High Endothelial Venule with Concomitant High CD8+ Tumor-Infiltrating Lymphocytes Is Associated with a Favorable Prognosis in Resected Gastric Cancer
Abstract
1. Introduction
2. Materials and Methods
2.1. Patients
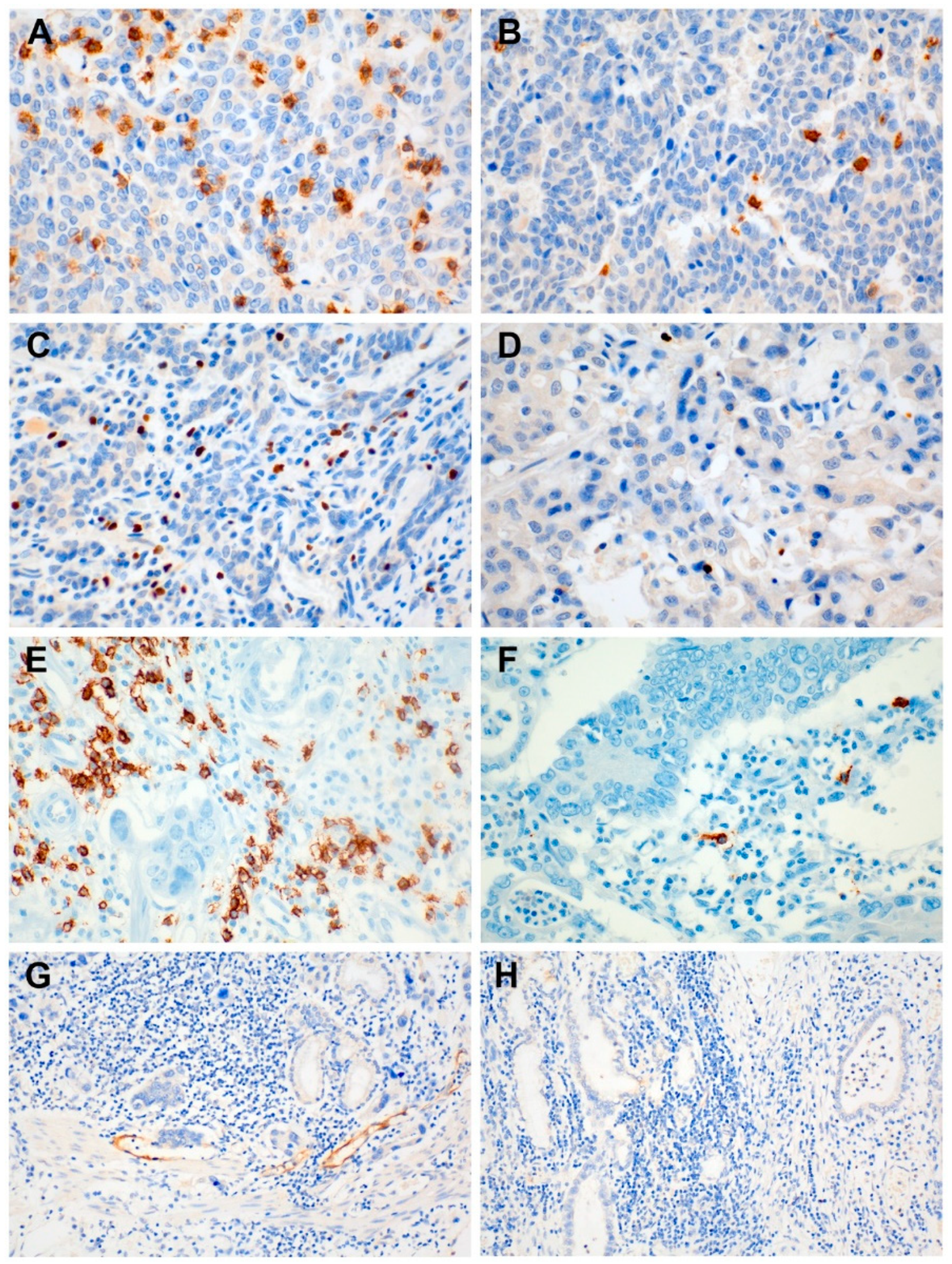
2.2. Immunohistochemistry
2.3. Evaluation of Immunohistochemistry
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
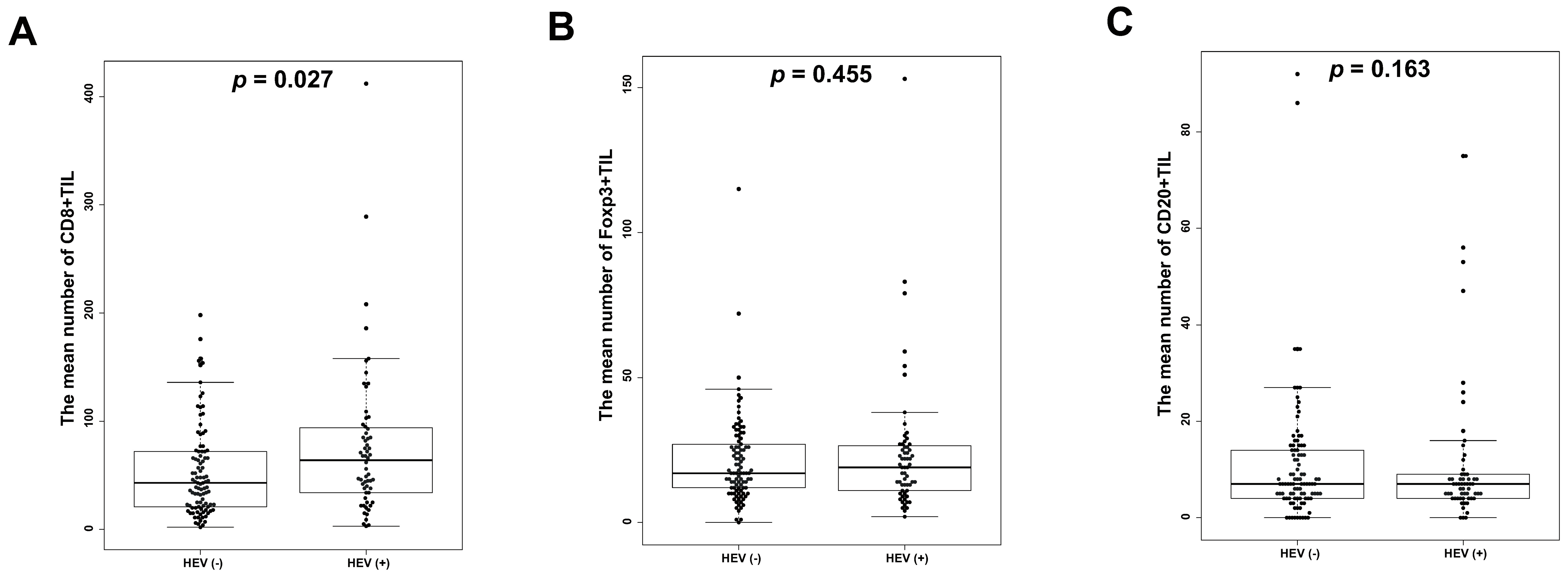
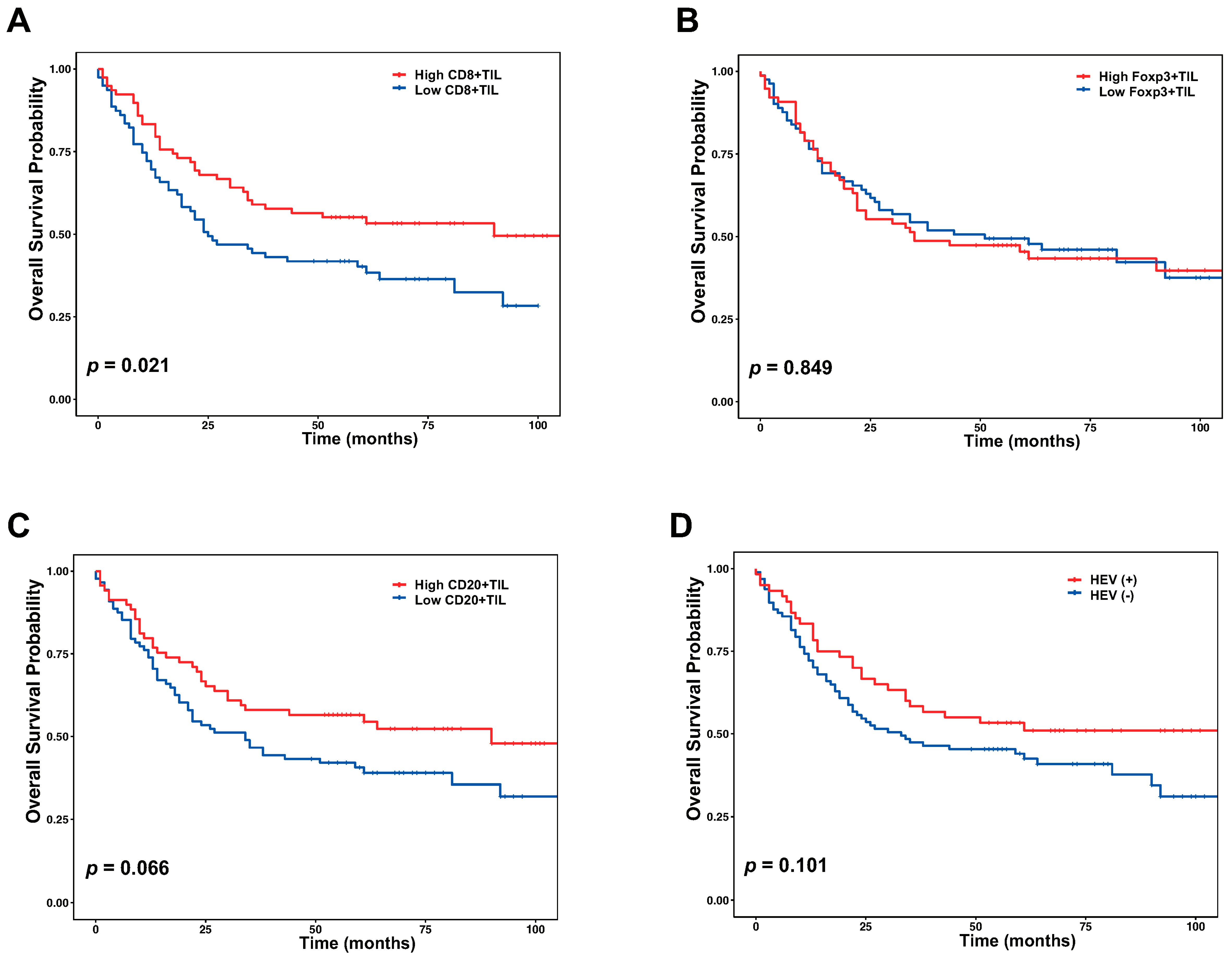
3.2. Correlation of HEVs and TILs with Clinicopathological Factors and Survival
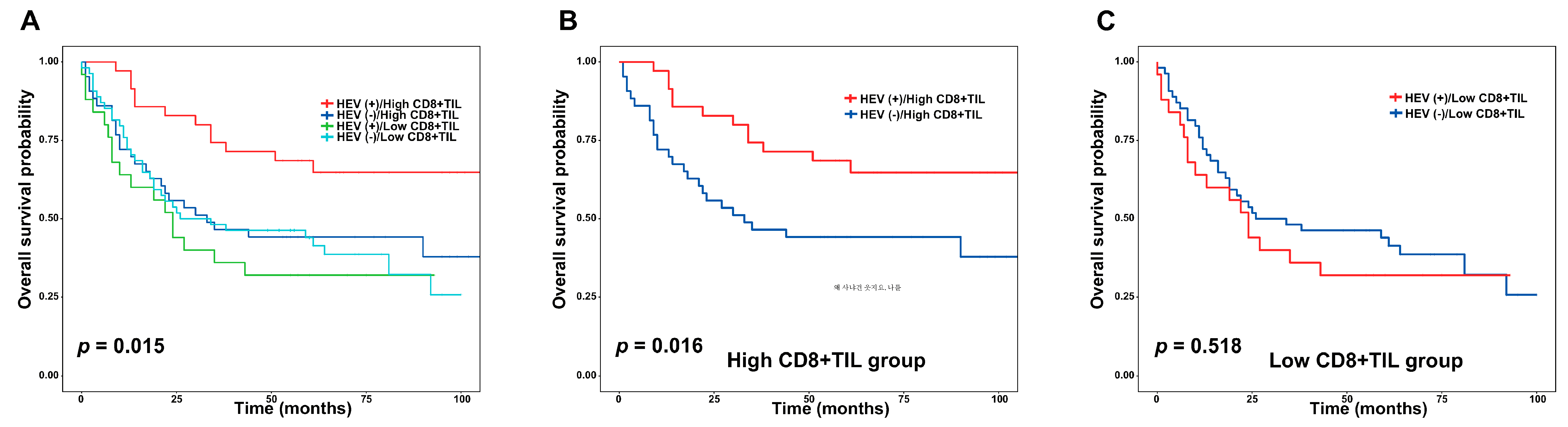
3.3. Combined Analysis with CD8+ TIL and HEV.
3.4. Univariate and Multivariate Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I.; Siegel, R.L.; Torre, L.A.; Jemal, A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J. Clin. 2018, 68, 394–424. [Google Scholar] [CrossRef] [PubMed]
- Jim, M.A.; Pinheiro, P.S.; Carreira, H.; Espey, D.K.; Wiggins, C.L.; Weir, H.K. Stomach cancer survival in the United States by race and stage (2001–2009): Findings from the CONCORD-2 study. Cancer 2017, 123, 4994–5013. [Google Scholar] [CrossRef] [PubMed]
- Gong, J.; Chehrazi-Raffle, A.; Reddi, S.; Salgia, R. Development of PD-1 and PD-L1 inhibitors as a form of cancer immunotherapy: A comprehensive review of registration trials and future considerations. J. Immunother. Cancer 2018, 6, 8. [Google Scholar] [CrossRef] [PubMed]
- Kang, Y.-K.; Boku, N.; Satoh, T.; Ryu, M.-H.; Chao, Y.; Kato, K.; Chung, H.C.; Chen, J.-S.; Muro, K.; Kang, W.K. Nivolumab in patients with advanced gastric or gastro-oesophageal junction cancer refractory to, or intolerant of, at least two previous chemotherapy regimens (ONO-4538-12, ATTRACTION-2): A randomised, double-blind, placebo-controlled, phase 3 trial. Lancet 2017, 390, 2461–2471. [Google Scholar] [CrossRef]
- Zhang, Y.; Huang, S.; Gong, D.; Qin, Y.; Shen, Q. Programmed death-1 upregulation is correlated with dysfunction of tumor-infiltrating CD8+ T lymphocytes in human non-small cell lung cancer. Cell. Mol. Immunol. 2010, 7, 389–395. [Google Scholar] [CrossRef]
- Kilinc, M.O.; Gu, T.; Harden, J.L.; Virtuoso, L.P.; Egilmez, N.K. Central role of tumor-associated CD8+ T effector/memory cells in restoring systemic antitumor immunity. J. Immunol. 2009, 182, 4217–4225. [Google Scholar] [CrossRef]
- Avram, G.; Sanchez-Sendra, B.; Martin, J.M.; Terradez, L.; Ramos, D.; Monteagudo, C. The density and type of MECA-79-positive high endothelial venules correlate with lymphocytic infiltration and tumour regression in primary cutaneous melanoma. Histopathology 2013, 63, 852–861. [Google Scholar] [CrossRef]
- Ager, A.; May, M.J. Understanding high endothelial venules: Lessons for cancer immunology. Oncoimmunology 2015, 4, e1008791. [Google Scholar] [CrossRef]
- Girard, J.-P.; Springer, T.A. High endothelial venules (HEVs): Specialized endothelium for lymphocyte migration. Immunol. Today 1995, 16, 449–457. [Google Scholar] [CrossRef]
- Streeter, P.R.; Rouse, B.; Butcher, E.C. Immunohistologic and functional characterization of a vascular addressin involved in lymphocyte homing into peripheral lymph nodes. J. Cell Boil. 1988, 107, 1853–1862. [Google Scholar] [CrossRef]
- Hemmerich, S.; Butcher, E.C.; Rosen, S.D. Sulfation-dependent recognition of high endothelial venules (HEV)-ligands by L-selectin and MECA 79, and adhesion-blocking monoclonal antibody. J. Exp. Med. 1994, 180, 2219–2226. [Google Scholar] [CrossRef] [PubMed]
- Hiraoka, N.; Ino, Y.; Yamazaki-Itoh, R. Tertiary Lymphoid Organs in Cancer Tissues. Front. Immunol. 2016, 7, 244. [Google Scholar] [CrossRef] [PubMed]
- Martinet, L.; Le Guellec, S.; Filleron, T.; Lamant, L.; Meyer, N.; Rochaix, P.; Garrido, I.; Girard, J.P. High endothelial venules (HEVs) in human melanoma lesions: Major gateways for tumor-infiltrating lymphocytes. Oncoimmunology 2012, 1, 829–839. [Google Scholar] [CrossRef] [PubMed]
- Martinet, L.; Garrido, I.; Filleron, T.; Le Guellec, S.; Bellard, E.; Fournie, J.J.; Rochaix, P.; Girard, J.P. Human solid tumors contain high endothelial venules: Association with T- and B-lymphocyte infiltration and favorable prognosis in breast cancer. Cancer Res. 2011, 71, 5678–5687. [Google Scholar] [CrossRef] [PubMed]
- Low, S.; Sakai, Y.; Hoshino, H.; Hirokawa, M.; Kawashima, H.; Higuchi, K.; Imamura, Y.; Kobayashi, M. High endothelial venule-like vessels and lymphocyte recruitment in diffuse sclerosing variant of papillary thyroid carcinoma. Pathology 2016, 48, 666–674. [Google Scholar] [CrossRef] [PubMed]
- Sakai, Y.; Hoshino, H.; Kitazawa, R.; Kobayashi, M. High endothelial venule-like vessels and lymphocyte recruitment in testicular seminoma. Andrology 2014, 2, 282–289. [Google Scholar] [CrossRef]
- Klebanoff, C.A.; Gattinoni, L.; Restifo, N.P. CD8+ T-cell memory in tumor immunology and immunotherapy. Immunol. Rev. 2006, 211, 214–224. [Google Scholar] [CrossRef]
- Hinrichs, C.S.; Rosenberg, S.A. Exploiting the curative potential of adoptive T-cell therapy for cancer. Immunol. Rev. 2014, 257, 56–71. [Google Scholar] [CrossRef]
- Roybal, K.T.; Williams, J.Z.; Morsut, L.; Rupp, L.J.; Kolinko, I.; Choe, J.H.; Walker, W.J.; McNally, K.A.; Lim, W.A. Engineering T cells with customized therapeutic response programs using synthetic notch receptors. Cell 2016, 167, 419–432. [Google Scholar] [CrossRef]
- Bento, D.C.; Jones, E.; Junaid, S.; Tull, J.; Williams, G.T.; Godkin, A.; Ager, A.; Gallimore, A. High endothelial venules are rare in colorectal cancers but accumulate in extra-tumoral areas with disease progression. Oncoimmunology 2015, 4, e974374. [Google Scholar] [CrossRef]
- Figenschau, S.L.; Fismen, S.; Fenton, K.A.; Fenton, C.; Mortensen, E.S. Tertiary lymphoid structures are associated with higher tumor grade in primary operable breast cancer patients. BMC Cancer 2015, 15, 101. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Kim, J.Y.; Park, I.A.; Song, I.H.; Yu, J.H.; Ahn, J.-H.; Gong, G. Prognostic significance of tumor-infiltrating lymphocytes and the tertiary lymphoid structures in HER2-positive breast cancer treated with adjuvant trastuzumab. Am. J. Clin. Pathol. 2015, 144, 278–288. [Google Scholar] [CrossRef] [PubMed]
- Bertrand, F.; Rochotte, J.; Colacios, C.; Montfort, A.; Andrieu-Abadie, N.; Levade, T.; Benoist, H.; Segui, B. Targeting TNF alpha as a novel strategy to enhance CD8(+) T cell-dependent immune response in melanoma? Oncoimmunology 2016, 5, e1068495. [Google Scholar] [CrossRef] [PubMed]
- Peske, J.D.; Woods, A.B.; Engelhard, V.H. Control of CD8 T-Cell Infiltration into Tumors by Vasculature and Microenvironment. Adv. Cancer Res. 2015, 128, 263–307. [Google Scholar]
- Hinrichs, C.S.; Borman, Z.A.; Cassard, L.; Gattinoni, L.; Spolski, R.; Yu, Z.; Sanchez-Perez, L.; Muranski, P.; Kern, S.J.; Logun, C. Adoptively transferred effector cells derived from naive rather than central memory CD8+ T cells mediate superior antitumor immunity. Proc. Natl. Acad. Sci. USA 2009, 106, 17469–17474. [Google Scholar] [CrossRef]
- Yu, P.; Lee, Y.; Liu, W.; Chin, R.K.; Wang, J.; Wang, Y.; Schietinger, A.; Philip, M.; Schreiber, H.; Fu, Y.X. Priming of naive T cells inside tumors leads to eradication of established tumors. Nat. Immunol. 2004, 5, 141–149. [Google Scholar] [CrossRef]
- Spiotto, M.T.; Yu, P.; Rowley, D.A.; Nishimura, M.I.; Meredith, S.C.; Gajewski, T.F.; Fu, Y.-X.; Schreiber, H. Increasing tumor antigen expression overcomes “ignorance” to solid tumors via crosspresentation by bone marrow-derived stromal cells. Immunity 2002, 17, 737–747. [Google Scholar] [CrossRef]
- Bai, X.-F.; Liu, J.; Li, O.; Zheng, P.; Liu, Y. Antigenic drift as a mechanism for tumor evasion of destruction by cytolytic T lymphocytes. J. Clin. Investig. 2003, 111, 1487–1496. [Google Scholar] [CrossRef]
- Hori, S.; Sakaguchi, S. Foxp3: A critical regulator of the development and function of regulatory T cells. Microbes Infect. 2004, 6, 745–751. [Google Scholar] [CrossRef]
- Gao, Q.; Qiu, S.-J.; Fan, J.; Zhou, J.; Wang, X.-Y.; Xiao, Y.-S.; Xu, Y.; Li, Y.-W.; Tang, Z.-Y. Intratumoral balance of regulatory and cytotoxic T cells is associated with prognosis of hepatocellular carcinoma after resection. J. Clin. Oncol. 2007, 25, 2586–2593. [Google Scholar] [CrossRef]
- Petersen, R.P.; Campa, M.J.; Sperlazza, J.; Conlon, D.; Joshi, M.B.; Harpole, D.H., Jr.; Patz, E.F., Jr. Tumor infiltrating Foxp3+ regulatory T-cells are associated with recurrence in pathologic stage I NSCLC patients. Cancer 2006, 107, 2866–2872. [Google Scholar] [CrossRef] [PubMed]
- Heimberger, A.B.; Abou-Ghazal, M.; Reina-Ortiz, C.; Yang, D.S.; Sun, W.; Qiao, W.; Hiraoka, N.; Fuller, G.N. Incidence and prognostic impact of FoxP3+ regulatory T cells in human gliomas. Clin. Cancer Res. 2008, 14, 5166–5172. [Google Scholar] [CrossRef] [PubMed]
- Perrone, G.; Ruffini, P.A.; Catalano, V.; Spino, C.; Santini, D.; Muretto, P.; Spoto, C.; Zingaretti, C.; Sisti, V.; Alessandroni, P.; et al. Intratumoural FOXP3-positive regulatory T cells are associated with adverse prognosis in radically resected gastric cancer. Eur. J. Cancer 2008, 44, 1875–1882. [Google Scholar] [CrossRef] [PubMed]
- Mizukami, Y.; Kono, K.; Kawaguchi, Y.; Akaike, H.; Kamimura, K.; Sugai, H.; Fujii, H. Localisation pattern of Foxp3+ regulatory T cells is associated with clinical behaviour in gastric cancer. Br. J. Cancer 2008, 98, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Roncarolo, M.G.; Gregori, S. Is FOXP3 a bona fide marker for human regulatory T cells? Eur. J. Immunol. 2008, 38, 925–927. [Google Scholar] [CrossRef]
- Walker, M.R.; Kasprowicz, D.J.; Gersuk, V.H.; Bènard, A.; Van Landeghen, M.; Buckner, J.H.; Ziegler, S.F. Induction of FoxP3 and acquisition of T regulatory activity by stimulated human CD4+ CD25–T cells. J. Clin. Investig. 2003, 112, 1437–1443. [Google Scholar] [CrossRef]
- Inamura, S.; Shinagawa, T.; Hoshino, H.; Sakai, Y.; Imamura, Y.; Yokoyama, O.; Kobayashi, M. Appearance of High Endothelial Venule-Like Vessels in Benign Prostatic Hyperplasia is Associated With Lower Urinary tract Symptoms. Prostate 2017, 77, 794–802. [Google Scholar] [CrossRef]
| CD8 | FOXP3 | CD20 | HEV | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Variables | High (n = 78) (%) | Low (n = 79) (%) | p Value | High (n = 74) (%) | Low (n = 83) (%) | p Value | High (n = 69) (%) | Low (n = 88) (%) | p Value | Positive (n = 60) (%) | Negative (n = 97) (%) | p Value |
| Age | 0.923 | 0.035 * | 0.594 | 0.749 | ||||||||
| ≥66 | 47 (60.3) | 46 (58.2) | 52 (68.4) | 41 (50.6) | 43 (62.3) | 50 (56.8) | 37 (61.7) | 56 (57.7) | ||||
| <66 | 31 (39.7) | 33 (41.8) | 24 (31.6) | 40 (49.4) | 26 (37.7) | 38 (43.2) | 23 (38.3) | 41 (42.3) | ||||
| Gender | 0.342 | 0.509 | 0.728 | 0.591 | ||||||||
| Male | 54 (69.2) | 61(77.2) | 58 (76.3) | 57 (70.4) | 52 (75.4) | 63 (71.6) | 42 (70.0) | 73 (75.3) | ||||
| Female | 24 (30.8) | 18 (22.8) | 18 (23.7) | 24 (29.6) | 17 (24.6) | 25 (28.4) | 18 (30.0) | 24 (24.7) | ||||
| Tumor size | 0.092 | 0.918 | 0.994 | 0.116 | ||||||||
| ≥5.5 | 31 (39.7) | 43 (54.4) | 35 (46.1) | 39 (48.1) | 32 (46.4) | 42 (47.7) | 23 (38.3) | 51 (52.6) | ||||
| <5.5 | 47 (60.3) | 36 (45.6) | 41 (53.9) | 42 (51.9) | 37 (53.4) | 46 (52.3) | 37 (61.7) | 46 (47.4) | ||||
| Histologic grade | 0.169 | 0.266 | 0.838 | 0.083 | ||||||||
| Well | 11 (14.1) | 5 (6.3) | 10 (13.2) | 6 (7.4) | 7 (10.1) | 9 (10.2) | 8 (13.3) | 8 (8.2) | ||||
| Moderate | 28 (35.9) | 25 (31.6) | 28 (36.8) | 25 (30.9) | 25 (36.2) | 28 (31.8) | 14 (23.3) | 39 (40.2) | ||||
| Poorly | 39 (50.0) | 49 (62.0) | 38 (50.0) | 50 (61.7) | 37 (53.6) | 51 (58.0) | 38 (63.3) | 50 (51.5) | ||||
| Lauren classification | 0.096 | 0.146 | 0.132 | 0.454 | ||||||||
| Intestinal | 42 (53.8) | 33 (41.8) | 41 (53.9) | 34 (42.0) | 35 (50.7) | 40 (45.5) | 25 (41.7) | 50 (51.5) | ||||
| Diffuse | 19 (24.4) | 32 (40.5) | 19 (25.0) | 32 (39.5) | 17 (24.6) | 34 (38.6) | 21 (35.0) | 30 (30.9) | ||||
| Mixed | 17 (21.8) | 14 (17.7) | 16 (21.1) | 15 (18.5) | 17 (24.6) | 14 (15.9) | 14 (23.3) | 17 (17.5) | ||||
| pT stage | 0.045 * | 0.910 | 0.181 | 1.000 | ||||||||
| T2 | 49 (62.8) | 36 (45.6) | 42 (55.3) | 43 (53.1) | 42 (60.9) | 43 (48.9) | 32 (53.3) | 53 (54.6) | ||||
| T3/T4 | 29 (37.2) | 43(54.4) | 34 (44.7) | 38 (46.9) | 27 (30.1) | 45 (51.1) | 28 (46.7) | 44 (45.4) | ||||
| pN stage | 0.011 * | 0.849 | 0.503 | 0.427 | ||||||||
| N0 | 37 (47.4) | 21 (26.6) | 27 (35.5) | 31 (38.3) | 28 (40.6) | 30 (34.1) | 25 (41.7) | 33 (34.0) | ||||
| N1/N2/N3 | 41 (52.6) | 58 (73.4) | 49 (64.5) | 50 (61.7) | 41 (59.4) | 58 (65.9) | 35 (58.3) | 64 (66.0) | ||||
| pM stage | 0.318 | 0.708 | 1.000 | 0.291 | ||||||||
| M0 | 72 (92.3) | 68 (86.1) | 69 (90.8) | 71 (87.7) | 62 (89.9) | 78 (88.6) | 56 (93.3) | 84 (86.6) | ||||
| M1 | 6 (7.7) | 11 (13.9) | 7 (9.2) | 10 (12.3) | 7 (10.1) | 10 (11.4) | 4 (6.7) | 13 (13.4) | ||||
| Lymphovascular invasion | 0.217 | 0.830 | 0.202 | 0.962 | ||||||||
| Yes | 47 (60.3) | 56 (70.9) | 51 (67.1) | 52 (64.2) | 41 (59.4) | 62 (70.5) | 40 (66.7) | 63 (64.9) | ||||
| No | 31 (39.7) | 23 (29.1) | 25 (32.9) | 29 (35.8) | 28 (40.6) | 26 (29.5) | 20 (33.3) | 34 (35.1) | ||||
| Perineural invasion | 0.174 | 0.170 | 0.058 | 0.005 * | ||||||||
| Yes | 33 (42.3) | 43 (54.5) | 32 (42.1) | 44 (54.3) | 42 (60.9) | 39 (44.3) | 38 (63.3) | 38 (39.2) | ||||
| No | 45 (57.7) | 36 (45.6) | 44 (57.9) | 37 (45.7) | 27 (30.1) | 48 (55.7) | 22 (36.7) | 59 (60.8) | ||||
| High CD8 with Positive HEV | |||
|---|---|---|---|
| Variables | Yes (n = 35) (%) | No (n = 122) (%) | p Value |
| Age | 0.765 | ||
| ≥66 | 22 (62.9) | 71 (58.2) | |
| <66 | 13 (37.1) | 51 (41.8) | |
| Gender | 0.174 | ||
| Male | 22 (62.9) | 93 (76.2) | |
| Female | 13 (37.1) | 29 (23.8) | |
| Tumor size | 0.125 | ||
| ≥5.5 | 12 (34.4) | 62 (50.8) | |
| <5.5 | 23 (65.7) | 60 (49.2) | |
| Histologic grade | 0.146 | ||
| Well | 4 (11.4) | 12 (9.8) | |
| Moderate | 7 (20.0) | 46 (37.7) | |
| Poorly | 24 (68.6) | 64 (52.5) | |
| Lauren classification | 0.137 | ||
| Intestinal | 15 (42.9) | 60 (49.2) | |
| Diffuse | 9 (25.7) | 42 (34.4) | |
| Mixed | 11 (31.4) | 20 (16.4) | |
| T stage | 0.832 | ||
| T2/T3 | 20 (57.1) | 65 (53.3) | |
| T4 | 15 (42.9) | 57 (46.7) | |
| n stage | 0.048 * | ||
| N0 | 19 (54.3) | 39 (32.0) | |
| ≥N1 | 16 (45.7) | 83 (68.0) | |
| Lymphovascular invasion | 1.000 | ||
| Yes | 23 (65.7) | 80 (65.6) | |
| No | 12 (34.3) | 42 (29.1) | |
| Perineural invasion | 0.831 | ||
| Yes | 18 (51.4) | 58 (47.5) | |
| No | 17 (48.6) | 64 (52.5) | |
| Clinicopathologic Factors | Univariate Analysis | Multivariate Analysis | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | p Value | HR | 95% CI | p Value | |
| Age (years), ≥66 vs. <66 | 1.720 | 1.098–2.696 | 0.018 * | 1.967 | 1.249–3.096 | 0.003 * |
| Gender, female vs. male | 0.843 | 0.533–1.333 | 0.465 | |||
| Tumor size, ≥5.5 vs. <5.5 | 1.837 | 1.202–2.808 | 0.005 * | 1.059 | 0.668–1.678 | 0.808 |
| Histologic grade, poorly vs. well/moderately | 1.286 | 0.593–2.788 | 0.524 | |||
| pT stage, pT4 vs. pT2/3 | 2.726 | 1.768–4.204 | <0.001 * | 1.880 | 1.165–3.033 | 0.010 * |
| pN stage, ≥pN1 vs. pN0 | 4.371 | 2.531–7.549 | <0.001 * | 2.972 | 1.668–5.295 | <0.001 * |
| pM stage M1 vs. M0 | 4.079 | 2.408–6.910 | <0.001 * | 1.894 | 1.077–3.330 | 0.027 * |
| Lymphovascular invasion, Yes vs. No | 3.229 | 1.898–5.494 | <0.001 * | 1.504 | 0.792–2.857 | 0.212 |
| Perineural invasion, Yes vs. No | 1.457 | 0.957–2.217 | 0.079 | |||
| R0 resection No vs. Yes | 2.973 | 1.729–5.109 | <0.001 * | 2.120 | 0.663–6.780 | 0.205 |
| CD8 High vs. Low | 0.611 | 0.400–0.933 | 0.023 * | 0.799 | 0.507–1.254 | 0.327 |
| FOXP3 High vs. Low | 0.887 | 0.576–1.335 | 0.539 | |||
| CD20 High vs. Low | 0.669 | 0.431–1.030 | 0.068 | |||
| HEV Yes vs. No | 0.693 | 0.444–1.081 | 0.106 | |||
| High CD8/ positive HEV Yes vs. No | 0.399 | 0.217–0.735 | 0.003 * | 0.464 | 0.243–0.883 | 0.019 * |
| High FOXP3/ Positive HEV Yes vs. No | 0.661 | 0.379–1.153 | 0.145 | |||
| High CD20/ positive HEV Yes vs. No | 0.540 | 0.271–1.078 | 0.081 | |||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hong, S.A.; Hwang, H.W.; Kim, M.K.; Lee, T.J.; Yim, K.; Won, H.S.; Sun, D.S.; Kim, E.Y.; Ko, Y.H. High Endothelial Venule with Concomitant High CD8+ Tumor-Infiltrating Lymphocytes Is Associated with a Favorable Prognosis in Resected Gastric Cancer. J. Clin. Med. 2020, 9, 2628. https://doi.org/10.3390/jcm9082628
Hong SA, Hwang HW, Kim MK, Lee TJ, Yim K, Won HS, Sun DS, Kim EY, Ko YH. High Endothelial Venule with Concomitant High CD8+ Tumor-Infiltrating Lymphocytes Is Associated with a Favorable Prognosis in Resected Gastric Cancer. Journal of Clinical Medicine. 2020; 9(8):2628. https://doi.org/10.3390/jcm9082628
Chicago/Turabian StyleHong, Soon Auck, Hye Won Hwang, Min Kyoon Kim, Tae Jin Lee, Kwangil Yim, Hye Sung Won, Der Sheng Sun, Eun Young Kim, and Yoon Ho Ko. 2020. "High Endothelial Venule with Concomitant High CD8+ Tumor-Infiltrating Lymphocytes Is Associated with a Favorable Prognosis in Resected Gastric Cancer" Journal of Clinical Medicine 9, no. 8: 2628. https://doi.org/10.3390/jcm9082628
APA StyleHong, S. A., Hwang, H. W., Kim, M. K., Lee, T. J., Yim, K., Won, H. S., Sun, D. S., Kim, E. Y., & Ko, Y. H. (2020). High Endothelial Venule with Concomitant High CD8+ Tumor-Infiltrating Lymphocytes Is Associated with a Favorable Prognosis in Resected Gastric Cancer. Journal of Clinical Medicine, 9(8), 2628. https://doi.org/10.3390/jcm9082628






