Prolonged QT Interval in SARS-CoV-2 Infection: Prevalence and Prognosis
Abstract
:1. Introduction
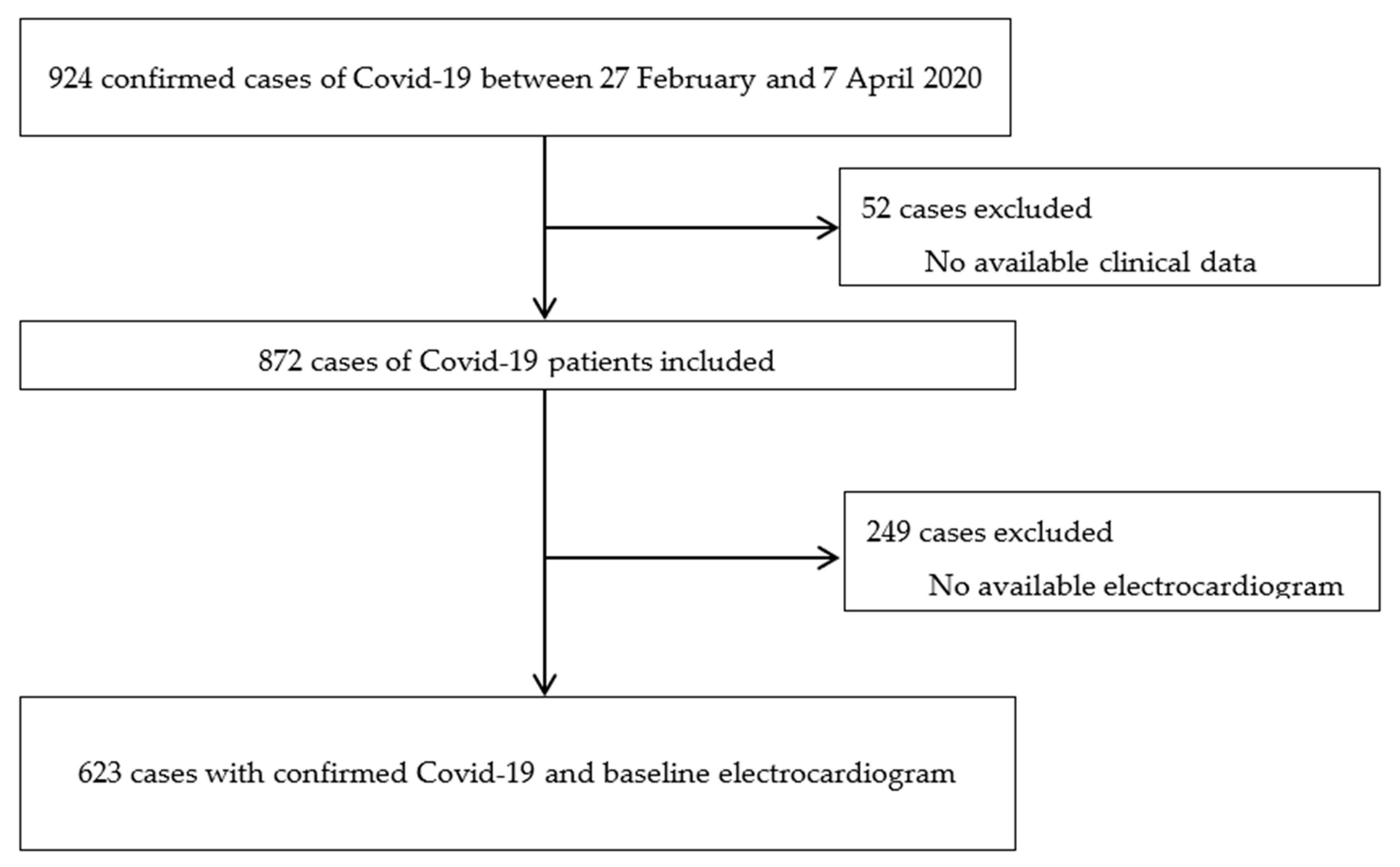
2. Experimental Section
Statistical Analysis
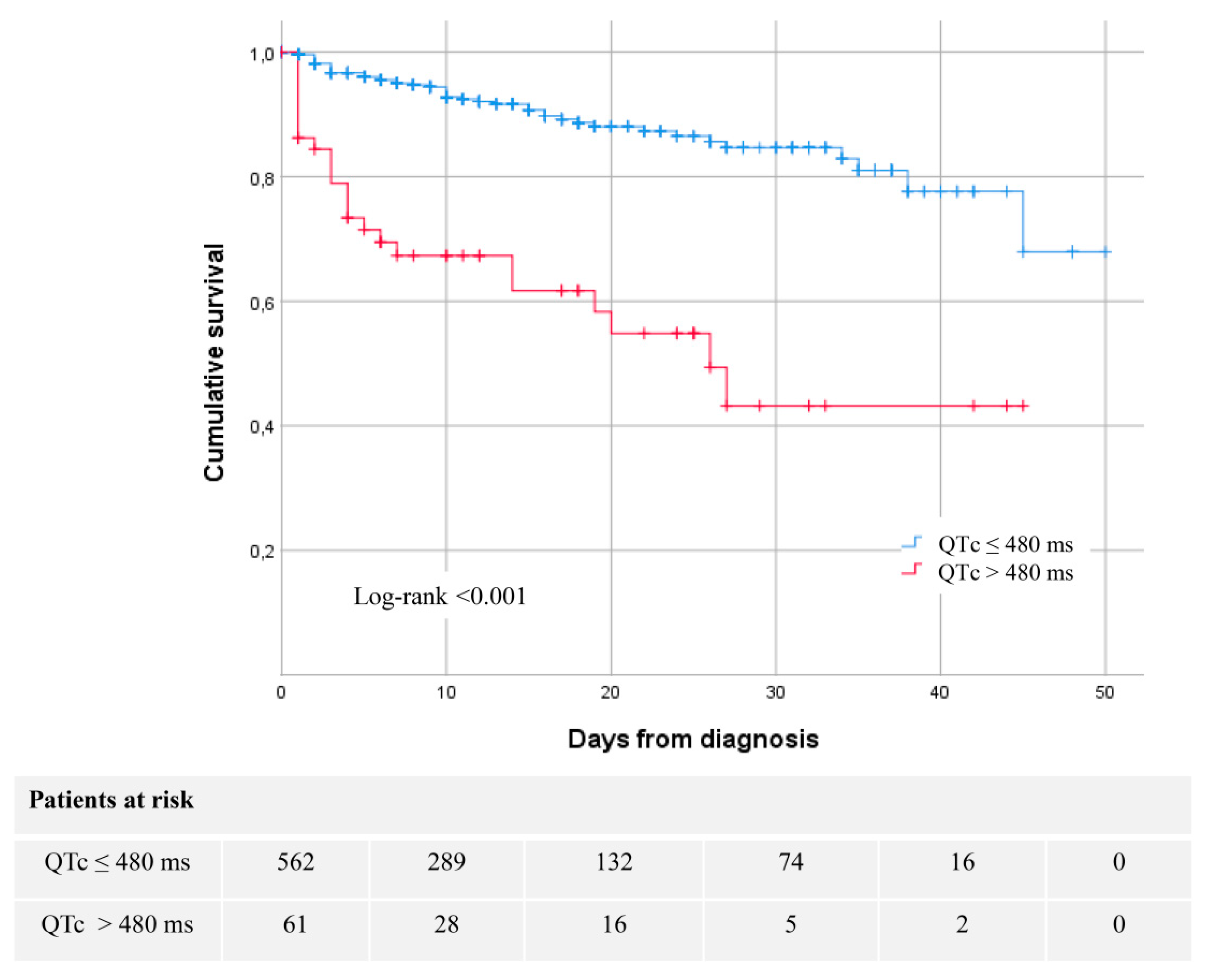
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Kochi, A.N.; Tagliari, A.P.; Forleo, G.B.; Fassini, G.M.; Tondo, C. Cardiac and arrhythmic complications in patients with COVID-19. J. Cardiovasc. Electrophysiol. 2020, 31, 1003–1008. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Saleh, M.; Gabriels, J.; Chang, D.; Kim, B.S.; Mansoor, A.; Mahmood, E.; Makker, P.; Ismail, H.; Goldner, B.; Willner, J.; et al. The Effect of Chloroquine, Hydroxychloroquine and Azithromycin on the Corrected QT Interval in Patients with SARS-CoV-2 Infection. Circ. Arrhythm. Electrophysiol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Mercuro, N.J.; Yen, C.F.; Shim, D.J.; Maher, T.R.; McCoy, C.M.; Zimetbaum, P.J.; Gold, H.S. Risk of QT Interval Prolongation Associated with Use of Hydroxychloroquine with or without Concomitant Azithromycin among Hospitalized Patients Testing Positive for Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Ramireddy, A.; Chugh, H.; Reinier, K.; Ebinger, J.; Park, E.; Thompson, M.; Cingolani, E.; Cheng, S.; Marban, E.; Albert, C.M.; et al. Experience With Hydroxychloroquine and Azithromycin in the Coronavirus Disease 2019 Pandemic: Implications for QT Interval Monitoring. J. Am. Heart Assoc. 2020, 9, e017144. [Google Scholar] [CrossRef] [PubMed]
- Chorin, E.; Dai, M.; Shulman, E.; Wadhwani, L.; Bar-Cohen, R.; Barbhaiya, C.; Aizer, A.; Holmes, D.; Bernstein, S.; Spinelli, M.; et al. The QT interval in patients with COVID-19 treated with hydroxychloroquine and azithromycin. Nat. Med. 2020, 26, 808–809. [Google Scholar] [CrossRef]
- Bun, S.; Taghji, P.; Courjon, J.; Squara, F.; Scarlatti, D.; Theodore, G.; Baudouy, D.; Sartre, B.; Labbaoui, M.; Dellamonica, J.; et al. QT interval prolongation under hydroxychloroquine/ azithromycin association for inpatients with SARS-CoV-2 lower respiratory tract infection. Clin. Pharmacol. Ther. 2020. [Google Scholar] [CrossRef]
- Furlan-Daniel, R.A.; Santos, L.F.S.; Geleilete, T.J.M.; Restini, C.B.A.; Bestetti, R.B. Abnormalities in electrocardiographic ventricular repolarization in patients with dengue virus infection. J. Infect. Dev. Ctries. 2019, 13, 759–763. [Google Scholar] [CrossRef] [Green Version]
- Chastain, D.B.; Veve, M.P.; Wagner, J.L. Abnormal QTc syndrome in HIV-infected patients: A systematic review of prevalence and risk factors. Antivir. Ther. 2019, 24, 459–465. [Google Scholar] [CrossRef]
- Reinsch, N.; Arendt, M.; Geisel, M.H.; Schulze, C.; Holzendorf, V.; Warnke, A.; Neumann, T.; Brockmeyer, N.H.; Schadendorf, D.; Eisele, L.; et al. Prolongation of the QTc interval in HIV-infected individuals compared to the general population. Infection 2017, 45, 659–667. [Google Scholar] [CrossRef]
- Alexander, L.K.; Keene, B.W.; Yount, B.L.; Geratz, J.D.; Small, J.D.; Baric, R.S. ECG changes after rabbit coronavirus infection. J. Electrocardiol. 1999, 32, 21–32. [Google Scholar] [CrossRef]
- Wang, Z.; Yang, B.; Li, Q.; Wen, L.; Zhang, R. Clinical Features of 69 Cases with Coronavirus Disease 2019 in Wuhan, China. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Lazzerini, P.E.; Acampa, M.; Capecchi, P.L.; Fineschi, I.; Selvi, E.; Moscadelli, V.; Zimbone, S.; Gentile, D.; Galeazzi, M.; Laghi-Pasini, F. Antiarrhythmic potential of anticytokine therapy in rheumatoid arthritis: Tocilizumab reduces corrected qt interval by controlling systemic inflammation. Arthritis Care Res. 2015, 67, 332–339. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kobayashi, H.; Kobayashi, Y.; Yokoe, I.; Kitamura, N.; Nishiwaki, A.; Takei, M.; Giles, J.T. Heart rate–corrected qt interval duration in rheumatoid arthritis and its reduction with treatment with the interleukin 6 inhibitor tocilizumab. J. Rheumatol. 2018, 45, 1620–1627. [Google Scholar] [CrossRef] [PubMed]
- Lazzerini, P.E.; Acampa, M.; Capecchi, P.L.; Hammoud, M.; Maffei, S.; Bisogno, S.; Barreca, C.; Galeazzi, M.; Laghi-Pasini, F. Association between high sensitivity C-reactive protein, heart rate variability and corrected QT interval in patients with chronic inflammatory arthritis. Eur. J. Intern. Med. 2013, 24, 368–374. [Google Scholar] [CrossRef] [PubMed]
- Panoulas, V.; Toms, T.; Douglas, K.; Sandoo, A.; Metsios, G.; Stavropoulos-Kalonoglou, A.; Kitas, G. Prolonged Qtc Interval Predicts All-cause Mortality in Patients with Rheumatoid Arthritis: An Association Driven by High Inflammatory Burden—PubMed—NCBI. Available online: https://www.ncbi.nlm.nih.gov/pubmed/?term=24097136 (accessed on 27 April 2020).
- Kazumi, T.; Kawaguchi, A.; Hirano, T.; Yoshino, G. C-reactive protein in young, apparently healthy men: Associations with serum Leptin, QTc interval, and high-density lipoprotein-cholesterol. Metabolism 2003, 52, 1113–1116. [Google Scholar] [CrossRef]
- Wu, K.C.; Zhang, L.; Haberlen, S.A.; Ashikaga, H.; Brown, T.T.; Budoff, M.J.; D’Souza, G.; Kingsley, L.A.; Palella, F.J.; Margolick, J.B.; et al. Predictors of electrocardiographic QT interval prolongation in men with HIV. Heart 2019, 105, 559–565. [Google Scholar] [CrossRef]
- 2015 ESC Guidelines for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death: The Task Force for the Management of Patients With Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the Europe. Available online: https://pubmed.ncbi.nlm.nih.gov/26320108/ (accessed on 1 July 2020).
- Jankelson, L.; Karam, G.; Becker, M.L.; Chinitz, L.A.; Tsai, M.-C. QT prolongation, torsades de pointes, and sudden death with short courses of chloroquine or hydroxychloroquine as used in COVID-19: A systematic review. Heart Rhythm 2020. [Google Scholar] [CrossRef]
- Borba, M.G.S.; Val, F.F.A.; Sampaio, V.S.; Alexandre, M.A.A.; Melo, G.C.; Brito, M.; Mourão, M.P.G.; Brito-Sousa, J.D.; Baía-da-Silva, D.; Guerra, M.V.F.; et al. Effect of High vs Low Doses of Chloroquine Diphosphate as Adjunctive Therapy for Patients Hospitalized With Severe Acute Respiratory Syndrome Coronavirus 2 (SARS-CoV-2) Infection: A Randomized Clinical Trial. JAMA Netw. Open 2020, 3, e208857. [Google Scholar] [CrossRef] [Green Version]
- Chang, D.; Saleh, M.; Gabriels, J.; Ismail, H.; Goldner, B.; Willner, J.; Beldner, S.; Mitra, R.; John, R.; Epstein, L.M. Inpatient Use of Ambulatory Telemetry Monitors for COVID-19 Patients Treated with Hydroxychloroquine and/or Azithromycin. J. Am. Coll. Cardiol. 2020. [Google Scholar] [CrossRef]
- Hooks, M.; Bart, B.; Vardeny, O.; Westanmo, A.; Adabag, S. Effects of Hydroxychloroquine Treatment on QT Interval. Heart Rhythm 2020. [Google Scholar] [CrossRef]
- Rijnbeek, P.R.; Van Herpen, G.; Bots, M.L.; Man, S.; Verweij, N.; Hofman, A.; Hillege, H.; Numans, M.E.; Swenne, C.A.; Witteman, J.C.M.; et al. Normal values of the electrocardiogram for ages 16–90 years. J. Electrocardiol. 2014, 47, 914–921. [Google Scholar] [CrossRef] [PubMed]
- Waheed, S.; Malik, R.; Waheed, S.; Parashara, D.; Perez, J. Association of QT interval with mortality by kidney function: Results from the National Health and Nutrition Examination Survey (NHANES). Open Heart 2017, 4, e000683. [Google Scholar] [CrossRef]
- Liu, P.; Wang, L.; Han, D.; Sun, C.; Xue, X.; Li, G. Acquired long QT syndrome in chronic kidney disease patients. Ren. Fail. 2020, 42, 54–65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cox, A.J.; Azeem, A.; Yeboah, J.; Soliman, E.Z.; Aggarwal, S.R.; Bertoni, A.G.; Carr, J.J.; Freedman, B.I.; Herrington, D.M.; Bowden, D.W. Heart rate-corrected QT interval is an independent predictor of all-cause and cardiovascular mortality in individuals with type 2 Diabetes: The diabetes heart study. Diabetes Care 2014, 37, 1454–1461. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Goldenberg, I.; Moss, A.J.; Zareba, W. QT interval: How to measure it and what is “normal”. J. Cardiovasc. Electrophysiol. 2006, 17, 333–336. [Google Scholar] [CrossRef] [PubMed]
- Park, C.S.; Cho, H.-J.; Choi, E.-K.; Lee, S.E.; Kim, M.-S.; Kim, J.-J.; Choi, J.-O.; Jeon, E.-S.; Hwang, K.-K.; Chae, S.C.; et al. J-curve relationship between corrected QT interval and mortality in acute heart failure patients. Korean J. Intern. Med. 2020. [Google Scholar] [CrossRef]
- Kolo, P.; Opadijo, O.; Omotoso, A.; Katibi, I.; Balogun, M.; Araoye, M. Prognostic Significance of Qt Interval Prolongation in Adult Nigerians with Chronic Heart Failure—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/19320406/ (accessed on 9 August 2020).
- Montanez, A.; Ruskin, J.N.; Hebert, P.R.; Lamas, G.A.; Hennekens, C.H. Prolonged QTc Interval and Risks of Total and Cardiovascular Mortality and Sudden Death in the General Population: A Review and Qualitative Overview of the Prospective Cohort Studies. Arch. Intern. Med. 2004, 164, 943–948. [Google Scholar] [CrossRef] [Green Version]
- Alexander, L.; Small, D.; Edwards, S.; Baric, R. An Experimental Model for Dilated Cardiomyopathy After Rabbit Coronavirus Infection. Available online: https://pubmed.ncbi.nlm.nih.gov/1309370/ (accessed on 6 July 2020).
- Edwards, S.; Small, J.; Geratz, J.; Alexander, L.; Baric, R. An Experimental Model for Myocarditis and Congestive Heart Failure After Rabbit Coronavirus Infection. J. Infect. Dis. 1992, 165, 134–140. [Google Scholar] [CrossRef] [Green Version]
- Szekely, Y.; Lichter, Y.; Taieb, P.; Banai, A.; Hochstadt, A.; Merdler, I.; Gal Oz, A.; Rothschild, E.; Baruch, G.; Peri, Y.; et al. The Spectrum of Cardiac Manifestations in Coronavirus Disease 2019 (COVID-19)—A Systematic Echocardiographic Study. Circulation 2020. [Google Scholar] [CrossRef]
- McElvaney, O.J.; McEvoy, N.; McElvaney, O.F.; Carroll, T.P.; Murphy, M.P.; Dunlea, D.M.; Ní Choileáin, O.; Clarke, J.; O’Connor, E.; Hogan, G.; et al. Characterization of the Inflammatory Response to Severe COVID-19 Illness. Am. J. Respir. Crit. Care Med. 2020. [Google Scholar] [CrossRef]
- Feng, X.; Li, S.; Sun, Q.; Zhu, J.; Chen, B.; Xiong, M.; Cao, G. Immune-Inflammatory Parameters in COVID-19 Cases: A Systematic Review and Meta-Analysis. Front. Med. 2020, 7. [Google Scholar] [CrossRef]
- Al-Khatib, S.M.; Allen LaPointe, N.M.; Kramer, J.M.; Califf, R.M. What Clinicians Should Know about the QT Interval. J. Am. Med. Assoc. 2003, 289, 2120–2127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- LaPointe, N.M.A.; Al-Khatib, S.M.; Kramer, J.M.; Califf, R.M. Knowledge deficits related to the QT interval could affect patient safety. Ann. Noninvasive Electrocardiol. 2003, 8, 157–160. [Google Scholar] [CrossRef] [PubMed]
- Burke, G.M.; Wang, N.; Blease, S.; Levy, D.; Magnani, J.W. Assessment of reproducibility—Automated and digital caliper ECG measurement in the Framingham Heart Study. J. Electrocardiol. 2014, 47, 288–293. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| QTc ≤ 480 (n = 562) | QTc > 480 (n = 61) | p-Value | Standardized Differences | |
|---|---|---|---|---|
| Women | 237 (42.2) | 30 (49.2) | 0.29 | 0.14107 |
| Age, years | 62.9 ± 16.9 | 76.6 ± 12.6 | <0.001 | −0.92172 |
| Diabetes | 88 (15.7) | 30 (49.2) | <0.001 | 0.76703 |
| Hypertension | 244 (43.4) | 46 (75.4) | <0.001 | 0.68911 |
| Dyslipidemia | 179 (31.9) | 33 (54.1) | <0.001 | 0.46121 |
| CV Risk factors | 360 (64.1) | 55 (90.2) | <0.001 | 0.65377 |
| Obesity | 97 (21.7) | 15 (28.8) | 0.239 | 0.16617 |
| Ischemic chronic disease | 36 (6.4) | 15 (24.6) | <0.001 | 0.51915 |
| Atrial fibrillation or flutter | 37 (6.6) | 15 (24.6) | <0.001 | 0.51245 |
| Heart failure | 20 (3.6) | 13 (21.3) | <0.001 | 0.55858 |
| Moderate to severe valve heart disease | 14 (2.5) | 9 (14.8) | <0.001 | 0.44769 |
| COPD | 42 (7.5) | 10 (16.4) | 0.017 | 0.27780 |
| Cancer | 64 (11.4) | 14 (23.0) | 0.010 | 0.31028 |
| CKD | 39 (6.9) | 18 (29.5) | <0.001 | 0.61132 |
| Peripheral vascular disease | 20 (3.6) | 7 (1.5) | 0.004 | 0.30370 |
| Stroke | 27 (4.8) | 8 (13.1) | 0.007 | 0.29411 |
| Systolic blood pressure, mmHg | 128.3 ± 19.0 | 130.4 ± 24.1 | 0.43 | −0.09693 |
| Diastolic blood pressure, mmHg | 77.1 ± 13.3 | 74.5 ± 16.4 | 0.23 | 0.17954 |
| Heart rate, bpm | 91.2 ± 18.0 | 88.3 ± 21.5 | 0.27 | 0.13995 |
| Respiratory rate, rpm | 24.5 ± 7.1 | 25.6 ± 7.1 | 0.37 | −0.15164 |
| Oxygen saturation, % | 95.1 ± 4.4 | 93.8 ± 6.1 | 0.13 | 0.23793 |
| Baseline FiO2, % | 25.9 ± 16.0 | 33.3 ± 25.4 | 0.033 | −0.34956 |
| PaO2/FiO2 < 300, n (%) | 180 (42.8) | 30 (60.0) | 0.020 | 0.35028 |
| Hemoglobin, g/dL | 13.6 ± 1.6 | 12.5 ± 2.0 | <0.001 | 0.59990 |
| White blood cell count, per µL | 7.04 ± 3.54 | 8.99 ± 4.76 | 0.003 | −0.46572 |
| Lymphocytes, per µL | 1.40 ± 2.2 | 1.74 ± 2.64 | 0.35 | −0.13720 |
| Platelet count | 209.0 ± 78.3 | 223.1 ± 109.0 | 0.33 | −0.14919 |
| Creatinine, mg/dL | 1.02 ± 0.56 | 1.66 ± 1.44 | 0.001 | −0.58761 |
| eGFR, mL/min/1.73 m2 | 83.0 ± 29.2 | 59.1 ± 32.0 | <0.001 | 0.77871 |
| Creatine phosphokinase, U/L | 93 (57–170) | 95 (47–290) | 0.97 | −0.18600 |
| Serum lactate, mmoL/L | 1.44 ± 0.67 | 1.76 ± 0.92 | 0.028 | −0.39636 |
| CRP, mg/dL | 9.4 ± 8.4 | 13.6 ± 11.0 | 0.005 | −0.43681 |
| Procalcitonin, ng/mL | 0.11 (0.08–0.21) | 0.22 (0.11–0.70) | <0.001 | 0.06087 |
| Lactate dehydrogenase, U/L | 309.9 ± 131.3 | 368.1 ± 159.1 | 0.003 | −0.39636 |
| D-dimer, ng/mL | 670 (430–1120) | 980 (650–1950) | <0.001 | −0.30192 |
| High sensitivity troponin T > 14 ng/L | 142 (30.7) | 42 (77.8) | <0.001 | 1.07117 |
| NT-proBNP, pg/mL | 157 (39–417) | 2065 (416–6780) | <0.001 | −0.68728 |
| Baseline QTc duration, milliseconds | 430.2 ± 23.5 | 505.4 ± 31.9 | <0.001 | −2.68874 |
| Abnormal chest radiography | 495 (88.7) | 54 (91.5) | 0.51 | 0.09446 |
| Alive (n = 549) | Dead (n = 74) | p-Value | Standardized Differences | |
|---|---|---|---|---|
| Women | 230 (41.9) | 37 (50.0) | 0.486 | 0.16319 |
| Age, years | 62.0 ± 16.6 | 81.2 ± 8.6 | <0.001 | −1.45609 |
| Diabetes | 90 (16.4) | 28 (37.8) | <0.001 | 0.49705 |
| Hypertension | 234 (42.6) | 56 (75.7) | <0.001 | 0.71397 |
| Dyslipidemia | 175 (31.9) | 37 (50.0) | 0.002 | 0.37500 |
| CV Risk factors | 345 (62.8) | 70 (94.6) | <0.001 | 0.95029 |
| Obesity | 96 (21.8) | 16 (26.7) | 0.40 | 0.11332 |
| Ischemic chronic disease | 31 (5.6) | 20 (27.0) | <0.001 | 0.60412 |
| Atrial fibrillation or flutter | 35 (6.4) | 17 (23.0) | <0.001 | 0.48252 |
| Heart failure | 18 (3.3) | 15 (20.3) | <0.001 | 0.54652 |
| Moderate to severe valve heart disease | 14 (2.6) | 9 (12.2) | <0.001 | 0.37460 |
| COPD | 38 (6.9) | 14 (18.9) | <0.001 | 0.36353 |
| Cancer | 61 (11.1) | 17 (23.0) | 0.004 | 0.31947 |
| CKD | 33 (6.0) | 24 (32.4) | <0.001 | 0.71171 |
| Peripheral vascular disease | 17 (3.1) | 10 (13.5) | <0.001 | 0.38439 |
| Stroke | 26 (4.7) | 9 (12.2) | 0.009 | 0.26943 |
| Systolic blood pressure, mmHg | 128.2 ± 18.6 | 130.8 ± 25.4 | 0.400 | −0.11696 |
| Diastolic blood pressure, mmHg | 77.4 ± 13.2 | 72.8 ± 16.1 | 0.022 | 0.31195 |
| Heart rate, bpm | 91.2 ± 17.9 | 88.5 ± 21.3 | 0.24 | 0.13723 |
| Respiratory rate, rpm | 24.1 ± 6.9 | 28.7 ± 7.1 | <0.001 | −0.66193 |
| Oxygen saturation, % | 95.2 ± 4.3 | 93.2 ± 5.9 | 0.006 | 0.38792 |
| Baseline FiO2, % | 25.1 ± 15.0 | 37.6 ± 26.7 | <0.001 | −0.57585 |
| PaO2/FiO2 < 300, n (%) | 165 (40.4) | 45 (71.4) | <0.001 | 0.65697 |
| Hemoglobin, g/dL | 13.6 ± 1.6 | 12.6 ± 2.1 | 0.006 | 0.57111 |
| White blood cell count, per µL | 6.86 ± 3.05 | 9.99 ± 6.26 | <0.001 | −0.63711 |
| Lymphocytes, per µL | 1.46 ± 2.33 | 1.24 ± 1.55 | 0.43 | 0.11148 |
| Platelet count | 210.8 ± 77.9 | 207.5 ± 107.3 | 0.80 | 0.03488 |
| Creatinine, mg/dL | 0.99 ± 0.49 | 1.72 ± 1.46 | <0.001 | −0.66936 |
| eGFR, mL/min/1.73 m2 | 84.0 ± 28.5 | 55.5 ± 31.9 | <0.001 | 0.94242 |
| Creatine phosphokinase, U/L | 91 (57–167) | 125 (49–290) | 0.28 | −0.33445 |
| Serum lactate, mmoL/L | 1.42 ± 0.66 | 1.79 ± 0.95 | 0.007 | −0.45164 |
| CRP, mg/dL | 8.89 ± 7.78 | 16.41 ± 12.35 | <0.001 | −0.72780 |
| Procalcitonin, ng/mL | 0.11 (0.08–0.20) | 0.26 (0.13–0.81) | <0.001 | 0.03618 |
| Lactate dehydrogenase, U/L | 1.42 ± 0.66 | 1.79 ± 0.95 | <0.001 | −0.66081 |
| D-dimer, ng/mL | 640 (420–1060) | 1190 (780–3570) | <0.001 | −0.47772 |
| High sensitivity troponin T > 14 ng/L | 135 (29.7) | 49 (79.0) | <0.001 | 1.13899 |
| NT-proBNP, pg/mL | 144 (39–367) | 1530 (550–4730) | <0.001 | −0.67258 |
| Baseline QTc duration, milliseconds | 434.0 ± 27.8 | 464.3 ± 51.9 | <0.001 | −0.72743 |
| QTc ≥ 480 ms | 36 (6.6) | 25 (33.8) | <0.001 | 0.72127 |
| Abnormal chest radiography | 481 (88.3) | 68 (94.4) | 0.115 | 0.22147 |
| No QTc Prolongation (n = 77) | QTc Prolongation (n = 168) | p-Value | |
|---|---|---|---|
| Women | 32 (41.6) | 61 (36.3) | 0.43 |
| Age, years | 62.1 ± 17.4 | 65.4 ± 15.0 | 0.14 |
| Diabetes | 10 (13) | 40 (23.8) | 0.051 |
| Hypertension | 32 (41.6) | 96 (57.1) | 0.023 |
| Dyslipidemia | 21 (27.3) | 65 (38.7) | 0.082 |
| Obesity | 13 (22.4) | 42 (28.8) | 0.36 |
| Ischemic chronic disease | 8 (10.4) | 14 (8.3) | 0.60 |
| Atrial fibrillation or flutter | 7 (9.1) | 23 (13.7) | 0.31 |
| Heart failure | 4 (5.2) | 10 (6.0) | 0.54 |
| Moderate to severe valve heart disease | 2 (2.6) | 6 (3.6) | 0.54 |
| COPD | 4 (5.2) | 21 (12.5) | 0.058 |
| Cancer | 13 (16.9) | 29 (17.3) | 0.94 |
| CKD | 5 (5.2) | 14 (8.3) | 0.28 |
| Peripheral vascular disease | 7 (9.1) | 5 (3.0) | 0.04 |
| Stroke | 2 (2.6) | 13 (7.7) | 0.097 |
| Systolic blood pressure, mmHg | 123.0 ± 18.8 | 128.4 ± 19.6 | 0.074 |
| Diastolic blood pressure, mmHg | 76.2 ± 14.7 | 75.2 ± 14.0 | 0.60 |
| Heart rate, bpm | 89.0 ± 15.0 | 91.2 ± 20.6 | 0.35 |
| Respiratory rate, rpm | 24.4 ± 6.4 | 26.2 ± 7.8 | 0.13 |
| Oxygen saturation, % | 95.9 ± 2.9 | 93.2 ± 6.3 | <0.001 |
| Baseline FiO2, % | 24.9 ± 14.3 | 30.4 ± 22.3 | 0.022 |
| PaO2/FiO2 < 300, n (%) | 12 (21.4) | 82 (58.2) | <0.001 |
| Hemoglobin, g/dL | 13.4 ± 1.5 | 13.6 ± 1.7 | 0.36 |
| White blood cell count, per µL | 6.3 ± 2.2 | 7.8 ± 3.6 | <0.001 |
| Lymphocytes, per µL | 1.56 ± 2.60 | 1.37 ± 1.81 | 0.51 |
| Platelet count | 205.1 ± 72.6 | 202.6 ± 75.0 | 0.81 |
| Creatinine, mg/dL | 1.04 ± 0.51 | 1.15 ± 0.73 | 0.26 |
| eGFR, mL/min/1.73 m2 | 81.1 ± 28.9 | 77.3 ± 29.7 | 0.34 |
| Creatine phosphokinase, U/L | 82 (50–156) | 108 (63–181) | 0.051 |
| Serum lactate, mmoL/L | 1.35 ± 0.59 | 1.55 ± 0.70 | 0.04 |
| CRP, mg/dL | 8.5 ± 7.7 | 11.6 ± 9.7 | 0.009 |
| Procalcitonin, ng/mL | 0.12 (0.07–0.17) | 0.13 (0.08–0.25) | 0.31 |
| Lactate dehydrogenase, U/L | 293.0 ± 92.5 | 348.8 ± 151.2 | 0.01 |
| D-dimer, ng/mL | 630 (410–940) | 760 (470–1240) | 0.027 |
| High sensitivity troponin T > 14 ng/L | 20 (33.9) | 60 (41.4) | 0.34 |
| NT-proBNP, pg/mL | 145 (42–303) | 246 (76–756) | 0.014 |
| Baseline QTc duration, milliseconds | 441.8 ± 38.5 | 435.38 ± 31.6 | 0.17 |
| Baseline QTc ≥ 480 ms | 8 (10.4) | 20 (11.9) | 0.73 |
| Abnormal chest radiography | 69 (90.8) | 156 (92.9) | 0.58 |
| Tocilizumab | 14 (18.2) | 54 (32.1) | 0.023 |
| No hydroxychloroquine or azithromycin | 6 (7.8) | 1 (0.6) | 0.015 |
| Hydroxychloroquine alone | 2 (2.6) | 1 (1.8) | |
| Azithromycin alone | 1 (1.3) | 1 (0.6) | |
| Hydroxychloroquine + Azithromycin | 68 (88.3) | 163 (97.0) | |
| Oxygen support | 46 (59.7) | 91 (54.2) | <0.001 |
| High Flow Nasal Cannula | 2 (2.6) | 5 (3.0) | |
| Non-invasive ventilation | 1 (1.3) | 16 (9.5) | |
| Intubation and invasive ventilation | 1 (1.3) | 37 (22.0) | |
| Longest QTc duration, milliseconds | 440.4 ± 37.9 | 476.3 ± 48.9 | <0.001 |
| Length of hospitalization, days | 10 (6–18) | 17 (9–29.5) | <0.001 |
| Dead | 5 (6.5) | 25 (14.9) | 0.045 |
| QTc ≤ 480 (n = 562) | QTc > 480 (n = 61) | p-Value | |
|---|---|---|---|
| Tocilizumab | 94 (16.7) | 11 (18.0) | 0.80 |
| No hydroxychloroquine or azithromycin | 9 (1.6) | 7 (11.5) | <0.001 |
| Hydroxychloroquine | 15 (2.7) | 1 (1.6) | |
| Azithromycin | 7 (1.2) | 3 (4.9) | |
| Hydroxychloroquine + Azithromycin | 531 (94.5) | 50 (82.0) | |
| Oxygen support | 337 (60.0) | 40 (65.6) | 0.12 |
| High Flow Nasal Cannula | 9 (1.6) | 1 (1.6) | |
| Non-invasive ventilation | 27 (4.8) | 3 (4.9) | |
| Intubation and invasive ventilation | 36 (6.4) | 8 (13.1) | |
| QTc prolongation during hospitalization | 148 (68.2) | 20 (71.4) | 0.73 |
| Longest QTc duration, milliseconds | 455.8 ± 40.5 | 536.5 ± 47.8 | <0.001 |
| Length of hospitalization, days | 10 (5–19) | 10 (3–23) | 0.68 |
| Death | 49 (8.7) | 25 (41.0) | <0.001 |
| Alive (n = 549) | Dead (n = 74) | p-Value | |
|---|---|---|---|
| Tocilizumab | 96 (17.5) | 9 (12.2) | 0.25 |
| No hydroxychloroquine or azithromycin | 9 (1.6) | 7 (9.5) | <0.001 |
| Hydroxychloroquine | 12 (2.2) | 4 (5.4) | |
| Azithromycin | 6 (1.1) | 4 (5.4) | |
| Hydroxychloroquine + Azithromycin | 522 (95.1) | 59 (79.7) | |
| Oxygen support | 324 (59.0) | 53 (71.6) | <0.001 |
| High Flow Nasal Cannula | 9 (1.6) | 1 (1.4) | |
| Non-invasive ventilation | 20 (3.6) | 8 (10.8) | |
| Intubation and invasive ventilation | 33 (6.0) | 11 (14.9) | |
| QTc prolongation during hospitalization | 143 (66.5) | 25 (83.3) | 0.045 |
| Longest QTc duration, milliseconds | 460.3 ± 45.3 | 499.0 ± 58.2 | <0.001 |
| Length of hospitalization, days | 10 (5–20) | 6 (3–16) | 0.007 |
| Univariate HR (95%CI) | Adjusted HR (95%CI) * | |
|---|---|---|
| Age (per every year) | 1.01 (1.08–1.12), p < 0.001 | 1.08 (1.06–1.11), p < 0.001 |
| Baseline QTc > 480 ms | 4.87 (2.98–7.96), p < 0.001 | 2.68 (1.58–4.55), p < 0.001 |
| Chronic kidney disease | 6.07 (3.70–10.05), p < 0.001 | 2.62 (1.55–4.46), p < 0.001 |
| Treatment with azithromycin and hydroxychloroquine | 0.12 (0.05–0.26), p < 0.001 | 0.31 (0.13–0.72), p = 0.007 |
| Ischemic chronic disease | 3.60 (2.13–6.09), p < 0.001 | - |
| Atrial fibrillation or flutter | 3.04 (1.74–5.30), p < 0.001 | - |
| Heart failure | 5.43 (3.05–9.66), p < 0.001 | - |
| Any cardiovascular risk factor | 7.09 (2.58–19.45), p < 0.001 | - |
| Baseline ECG (n = 623) | Without Baseline ECG (n = 249) | p-Value | |
|---|---|---|---|
| Women | 267 (42.9) | 119 (47.8) | 0.19 |
| Age, years | 64.2 ± 17.0 | 57.3 ± 19.6 | <0.001 |
| Diabetes | 118 (18.9) | 55 (22.19) | 0.29 |
| Hypertension | 290 (46.5) | 93 (37.3) | 0.013 |
| Dyslipidemia | 69 (27.7) | 212 (34.0) | 0.07 |
| Any CV risk factor | 415 (66.6) | 150 (60.2) | 0.08 |
| Obesity | 112 (22.4) | 46 (21.8) | 0.86 |
| Ischemic chronic disease | 51 (8.2) | 9 (3.6) | 0.016 |
| Atrial fibrillation or flutter | 52 (8.3) | 18 (7.2) | 0.58 |
| Heart failure | 33 (5.3) | 10 (4.0) | 0.43 |
| Moderate to severe valve heart disease | 23 (3.7) | 6 (2.4) | 0.34 |
| COPD | 52 (8.3) | 14 (5.6) | 0.17 |
| Cancer | 78 (12.5) | 33 (13.3) | 0.77 |
| CKD | 57 (9.1) | 18 (7.2) | 0.36 |
| Peripheral vascular disease | 27 (4.3) | 7 (2.8) | 0.29 |
| Stroke | 35 (5.6) | 16 (6.4) | 0.65 |
| Systolic blood pressure, mmHg | 128.5 ± 19.5 | 129.1 ± 19.4 | 0.68 |
| Diastolic blood pressure, mmHg | 76.9 ± 13.7 | 76.5 ± 13.5 | 0.72 |
| Heart rate, bpm | 90.9 ± 18.4 | 89.4 ± 16.4 | 0.27 |
| Respiratory rate, rpm | 24.6 ± 7.1 | 22.4 ± 8.2 | 0.011 |
| Oxygen saturation, % | 95.1 ± 4.4 | 93.8 ± 6.1 | 0.13 |
| Baseline FiO2, % | 26.6 ± 17.2 | 24.9 ± 8.2 | 0.42 |
| PaO2/FiO2 < 300, n (%) | 210 (44.6) | 41 (41.4) | 0.56 |
| Hemoglobin, g/dL | 13.5 ± 1.7 | 13.4 ± 1.8 | 0.34 |
| White blood cell count, per µL | 7.23 ± 3.7 | 6.31 ± 2.8 | 0.001 |
| Lymphocytes, per µL | 1.44 ± 2.26 | 1.48 ± 1.18 | 0.71 |
| Platelet count | 210.4 ± 81.8 | 220.5 ± 86.5 | 0.13 |
| Creatinine, mg/dL | 1.08 ± 0.72 | 0.95 ± 0.46 | 0.002 |
| eGFR, mL/min/1.73 m2 | 80.7 ± 30.3 | 88.3 ± 32.4 | 0.003 |
| Creatine phosphokinase, U/L | 93 (57–175) | 78 (50–151) | 0.079 |
| Serum lactate, mmoL/L | 1.3 (1.03–1.67) | 1.25 (0.93–1.6) | 0.16 |
| CRP, mg/dL | 7.3 (3.1–14.1) | 4.0 (1.5–9.3) | <0.001 |
| Procalcitonin, ng/mL | 0.12 (0.08–0.24) | 0.09 (0.05–0.20) | <0.001 |
| Lactate dehydrogenase, U/L | 315.9 ± 135.1 | 295.6 ± 160.6 | 0.15 |
| D-dimer, ng/mL | 690 (440–1190) | 610 (370–910) | 0.004 |
| High sensitivity troponin T > 14 ng/L | 184 (35.7) | 41 (30.4) | 0.25 |
| NT-proBNP, pg/mL | 180 (48–540) | 97 (25–346) | 0.013 |
| Abnormal chest radiography | 549 (89.0) | 161 (72.2) | <0.001 |
| Tocilizumab | 105 (16.9) | 14 (5.6) | <0.001 |
| No hydroxychloroquine or azithromycin | 16 (2.6) | 60 (24.1) | <0.001 |
| Hydroxychloroquine | 16 (2.6) | 11 (4.4) | |
| Azithromycin | 10 (1.6) | 11 (4.4) | |
| Hydroxychloroquine + Azithromycin | 581 (93.3) | 167 (67.1) | |
| Oxygen support | 377 (60.5) | 78 (31.3) | <0.001 |
| High Flow Nasal Cannula | 10 (1.6) | 3 (1.2) | |
| Non-invasive ventilation | 28 (4.5) | 4 (1.6) | |
| Intubation and invasive ventilation | 44 (7.1) | 11 (4.4) | |
| Length of hospitalization, days | 10 (5–19) | 8 (1–17) | <0.001 |
| Death | 74 (11.9) | 27 (10.8) | 0.66 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Farré, N.; Mojón, D.; Llagostera, M.; Belarte-Tornero, L.C.; Calvo-Fernández, A.; Vallés, E.; Negrete, A.; García-Guimaraes, M.; Bartolomé, Y.; Fernández, C.; et al. Prolonged QT Interval in SARS-CoV-2 Infection: Prevalence and Prognosis. J. Clin. Med. 2020, 9, 2712. https://doi.org/10.3390/jcm9092712
Farré N, Mojón D, Llagostera M, Belarte-Tornero LC, Calvo-Fernández A, Vallés E, Negrete A, García-Guimaraes M, Bartolomé Y, Fernández C, et al. Prolonged QT Interval in SARS-CoV-2 Infection: Prevalence and Prognosis. Journal of Clinical Medicine. 2020; 9(9):2712. https://doi.org/10.3390/jcm9092712
Chicago/Turabian StyleFarré, Núria, Diana Mojón, Marc Llagostera, Laia C. Belarte-Tornero, Alicia Calvo-Fernández, Ermengol Vallés, Alejandro Negrete, Marcos García-Guimaraes, Yolanda Bartolomé, Camino Fernández, and et al. 2020. "Prolonged QT Interval in SARS-CoV-2 Infection: Prevalence and Prognosis" Journal of Clinical Medicine 9, no. 9: 2712. https://doi.org/10.3390/jcm9092712
APA StyleFarré, N., Mojón, D., Llagostera, M., Belarte-Tornero, L. C., Calvo-Fernández, A., Vallés, E., Negrete, A., García-Guimaraes, M., Bartolomé, Y., Fernández, C., García-Duran, A. B., Marrugat, J., & Vaquerizo, B. (2020). Prolonged QT Interval in SARS-CoV-2 Infection: Prevalence and Prognosis. Journal of Clinical Medicine, 9(9), 2712. https://doi.org/10.3390/jcm9092712





