Epidemiology and Comorbidities of Excoriation Disorder: A Retrospective Case-Control Study
Abstract
:1. Introduction
2. Experimental Section
3. Results
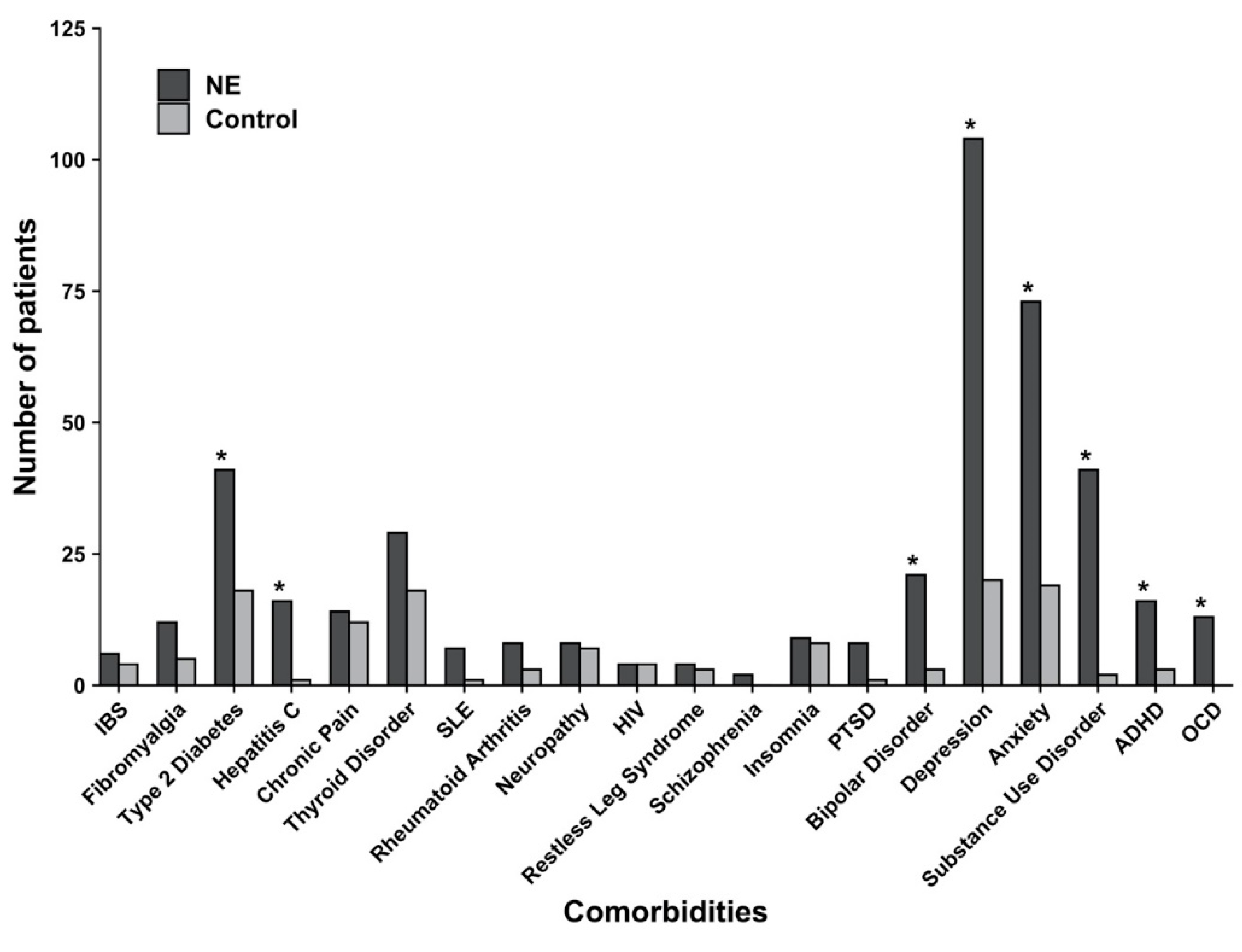
3.1. Comorbidities Associated with Excoriation Disorder
3.2. Clinical Features and Treatment Patterns of Excoriation Disorder
3.3. Outcomes of Excoriation Disorder
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Arnold, L.M.; Auchenbach, M.B.; McElroy, S.L. Psychogenic excoriation. Clinical features, proposed diagnostic criteria, epidemiology and approaches to treatment. CNS Drugs 2001, 15, 351–359. [Google Scholar] [CrossRef] [PubMed]
- Mutasim, D.F.; Adams, B.B. The psychiatric profile of patients with psychogenic excoriation. J. Am. Acad. Dermatol. 2009, 61, 611–613. [Google Scholar] [CrossRef] [PubMed]
- Brodin, M.B. Neurotic excoriations. J. Am. Acad. Dermatol. 2009, 63, 341–342. [Google Scholar] [CrossRef] [PubMed]
- Gieler, U.; Consoli, S.G.; Tomás-Aragones, L.; Linder, D.M.; Jemec, G.B.E.; Poot, F.; Szepietowski, J.C.; De Korte, J.; Taube, K.M.; Lvov, A.; et al. Self-inflicted lesions in dermatology: Terminology and classification—A position paper from the European Society for Dermatology and Psychiatry (ESDaP). Acta Dermeto Venereol. 2013, 93, 4–12. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilhelm, S.; Keuthen, N.J.; Deckersbach, T.; Engelhard, I.M.; Forker, A.E.; Baer, L.; O’Sullivan, R.L.; Jenike, M.A. Self-injurious skin picking: Clinical characteristics and comorbidity. J. Clin. Psychiatry 1999, 60, 454–459. [Google Scholar] [CrossRef]
- Hayes, S.L.; Storch, E.A.; Berlanga, L. Skin picking behaviors: An examination of the prevalence and severity in a community sample. J. Anxiety Disord. 2009, 23, 314–319. [Google Scholar] [CrossRef] [Green Version]
- Keuthen, N.J.; Koran, L.M.; Aboujaoude, E.; Large, M.D.; Serpe, R.T. The prevalence of pathologic skin picking in US adults. Compr. Psychiatry 2010, 51, 183–186. [Google Scholar] [CrossRef]
- Leibovici, V.; Koran, L.M.; Murad, S.; Siam, I.; Odlaug, B.; Mandelkorn, U.; Feldman-Weisz, V.; Keuthen, N.J. Excoriation (skin-picking) disorder in adults: A cross-cultural survey of Israeli Jewish and Arab samples. Compr. Psychiatry 2015, 58, 102–107. [Google Scholar] [CrossRef]
- Torales, J.; Díaz, N.R.; Barrios, I.; Navarro, R.; García, O.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A.; Jafferany, M. Psychodermatology of skin picking (excoriation disorder): A comprehensive review. Dermatol. Ther. 2020. [Google Scholar] [CrossRef]
- Jones, G.; Keuthen, N.; Greenberg, E. Assessment and treatment of trichotillomania (hair pulling disorder) and excoriation (skin picking) disorder. Clin. Dermatol. 2018, 36, 728–736. [Google Scholar] [CrossRef]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; DSM-5; American Psychiatric Association: Arlington, TX, USA, 2013. [Google Scholar]
- Arnold, L.M.; McElroy, S.L.; Mutasim, D.F.; Dwight, M.M.; Lamerson, C.L.; Morris, E.M. Characteristics of 34 adults with psychogenic excoriation. J. Clin. Psychiatry 1998, 59, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Yalçin, M.; Tellioğlu, E.; Yildirim, D.U.; Savrun, B.M.; Özmen, M.; Aydemir, E.H. Psychiatric Features in Neurotic Excoriation Patients: The Role of Childhood Trauma. Noro Psikiyatri Arşivi 2015, 52, 336–341. [Google Scholar]
- Jafferany, M.; Stoep, A.V.; Dumitrescu, A.; Hornung, R.L. The knowledge, awareness, and practice patterns of dermatologists toward psychocutaneous disorders: Results of a survey study. Int. J. Dermatol. 2010, 49, 784–789. [Google Scholar] [CrossRef]
- Ruxton, G.D.; Neuhäuser, M. Review of alternative approaches to calculation of a confidence interval for the odds ratio of a 2 × 2 contingency table. Methods Ecol. Evol. 2012, 4, 9–13. [Google Scholar] [CrossRef]
- Benjamini, Y.; Hochberg, Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to Multiple Testing. J. Royal Stat. Soc. Ser. B (Methodol.) 1995, 57, 289–300. [Google Scholar] [CrossRef]
- Claréus, B.; Renström, E.A. Physicians’ gender bias in the diagnostic assessment of medically unexplained symptoms and its effect on patient–physician relations. Scand. J. Psychol. 2019, 60, 338–347. [Google Scholar] [CrossRef]
- Smith, E.C. Gender-biased Diagnosing, the Consequences of Psychosomatic Misdiagnosis and ‘Doing Credibility; Occidental College Sociology Student Scholarship: Los Angeles, CA, USA, 2011. [Google Scholar]
- Walther, M.R.; Flessner, C.A.; Conelea, C.A.; Woods, D.W. The Milwaukee Inventory for the Dimensions of Adult Skin Picking (MIDAS): Initial development and psychometric properties. J. Behav. Ther. Exp. Psychiatry 2009, 40, 127–135. [Google Scholar] [CrossRef]
- Flessner, C.A.; Woods, D.W.; Franklin, M.E.; Keuthen, N.J.; Piacentini, J. Styles of pulling in youths with trichotillomania: Exploring differences in symptom severity, phenomenology, and comorbid psychiatric symptoms. Behav. Res. Ther. 2008, 46, 1055–1061. [Google Scholar] [CrossRef]
- Khopkar, U.; Pande, S. Etiopathogenesis of pruritus due to systemic causes: Implications for treatment. Indian J. Dermatol. Venereol. Leprol. 2007, 73, 215–217. [Google Scholar] [CrossRef]
- Jafferany, M.; Stoep, A.V.; Dumitrescu, A.; Hornung, R.L. Psychocutaneous disorders: A survey study of psychiatrists’ awareness and treatment patterns. South. Med. J. 2010, 103, 1199–1203. [Google Scholar] [CrossRef]
- Simeon, D.; Stein, D.J.; Gross, S.; Islam, N.; Schmeidler, J.; Hollander, E. A double-blind trial of fluoxetine in pathologic skin picking. J. Clin. Psychiatry 1997, 58, 341–347. [Google Scholar] [CrossRef] [PubMed]
- Bloch, M.R.; Elliott, M.; Thompson, H.; Koran, L.M. Fluoxetine in pathologic skin-picking: Open-label and double-blind results. Psychosomatics 2001, 42, 314–319. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grant, J.E.; Odlaug, B.L.; Chamberlain, S.R.; Kim, S.W. A double-blind, placebo-controlled trial of lamotrigine for pathological skin picking: Treatment efficacy and neurocognitive predictors of response. J. Clin. Psychopharmacol. 2010, 30, 396–403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Keuthen, N.J.; Jameson, M.; Loh, R.; Deckersbach, T.; Wilhelm, S.; Dougherty, D.D. Open-label escitalopram treatment for pathological skin picking. Int. Clin. Psychopharmacol. 2007, 22, 268–274. [Google Scholar] [CrossRef]
- Selles, R.R.; Mcguire, J.F.; Small, B.J.; Storch, E.A. A systematic review and meta-analysis of psychiatric treatments for excoriation (skin-picking) disorder. Gen. Hosp. Psychiatry 2016, 41, 29–37. [Google Scholar] [CrossRef]
- Odlaug, B.L.; Hampshire, A.; Chamberlain, S.R.; Grant, J.E. Abnormal brain activation in excoriation (skin-picking) disorder: Evidence from an executive planning fMRI study. Br. J. Psychiatry 2016, 208, 168–174. [Google Scholar] [CrossRef] [Green Version]
- Harries, M.D.; Chamberlain, S.R.; Redden, S.A.; Odlaug, B.L.; Blum, A.W.; Grant, J.E. A structural MRI study of excoriation (skin-picking) disorder and its relationship to clinical severity. Psychiatry Res. Neuroimaging 2017, 269, 26–30. [Google Scholar] [CrossRef] [Green Version]
- Grant, J.E.; Chamberlain, S.R.; Redden, S.A.; Leppink, E.W.; Odlaug, B.L.; Kim, S.W. N-Acetylcysteine in the Treatment of Excoriation Disorder: A Randomized Clinical Trial. JAMA Psychiatry 2016, 73, 490–496. [Google Scholar] [CrossRef] [Green Version]
- Lochner, C.; Roos, A.; Stein, D.J. Excoriation (skin-picking) disorder: A systematic review of treatment options. Neuropsychiatr. Dis. Treat. 2017, 13, 1867–1872. [Google Scholar] [CrossRef] [Green Version]
| Patient Characteristics | All Patients | Resolution of Disease, n (%) | Improvement of Disease, n (%) | No Change or Worsened, n (%) |
|---|---|---|---|---|
| Number of patients | 250 | 11 (4) | 42 (17) | 91 (36) |
| Sex, n (%) | ||||
| Female | 190 (76) | 7 (4) | 35 (18) | 70 (37) |
| Male | 60 (24) | 4 (7) | 7 (12) | 21 (35) |
| Race, n (%) | ||||
| Caucasian | 204 (82) | 8 (4) | 35 (17) | 73 (36) |
| Black | 34 (14) | 2 (6) | 6 (18) | 15 (44) |
| Other | 7 (3) | 0 | 0 | 2 (2) |
| Asian | 5 (2) | 1 (9) | 1 (2) | 1 (1) |
| Marital Status, n (%) | ||||
| Single | 110 (44) | 7 (6) | 14 (13) | 40 (36) |
| Married | 83 (33) | 2 (2) | 13 (16) | 31 (37) |
| Divorced/Separated | 29 (12) | 2 (7) | 7 (24) | 10 (34) |
| Widowed | 15 (6) | 0 (0) | 5 (33) | 5 (33) |
| Employment Status, n (%) | ||||
| Unemployed | 119 (48) | 5 (4) | 20 (17) | 50 (42) |
| Disease Characteristics | ||||
| Duration (years), mean ± SD | 2.9 ± 0.4 (n = 224) | 3.1 ± 1.3 (n = 11, 5%) | 5.4 ± 2.0 (n = 36, 16%) | 1.7 ± 0.3 (n = 78, 35%) |
| Patient Characteristics/Diseases | Excoriation Disorder (n = 250) | Control (n = 250) | Odds Ratio (95% CI) | Adjusted p-Value |
|---|---|---|---|---|
| Age (years), mean ± SD | 49 ± 16 | 49 ± 16 | --- | --- |
| Sex, n (%) | ||||
| Male | 60 (24) | 60 (24) | --- | --- |
| Female | 190 (76) | 190 (76) | --- | --- |
| Race/Ethnicity, n (%) | ||||
| Caucasian | 204 (82) | 204 (82) | --- | --- |
| Black | 34 (14) | 34 (14) | --- | --- |
| Asian | 5 (2) | 5 (2) | --- | --- |
| Other | 7 (3) | 7 (3) | --- | --- |
| Medical Comorbidities, n (%) | ||||
| IBS | 6 (2) | 4 (2) | 1.51 (0.42, 5.43) | 0.939 |
| Fibromyalgia | 12 (5) | 5 (2) | 2.47 (0.86, 7.12) | 0.228 |
| Type 2 Diabetes | 41 (16) | 18 (7) | 2.53 (1.41, 4.54) | 0.006 |
| Hepatitis C | 16 (6) | 1 (0.4) | 17.03 (2.24, 129.40) | <0.001 |
| Chronic Pain | 14 (6) | 12 (5) | 1.18 (0.53, 2.60) | 0.916 |
| Thyroid Disorder | 29 (12) | 18 (7) | 1.69 (0.91, 3.13) | 0.167 |
| SLE | 7 (3) | 1 (0.4) | 7.17 (0.88, 58.73) | 0.136 |
| Rheumatoid Arthritis | 8 (3) | 3 (1) | 2.72 (0.71, 10.38) | 0.340 |
| Neuropathy | 8 (3) | 7 (3) | 1.15 (0.41, 3.21) | 0.933 |
| HIV | 4 (2) | 4 (2) | 1 (0.25, 4.04) | 1.000 |
| Restless Leg Syndrome | 4 (2) | 3 (1) | 1.34 (0.30, 6.04) | 1.000 |
| Psychiatric Comorbidities, n (%) | ||||
| Schizophrenia | 2(1) | 0 (0) | 5.04 (0.24, 105.52) * | 0.713 |
| Insomnia | 9 (4) | 8 (3) | 1.13 (0.43, 2.98) | 1.000 |
| PTSD | 8 (3) | 1 (0.4) | 8.23 (1.02, 66.31) | 0.082 |
| Bipolar Disorder | 21 (8) | 3 (1) | 7.55 (2.22, 25.65) | 0.002 |
| Depression | 104 (42) | 20 (8) | 8.19 (4.86, 13.80) | 0.002 |
| Anxiety | 73 (29) | 19 (8) | 5.01 (2.92, 8.62) | 0.002 |
| Substance Use Disorder | 41 (16) | 2 (1) | 24.33 (5.81, 101.77) | <0.001 |
| ADHD | 16 (6) | 3 (1) | 5.63 (1.62, 19.57) | 0.010 |
| OCD | 13 (5) | 0 (0) | 28.48 (1.68, 481.75) * | <0.001 |
| Clinical Characteristics | Number of ED patients (%) |
|---|---|
| Reported pruritus | 176 (71) |
| Lesion Location | |
| Scalp | 22 (9) |
| Face | 112 (45) |
| Trunk | 147 (59) |
| Upper extremities | 158 (63) |
| Lower extremities | 128 (51) |
| Complications | |
| Ulceration | 49 (20) |
| Infection | 23 (9) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kwon, C.; Sutaria, N.; Khanna, R.; Almazan, E.; Williams, K.; Kim, N.; Elmariah, S.; Kwatra, S.G. Epidemiology and Comorbidities of Excoriation Disorder: A Retrospective Case-Control Study. J. Clin. Med. 2020, 9, 2703. https://doi.org/10.3390/jcm9092703
Kwon C, Sutaria N, Khanna R, Almazan E, Williams K, Kim N, Elmariah S, Kwatra SG. Epidemiology and Comorbidities of Excoriation Disorder: A Retrospective Case-Control Study. Journal of Clinical Medicine. 2020; 9(9):2703. https://doi.org/10.3390/jcm9092703
Chicago/Turabian StyleKwon, Christina, Nishadh Sutaria, Raveena Khanna, Erik Almazan, Kyle Williams, Noori Kim, Sarina Elmariah, and Shawn G. Kwatra. 2020. "Epidemiology and Comorbidities of Excoriation Disorder: A Retrospective Case-Control Study" Journal of Clinical Medicine 9, no. 9: 2703. https://doi.org/10.3390/jcm9092703
APA StyleKwon, C., Sutaria, N., Khanna, R., Almazan, E., Williams, K., Kim, N., Elmariah, S., & Kwatra, S. G. (2020). Epidemiology and Comorbidities of Excoriation Disorder: A Retrospective Case-Control Study. Journal of Clinical Medicine, 9(9), 2703. https://doi.org/10.3390/jcm9092703





