The Role of Sense of Voice Presence and Anxiety Reduction in AVATAR Therapy
Abstract
1. Introduction
2. Methods
2.1. Participants:
2.2. Measures
2.2.1. Taken from Baseline and Follow-Up Assessments (Blind Assessors)
2.2.2. In-Session Measures (Self-Reported by Participants)
2.3. AVATAR Therapy
2.4. Statistical Analyses
3. Results
3.1. Demographics
3.2. Hypothesis 1 Sustained Levels of Sense of Voice Presence Across Therapy Sessions
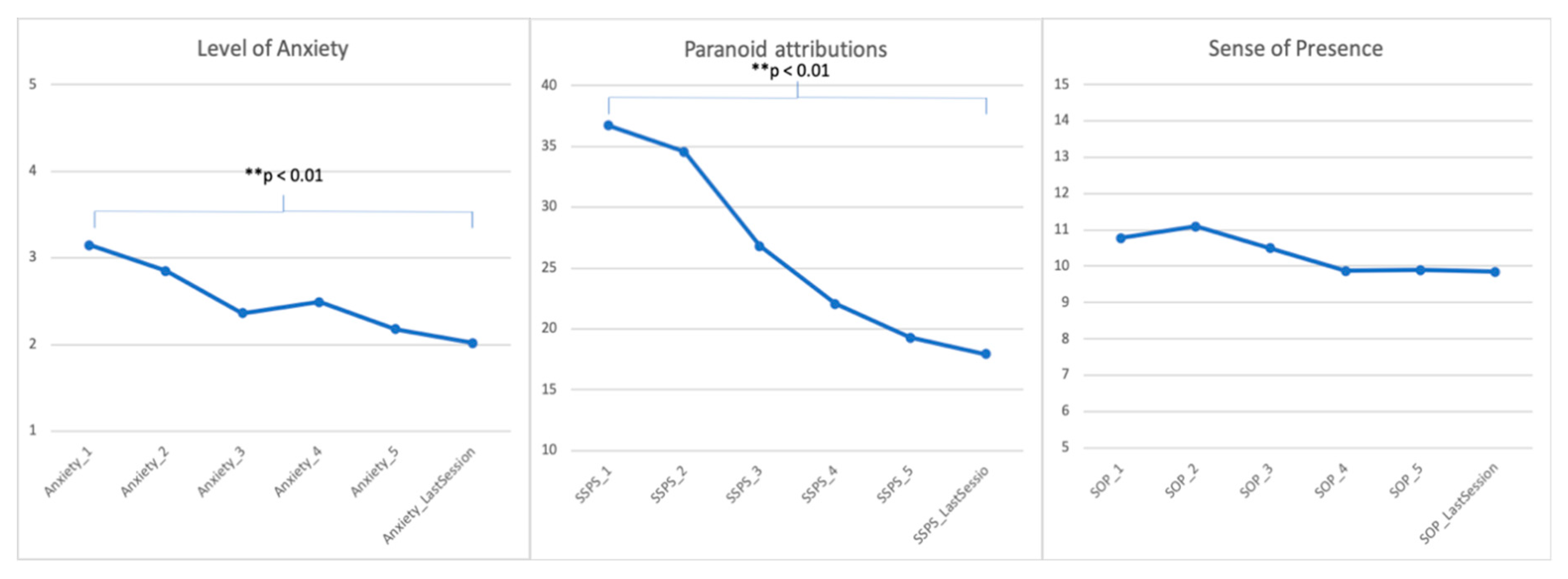
3.3. Hypotheses 2 Reduction of Anxiety and Paranoid Attributions Across Therapy Sessions
3.4. Hypothesis 3 Associations with Better Therapy Outcomes
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Data Sharing
References
- Woods, A.; Jones, N.; Bernini, M.; Callard, F.; Alderson-Day, B.; Badcock, J.C.; Bell, V.; Cook, C.C.H.; Csordas, T.; Humpston, C.; et al. Interdisciplinary Approaches to the Phenomenology of Auditory Verbal Hallucinations. Schizophr. Bull. 2014, 40, S246–S254. [Google Scholar] [CrossRef] [PubMed]
- Wilkinson, S.; Bell, V. The Representation of Agents in Auditory Verbal Hallucinations. Mind Lang. 2016, 31, 104–126. [Google Scholar] [CrossRef] [PubMed]
- Woods, A.; Jones, N.; Alderson-Day, B.; Callard, F.; Fernyhough, C. Experiences of hearing voices: Analysis of a novel phenomenological survey. Lancet Psychiatry 2016, 2, 323–331. [Google Scholar] [CrossRef]
- Beavan, V.; Read, J.; Cartwright, C. The prevalence of voice-hearers in the general population: A literature review. J. Ment. Health 2011, 20, 281–292. [Google Scholar] [CrossRef] [PubMed]
- Beavan, V. Towards a definition of hearing voices: A phenomenological approach. Psychos. Psychol. Soc. Integr. Approaches 2011, 3, 63–73. [Google Scholar] [CrossRef]
- McCarthy-Jones, S.; Thomas, N.; Strauss, C.; Dodgson, G.; Jones, N.; Woods, A.; Brewin, C.R.; Hayward, M.; Stephane, M.; Barton, J.; et al. Better Than Mermaids and Stray Dogs? Subtyping Auditory Verbal Hallucinations and Its Implications for Research and Practice. Schizophr. Bull. 2014, 40, S275–S284. [Google Scholar] [CrossRef] [PubMed]
- Steel, C.; Schnackenberg, J.; Perry, H.; Longden, E.; Greenfield, E.; Corstens, D. Making Sense of Voices: A case series. Psychosis 2019, 11, 3–15. [Google Scholar] [CrossRef]
- Hayward, M.; Jones, A.M.; Bogen-Johnston, L.; Thomas, N.; Strauss, C. Relating Therapy for distressing auditory hallucinations: A pilot randomized controlled trial. Schizophr. Res. 2017, 183, 137–142. [Google Scholar] [CrossRef]
- Leff, J.; Williams, G.; Huckvale, M.A.; Arbuthnot, M.; Leff, A.P. Computer-assisted therapy for medication-resistant auditory hallucinations: Proof-of-concept study. Br. J. Psychiatry 2013, 202, 428–433. [Google Scholar] [CrossRef] [PubMed]
- Craig, T.K.; Rus-Calafell, M.; Ward, T.; Leff, J.P.; Huckvale, M.; Howarth, E.; Emsley, R.; Garety, P.A. AVATAR therapy for auditory verbal hallucinations in people with psychosis: A single-blind, randomised controlled trial. Lancet Psychiatry 2018, 5, 31–40. [Google Scholar] [CrossRef]
- Leff, J.; Williams, G.; Huckvale, M.; Arbuthnot, M.; Leff, A.P. Avatar therapy for persecutory auditory hallucinations: What is it and how does it work? Psychos. Psychol. Soc. Integr. Approaches 2014, 6, 166–176. [Google Scholar] [CrossRef] [PubMed]
- Birchwood, M.; Dunn, G.; Meaden, A.; Tarrier, N.; Lewis, S.; Wykes, T.; Davies, L.; Michail, M.; Peters, E. The COMMAND trial of cognitive therapy to prevent harmful compliance with command hallucinations: Predictors of outcome and mediators of change. Psychol. Med. 2018, 48, 1966–1974. [Google Scholar] [CrossRef] [PubMed]
- Birchwood, M.; Michail, M.; Meaden, A.; Tarrier, N.; Lewis, S.; Wykes, T.; Davies, L.; Dunn, G.; Peters, E. Cognitive behaviour therapy to prevent harmful compliance with command hallucinations (COMMAND): A randomised controlled trial. Lancet Psychiatry 2014, 1, 23–33. [Google Scholar] [CrossRef]
- Birchwood, M.; Chadwick, P. The omnipotence of voices: Testing the validity of a cognitive model. Psychol. Med. 1997, 27, 1345–1353. [Google Scholar] [CrossRef] [PubMed]
- Garety, P.A.; Bebbington, P.; Fowler, D.; Freeman, D.; Kuipers, E. Implications for neurobiological research of cognitive models of psychosis: A theoretical paper. Psychol. Med. 2007, 37, 1377–1391. [Google Scholar] [CrossRef]
- du Sert, O.P.; Potvin, S.; Lipp, O.; Dellazizzo, L.; Laurelli, M.; Breton, R.; Lalonde, P.; Phraxayavong, K.; O’Connor, K.; Pelletier, J.F.; et al. Virtual reality therapy for refractory auditory verbal hallucinations in schizophrenia: A pilot clinical trial. Schizophr. Res. 2018, 197, 176–181. [Google Scholar] [CrossRef]
- Meyerbröker, K.; Emmelkamp, P. Virtual Reality Exposure Therapy for Anxiety Disorders: The State of the Art. In Advanced Computational Intelligence Paradigms in Healthcare 6. Virtual Reality in Psychotherapy, Rehabilitation, and Assessment; Brahnam, S., Jain, L., Eds.; Springer: Berlin/Heidelberg, Germany, 2011; pp. 47–62. [Google Scholar]
- Rus-Calafell, M.; Garety, P.; Sason, E.; Craig, T.J.K.; Valmaggia, L.R. Virtual reality in the assessment and treatment of psychosis: A systematic review of its utility, acceptability and effectiveness. Psychol. Med. 2017, 48, 1–30. [Google Scholar] [CrossRef]
- Freeman, D.; Bradley, J.; Antley, A.; Bourke, E.; DeWeever, N.; Evans, N.; Černis, E.; Sheaves, B.; Waite, F.; Dunn, G.; et al. Virtual reality in the treatment of persecutory delusions: Randomised controlled experimental study testing how to reduce delusional conviction. Br. J. Psychiatry 2016, 209, 62–67. [Google Scholar] [CrossRef]
- Pot-Kolder, R.M.C.A.; Geraets, C.N.W.; Veling, W.; van Beilen, M.; Staring, A.B.P.; Gijsman, H.J.; Delespaul, P.A.E.G.; van der Gaag, M. Virtual-reality-based cognitive behavioural therapy versus waiting list control for paranoid ideation and social avoidance in patients with psychotic disorders: A single-blind randomised controlled trial. Lancet Psychiatry 2018, 5, 217–226. [Google Scholar] [CrossRef]
- Craig, T.K.; Ward, T.; Rus-Calafell, M. AVATAR therapy for refractory hallucinations. In Brief Interventions for Psychosis: A Clinical Compendium; Pradhan, B., Pinninti, N., Rathod, S., Eds.; Springer: London, UK, 2016; pp. 41–54. [Google Scholar]
- Wilson, M. Six views of embodied cognition. Psychon. Bull. Rev. 2002, 9, 625–636. [Google Scholar] [CrossRef]
- Slater, M. How Colorful Was Your Day? Why Questionnaires Cannot Assess Presence in Virtual Environments. Presence Teleoperators Virtual Environ. 2004, 13, 484–493. [Google Scholar] [CrossRef]
- Nowac, K.; Biocca, F. The effect of the agency and anthropomorphism on users’ sense of telepresence, copresence, and social presence in virtual environments. Presence Teleoperators Virtual Environ. 2003, 12, 481–494. [Google Scholar] [CrossRef]
- Slater, M.; Usoh, M.; Steed, A. Depth of presence in virtual environments. Presence Teleoperators Virtual Environ. 1994, 3, 130–144. [Google Scholar] [CrossRef]
- Witmer, B.G.; Singer, M.J. Measuring Presence in Virtual Environments: A Presence Questionnaire. Presence Teleoperators Virtual Environ. 1998, 7, 225–240. [Google Scholar] [CrossRef]
- Riva, G.; Mantovani, F.; Capideville, C.S.; Preziosa, A.; Morganti, F.; Villani, D.; Gaggioli, A.; Botella, C.; Alcañiz, M. Affective interactions using virtual reality: The link between presence and emotions. Cyberpsychol. Behav. 2007, 10, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Riva, G.; Mantovani, F. Being There: Understanding the Feeling of Presence in a Synthetic Environment and its Potential for Clinical Change. In Virtual Reality in Psychological, Medical and Pedagogical Applications; Eichenberg, C., Ed.; InTech Open: Rijeka, Croatia, 2012. [Google Scholar]
- Ling, Y.; Nefs, H.T.; Morina, N.; Heynderickx, I.; Brinkman, W.P. A meta-analysis on the relationship between self-reported presence and anxiety in virtual reality exposure therapy for anxiety disorders. PLoS ONE 2014, 9, e96144. [Google Scholar] [CrossRef]
- Ward, T.; Rus-Calafell, M.; Ramadhan, Z.; Soumelidou, O.; Fornells-Ambrojo, M.; Garety, P.; Craig, T.K.J. AVATAR Therapy for Distressing Voices: A Comprehensive Account of Therapeutic Targets. Schizophr. Bull. 2020, sbaa061. [Google Scholar] [CrossRef]
- Haddock, G.; McCarron, J.; Tarrier, N.; Faragher, E.B. Scales to measure dimensions of hallucinations and delusions: The psychotic symptom rating scales (PSYRATS). Psychol. Med. 1999, 29, 879–889. [Google Scholar] [CrossRef]
- Moritz, S.; Andreou, C.; Schneider, B.C.; Wittekind, C.E.; Menon, M.; Balzan, R.P.; Woodward, T.S. Sowing the seeds of doubt: A narrative review on metacognitive training in schizophrenia. Clin. Psychol. Rev. 2014, 34, 358–366. [Google Scholar] [CrossRef]
- Chadwick, P.; Lees, S.; Birchwood, M. The revised Beliefs About Voices Questionnaire (BAVQ-R). Br. J. Psychiatry 2000, 177, 229–232. [Google Scholar] [CrossRef]
- Freeman, D.; Pugh, K.; Green, C.; Valmaggia, L.; Dunn, G.; Garety, P. A measure of state persecutory ideation for experimental studies. J. Nerv. Ment. Dis. 2007, 195, 781–784. [Google Scholar] [CrossRef] [PubMed]
- Schwind, V.; Knierim, P.; Haas, N.; Henze, N. Using Presence Questionnaires in Virtual Reality. In Proceedings of the Conference on Human Factors in Computing Systems, Glasgow, Scotland, 3 May 2019. [Google Scholar]
- Foa, E.; Kozak, M.J. Emotional processing of fear: Exposure to corrective information. Psychol. Bull. 1986, 99, 20–35. [Google Scholar] [CrossRef] [PubMed]
- Craske, M.G.; Treanor, M.; Conway, C.C.; Zbozinek, T.; Vervliet, B. Maximizing exposure therapy: An inhibitory learning approach. Behav. Res. 2014, 58, 10–23. [Google Scholar] [CrossRef] [PubMed]
- van der Gaag, M.; Valmaggia, L.; Smit, F. The effects of individually tailored formulation-based cognitive behavioural therapy in auditory hallucinations and delusions: A meta-analysis. Schizophr. Res. 2014, 156, 30–37. [Google Scholar] [CrossRef] [PubMed]
- Longden, E.; Corstens, D.; Escher, S.; Romme, M. Voice hearing in a biographical context: A model for formulating the relationship between voices and life history. Psychos. Psychol. Soc. Integr. Approaches 2012, 4, 224–234. [Google Scholar] [CrossRef]
- Morrison, A.P. The Interpretation of Intrusions in Psychosis: An Integrative Cognitive Approach to Hallucinations and Delusions. Behav. Cogn. Psychother. 2001, 29, 257–276. [Google Scholar] [CrossRef]
| N (%) | M (SD) | |
|---|---|---|
| Age | 43.87 (9.33) | |
| Gender | ||
| Male | 30 (77%) | |
| Female | 9 (23%) | |
| Ethnicity | ||
| White British | 13 (33%) | |
| Black British | 5 (13%) | |
| Black Caribbean | 3 (8%) | |
| Black African | 5 (13%) | |
| Asian Indian | 3 (8%) | |
| Other | 10 (25%) | |
| Education | ||
| Primary | 3 (8%) | |
| Secondary or equivalent | 18 (46%) | |
| Vocational education | 9 (23%) | |
| University degree | 9 (23%) | |
| Employment a | ||
| Employed full-time | 0 (0%) | |
| Employed part time | 3 (8%) | |
| Unemployed | 36 (92%) | |
| Student | 2 (5%) | |
| Housewife/husband | 1 (3%) | |
| Marital Status | ||
| Married/cohabiting | 1 (3%) | |
| Single | 30 (77%) | |
| Single in relationship | 3 (8%) | |
| Divorced | 5 (12%) | |
| Diagnosis | ||
| Paranoid Schizophrenia | 29 (74%) | |
| Schizoaffective Disorder | 6 (15%) | |
| Unspecific Psychosis | 1 (3%) | |
| Dep w/ psychotic symptoms | 3 (8%) | |
| N | M (SD) | |
| Number of voices | ||
| 1 | 10 (25%) | |
| 2 | 7 (18%) | |
| 3 | 7 (18%) | |
| 4 | 1 (3%) | |
| 5 | 9 (23%) | |
| Unsure/many | 5 (13%) | |
| Length_Illness (years) | 21.79 (11.04) |
| Session_1 | Session_2 | Session_3 | Session_4 | Session_5 | Session_Last | tS1-SLast | p | Cohen’s d | |
|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | |||||||||
| Anxiety | 3.15 (1.18) | 2.85 (1.33) | 2.36 (1.09) | 2.49 (1.25) | 2.18 (1.14) | 2.03 (1.16) | 4.29 | p < 0.001 | 0.7 |
| Anxiety S1–S3 | 3.33 | p < 0.001 | 0.6 | ||||||
| Anxiety S4–SLast | 0.97 | 0.33 | 0.2 | ||||||
| Sense of Presence | 10.78 (2.61) | 11.10 (2.48) | 10.49 (2.76) | 9.87 (3.05) | 9.90 (3.28) | 9.85 (3.21) | 1.70 | 0.10 | 0.2 |
| Paranoid Thoughts | 36.72 (9.32) | 34.54 (10.38) | 26.82 (12.85) | 22.06 (14.54) | 19.26 (12.23) | 17.95 (12.64) | 9.15 | p < 0.001 | 1.4 |
| Baseline M (SD) | 12-Week FU M (SD) | Improvement M (SD) | |
|---|---|---|---|
| PSYRATS-AH_TOTAL | 27.87 (4.61) | 21.41 (9.5) | 6.46 (8.52) |
| PSYRATS-AH_Frequency | 6.33 (2.08) | 4.87 (2.55) | 1.46 (2.01) |
| PSYRATS-AH_Distress | 14.75 (2.97) | 10.38 (5.52) | 4.35 (5.32) |
| BAVQ-R_Omnipotence | 9.87 (3.99) | 6.79 (4.51) | 2.05 (3.81) |
| t | Beta | p | R2 | F | df | p | |
|---|---|---|---|---|---|---|---|
| Improvement in PSYRATS-AH (Total) | |||||||
| Overall model | 0.24 | 2.62 | 4 | 0.04 * | |||
| Reduction of Anxiety | −52 | −0.07 | 0.61 | 1 | |||
| Sense of Presence | 0.93 | 0.14 | 0.35 | 1 | |||
| Reduction of Paranoid Attributions | 0.25 | 0.03 | 0.80 | 1 | |||
| Reduction of Anxiety * Sense of Voice Presence | 2.39 | 0.46 | 0.02 * | 1 | |||
| Improvement in PSYRATS-AH (Frequency) | |||||||
| Overall model | 0.28 | 3.02 | 4 | 0.03 * | |||
| Reduction of Anxiety | −0.66 | −0.08 | 0.51 | 1 | |||
| Sense of Presence | 0.56 | 0.07 | 0.64 | 1 | |||
| Reduction of Paranoid Attributions | 1.48 | 0.16 | 0.14 | 1 | |||
| Reduction of Anxiety * Sense of Voice Presence | 2.94 | 0.47 | 0.00 ** | 1 | |||
| Improvement in PSYRATS-AH (Distress) | |||||||
| Overall model | 0.09 | 0.80 | 4 | 0.53 | |||
| Reduction of Anxiety | −0.62 | −0.41 | 0.53 | 1 | |||
| Sense of Presence | 0.46 | 0.05 | 0.65 | 1 | |||
| Reduction of Paranoid Attributions | 0.61 | 0.00 | 0.54 | 1 | |||
| Reduction of Anxiety * Sense of Voice Presence | 1.67 | 0.37 | 0.10 | 1 | |||
| Improvement in omnipotence BAVQ-R | |||||||
| Overall model | 0.04 | 0.36 | 4 | 0.83 | |||
| Reduction of Anxiety | 0.26 | 0.05 | 0.26 | 1 | |||
| Sense of Presence | 0.39 | 0.08 | 0.69 | 1 | |||
| Reduction of Paranoid Attributions | −0.87 | 0.15 | 0.39 | 1 | |||
| Reduction of Anxiety * Sense of Voice Presence | 0.51 | 0.13 | 0.61 | 1 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rus-Calafell, M.; Ward, T.; Zhang, X.C.; Edwards, C.J.; Garety, P.; Craig, T. The Role of Sense of Voice Presence and Anxiety Reduction in AVATAR Therapy. J. Clin. Med. 2020, 9, 2748. https://doi.org/10.3390/jcm9092748
Rus-Calafell M, Ward T, Zhang XC, Edwards CJ, Garety P, Craig T. The Role of Sense of Voice Presence and Anxiety Reduction in AVATAR Therapy. Journal of Clinical Medicine. 2020; 9(9):2748. https://doi.org/10.3390/jcm9092748
Chicago/Turabian StyleRus-Calafell, Mar, Thomas Ward, Xiao Chi Zhang, Clementine J. Edwards, Philippa Garety, and Tom Craig. 2020. "The Role of Sense of Voice Presence and Anxiety Reduction in AVATAR Therapy" Journal of Clinical Medicine 9, no. 9: 2748. https://doi.org/10.3390/jcm9092748
APA StyleRus-Calafell, M., Ward, T., Zhang, X. C., Edwards, C. J., Garety, P., & Craig, T. (2020). The Role of Sense of Voice Presence and Anxiety Reduction in AVATAR Therapy. Journal of Clinical Medicine, 9(9), 2748. https://doi.org/10.3390/jcm9092748





