Etiology of Ischemic Strokes of Patients with Atrial Fibrillation and Therapy with Anticoagulants
Abstract
1. Introduction
2. Experimental Section
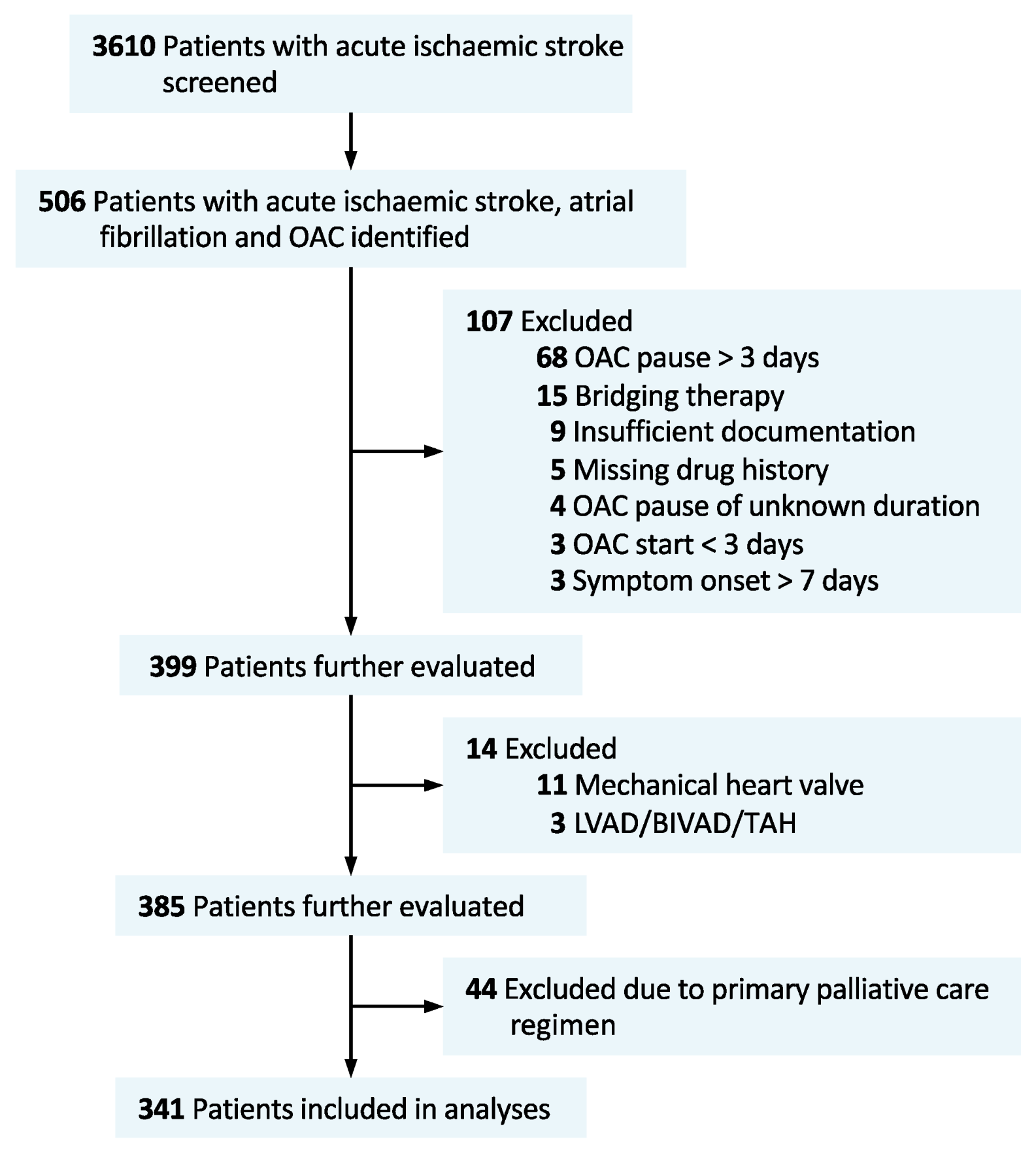
2.1. Patient Cohort Description, and Patient Involvement
2.2. Data Acquisition
2.3. Imaging Analysis
2.4. Etiologic Classification
2.5. Data Analysis
3. Results
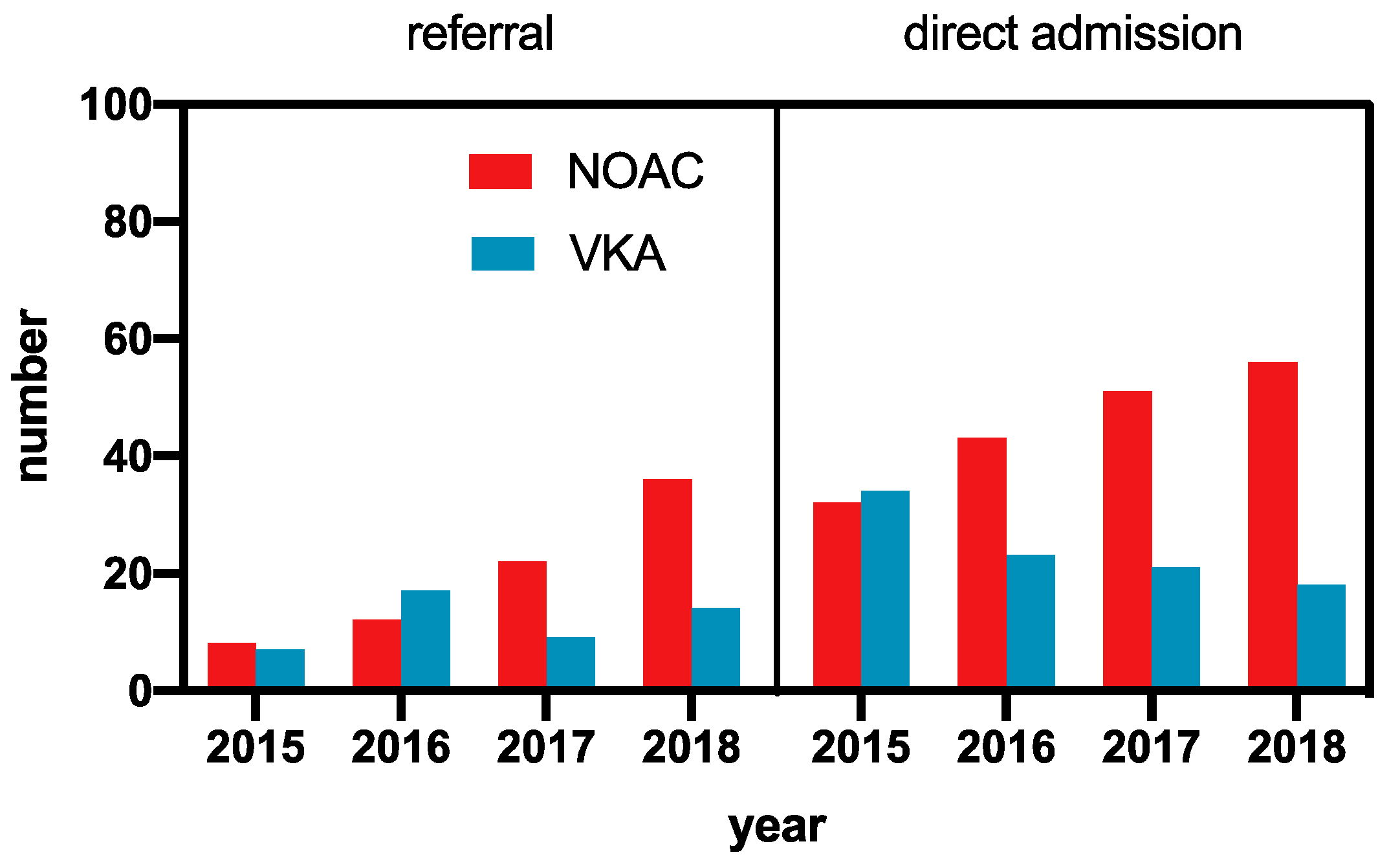
3.1. Time Trends
3.2. Coagulation Status
3.3. Dosage Errors
3.4. Medication Errors
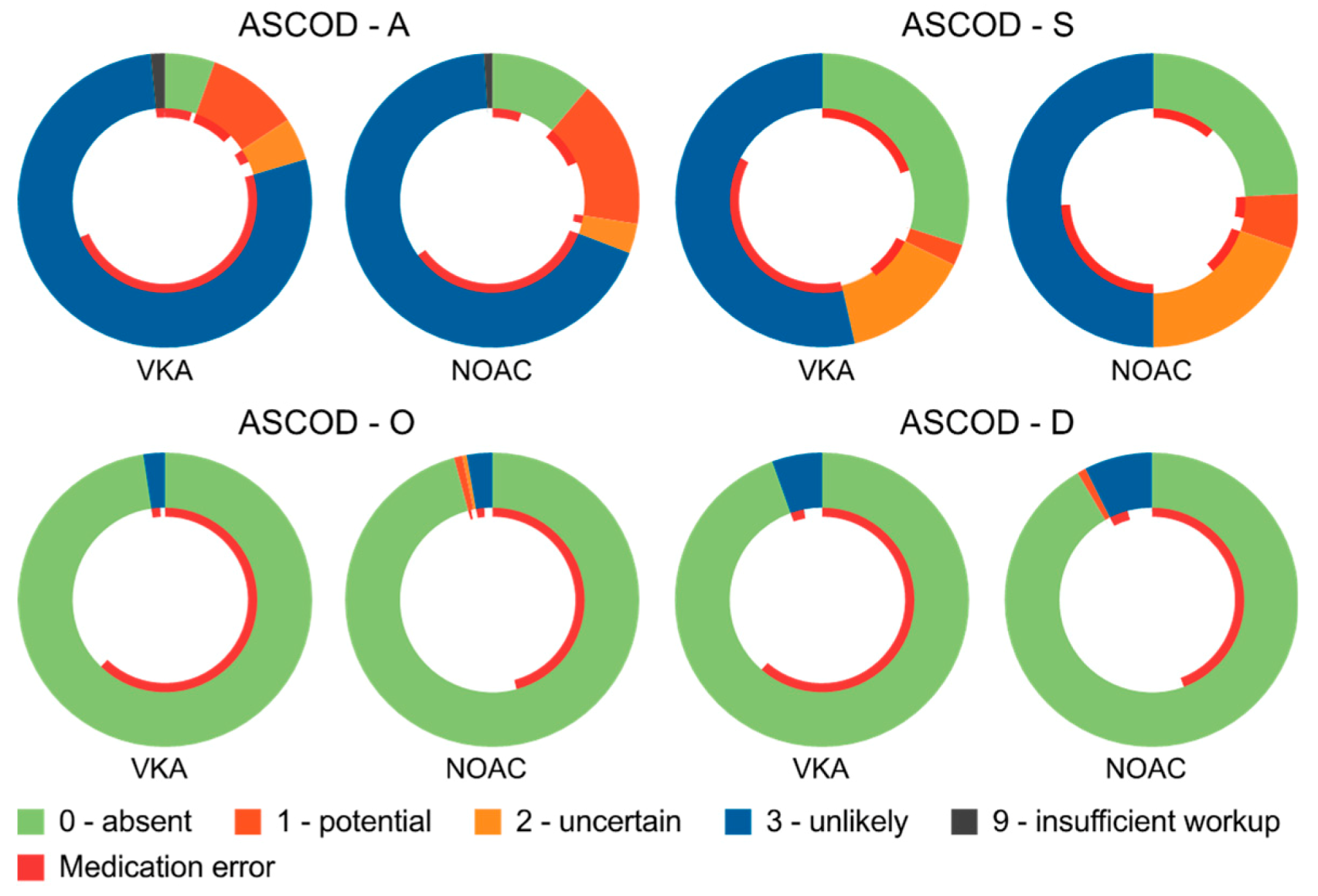
3.5. Etiologic Classification of OAC-Associated Strokes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hart, R.G.; Pearce, L.A.; Aguilar, M.I. Meta-analysis: Antithrombotic therapy to prevent stroke in patients who have nonvalvular atrial fibrillation. Ann. Intern. Med. 2007, 146, 857–867. [Google Scholar] [CrossRef] [PubMed]
- Connolly, S.J.; Eikelboom, J.; Joyner, C.; Diener, H.C.; Hart, R.; Golitsyn, S.; Flaker, G.; Avezum, A.; Hohnloser, S.H.; Diaz, R.; et al. Apixaban in patients with atrial fibrillation. N. Engl. J. Med. 2011, 364, 806–817. [Google Scholar] [CrossRef] [PubMed]
- Ruff, C.T.; Giugliano, R.P.; Braunwald, E.; Hoffman, E.B.; Deenadayalu, N.; Ezekowitz, M.D.; Camm, A.J.; Weitz, J.I.; Lewis, B.S.; Parkhomenko, A.; et al. Comparison of the efficacy and safety of new oral anticoagulants with warfarin in patients with atrial fibrillation: A meta-analysis of randomised trials. Lancet 2014, 383, 955–962. [Google Scholar] [CrossRef]
- Diener, H.C.; Connolly, S.J.; Ezekowitz, M.D.; Wallentin, L.; Reilly, P.A.; Yang, S.; Xavier, D.; Di Pasquale, G.; Yusuf, S.; RE-LY Study Group. Dabigatran compared with warfarin in patients with atrial fibrillation and previous transient ischaemic attack or stroke: A subgroup analysis of the RE-LY trial. Lancet Neurol. 2010, 9, 1157–1163. [Google Scholar] [CrossRef]
- Hankey, G.J.; Patel, M.R.; Stevens, S.R.; Becker, R.C.; Breithardt, G.; Carolei, A.; Diener, H.C.; Donnan, G.A.; Halperin, J.L.; Mahaffey, K.W.; et al. Rivaroxaban compared with warfarin in patients with atrial fibrillation and previous stroke or transient ischaemic attack: A subgroup analysis of ROCKET AF. Lancet Neurol. 2012, 11, 315–322. [Google Scholar] [CrossRef]
- Easton, J.D.; Lopes, R.D.; Bahit, M.C.; Wojdyla, D.M.; Granger, C.B.; Wallentin, L.; Alings, M.; Goto, S.; Lewis, B.S.; Rosenqvist, M.; et al. Apixaban compared with warfarin in patients with atrial fibrillation and previous stroke or transient ischaemic attack: A subgroup analysis of the ARISTOTLE trial. Lancet Neurol. 2012, 11, 503–511. [Google Scholar] [CrossRef]
- Rost, N.S.; Giugliano, R.P.; Ruff, C.T.; Murphy, S.A.; Crompton, A.E.; Norden, A.D.; Silverman, S.; Singhal, A.B.; Nicolau, J.C.; SomaRaju, B.; et al. Outcomes With Edoxaban Versus Warfarin in Patients With Previous Cerebrovascular Events: Findings From ENGAGE AF-TIMI 48 (Effective Anticoagulation With Factor Xa Next Generation in Atrial Fibrillation-Thrombolysis in Myocardial Infarction 48). Stroke 2016, 47, 2075–2082. [Google Scholar] [CrossRef]
- Seiffge, D.J.; De Marchis, G.M.; Koga, M.; Paciaroni, M.; Wilson, D.; Cappellari, M.; Macha Md, K.; Tsivgoulis, G.; Ambler, G.; Arihiro, S.; et al. Ischemic Stroke despite Oral Anticoagulant Therapy in Patients with Atrial Fibrillation. Ann. Neurol. 2020. [Google Scholar] [CrossRef]
- Drouet, L.; Bal Dit Sollier, C.; Steiner, T.; Purrucker, J. Measuring non-vitamin K antagonist oral anticoagulant levels: When is it appropriate and which methods should be used? Int. J. Stroke 2016, 11, 748–758. [Google Scholar] [CrossRef]
- Wardlaw, J.M.; Smith, E.E.; Biessels, G.J.; Cordonnier, C.; Fazekas, F.; Frayne, R.; Lindley, R.I.; O’Brien, J.T.; Barkhof, F.; Benavente, O.R.; et al. Neuroimaging standards for research into small vessel disease and its contribution to ageing and neurodegeneration. Lancet Neurol. 2013, 12, 822–838. [Google Scholar] [CrossRef]
- Fazekas, F.; Chawluk, J.B.; Alavi, A.; Hurtig, H.I.; Zimmerman, R.A. MR signal abnormalities at 1.5 T in Alzheimer’s dementia and normal aging. AJR Am. J. Roentgenol. 1987, 149, 351–356. [Google Scholar] [CrossRef] [PubMed]
- Amarenco, P.; Bogousslavsky, J.; Caplan, L.R.; Donnan, G.A.; Wolf, M.E.; Hennerici, M.G. The ASCOD phenotyping of ischemic stroke (Updated ASCO Phenotyping). Cerebrovasc. Dis. 2013, 36, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Bamford, J.; Sandercock, P.; Dennis, M.; Burn, J.; Warlow, C. Classification and natural history of clinically identifiable subtypes of cerebral infarction. Lancet 1991, 337, 1521–1526. [Google Scholar] [CrossRef]
- Wallentin, L.; Yusuf, S.; Ezekowitz, M.D.; Alings, M.; Flather, M.; Franzosi, M.G.; Pais, P.; Dans, A.; Eikelboom, J.; Oldgren, J.; et al. Efficacy and safety of dabigatran compared with warfarin at different levels of international normalised ratio control for stroke prevention in atrial fibrillation: An analysis of the RE-LY trial. Lancet 2010, 376, 975–983. [Google Scholar] [CrossRef]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomstrom-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association of Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2020. [Google Scholar] [CrossRef]
- European Medicines Agency. European Public Assessment Report (EPAR) for Xarelto; European Medicines Agency: Amsterdam, The Netherland, 2019.
- Stoll, S.; Macha, K.; Marsch, A.; Gerner, S.T.; Siedler, G.; Frohlich, K.; Volbers, B.; Strasser, E.F.; Schwab, S.; Kallmunzer, B. Ischemic stroke and dose adjustment of oral Factor Xa inhibitors in patients with atrial fibrillation. J. Neurol. 2020, 267, 1–6. [Google Scholar] [CrossRef]
- Macha, K.; Marsch, A.; Siedler, G.; Breuer, L.; Strasser, E.F.; Engelhorn, T.; Schwab, S.; Kallmunzer, B. Cerebral Ischemia in Patients on Direct Oral Anticoagulants. Stroke 2019, 50, 873–879. [Google Scholar] [CrossRef]
- Vrijens, B.; Heidbuchel, H. Non-vitamin K antagonist oral anticoagulants: Considerations on once- vs. twice-daily regimens and their potential impact on medication adherence. Europace 2015, 17, 514–523. [Google Scholar] [CrossRef]
- Costa, E.; Giardini, A.; Savin, M.; Menditto, E.; Lehane, E.; Laosa, O.; Pecorelli, S.; Monaco, A.; Marengoni, A. Interventional tools to improve medication adherence: Review of literature. Patient Prefer Adherence 2015, 9, 1303–1314. [Google Scholar] [CrossRef]
- Lip, G.Y.H.; Lane, D.A.; Buller, H.; Apostolakis, S. Development of a novel composite stroke and bleeding risk score in patients with atrial fibrillation: The AMADEUS Study. Chest 2013, 144, 1839–1847. [Google Scholar] [CrossRef]
- Mega, J.L.; Braunwald, E.; Wiviott, S.D.; Bassand, J.P.; Bhatt, D.L.; Bode, C.; Burton, P.; Cohen, M.; Cook-Bruns, N.; Fox, K.A.; et al. Rivaroxaban in patients with a recent acute coronary syndrome. N. Engl. J. Med. 2012, 366, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Eikelboom, J.W.; Connolly, S.J.; Bosch, J.; Dagenais, G.R.; Hart, R.G.; Shestakovska, O.; Diaz, R.; Alings, M.; Lonn, E.M.; Anand, S.S.; et al. Rivaroxaban with or without Aspirin in Stable Cardiovascular Disease. N. Engl. J. Med. 2017, 377, 1319–1330. [Google Scholar] [CrossRef] [PubMed]
- Powers, W.J.; Rabinstein, A.A.; Ackerson, T.; Adeoye, O.M.; Bambakidis, N.C.; Becker, K.; Biller, J.; Brown, M.; Demaerschalk, B.M.; Hoh, B.; et al. Guidelines for the Early Management of Patients With Acute Ischemic Stroke: 2019 Update to the 2018 Guidelines for the Early Management of Acute Ischemic Stroke: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2019, 50, e344–e418. [Google Scholar] [CrossRef] [PubMed]
- Mach, F.; Baigent, C.; Catapano, A.L.; Koskinas, K.C.; Casula, M.; Badimon, L.; Chapman, M.J.; De Backer, G.G.; Delgado, V.; Ference, B.A.; et al. 2019 ESC/EAS Guidelines for the management of dyslipidaemias: Lipid modification to reduce cardiovascular risk. Eur. Heart J. 2020, 41, 111–188. [Google Scholar] [CrossRef]
- Purrucker, J.C.; Haas, K.; Rizos, T.; Khan, S.; Poli, S.; Kraft, P.; Kleinschnitz, C.; Dziewas, R.; Binder, A.; Palm, F.; et al. Coagulation Testing in Acute Ischemic Stroke Patients Taking Non-Vitamin K Antagonist Oral Anticoagulants. Stroke 2017, 48, 152–158. [Google Scholar] [CrossRef]
- Paciaroni, M.; Agnelli, G.; Caso, V.; Silvestrelli, G.; Seiffge, D.J.; Engelter, S.; De Marchis, G.M.; Polymeris, A.; Zedde, M.L.; Yaghi, S.; et al. Causes and Risk Factors of Cerebral Ischemic Events in Patients With Atrial Fibrillation Treated With Non-Vitamin K Antagonist Oral Anticoagulants for Stroke Prevention. Stroke 2019, 50, 2168–2174. [Google Scholar] [CrossRef]
- Oesterle, A.; Laufs, U.; Liao, J.K. Pleiotropic Effects of Statins on the Cardiovascular System. Circ. Res. 2017, 120, 229–243. [Google Scholar] [CrossRef]
- Huisman, M.V.; Rothman, K.J.; Paquette, M.; Teutsch, C.; Diener, H.C.; Dubner, S.J.; Halperin, J.L.; Ma, C.S.; Zint, K.; Elsaesser, A.; et al. The Changing Landscape for Stroke Prevention in AF: Findings From the GLORIA-AF Registry Phase 2. J. Am. Coll. Cardiol. 2017, 69, 777–785. [Google Scholar] [CrossRef]
| VKA (n = 127) | NOAC (n = 214) | p-Value | |
|---|---|---|---|
| Age, mean (SD) | 79.4 (8.0) | 77.9 (8.9) | 0.119 |
| Women | 57 (44.9) | 102 (47.7) | 0.654 |
| NOAC | - | ||
| Apixaban | - | 65 (30.4) | |
| Dabigatran | - | 34 (15.9) | |
| Edoxaban | - | 14 (6.5) | |
| Rivaroxaban | - | 101 (47.2) | |
| Low-dose NOAC | - | 97/197 (49.2) | |
| Phenprocoumon | 125 (98.4) | - | |
| Concomitant antiplatelet therapy | 3 (2.4) | 22 (10.3) | 0.009 |
| Comorbidities | |||
| Arterial hypertension | 112 (88.2) | 195 (91.1) | 0.455 |
| Diabetes mellitus | 47 (37.0) | 71 (33.2) | 0.482 |
| Hyperlipidemia | 51 (40.2) | 67 (31.3) | 0.101 |
| Ischemic heart disease | 46 (36.2) | 75 (35.0) | 0.907 |
| Myocardial infarction | 19 (15.0) | 30 (14.0) | 0.873 |
| Peripheral artery disease | 16 (12.6) | 22 (10.3) | 0.594 |
| Stroke/TIA | 39 (30.7) | 81 (37.9) | 0.198 |
| Bleeding | 6 (4.7) | 14 (6.5) | 0.635 |
| Smoking | 14 (11.0) | 34 (15.9) | 0.26 |
| Malignancy, active | 4 (3.3) | 12 (5.9) | 0.428 |
| Renal function at admission | |||
| GFR; mean (SD) | 66.5 (22.3) | 68.2 (20.3) | 0.471 |
| GFR < 50 mL/min | 26 (20.5) | 43 (20.1) | >0.99 |
| GFR < 30 mL/min | 9 (7.1) | 8 (3.7) | 0.201 |
| Lipid levels, serum, mg/dl mmol/L | |||
| HDL cholesterol | 41 (34–51) 1.1 (0.9–1.3) | 44 (35–52) 1.1 (0.9–1.3) | 0.409 |
| LDL cholesterol | 90 (68–112) 2.3 (1.8–2.9) | 97 (71–118) 2.5 (1.8–3.1) | 0.202 |
| LDL cholesterol ≥ 70 mg/dl (≥1.8 mmol/L) | 89/120 (74.2) | 161/204 (78.9) | 0.34 |
| Triglycerides | 104 (72–129) | 97 (71–128) | 0.355 |
| Onset (last-seen-well in case exact onset is unknown) to admission *, hours | 3.7 (2.0–8.4) | 3.5 (1.5–7.0) | 0.445 |
| Functional status | |||
| Pre-stroke mRS | 2 (1–3) | 2 (1–3) | 0.943 |
| mRS at admission | 4 (3–4) | 3 (2–4) | 0.251 |
| mRS at discharge | 3 (2–4) | 3 (2–4) | 0.799 |
| NIHSS at admission | 7 (3–17) | 3 (3–16) | 0.758 |
| Imaging modality | |||
| CT | 123 (96.9) | 210 (98.1) | 0.477 |
| MRI | 32 (25.2) | 54 (25.2) | >0.99 |
| Large-vessel occlusion | 61 (48.0) | 109 (50.9) | 0.654 |
| IVT | 29 (22.8) | 16 (7.5) | <0.001 |
| EVT | 41 (32.3) | 74 (34.6) | 0.723 |
| CAS | 0 (0) | 4 (1.9) | 0.301 |
| CEA | 1 (0.8) | 7 (3.3) | 0.266 |
| Disease (Causality) | VKA (n = 127) | NOAC (n = 214) | p |
|---|---|---|---|
| Cardiac pathology (potential) | 127 | 214 | - |
| Atherosclerosis (potential) | 13/125 (10.4) | 35/212 (16.5) | 0.147 |
| Atherosclerosis (potential or uncertain) | 19/125 (15.2) | 42/212 (19.8) | 0.309 |
| Small-vessel disease (potential) | 3 (2.4) | 13 (6.1) | 0.184 |
| Small-vessel disease (potential or uncertain) | 21 (16.5) | 55 (25.7) | 0.059 |
| Other causes (potential) | 0 (0) | 2 (0.9) | 0.531 |
| Dissection (potential) | 0 (0) | 2 (0.9) | 0.531 |
| Insufficient work-up (N9) | 2 (1.6) | 2 (0.9) | 0.63 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Purrucker, J.C.; Hölscher, K.; Kollmer, J.; Ringleb, P.A. Etiology of Ischemic Strokes of Patients with Atrial Fibrillation and Therapy with Anticoagulants. J. Clin. Med. 2020, 9, 2938. https://doi.org/10.3390/jcm9092938
Purrucker JC, Hölscher K, Kollmer J, Ringleb PA. Etiology of Ischemic Strokes of Patients with Atrial Fibrillation and Therapy with Anticoagulants. Journal of Clinical Medicine. 2020; 9(9):2938. https://doi.org/10.3390/jcm9092938
Chicago/Turabian StylePurrucker, Jan C., Kyra Hölscher, Jennifer Kollmer, and Peter A. Ringleb. 2020. "Etiology of Ischemic Strokes of Patients with Atrial Fibrillation and Therapy with Anticoagulants" Journal of Clinical Medicine 9, no. 9: 2938. https://doi.org/10.3390/jcm9092938
APA StylePurrucker, J. C., Hölscher, K., Kollmer, J., & Ringleb, P. A. (2020). Etiology of Ischemic Strokes of Patients with Atrial Fibrillation and Therapy with Anticoagulants. Journal of Clinical Medicine, 9(9), 2938. https://doi.org/10.3390/jcm9092938





