Minimally Invasive Intraoral Approach to Submandibular Lodge
Abstract
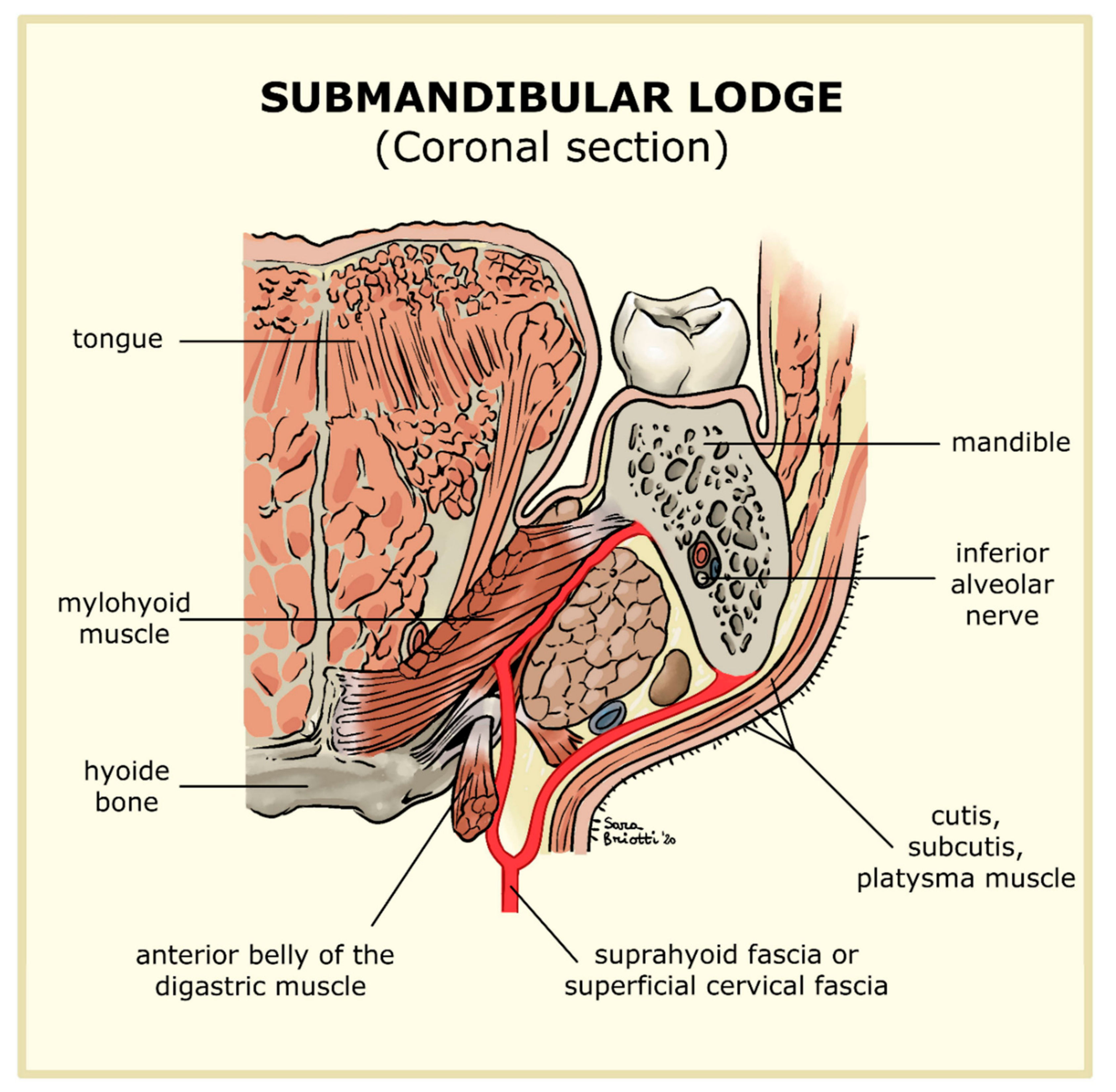
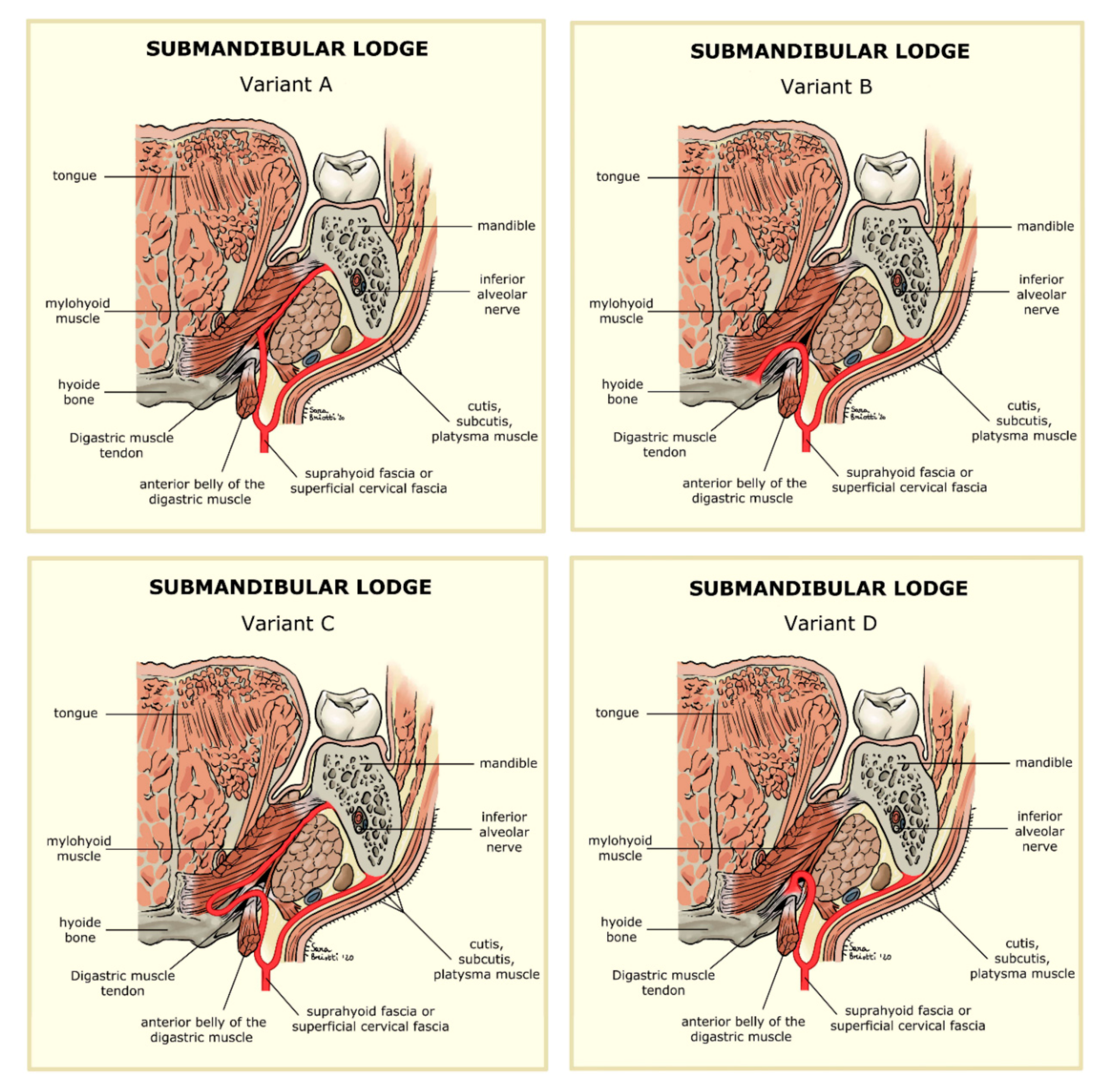
1. Introduction
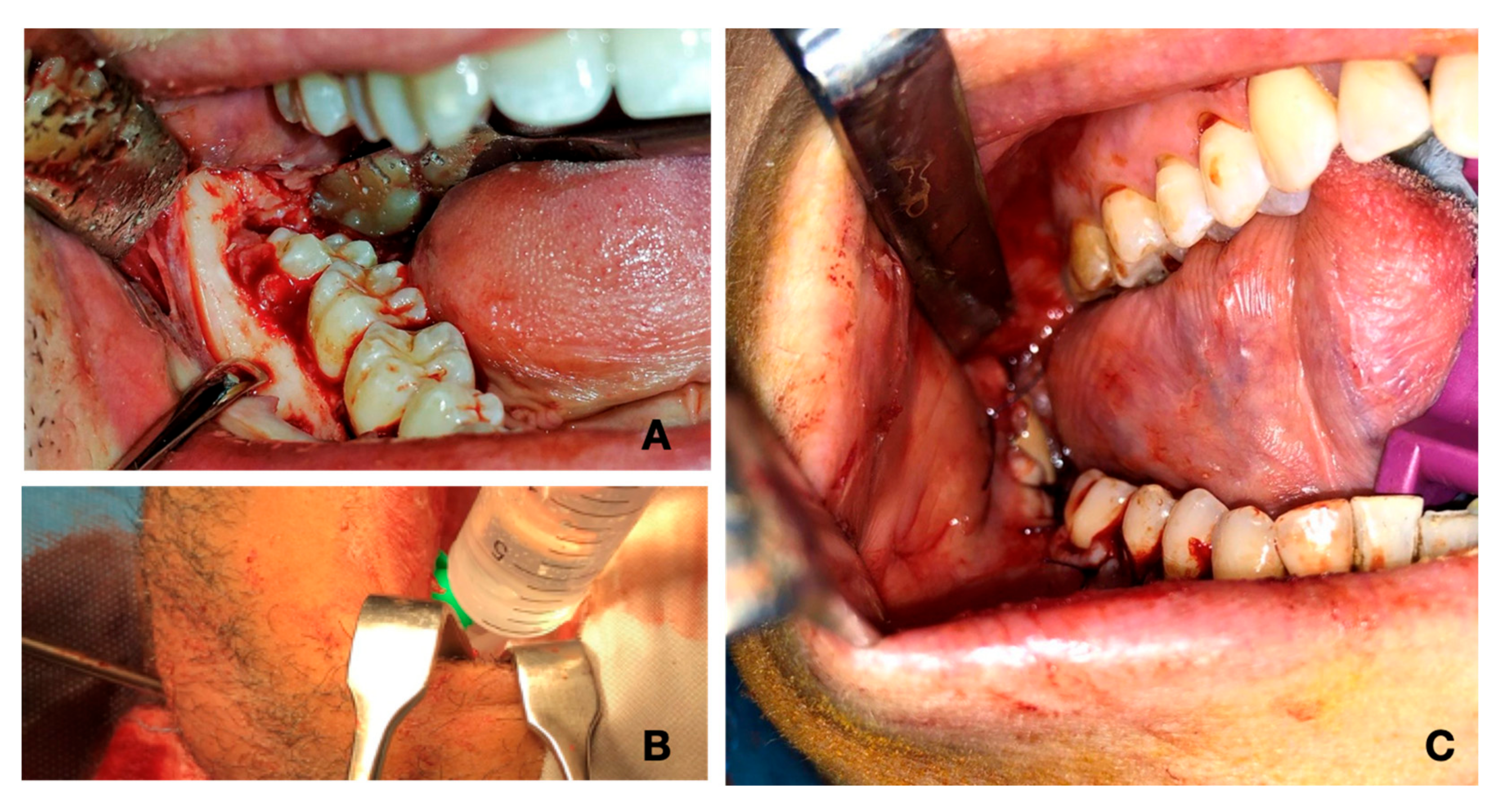
2. Experimental Section
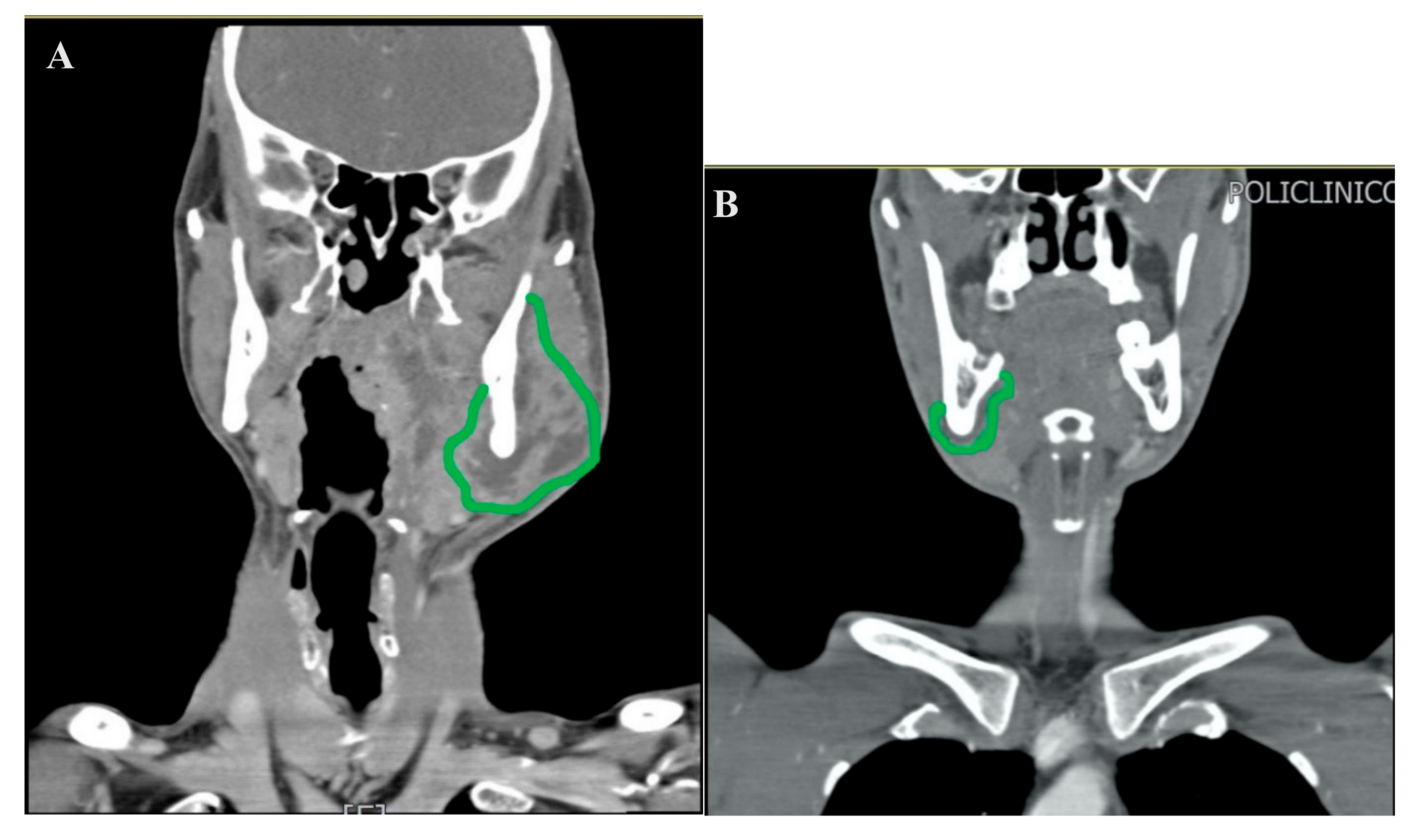
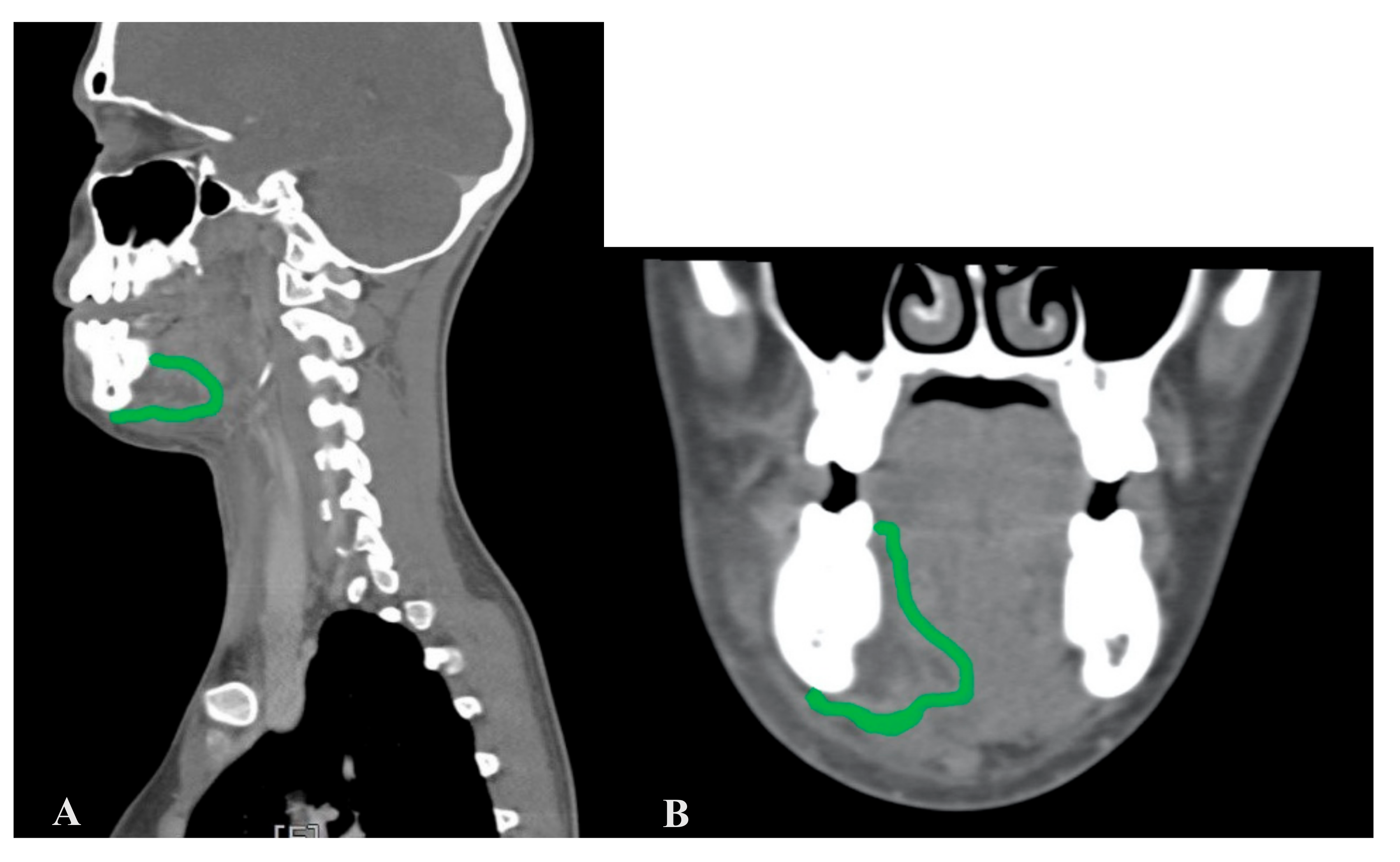
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Moghimi, M.; Baart, J.A.; Karagozoglu, K.H.; Forouzanfar, T. Spread of odontogenic infections: A retrospective analysis and review of the literature. Quintessence Int. 2013, 44, 351–361. [Google Scholar] [PubMed]
- Bali, R.K.; Sharma, P.; Gaba, S.; Kaur, A.; Ghanghas, P. A review of complications of odontogenic infections. Natl. J. Maxillofac. Surg. 2015, 6, 136–143. [Google Scholar] [CrossRef] [PubMed]
- Bakathir, A.A.; Moos, K.F.; Ayoub, A.F.; Bagg, J. Factors Contributing to the Spread of Odontogenic infections: A prospective pilot study. Sultan Qaboos Univ. Med. J. 2009, 9, 296–304. [Google Scholar] [PubMed]
- Green, A.W.; Flower, E.A.; New, N.E. Mortality associated with odontogenic infection! Br. Dent. J. 2001, 190, 529–530. [Google Scholar] [CrossRef] [PubMed]
- D’Erme, G.; Galli, M.; Candelori, F.; Federici, F.R.; Greco, A.; Ralli, M. A rare case of odontogenic bilateral submandibular abscess. Otorinolaringologia 2020, 70. [Google Scholar]
- Pesis, M.; Bar-Droma, E.; Ilgiyaev, A.; Givol, N. Deep Neck Infections Are Life Threatening Infections of Dental Origin: A Presentation and Management of Selected Cases. ISR. Med. Assoc. J. IMAJ 2019, 12, 806–811. [Google Scholar] [PubMed]
- Fusconi, M.; Greco, A.; Galli, M.; Polimeni, A.; Yusef, M.; Di Cianni, S.; De Soccio, G.; FR, F.S.; Lombardi, R.; de Vincentiis, M. Odontogenic phlegmons and abscesses in relation to the financial situation of Italian families. Minerva Stomatol. 2019, 68, 236–241. [Google Scholar] [CrossRef] [PubMed]
- D’Erme, G.; Galli, M.; Federici, F.R.; Colizza, A.; Ralli, M.; de Vincentiis, M. Report of a rare case of Lemierre’s syndrome associated with a multidrug resistant dental abscess. Otorinolaringologia 2019, 69. [Google Scholar]
- Heim, N.; Faron, A.; Wiedemeyer, V.; Reich, R.; Martini, M. Microbiology and antibiotic sensitivity of head and neck space infections of odontogenic origin. Differences in inpatient and outpatient management. J. Cranio-Maxillofac. Surg. 2017, 45, 1731–1735. [Google Scholar] [CrossRef] [PubMed]
- Kitamura, S. Anatomy of the fasciae and fascial spaces of the maxillofacial and the anterior neck regions. Anat. Sci. Int. 2018, 93, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Kohan, E.J.; Wirth, G.A. Anatomy of the neck. Okajimas Folia Anat. Jpn. 2014, 41, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Carlson, G.W. Surgical anatomy of the neck. Surg. Clin. North Am. 1993, 73, 837–852. [Google Scholar] [CrossRef]
- Testut, L.; Jacob, O. Anatomia Umana; UTET: Torino, Italy, 1972; Volume 5. [Google Scholar]
- Calearo, C.V.; Teatini, G. Functional neck dissection. Anatomical grounds, surgical technique, clinical observations. Ann. Otol. Rhinol. Laryngol. 1983, 92, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Osborn, T.M.; Assael, L.A.; Bell, R.B. Deep space neck infection: Principles of surgical management. Oral Maxillofac. Surg. Clin. North Am. 2008, 20, 353–365. [Google Scholar] [CrossRef] [PubMed]

© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Galli, M.; Fusconi, M.; Federici, F.R.; Candelori, F.; De Vincentiis, M.; Polimeni, A.; Testarelli, L.; Cassese, B.; Miccoli, G.; Greco, A. Minimally Invasive Intraoral Approach to Submandibular Lodge. J. Clin. Med. 2020, 9, 2971. https://doi.org/10.3390/jcm9092971
Galli M, Fusconi M, Federici FR, Candelori F, De Vincentiis M, Polimeni A, Testarelli L, Cassese B, Miccoli G, Greco A. Minimally Invasive Intraoral Approach to Submandibular Lodge. Journal of Clinical Medicine. 2020; 9(9):2971. https://doi.org/10.3390/jcm9092971
Chicago/Turabian StyleGalli, Massimo, Massimo Fusconi, Francesca Romana Federici, Francesca Candelori, Marco De Vincentiis, Antonella Polimeni, Luca Testarelli, Benedetta Cassese, Gabriele Miccoli, and Antonio Greco. 2020. "Minimally Invasive Intraoral Approach to Submandibular Lodge" Journal of Clinical Medicine 9, no. 9: 2971. https://doi.org/10.3390/jcm9092971
APA StyleGalli, M., Fusconi, M., Federici, F. R., Candelori, F., De Vincentiis, M., Polimeni, A., Testarelli, L., Cassese, B., Miccoli, G., & Greco, A. (2020). Minimally Invasive Intraoral Approach to Submandibular Lodge. Journal of Clinical Medicine, 9(9), 2971. https://doi.org/10.3390/jcm9092971









