, R.; Ghufran, A.; Brahmbhatt, R.; Lucey, M.R. Abusive drinking after liver transplantation is associated with allograft loss and advanced allograft fibrosis. Liver Transpl. 2013, 19, 1377–1386. [Google Scholar] [CrossRef] [PubMed]
- Zemore, S.E. The effect of social desirability on reported motivation, substance use severity, and treatment attendance. J. Subst. Abus. Treat. 2012, 42, 400–412. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lopez Pelayo, H.; Altamirano, J.; Lopez, E.; Barrio, P.; Lopez, A.; Gual, A.; Lligoña, A. Role of Alcohol and Drug Detection by Regular Urine Sample Testing in pre-transplant evaluation for Alcohol Liver Disease. Adicciones 2018, 20, 1121. [Google Scholar] [CrossRef] [Green Version]
- Reisfield, G.M.; Goldberger, B.A.; Crews, B.O.; Pesce, A.J.; Wilson, G.R.; Teitelbaum, S.A.; Bertholf, R.L. Ethyl glucuronide, ethyl sulfate, and ethanol in urine after sustained exposure to an ethanol-based hand sanitizer. J. Anal. Toxicol. 2011, 35, 85–91. [Google Scholar] [CrossRef] [Green Version]
- Liu, Y.; Zhang, X.; Li, J.; Huang, Z.; Lin, Z.; Wang, J.; Zhang, C.; Rao, Y. Stability of Ethyl Glucuronide, Ethyl Sulfate, Phosphatidylethanols and Fatty Acid Ethyl Esters in Postmortem Human Blood. J. Anal. Toxicol. 2018, 42, 346–352. [Google Scholar] [CrossRef] [Green Version]
- Barrio, P.; Mondon, S.; Teixidor, L.; Ortega, L.; Vieta, E.; Gual, A. One Year Clinical Correlates of EtG Positive Urine Screening in Alcohol-Dependent Patients: A Survival Analysis. Alcohol Alcohol. 2017, 52, 460–465. [Google Scholar] [CrossRef]


| Variable | AUDIT negative (score <8) | AUDIT positive (score ≥8) |
|---|---|---|
| Sex (% men) | 83.3 | 87.5 |
| Age (years) | 56.8 | 53.6 |
| ASAT (mean (SD)) | 47.6 (20) UI/L | 34.6 (4) UI/L |
| ALAT (mean (SD)) | 34.9 (25) UI/L | 33 (28) UI/L |
| GGT (mean (SD)) | 89.9 (86) UI/L | 75.6 (11) UI/L |
| EtG positive (%) | 2.4% | 62.5% |
| EtS positive (%) | 19.5% | 62.5% |
| PeTH positive (%) | 7.1% | 25% |
| HEtG positive (%) | 3.4% | 66.7% |
| TLFB positive (%) | 0% | 37.5% |
| All biomarkers negative (%) | 76.2% | 37.5% |
| Other drugs used (%) | 11.9% | 25% |
| VHC (%) | 28.6% | 25% |
| Biomarker | Characteristics | References |
|---|---|---|
| EtG | Obtained from urine. Sensible to urine infections and reduced kidney function. Suitable for abstinence monitoring. Time-frame of detection up to a few days. Cut-off 0.5 mg/L | [15,16,17,19,20,27,28,29,30] |
| EtS | Obtained from urine. Sensible to urine infections and reduced kidney function. Suitable for abstinence monitoring. Time-frame of detection up to a few days. Cut-off 0.05 mg/L. | [17,19,20,31,32,33] |
| PeTH | Obtained from dried blood spots. Suitable for abstinence and heavy drinking monitoring. Timeframe of detection from days to weeks. Cut-off 20 ng/mL | [19,21,22,23,24] |
| HEtG | Obtained from hair. Sensible to contamination and extraction methods. Suitable for abstinence monitoring over long periods of time. Timeframe of detection from weeks to months. Cut-off 7 pg/mL. | [19] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barrio, P.; Gual, A.; Lligoña, A.; Teixidor, L.; Weinmann, W.; Yegles, M.; Wurst, F.M. Phosphatidylethanol for Monitoring Alcohol Use in Liver Transplant Candidates: An Observational Study. J. Clin. Med. 2020, 9, 3060. https://doi.org/10.3390/jcm9093060
Barrio P, Gual A, Lligoña A, Teixidor L, Weinmann W, Yegles M, Wurst FM. Phosphatidylethanol for Monitoring Alcohol Use in Liver Transplant Candidates: An Observational Study. Journal of Clinical Medicine. 2020; 9(9):3060. https://doi.org/10.3390/jcm9093060
Chicago/Turabian StyleBarrio, Pablo, Antoni Gual, Anna Lligoña, Lidia Teixidor, Wolfgang Weinmann, Michel Yegles, and Friedrich M. Wurst. 2020. "Phosphatidylethanol for Monitoring Alcohol Use in Liver Transplant Candidates: An Observational Study" Journal of Clinical Medicine 9, no. 9: 3060. https://doi.org/10.3390/jcm9093060
APA StyleBarrio, P., Gual, A., Lligoña, A., Teixidor, L., Weinmann, W., Yegles, M., & Wurst, F. M. (2020). Phosphatidylethanol for Monitoring Alcohol Use in Liver Transplant Candidates: An Observational Study. Journal of Clinical Medicine, 9(9), 3060. https://doi.org/10.3390/jcm9093060






