Care Dependency in Non-Hospitalized Patients with COVID-19
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Participants
2.2. Measures
2.3. Statistics
3. Results
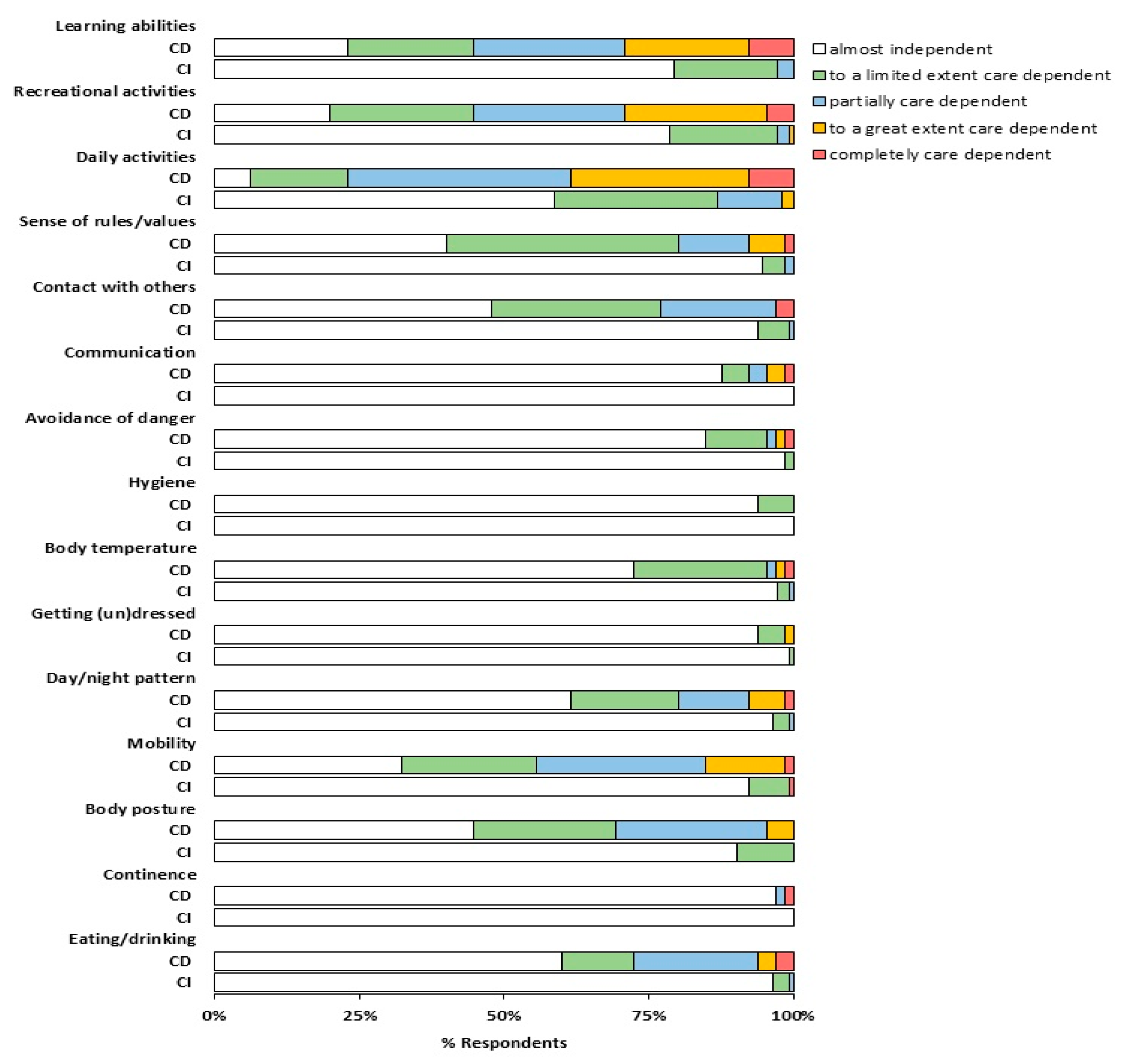
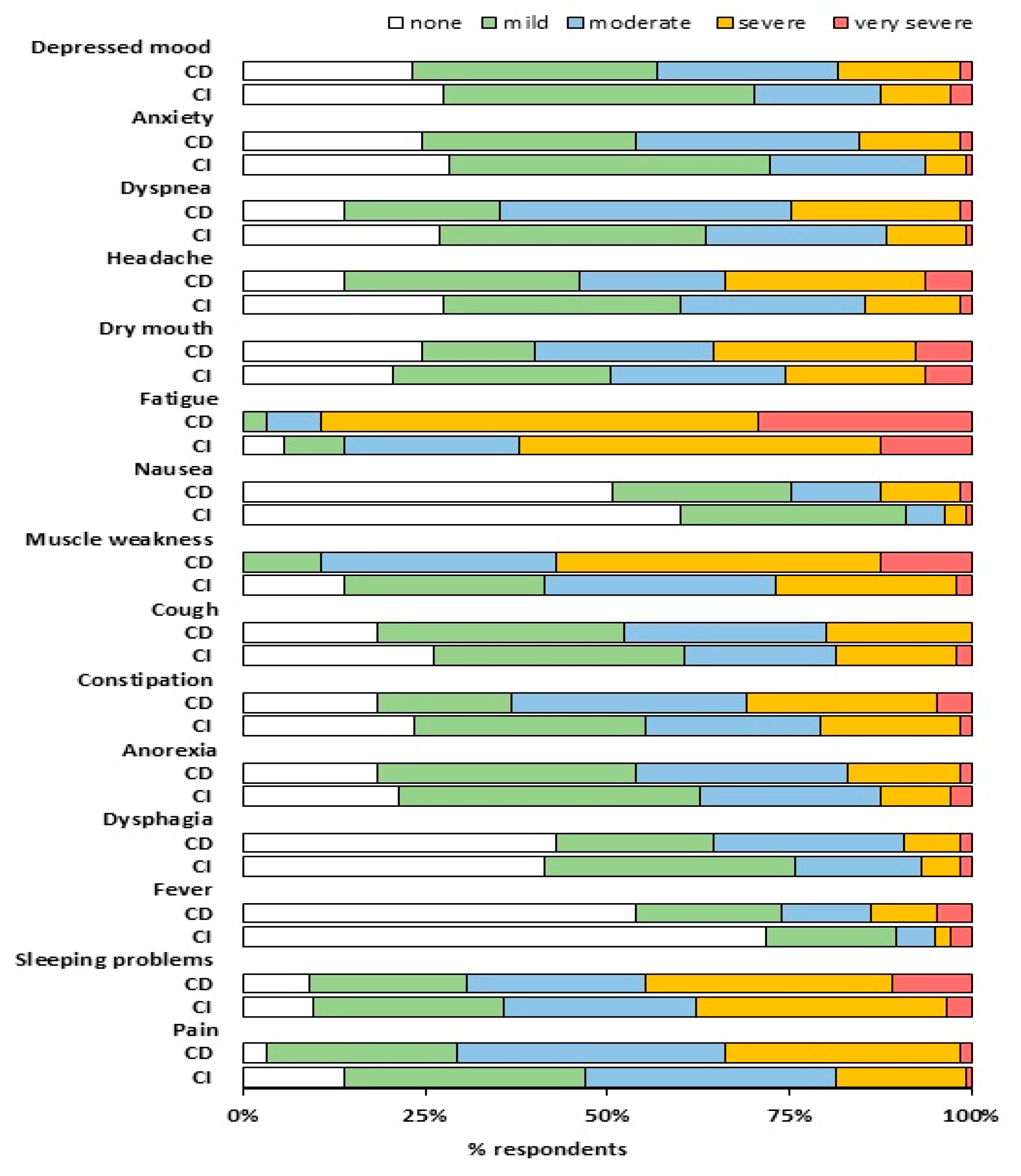
Level of Care Dependency
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lechien, J.R.; Chiesa-Estomba, C.M.; Place, S.; Van Laethem, Y.; Cabaraux, P.; Mat, Q.; Huet, K.; Plzak, J.; Horoi, M.; Hans, S.; et al. Clinical and epidemiological characteristics of 1420 European patients with mild-to-moderate coronavirus disease 2019. J. Intern. Med. 2020, 228, 335–344. [Google Scholar] [CrossRef]
- Lapostolle, F.; Schneider, E.; Vianu, I.; Dollet, G.; Roche, B.; Berdah, J.; Michel, J.; Goix, L.; Chanzy, E.; Petrovic, T.; et al. Clinical features of 1487 COVID-19 patients with outpatient management in the Greater Paris: The COVID-call study. Intern. Emerg. Med. 2020, 15, 813–817. [Google Scholar] [CrossRef] [PubMed]
- Goërtz, Y.M.J.; Van Herck, M.; Delbressine, J.M.; Vaes, A.W.; Meys, R.; Machado, F.V.C.; Houben-Wilke, S.; Burtin, C.; Posthuma, R.; Franssen, F.M.E.; et al. Persistent symptoms 3 months after a SARS-CoV-2 infection: The post-COVID-19 syndrome? ERJ Open Res. 2020, in press. [Google Scholar]
- Carfì, A.; Bernabei, R.; Landi, F. Persistent Symptoms in Patients After Acute COVID-19. JAMA 2020, 324, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Belli, S.; Balbi, B.; Prince, I.; Cattaneo, D.; Masocco, F.; Zaccaria, S.; Bertalli, L.; Cattini, F.; Lomazzo, A.; Dal Negro, F.; et al. Low physical functioning and impaired performance of activities of daily life in COVID-19 patients who survived the hospitalisation. Eur. Respir. J. 2020. [Google Scholar] [CrossRef]
- Public Facebook Group: Corona Ervaringen en Langdurige Klachten! Available online: https://www.facebook.com/groups/236723204035929.9 (accessed on 4 June 2020).
- Public Facebook Group: Corona Patiënten Met Langdurige Klachten (Vlaanderen). Available online: https://www.facebook.com/groups/241043323639334 (accessed on 4 June 2020).
- Bruera, E.; Kuehn, N.; Miller, M.J.; Selmser, P.; Macmillan, K. The Edmonton Symptom Assessment System (ESAS): A simple method for the assessment of palliative care patients. J. Palliat. Care 1991, 7, 6–9. [Google Scholar] [CrossRef]
- Dijkstra, A.; Tiesinga, L.J.; Goossen, W.T.; Dassen, T.W. Further psychometric testing of the Dutch Care Dependency Scale on two different patient groups. Int. J. Nurs. Pract. 2002, 8, 305–314. [Google Scholar] [CrossRef]
- Dijkstra, A.; Tiesinga, L.J.; Plantinga, L.; Veltman, G.; Dassen, T.W. Diagnostic accuracy of the care dependency scale. J. Adv. Nurs. 2005, 50, 410–416. [Google Scholar] [CrossRef]
- Sheehy, L.M. Considerations for Postacute Rehabilitation for Survivors of COVID-19. JMIR Public Health Surveill. 2020, 6, e19462. [Google Scholar] [CrossRef]
- Caljouw, M.A.; Cools, H.J.; Gussekloo, J. Natural course of care dependency in residents of long-term care facilities: Prospective follow-up study. BMC Geriatr. 2014, 14, 67. [Google Scholar] [CrossRef]
- Millán-Calenti, J.C.; Tubío, J.; Pita-Fernández, S.; González-Abraldes, I.; Lorenzo, T.; Fernández-Arruty, T.; Maseda, A. Prevalence of functional disability in activities of daily living (ADL), instrumental activities of daily living (IADL) and associated factors, as predictors of morbidity and mortality. Arch. Gerontol. Geriatr. 2010, 50, 306–310. [Google Scholar] [CrossRef]
- Fitzsimons, D.; Mullan, D.; Wilson, J.S.; Conway, B.; Corcoran, B.; Dempster, M.; Gamble, J.; Stewart, C.; Rafferty, S.; McMahon, M.; et al. The challenge of patients’ unmet palliative care needs in the final stages of chronic illness. Palliat. Med. 2007, 21, 313–322. [Google Scholar] [CrossRef]
- Janssen, D.J.; Franssen, F.M.; Wouters, E.F.; Schols, J.M.; Spruit, M.A. Impaired health status and care dependency in patients with advanced COPD or chronic heart failure. Qual. Life Res. 2011, 20, 1679–1688. [Google Scholar] [CrossRef]
- Bleijenberg, N.; Zuithoff, N.P.A.; Smith, A.K.; de Wit, N.J.; Schuurmans, M.J. Disability in the Individual ADL, IADL, and Mobility among Older Adults: A Prospective Cohort Study. J. Nutr. Health Aging 2017, 21, 897–903. [Google Scholar] [CrossRef]
- Chen, Z.; Fan, V.S.; Belza, B.; Pike, K.; Nguyen, H.Q. Association between Social Support and Self-Care Behaviors in Adults with Chronic Obstructive Pulmonary Disease. Ann. Am. Thorac. Soc. 2017, 14, 1419–1427. [Google Scholar] [CrossRef]
- Prazeres, F.; Santiago, L. Relationship between health-related quality of life, perceived family support and unmet health needs in adult patients with multimorbidity attending primary care in Portugal: A multicentre cross-sectional study. Health Qual. Life Outcomes 2016, 14, 156. [Google Scholar] [CrossRef]
- Nakken, N.; Janssen, D.J.; van den Bogaart, E.H.; Wouters, E.F.; Franssen, F.M.; Vercoulen, J.H.; Spruit, M.A. Informal caregivers of patients with COPD: Home Sweet Home? Eur. Respir. Rev. 2015, 24, 498–504. [Google Scholar] [CrossRef]
- Miravitlles, M.; Peña-Longobardo, L.M.; Oliva-Moreno, J.; Hidalgo-Vega, Á. Caregivers’ burden in patients with COPD. Int. J. Chron. Obstruct. Pulm. Dis. 2015, 10, 347–356. [Google Scholar] [CrossRef]
- Chan, E.Y.Y.; Gobat, N.; Kim, J.H.; Newnham, E.A.; Huang, Z.; Hung, H.; Dubois, C.; Hung, K.K.C.; Wong, E.L.Y.; Wong, S.Y.S. Informal home care providers: The forgotten health-care workers during the COVID-19 pandemic. Lancet 2020, 395, P1957–P1959. [Google Scholar] [CrossRef]
- Janssen, D.J.; Schols, J.M.; Wouters, E.F.; Spruit, M.A. One-year stability of care dependency in patients with advanced chronic organ failure. J. Am. Med. Direct. Assoc. 2014, 15, 127–132. [Google Scholar] [CrossRef]
- Nakken, N.; Spruit, M.A.; van den Bogaart, E.H.; van Vliet, M.; de Vries, G.J.; Custers, F.L.; Vercoulen, J.H.; Asijee, G.M.; Muris, J.W.; Vanfleteren, L.E.; et al. Health Status and Morbidities in Resident Relatives of Patients With COPD. J. Am. Med. Direct. Assoc. 2016, 17, 276. [Google Scholar] [CrossRef]
- Poot, A.J.; Caljouw, M.A.; Waard, C.S.; Wind, A.W.; Gussekloo, J. Satisfaction in Older Persons and General Practitioners during the Implementation of Integrated Care. PLoS ONE 2016, 11, e0164536. [Google Scholar] [CrossRef]
- Hajek, A.; König, H.H. Longitudinal Predictors of Functional Impairment in Older Adults in Europe—Evidence from the Survey of Health, Ageing and Retirement in Europe. PLoS ONE 2016, 11, e0146967. [Google Scholar] [CrossRef]
- Dijkstra, A.; Hakverdioğlu, G.; Muszalik, M.; Andela, R.; Korhan, E.A.; Kędziora-Kornatowska, K. Health related quality of life and care dependency among elderly hospital patients: An international comparison. Tohoku J. Exp. Med. 2015, 235, 193–200. [Google Scholar] [CrossRef]
- Koller, D.; Schön, G.; Schäfer, I.; Glaeske, G.; van den Bussche, H.; Hansen, H. Multimorbidity and long-term care dependency—A five-year follow-up. BMC Geriatr. 2014, 14, 70. [Google Scholar] [CrossRef]
- Greenhalgh, T.; Knight, M.; A’Court, C.; Buxton, M.; Husain, L. Management of post-acute covid-19 in primary care. BMJ 2020, 370, m3026. [Google Scholar] [CrossRef]
- Vaes, A.W.; Wouters, E.F.; Franssen, F.M.; Uszko-Lencer, N.H.; Stakenborg, K.H.; Westra, M.; Meijer, K.; Schols, A.M.; Janssen, P.P.; Spruit, M.A. Task-Related Oxygen Uptake During Domestic Activities of Daily Life in Patients With COPD and Healthy Elderly Subjects. Chest 2011, 140, 970–979. [Google Scholar] [CrossRef]
- Dijkstra, A.; Coleman, M.; Tomas, C.; Välimäki, M.; Dassen, T. Cross-cultural psychometric testing of the Care Dependency Scale with data. J. Adv. Nurs. 2003, 43, 181–187. [Google Scholar] [CrossRef]
| Variables | All Patients (n = 1837) | Belgium Facebook Group (n = 210) | |||
|---|---|---|---|---|---|
| Gender—female, n (%) | 1581 (86.1) | 184 (87.6) | |||
| Age, years a | 47.0 (38.0–54.0) | 44.0 (37.0–52.3) | |||
| BMI, kg/m2 a | 25.1 (22.5–28.7) | 25.1 (22.2–28.6) | |||
| Marital status—married/living with partner, n (%) | 1308 (71.2) | 147 (70.0) | |||
| Children living at home, yes, n (%) | 949 (51.7) | 118 (56.2) | |||
| 1 | 310 (32.7) | 30 (25.4) | |||
| 2 | 480 (50.6) | 69 (58.5) | |||
| 3 | 131 (13.8) | 14 (11.9) | |||
| ≥4 | 28 (2.9) | 5 (4.2) | |||
| Comorbidities before COVID-19, n (%) | None | 1132 (61.6) | 129 (61.4) | ||
| 1 | 465 (25.3) | 49 (23.3) | |||
| ≥2 | 240 (13.1) | 32 (15.2) | |||
| Health status, n (%) | Before infection | After infection | Before infection | After infection | |
| Good | 1576 (85.8) | 117 (6.4) * | 175 (83.3) | 15 (7.1) * | |
| Moderate | 249 (13.6) | 1170 (63.7) * | 35 (16.7) | 137 (65.2) * | |
| Poor | 12 (0.7) | 550 (29.9) * | 0.0 | 58 (27.6) * | |
| CDS Score ≤ 68 Points (n = 65) | CDS Score > 69 Points (n = 145) | ||||
|---|---|---|---|---|---|
| Gender—female, n (%) | 56 (86.2) | 128 (88.3) | |||
| Age, years a | 41.0 (33.5–51.0) | 45.0 (38.5–53.0) * | |||
| BMI, kg/m2 a | 25.1 (21.9–29.0) | 25.1 (22.5–28.5) | |||
| Marital status—married/living with partner, n (%) | 45 (69.2) | 102 (70.3) | |||
| Children living at home, yes, n (%) | 29 (44.6) | 89 (61.4) * | |||
| 1 | 9 (31.0) | 21 (23.6) | |||
| 2 | 14 (48.3) | 55 (61.8) | |||
| 3 | 3 (10.3) | 11 (12.4) | |||
| ≥4 | 3 (10.3) | 2 (2.2) | |||
| Comorbidities before COVID-19, n (%) | None | 39 (60.0) | 90 (62.1) | ||
| 1 | 13 (20.0) | 36 (24.8) | |||
| ≥2 | 13 (20.0) | 19 (13.1) | |||
| COVID-19 Diagnosis | |||||
| Based on CT/RT-PCR testing, n (%) | 15 (23.1) | 34 (23.4) | |||
| Based on symptoms, n (%) | 32 (49.2) | 73 (50.3) | |||
| Undiagnosed, n (%) | 18 (27.7) | 38 (26.2) | |||
| Health status before, n (%) | Before infection | After infection | Before infection | After infection | |
| Good | 48 (73.8) | 1 (1.5) # | 127 (87.6) * | 14 (9.7) *,# | |
| Moderate | 17 (26.2) | 29 (44.6) # | 18 (12.4) * | 108 (74.5) *,# | |
| Poor | - | 35 (53.8) # | - | 23 (15.9) *,# | |
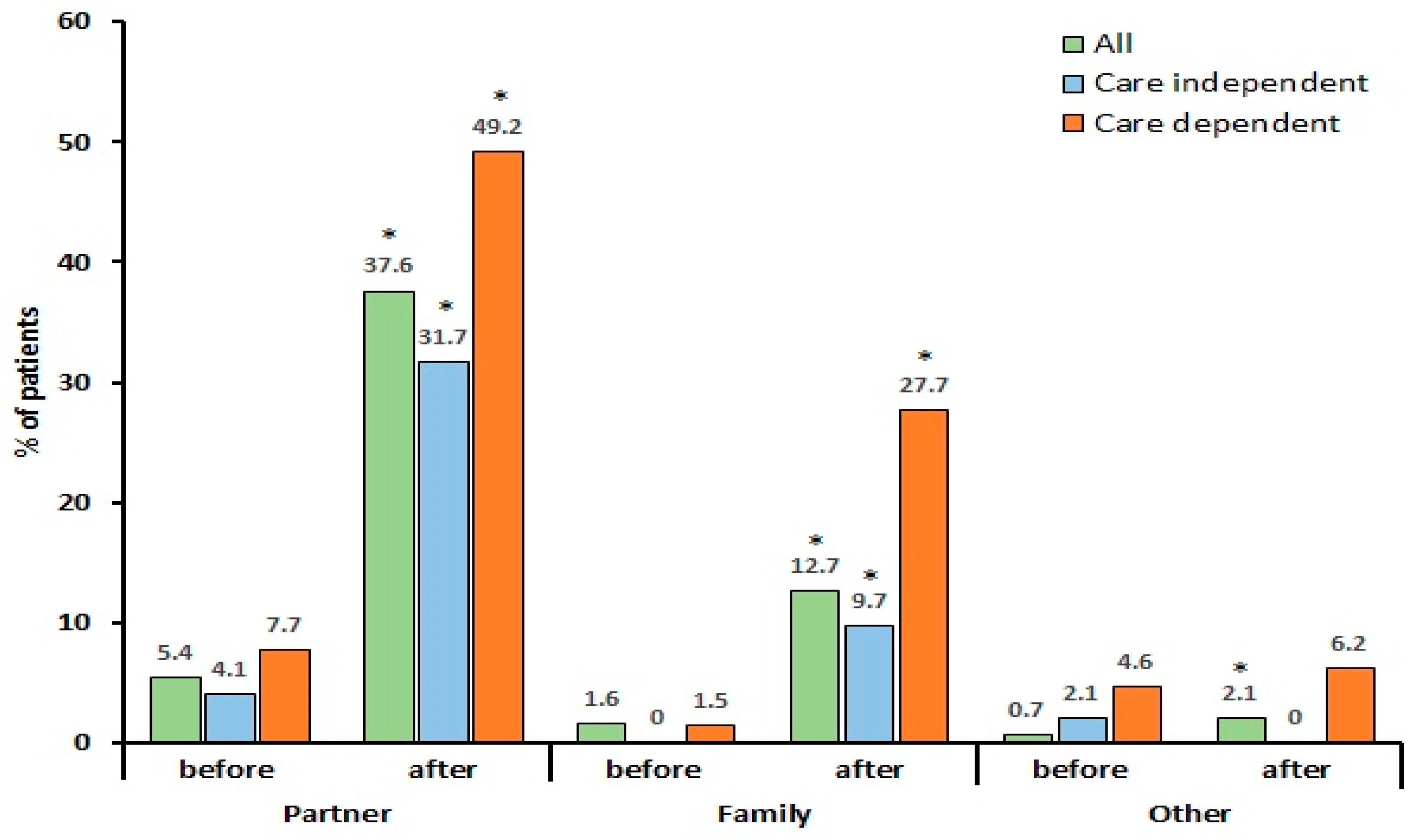
| Need for help with personal care, n (%) | Before infection | After infection | Before infection | After infection | |
| Partner | 5 (7.7) | 32 (49.2) # | 6 (4.1) | 46 (31.7) *,# | |
| Family | 1 (1.5) | 18 (27.7) # | 0.0 | 14 (9.7) *,# | |
| Nurse | 1 (1.5) | 2 (3.1) | 0.0 | 0.0 * | |
| Other | 2 (3.1) | 2 (3.1) | 3 (2.1) | 0.0 * | |
| Perceived support from family, n (%) | |||||
| Very often | 26 (40.0) | 45 (31.0) | |||
| Regularly | 21 (32.3) | 48 (33.1) | |||
| Occasionally | 13 (20.0) | 44 (30.3) | |||
| Rarely or never | 4 (6.2) | 6 (4.1) | |||
| Not applicable | 1 (1.5) | 2 (1.4) | |||
| CDS, sum score a | 64.0 (61.5–67.0) | 74.0 (72.0–75.0) * | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vaes, A.W.; Machado, F.V.C.; Meys, R.; Delbressine, J.M.; Goertz, Y.M.J.; Van Herck, M.; Houben-Wilke, S.; Franssen, F.M.E.; Vijlbrief, H.; Spies, Y.; et al. Care Dependency in Non-Hospitalized Patients with COVID-19. J. Clin. Med. 2020, 9, 2946. https://doi.org/10.3390/jcm9092946
Vaes AW, Machado FVC, Meys R, Delbressine JM, Goertz YMJ, Van Herck M, Houben-Wilke S, Franssen FME, Vijlbrief H, Spies Y, et al. Care Dependency in Non-Hospitalized Patients with COVID-19. Journal of Clinical Medicine. 2020; 9(9):2946. https://doi.org/10.3390/jcm9092946
Chicago/Turabian StyleVaes, Anouk W., Felipe V.C. Machado, Roy Meys, Jeannet M. Delbressine, Yvonne M.J. Goertz, Maarten Van Herck, Sarah Houben-Wilke, Frits M.E. Franssen, Herman Vijlbrief, Yvonne Spies, and et al. 2020. "Care Dependency in Non-Hospitalized Patients with COVID-19" Journal of Clinical Medicine 9, no. 9: 2946. https://doi.org/10.3390/jcm9092946
APA StyleVaes, A. W., Machado, F. V. C., Meys, R., Delbressine, J. M., Goertz, Y. M. J., Van Herck, M., Houben-Wilke, S., Franssen, F. M. E., Vijlbrief, H., Spies, Y., Van ’t Hul, A. J., Burtin, C., Janssen, D. J. A., & Spruit, M. A. (2020). Care Dependency in Non-Hospitalized Patients with COVID-19. Journal of Clinical Medicine, 9(9), 2946. https://doi.org/10.3390/jcm9092946





