Retinal Pigment Epithelial and Outer Retinal Atrophy in Age-Related Macular Degeneration: Correlation with Macular Function
Abstract
:1. Introduction
2. Methods
2.1. Subjects
2.2. Multimodal Imaging and Visual Function Test Methods
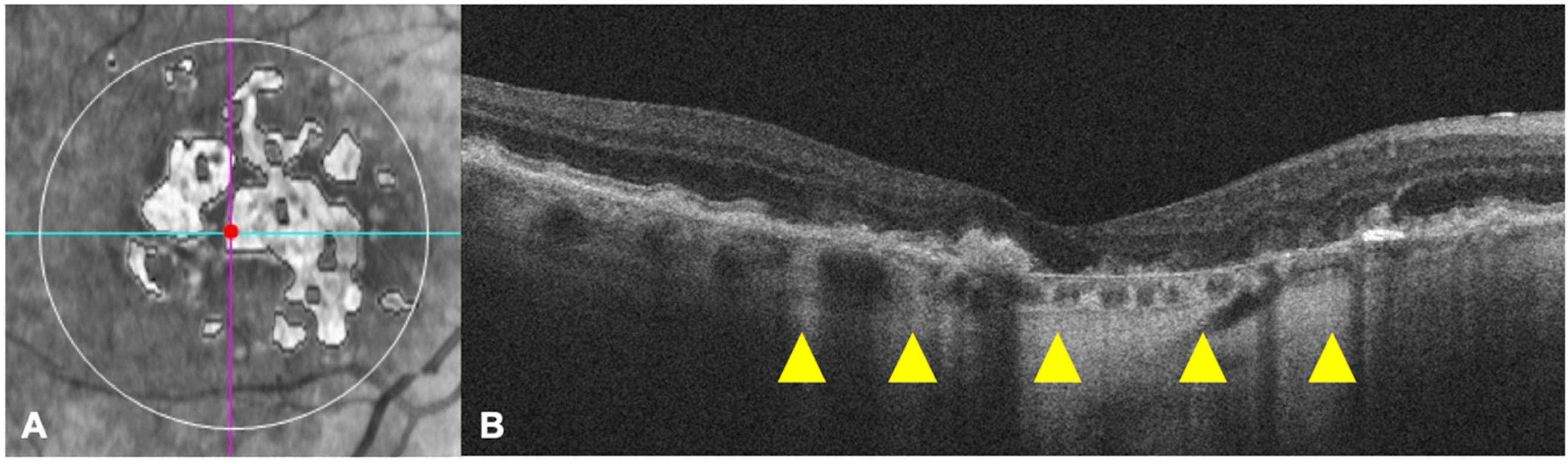
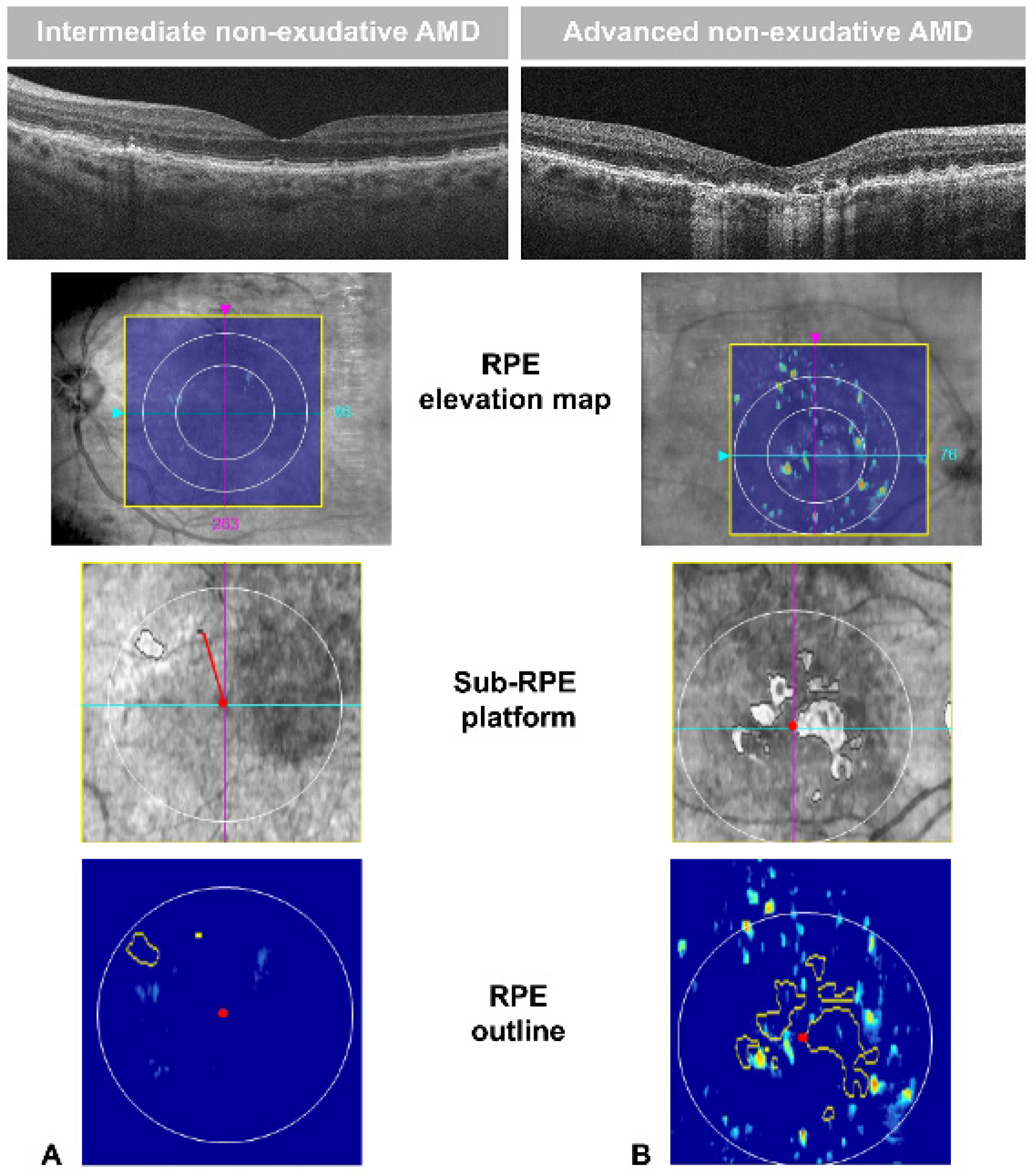
2.3. Definition of neAMD Lesions
2.4. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Klein, R.; Klein, B.E.K.; Lee, K.E.; Cruickshanks, K.J.; Gangnon, R.E. Changes in Visual Acuity in a Population Over a 15-Year Period: The Beaver Dam Eye Study. Am. J. Ophthalmol. 2006, 142, 539–549.e2. [Google Scholar] [CrossRef] [PubMed]
- Klein, R.; Chou, C.F.; Klein, B.E.K.; Zhang, X.; Meuer, S.M.; Saaddine, J.B. Prevalence of Age-Related Macular Degeneration in the US Population. Arch. Ophthalmol. 2011, 129, 75–80. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Age-Related Eye Disease Study Research Group. Risk Factors Associated with Age-Related Macular Degeneration: A Case-Control Study in the Age-Related Eye Disease Study: Age-Related Eye Disease Study Report Number 3. Ophthalmology 2000, 107, 2224–2232. [Google Scholar] [CrossRef]
- Ferris, F.L.; Wilkinson, C.P.; Bird, A.; Chakravarthy, U.; Chew, E.; Csaky, K.; Sadda, S.R. Clinical Classification of Age-Related Macular Degeneration. Ophthalmology 2013, 120, 844–851. [Google Scholar] [CrossRef] [PubMed]
- Sadda, S.R.; Guymer, R.; Holz, F.G.; Schmitz-Valckenberg, S.; Curcio, C.A.; Bird, A.C.; Blodi, B.A.; Bottoni, F.; Chakravarthy, U.; Chew, E.Y.; et al. Consensus Definition for Atrophy Associated with Age-Related Macular Degeneration on OCT: Classification of Atrophy Report 3. Ophthalmology 2018, 125, 537–548. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, Z.; Luu, C.D.; Ayton, L.N.; Goh, J.K.; Lucci, L.M.; Hubbard, W.C.; Hageman, J.L.; Hageman, G.S.; Guymer, R.H. Optical Coherence Tomography-Defined Changes Preceding the Development of Drusen-Associated Atrophy in Age-Related Macular Degeneration. Ophthalmology 2014, 121, 2415–2422. [Google Scholar] [CrossRef] [PubMed]
- Holz, F.G.; Sadda, S.V.R.; Staurenghi, G.; Lindner, M.; Bird, A.C.; Blodi, B.A.; Bottoni, F.; Chakravarthy, U.; Chew, E.Y.; Csaky, K.; et al. Imaging Protocols in Clinical Studies in Advanced Age-Related Macular Degeneration: Recommendations from Classification of Atrophy Consensus Meetings. Ophthalmology 2017, 124, 464–478. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zarbin, M.A.; Casaroli-Marano, R.P.; Rosenfeld, P.J. Age-Related Macular Degeneration: Clinical Findings, Histopathology and Imaging Techniques. In Developments in Ophthalmology; S. Karger AG: Berlin, Germany, 2014; Volume 53, pp. 1–32. [Google Scholar] [CrossRef]
- Guymer, R.H.; Rosenfeld, P.J.; Curcio, C.A.; Holz, F.G.; Staurenghi, G.; Freund, K.B.; Schmitz-Valckenberg, S.; Sparrow, J.; Spaide, R.F.; Tufail, A.; et al. Incomplete Retinal Pigment Epithelial and Outer Retinal Atrophy in Age-Related Macular Degeneration: Classification of Atrophy Meeting Report 4. Ophthalmology 2020, 127, 394–409. [Google Scholar] [CrossRef] [PubMed]
- Kraszewska, O.; Davis, Q.; Stintsman, B.; Feig, R.; Levy, R.; Manning, C. Flash Electroretinogram (FERG) in Age-Related Macular Degeneration (AMD). Investig. Ophthalmol. Vis. Sci. 2018, 59, 2416. [Google Scholar]
- Abdel Kader, M. Electrophysiological Study of Age Related Macular Degeneration. New Front. Ophthalmol. 2017, 3, 1–6. [Google Scholar] [CrossRef]
- Gerth, C.; Delahunt, P.B.; Alam, S.; Morse, L.S.; Werner, J.S. Cone-Mediated Multifocal Electroretinogram in Age-Related Macular Degeneration: Progression over a Long-Term Follow-Up. Arch. Ophthalmol. 2006, 124, 345–352. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Capoluongo, E.; Concolino, P.; Piccardi, M.; Marangoni, D.; Mello, E.; Minnella, A.M.; Savastano, C.; Fadda, A.; Zuppi, C.; Bisti, S.; et al. Retinal Function and CFH-ARMS2 Polymorphisms Analysis: A Pilot Study in Italian AMD Patients. Neurobiol. Aging 2012, 33, 1852.e5–1852.e12. [Google Scholar] [CrossRef] [PubMed]
- Falsini, B.; Fadda, A.; Iarossi, G.; Piccardi, M.; Canu, D.; Minnella, A.; Serrao, S.; Scullica, L. Retinal Sensitivity to Flicker Modulation: Reduced by Early Age-Related Maculopathy. Investig. Ophthalmol. Vis. Sci. 2000, 41, 1498–1506. [Google Scholar]
- Falsini, B.; Serrao, S.; Fadda, A.; Iarossi, G.; Porrello, G.; Cocco, F.; Merendino, E. Focal Electroretinograms and Fundus Appearance in Nonexudative Age-Related Macular Degeneration. Graefe’s Arch. Clin. Exp. Ophthalmol. 1999, 237, 193–200. [Google Scholar] [CrossRef] [PubMed]
- De Oliveira Dias, J.R.; Zhang, Q.; Garcia, J.M.B.; Zheng, F.; Motulsky, E.H.; Roisman, L.; Miller, A.; Chen, C.-L.; Kubach, S.; de Sisternes, L.; et al. Natural History of Subclinical Neovascularization in Nonexudative Age-Related Macular Degeneration Using Swept-Source OCT Angiography. Ophthalmology 2018, 125, 255–266. [Google Scholar] [CrossRef] [PubMed]
- Galli-Resta, L.; Piccardi, M.; Ziccardi, L.; Fadda, A.; Minnella, A.; Marangoni, D.; Placidi, G.; Resta, G.; Falsini, B. Early Detection of Central Visual Function Decline in Cone-Rod Dystrophy by the Use of Macular Focal Cone Electroretinogram. Investig. Ophthalmol. Vis. Sci. 2013, 54, 6560–6569. [Google Scholar] [CrossRef] [PubMed]
- Querques, G.; Querques, L.; Martinelli, D.; Massamba, N.; Coscas, G.; Soubrane, G.; Souied, E.H. Pathologic Insights from Integrated Imaging of Reticular Pseudodrusen in Age-Related Macular Degeneration. Retina 2011, 31, 518–526. [Google Scholar] [CrossRef] [PubMed]
- Kiernan, D.F.; Zelkha, R.; Hariprasad, S.M.; Lim, J.I.; Blair, M.P.; Mieler, W.F. En Face Spectral-Domain Optical Coherence Tomography Outer Retinal Analysis and Relation to Visual Acuity. Retina 2012, 32, 1077–1086. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pappuru, R.R.; Ouyang, Y.; Nittala, M.G.; Hemmati, H.D.; Keane, P.A.; Walsh, A.C.; Sadda, S.R. Relationship between Outer Retinal Thickness Substructures and Visual Acuity in Eyes with Dry Age-Related Macular Degeneration. Investig. Ophthalmol. Vis. Sci. 2011, 52, 6743–6748. [Google Scholar] [CrossRef] [PubMed]
- Lujan, B.J.; Rosenfeld, P.J.; Gregori, G.; Wang, F.; Knighton, R.W.; Feuer, W.J.; Puliafito, C.A. Spectral Domain Optical Coherence Tomography Imaging of Geographic Atrophy. Ophthalmic Surg. Lasers Imaging 2009, 40, 96–101. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Age (Years) | Sex | Disease Stage | fERG Amplitude (µV) | BCVA (LogMAR) | RPE-Elevation 3 mm Circle Area (mm2) | RPE-Elevation 5 mm Circle Area (mm2) | SRI Area (mm2) | SRI Fovea Distance (mm) | |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 83 | M | E | 1.12 | 0 | 0 | 0 | 0 | XXX |
| 2 | 54 | F | I | 1.94 | 0 | 0 | 0 | 0 | XXX |
| 3 | 73 | M | A | 0.82 | 0 | 1.4 | 2.8 | 6.9 | 0.1 |
| 4 | 60 | F | E | 1.96 | 0.04 | 0 | 0 | 0 | XXX |
| 5 | 64 | F | E | 1.49 | 0 | 0 | 0 | 0 | XXX |
| 6 | 77 | F | I | 0.89 | 0.1 | 0.5 | 0.5 | 0 | XXX |
| 7 | 63 | F | E | 1.54 | 0 | 0 | 0 | 0 | XXX |
| 8 | 70 | M | I | 0.82 | 0.2 | 0.1 | 0.3 | 0.1 | 0.9 |
| 9 | 59 | M | A | 1.66 | 0 | 1.2 | 2.8 | 5.4 | 0.5 |
| 10 | 63 | F | I | 1.37 | 0 | 0 | 0 | 0 | XXX |
| 11 | 70 | F | A | 1.33 | 0.5 | 0.7 | 1.8 | 2.3 | 0 |
| 12 | 63 | M | A | 0.14 | 1 | 0.2 | 1.2 | 7.8 | 0 |
| 13 | 74 | F | A | 1.75 | 0.3 | 2.1 | 3.2 | 4.3 | 0 |
| 14 | 79 | M | A | 0.82 | 0.04 | 2.2 | 4.1 | 3.5 | 0 |
| 15 | 54 | F | E | 1.15 | 0.1 | 0 | 0 | 0 | XXX |
| 16 | 55 | M | E | 1.43 | 0 | 0 | 0 | 0 | XXX |
| 17 | 68 | F | I | 2.11 | 0 | 0.3 | 0.3 | 0 | XXX |
| 18 | 72 | M | I | 1.80 | 0.7 | 0 | 0 | 0.1 | 0.1 |
| 19 | 69 | M | I | 0.78 | 0 | 0 | 0.1 | 0 | XXX |
| 20 | 81 | F | A | 1.15 | 0.14 | 0.2 | 0.2 | 1.7 | 0 |
| 21 | 74 | F | A | 0.55 | 0.3 | 0.2 | 0.3 | 13 | 0 |
| 22 | 56 | M | I | 0.46 | 0.3 | 0 | 0 | 3.3 | 0 |
| 23 | 64 | F | I | 1.26 | 0 | 0 | 0 | 0 | XXX |
| 24 | 87 | M | A | 0.74 | 0.14 | 6.3 | 10.9 | 0 | XXX |
| 25 | 59 | F | E | 1.07 | 0 | 0 | 0 | 0 | XXX |
| 26 | 64 | F | I | 0.44 | 0 | 0 | 0 | 0 | XXX |
| 27 | 78 | F | I | 1.04 | 0.04 | 0 | 0 | 0 | XXX |
| 28 | 80 | F | A | 0.18 | 0.7 | 0.1 | 0.7 | 6.3 | 0 |
| 29 | 75 | M | I | 0.25 | 1.1 | 0 | 0.4 | 1.4 | 1.5 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Savastano, M.C.; Falsini, B.; Cozzupoli, G.M.; Savastano, A.; Gambini, G.; De Vico, U.; Minnella, A.M.; Placidi, G.; Piccardi, M.; Rizzo, S. Retinal Pigment Epithelial and Outer Retinal Atrophy in Age-Related Macular Degeneration: Correlation with Macular Function. J. Clin. Med. 2020, 9, 2973. https://doi.org/10.3390/jcm9092973
Savastano MC, Falsini B, Cozzupoli GM, Savastano A, Gambini G, De Vico U, Minnella AM, Placidi G, Piccardi M, Rizzo S. Retinal Pigment Epithelial and Outer Retinal Atrophy in Age-Related Macular Degeneration: Correlation with Macular Function. Journal of Clinical Medicine. 2020; 9(9):2973. https://doi.org/10.3390/jcm9092973
Chicago/Turabian StyleSavastano, Maria C., Benedetto Falsini, Grazia M. Cozzupoli, Alfonso Savastano, Gloria Gambini, Umberto De Vico, Angelo M. Minnella, Giorgio Placidi, Marco Piccardi, and Stanislao Rizzo. 2020. "Retinal Pigment Epithelial and Outer Retinal Atrophy in Age-Related Macular Degeneration: Correlation with Macular Function" Journal of Clinical Medicine 9, no. 9: 2973. https://doi.org/10.3390/jcm9092973
APA StyleSavastano, M. C., Falsini, B., Cozzupoli, G. M., Savastano, A., Gambini, G., De Vico, U., Minnella, A. M., Placidi, G., Piccardi, M., & Rizzo, S. (2020). Retinal Pigment Epithelial and Outer Retinal Atrophy in Age-Related Macular Degeneration: Correlation with Macular Function. Journal of Clinical Medicine, 9(9), 2973. https://doi.org/10.3390/jcm9092973






