Tunnel/Pouch versus Coronally Advanced Flap Combined with a Connective Tissue Graft for the Treatment of Maxillary Gingival Recessions: Four-Year Follow-Up of a Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
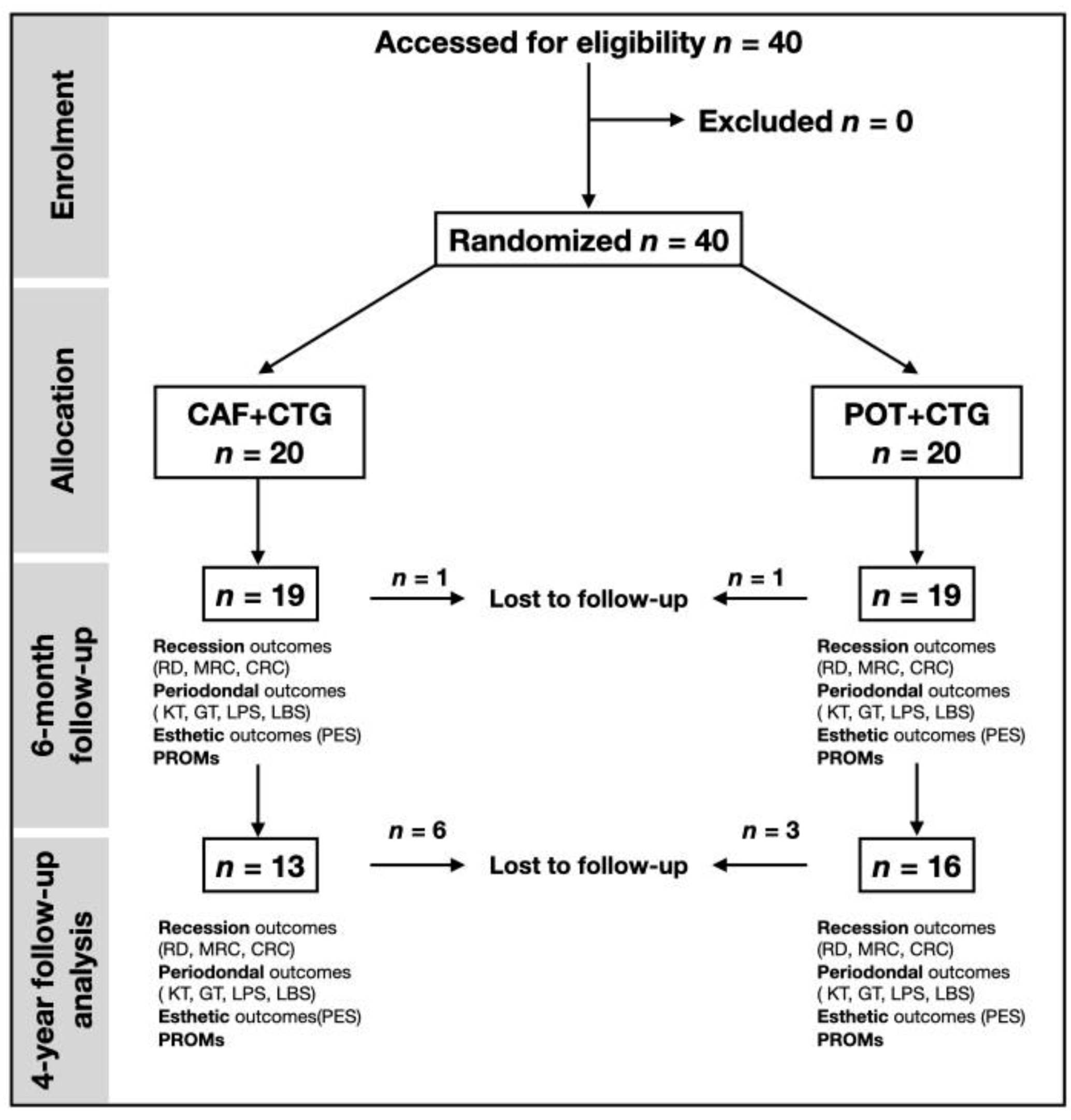
2.1. Study Design
2.2. Study Population
- Miller’s class I recessions;
- Recession of 2 mm to 5 mm;
- Maxillary incisors, canines or premolars;
- Identifiable cementoenamel junction (CEJ);
- Patients were at least 18 years old;
- No/controlled periodontal disease;
- ASA1 or ASA2 (American Society of Anesthesiologists) general health status;
- Providing a signed informed consent form.
- Smokers;
- Presence of cervical carious lesion;
- Pocket depth greater than 4 mm;
- Sites where previous muco-gingival therapy was performed;
- Pregnancy.
2.3. Patient Inclusion (Informed Consent, Patient Registration and Randomization)
2.4. Surgical Procedure
2.5. Post-Operative Instructions and Follow-Up
2.6. Data Collection
2.7. Statistical Analysis
3. Results
3.1. Patient Characteristics
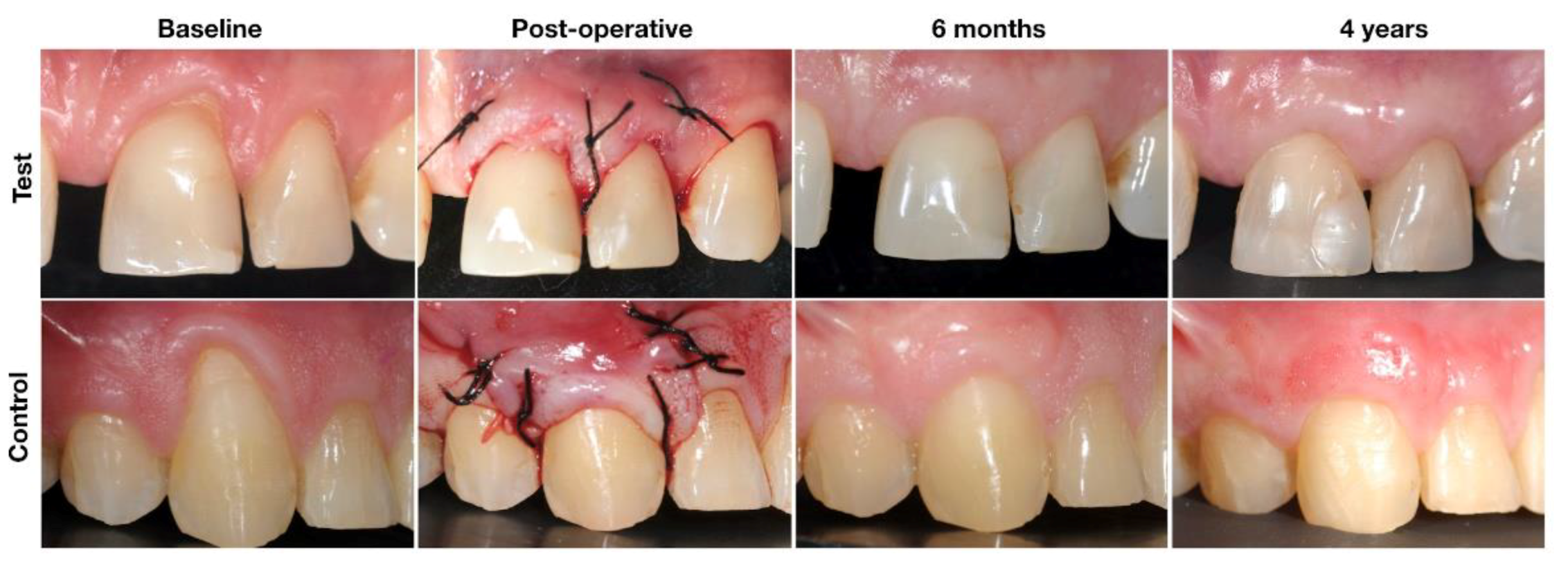
3.2. Recession Coverage
3.3. Gain of Keratinized Tissue
3.4. Gingival Thickness
3.5. Pink Esthetic Score
3.6. Patient-Related Esthetic Outcomes
4. Discussion
4.1. Mean Root Coverage (MRC)
4.2. Complete Root Coverage (CRC)
4.3. Keratinized Tissue (KT) and Gingival Thickness (GT)
4.4. Esthetic Outcomes
4.5. Additional Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gartrell, J.R.; Mathews, D.P. Gingival recession. The condition, process, and treatment. Dent. Clin. N. Am. 1976, 20, 199–213. [Google Scholar]
- Gorman, W.J. Prevalence and etiology of gingival recession. J Periodontol. 1967, 38, 316–322. [Google Scholar] [CrossRef]
- Winders, R.V. Gingival recession of mandibular incisors related to malocclusions of the teeth. J. Wis. State Dent. Soc. 1971, 47, 339–343. [Google Scholar]
- Al-Wahadni, A.; Linden, G.J. Dentine hypersensitivity in Jordanian dental attenders: A case control study. J. Clin. Periodontol. 2002, 29, 688–693. [Google Scholar] [CrossRef] [PubMed]
- Joshipura, K.J.; Kent, R.L.; De Paola, P.F. Gingival recession: Intra-oral distribution and associated factors. J. Periodontol. 1994, 65, 864–871. [Google Scholar] [CrossRef] [PubMed]
- Kassab, M.M.; Cohen, R.E. Treatment of gingival recession. J. Am. Dent. Assoc. 2002, 133, 1499–1506. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, H.C.; Atkins, J.H. Free autogenous gingival grafts. 3. Utilization of grafts in the treatment of gingival recession. Periodontics 1968, 6, 152–160. [Google Scholar] [PubMed]
- Allen, E.P.; Miller, P.D. Coronal positioning of existing gingiva: Short term results in the treatment of shallow marginal tissue recession. J. Periodontol. 1989, 60, 316–319. [Google Scholar] [CrossRef] [PubMed]
- Bernimoulin, J.P.; Lüscher, B.; Mühlemann, H.R. Coronally repositioned periodontal flap. Clinical evaluation after one year. J. Clin. Periodontol. 1975, 2, 1–13. [Google Scholar] [CrossRef]
- Cairo, F.; Nieri, M.; Pagliaro, U. Efficacy of periodontal plastic surgery procedures in the treatment of localized facial gingival recessions. A systematic review. J. Clin. Periodontol. 2014, 41, S44–S62. [Google Scholar] [CrossRef]
- Chambrone, L.; Tatakis, D.N. Periodontal soft tissue root coverage procedures: A systematic review from the AAP Regeneration Workshop. J. Periodontol. 2015, 86, S8–S51. [Google Scholar] [CrossRef] [PubMed]
- Langer, B.; Langer, L. Subepithelial connective tissue graft technique for root coverage. J. Periodontol. 1985, 56, 715–720. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.J.; Solt, C.W. A surgical procedure for the treatment of localized gingival recession in conjunction with root surface citric acid conditioning. J. Periodontol. 1980, 51, 505–509. [Google Scholar] [CrossRef] [PubMed]
- Cairo, F.; Pagliaro, U.; Nieri, M. Treatment of gingival recession with coronally advanced flap procedures: A systematic review. J. Clin. Periodontol. 2008, 35, 136–162. [Google Scholar] [CrossRef] [PubMed]
- Dodge, A.; Garcia, J.; Luepke, P.; Lai, Y.L.; Kassab, M.; Lin, G.H. The effect of partially exposed connective tissue graft on root-coverage outcomes: A systematic review and meta-analysis. Eur. J. Oral. Sci. 2018, 126, 84–92. [Google Scholar] [CrossRef]
- Chambrone, L.; Ortega, M.A.S.; Sukekava, F.; Rotundo, R.; Kalemaj, Z.; Buti, J.; Prato, G.P.P. Root coverage procedures for treating localised and multiple recession-type defects. Cochrane Database Syst Rev. 2018, 10, Cd007161. [Google Scholar] [CrossRef]
- Tavelli, L.; Ravidà, A.; Lin, G.H.; Del Amo, F.S.; Tattan, M.; Wang, H.L. Comparison between Subepithelial Connective Tissue Graft and De-epithelialized Gingival Graft: A systematic review and a meta-analysis. J. Int. Acad. Periodontol. 2019, 21, 82–96. [Google Scholar]
- Dai, A.; Huang, J.P.; Ding, P.H.; Chen, L.L. Long-term stability of root coverage procedures for single gingival recessions: A systematic review and meta-analysis. J. Clin. Periodontol. 2019, 46, 572–585. [Google Scholar] [CrossRef]
- Cairo, F. Periodontal plastic surgery of gingival recessions at single and multiple teeth. Periodontology 2000 2017, 75, 296–316. [Google Scholar] [CrossRef]
- Prato, G.P.; Franceschi, D.; Cortellini, P.; Chambrone, L. Long-term evaluation (20 years) of the outcomes of subepithelial connective tissue graft plus coronally advanced flap in the treatment of maxillary single recession-type defects. J. Periodontol. 2018, 89, 1290–1299. [Google Scholar] [CrossRef]
- Allen, A.L. Use of the supraperiosteal envelope in soft tissue grafting for root coverage. I. Rationale and technique. Int. J. Periodontics restor. Dent. 1994, 14, 302–315. [Google Scholar]
- Zabalegui, I.; Sicilia, A.; Cambra, J.; Gil, J.; Sanz, M. Treatment of multiple adjacent gingival recessions with the tunnel subepithelial connective tissue graft: A clinical report. Int. J. Periodontics restor. Dent. 1999, 19, 199–206. [Google Scholar]
- Raetzke, P.B. Covering localized areas of root exposure employing the “envelope” technique. J. Periodontol. 1985, 56, 397–402. [Google Scholar] [CrossRef] [PubMed]
- Aroca, S.; Keglevich, T.; Nikolidakis, D.; Gera, I.; Nagy, K.; Azzi, R.; Etienne, D. Treatment of class III multiple gingival recessions: A randomized-clinical trial. J. Clin. Periodontol. 2010, 37, 88–97. [Google Scholar] [CrossRef] [PubMed]
- Azzi, R.; Takei, H.H.; Etienne, D.; Carranza, F.A. Root coverage and papilla reconstruction using autogenous osseous and connective tissue grafts. Int. J. Periodontics Restor. Dent. 2001, 21, 141–147. [Google Scholar]
- Zuhr, O.; Fickl, S.; Wachtel, H.; Bolz, W.; Hürzeler, M.B. Covering of gingival recessions with a modified microsurgical tunnel technique: Case report. Int. J. Periodontics Restor. Dent. 2007, 27, 457–463. [Google Scholar]
- Tavelli, L.; Barootchi, S.; Nguyen, T.V.; Tattan, M.; Ravidà, A.; Wang, H.-L. Efficacy of tunnel technique in the treatment of localized and multiple gingival recessions: A systematic review and a meta-analysis. J. Periodontol. 2018, 89, 1075–1090. [Google Scholar] [CrossRef]
- Azaripour, A.; Kissinger, M.; Farina, V.S.L.; Van Noorden, C.J.F.; Gerhold-Ay, A.; Willershausen, B.; Cortellini, P. Root coverage with connective tissue graft associated with coronally advanced flap or tunnel technique: A randomized, double-blind, mono-centre clinical trial. J. Clin. Periodontol. 2016, 43, 1142–1150. [Google Scholar] [CrossRef]
- Bherwani, C.; Kulloli, A.; Kathariya, R.; Shetty, S.; Agrawal, P.; Gujar, D.; Desai, A. Zucchelli’s technique or tunnel technique with subepithelial connective tissue graft for treatment of multiple gingival recessions. J. Int. Acad. Periodontol. 2014, 16, 34–42. [Google Scholar]
- Salhi, L.; Lecloux, G.; Seidel, L.; Rompen, E.; Lambert, F. Coronally advanced flap versus the pouch technique combined with a connective tissue graft to treat Miller’s class I gingival recession: A randomized controlled trial. J. Clin. Periodontol. 2014, 41, 387–395. [Google Scholar] [CrossRef]
- Santamaria, M.P.; Da Neves, F.L.S.; Silveira, C.A.; Mathias, I.F.; Fernandes-Dias, S.B.; Jardini, M.A.N.; Tatakis, D.N. Connective tissue graft and tunnel or trapezoidal flap for the treatment of single maxillary gingival recessions: A randomized clinical trial. J. Clin. Periodontol. 2017, 44, 540–547. [Google Scholar] [CrossRef] [PubMed]
- Tözüm, T.F.; Keçeli, H.G.; Güncü, G.N.; Hatipoğlu, H.; Sengün, D. Treatment of gingival recession: Comparison of two techniques of subepithelial connective tissue graft. J. Periodontol. 2005, 76, 1842–1848. [Google Scholar] [CrossRef] [PubMed]
- Rossberg, M.; Eickholz, P.; Raetzke, P.; Ratka-Krüger, P. Long-term results of root coverage with connective tissue in the envelope technique: A report of 20 cases. Int. J. Periodontics Restor. Dent. 2008, 28, 19–27. [Google Scholar]
- Rompen, E.H.; Kohl, J.; Nusgens, B.; Lapiere, C.M. Kinetic aspects of gingival and periodontal ligament fibroblast attachment to surface-conditioned dentin. J. Dent. Res. 1993, 72, 607–612. [Google Scholar] [CrossRef]
- Vanheusden, A.J.; Goffinet, G.; Zahedi, S.; Nusgens, B.; Lapière, C.M.; Rompen, E.H. In vitro stimulation of human gingival epithelial cell attachment to dentin by surface conditioning. J. Periodontol. 1999, 70, 594–603. [Google Scholar] [CrossRef]
- Vanheusden, A.; Nusgens, B.; Goffinet, G.; Zahedi, S.; Lapière, C.M.; Rompen, E. In vitro modulation of human gingival epithelial cell attachment and migration by minocycline-HCL. J. Periodontal Res. 1998, 33, 377–385. [Google Scholar] [CrossRef]
- Fürhauser, R.; Florescu, D.; Benesch, T.; Haas, R.; Mailath, G.; Watzek, G. Evaluation of soft tissue around single-tooth implant crowns: The pink esthetic score. Clin. Oral Implant. Res. 2005, 16, 639–644. [Google Scholar] [CrossRef]
- Palmer, R.M.; Cortellini, P.; Group B of the European Workshop on Periodontology. Periodontal tissue engineering and regeneration: Consensus Report of the Sixth European Workshop on Periodontology. J. Clin. Periodontol. 2008, 35, 83–86. [Google Scholar] [CrossRef]
- Leknes, K.N.; Amarante, E.S.; Price, D.E.; Bøe, O.E.; Skavland, R.J.; Lie, T. Coronally positioned flap procedures with or without a biodegradable membrane in the treatment of human gingival recession. A 6-year follow-up study. J. Clin. Periodontol. 2005, 32, 518–529. [Google Scholar] [CrossRef]
- Prato, G.P.P.; Franceschi, D.; Rotundo, R.; Cairo, F.; Cortellini, P.; Nieri, M. Long-Term 8-Year Outcomes of Coronally Advanced Flap for Root Coverage. J. Periodontol. 2012, 83, 590–594. [Google Scholar] [CrossRef]
- Prato, G.P.P.; Rotundo, R.; Franceschi, D.; Cairo, F.; Cortellini, P.; Nieri, M. Fourteen-year outcomes of coronally advanced flap for root coverage: Follow-up from a randomized trial. J. Clin. Periodontol. 2011, 38, 715–720. [Google Scholar] [CrossRef]
- McGuire, M.K.; Scheyer, E.T.; Nunn, M. Evaluation of Human Recession Defects Treated With Coronally Advanced Flaps and Either Enamel Matrix Derivative or Connective Tissue: Comparison of Clinical Parameters at 10 Years. J. Periodontol. 2012, 83, 1353–1362. [Google Scholar] [CrossRef] [PubMed]
- Prato, G.P.P.; Cairo, F.; Nieri, M.; Franceschi, D.; Rotundo, R.; Cortellini, P. Coronally advanced flap versus connective tissue graft in the treatment of multiple gingival recessions: A split-mouth study with a 5-year follow-up. J. Clin. Periodontol. 2010, 37, 644–650. [Google Scholar] [CrossRef] [PubMed]
- Rasperini, G.; Acunzo, R.; Pellegrini, G.; Pagni, G.; Tonetti, M.; Prato, G.P.P.; Cortellini, P. Predictor factors for long-term outcomes stability of coronally advanced flap with or without connective tissue graft in the treatment of single maxillary gingival recessions: 9 years results of a randomized controlled clinical trial. J. Clin. Periodontol. 2018, 45, 1107–1117. [Google Scholar] [CrossRef] [PubMed]
- Harris, R.J. Root coverage with connective tissue grafts: An evaluation of short- and long-term results. J. Periodontol. 2002, 73, 1054–1059. [Google Scholar] [CrossRef]
- Zucchelli, G.; De Sanctis, M. Long-Term Outcome Following Treatment of Multiple Miller Class I and II Recession Defects in Esthetic Areas of the Mouth. J. Periodontol. 2005, 76, 2286–2292. [Google Scholar] [CrossRef]
- Zahedi, S.; Blase, D.; Bercy, P. Is periodontal guided tissue regeneration a reproducible technic? A review of the literature. Rev. Belge. Med. Dent. 1998, 53, 217–236. [Google Scholar]
- Rebele, S.F.; Zuhr, O.; Schneider, D.; Jung, R.E.; Hürzeler, M.B. Tunnel technique with connective tissue graft versus coronally advanced flap with enamel matrix derivative for root coverage: A RCT using 3D digital measuring methods. Part II. Volumetric studies on healing dynamics and gingival dimensions. J. Clin. Periodontol. 2014, 41, 593–603. [Google Scholar] [CrossRef]
- Gonzalez-Martin, O.; Veltri, M.; Moraguez, O.; Belser, U.C. Quantitative three-dimensional methodology to assess volumetric and profilometric outcome of subepithelial connective tissue grafting at pontic sites: A prospective pilot study. Int. J. Periodontics Restor. Dent. 2014, 34, 673–679. [Google Scholar] [CrossRef]
- Cairo, F.; Rotundo, R.; Miller, P.D.; Prato, G.P.P. Root Coverage Esthetic Score: A System to Evaluate the Esthetic Outcome of the Treatment of Gingival Recession Through Evaluation of Clinical Cases. J. Periodontol. 2009, 80, 705–710. [Google Scholar] [CrossRef]

| CAF + CTG N = 20 | POT + CTG N = 20 | |
|---|---|---|
| Gender (male/female) | 8/12 | 6/14 |
| Age (years: mean ± SD) | 44.3 ± 13.6 | 42.8 ± 12.8 |
| No. of teeth treated | 27 | 23 |
| Ratio teeth/patient | 5.4 | 4.6 |
| Single recession site | 15 | 16 |
| Multiple recession site | 5 | 4 |
| Type of teeth | ||
| Incisor | 7 | 5 |
| Canine | 18 | 13 |
| Premolar | 2 | 5 |
| Parameter | Group | Baseline Mean ± SD | Six Months Mean ± SD | Four Years Mean ± SD | p-Value Baseline vs. Six Months * | p-Value Six Months vs. Four Years ** |
|---|---|---|---|---|---|---|
| RD (mm) | POT + CTG | 2.78 ± 0.94 | 0.29 ± 0.61 | 0.38 ± 0.72 | <0.0001 | 0.48 |
| CAF + CTG | 3.03 ± 0.90 | 0.16 ± 0.50 | 0.15 ± 0.38 | <0.0001 | 0.67 | |
| p-value | 0.39 | 0.47 | 0.33 | 0.080 | 0.44 | |
| GT (mm) | POT + CTG | 1.08 ± 0.34 | 1.37 ± 0.37 | 2.06 ± 0.77 | 0.0075 | 0.0075 |
| CAF + CTG | 1.03 ± 0.26 | 1.25 ± 0.35 | 1.23 ± 0.33 | 0.035 | 1.00 | |
| p-value | 0.60 | 0.32 | 0.0012 | 0.79 | 0.019 | |
| KT (mm) | POT + CTG | 3.55 ± 0.95 | 4.68 ± 1.06 | 5.00 ± 0.82 | 0.0004 | 0.42 |
| CAF + CTG | 3.28 ± 0.97 | 3.53 ± 1.12 | 3.62 ± 1.26 | 0.52 | 0.19 | |
| p-value | 0.37 | 0.0024 | 0.0014 | 0.019 | 0.88 | |
| MRC (%) | POT + CTG | NA | 91.3 ± 17.6 | 90.1 ± 18.2 | NA | 0.56 |
| CAF + CTG | NA | 96.3 ± 12.1 | 95.9 ± 10.4 | NA | 0.79 | |
| p-value | NA | 0.31 | 0.32 | NA | 0.59 | |
| CRC (%) | POT + CTG | NA | 17/19 (89.5) | 13/16 (81.3) | NA | 0.32 |
| CAF + CTG | NA | 19/19 (100.0) | 13/13 (100.0) | NA | 0.99 | |
| p-value | NA | 0.49 | 0.52 | NA | 0.57 | |
| LPS (%) | POT + CTG | 0.00 ± 0.00 | 0.00 ± 0.00 | 1.56 ± 6.3 | 0.99 | 0.33 |
| CAF + CTG | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.99 | 0.99 | |
| p-value | 0.99 | 0.99 | 0.38 | 0.99 | 0.38 | |
| LBS (%) | POT + CTG | 0.05 ± 0.22 | 1.32 ± 5.74 | 1.56 ± 6.25 | 0.35 | 0.33 |
| CAF + CTG | 1.25 ± 5.59 | 1.32 ± 5.74 | 0.00 ± 0.00 | 1.00 | 0.99 | |
| p-value | 0.34 | 0.99 | 0.38 | 0.59 | 0.38 |
| Parameter | Group | Baseline Mean ± SD | Six Months Mean ± SD | Four Years Mean ± SD | p-Value Baseline vs. Six Months * | p-Value Six Months vs. Four Years ** |
|---|---|---|---|---|---|---|
| Mesial papilla | POT + CTG | 1.70 ± 0.47 | 1.84 ± 0.37 | 1.88 ± 0.34 | 0.33 | 0.33 |
| CAF + CTG | 1.80 ± 0.41 | 1.84 ± 0.37 | 1.77 ± 0.44 | 0.33 | 0.34 | |
| p-value | 0.48 | 0.99 | 0.47 | 0.66 | 0.17 | |
| Distal papilla | POT + CTG | 1.75 ± 0.44 | 1.84 ± 0.37 | 1.94 ± 0.25 | 0.16 | 0.33 |
| CAF + CTG | 1.85 ± 0.49 | 1.89 ± 0.32 | 1.85 ± 0.38 | 0.67 | 0.34 | |
| p-value | 0.50 | 0.64 | 0.44 | 0.71 | 0.17 | |
| Level of soft tissue margin | POT + CTG | 0.95 ± 0.39 | 2.00 ± 0.00 | 2.00 ± 0.00 | <0.0001 | 0.99 |
| CAF + CTG | 0.90 ± 0.45 | 2.00 ± 0.00 | 1.85 ± 0.38 | <0.0001 | 0.17 | |
| p-value | 0.71 | 0.99 | 0.11 | 0.42 | 0.11 | |
| Soft tissue contour | POT + CTG | 1.30 ± 0.47 | 1.95 ± 0.23 | 1.81 ± 0.54 | <0.0001 | 0.33 |
| CAF + CTG | 1.20 ± 0.41 | 1.89 ± 0.32 | 1.77 ± 0.44 | <0.0001 | 0.34 | |
| p-value | 0.48 | 0.56 | 0.82 | 0.77 | 0.76 | |
| Alveolar process | POT + CTG | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.99 | 0.99 |
| CAF + CTG | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.00 ± 0.00 | 0.99 | 0.99 | |
| p-value | 0.99 | 0.99 | 0.99 | 0.99 | 0.99 | |
| Color | POT + CTG | 1.85 ± 0.37 | 2.00 ± 0.00 | 2.00 ± 0.00 | 0.083 | 0.99 |
| CAF + CTG | 1.85 ± 0.37 | 2.00 ± 0.00 | 1.92 ± 0.28 | 0.083 | 0.34 | |
| p-value | 0.99 | 0.99 | 0.28 | 0.99 | 0.28 | |
| Texture | POT + CTG | 1.15 ± 0.37 | 1.95 ± 0.23 | 1.94 ± 0.25 | <0.0001 | 0.99 |
| CAF + CTG | 1.05 ± 0.22 | 1.32 ± 0.48 | 1.15 ± 0.38 | 0.021 | 0.99 | |
| p-value | 0.30 | <0.0001 | <0.0001 | 0.0007 | 0.99 | |
| PES | POT + CTG | 8.70 ± 1.53 | 11.6 ± 0.61 | 11.6 ± 0.73 | <0.0001 | 1.00 |
| CAF + CTG | 8.55 ± 1.19 | 11.0 ± 1.03 | 10.3 ± 1.65 | <0.0001 | 0.25 | |
| p-value | 0.73 | 0.027 | 0.011 | 0.44 | 0.25 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Salem, S.; Salhi, L.; Seidel, L.; Lecloux, G.; Rompen, E.; Lambert, F. Tunnel/Pouch versus Coronally Advanced Flap Combined with a Connective Tissue Graft for the Treatment of Maxillary Gingival Recessions: Four-Year Follow-Up of a Randomized Controlled Trial. J. Clin. Med. 2020, 9, 2641. https://doi.org/10.3390/jcm9082641
Salem S, Salhi L, Seidel L, Lecloux G, Rompen E, Lambert F. Tunnel/Pouch versus Coronally Advanced Flap Combined with a Connective Tissue Graft for the Treatment of Maxillary Gingival Recessions: Four-Year Follow-Up of a Randomized Controlled Trial. Journal of Clinical Medicine. 2020; 9(8):2641. https://doi.org/10.3390/jcm9082641
Chicago/Turabian StyleSalem, Souheil, Leila Salhi, Laurence Seidel, Geoffrey Lecloux, Eric Rompen, and France Lambert. 2020. "Tunnel/Pouch versus Coronally Advanced Flap Combined with a Connective Tissue Graft for the Treatment of Maxillary Gingival Recessions: Four-Year Follow-Up of a Randomized Controlled Trial" Journal of Clinical Medicine 9, no. 8: 2641. https://doi.org/10.3390/jcm9082641
APA StyleSalem, S., Salhi, L., Seidel, L., Lecloux, G., Rompen, E., & Lambert, F. (2020). Tunnel/Pouch versus Coronally Advanced Flap Combined with a Connective Tissue Graft for the Treatment of Maxillary Gingival Recessions: Four-Year Follow-Up of a Randomized Controlled Trial. Journal of Clinical Medicine, 9(8), 2641. https://doi.org/10.3390/jcm9082641






