Trajectories of Short Physical Performance Battery Are Strongly Associated with Future Major Mobility Disability: Results from the LIFE Study
Abstract
1. Introduction
2. Methods
2.1. LIFE Study Overview
2.2. Intervention
2.3. Follow-Up Visits and Outcome Assessment
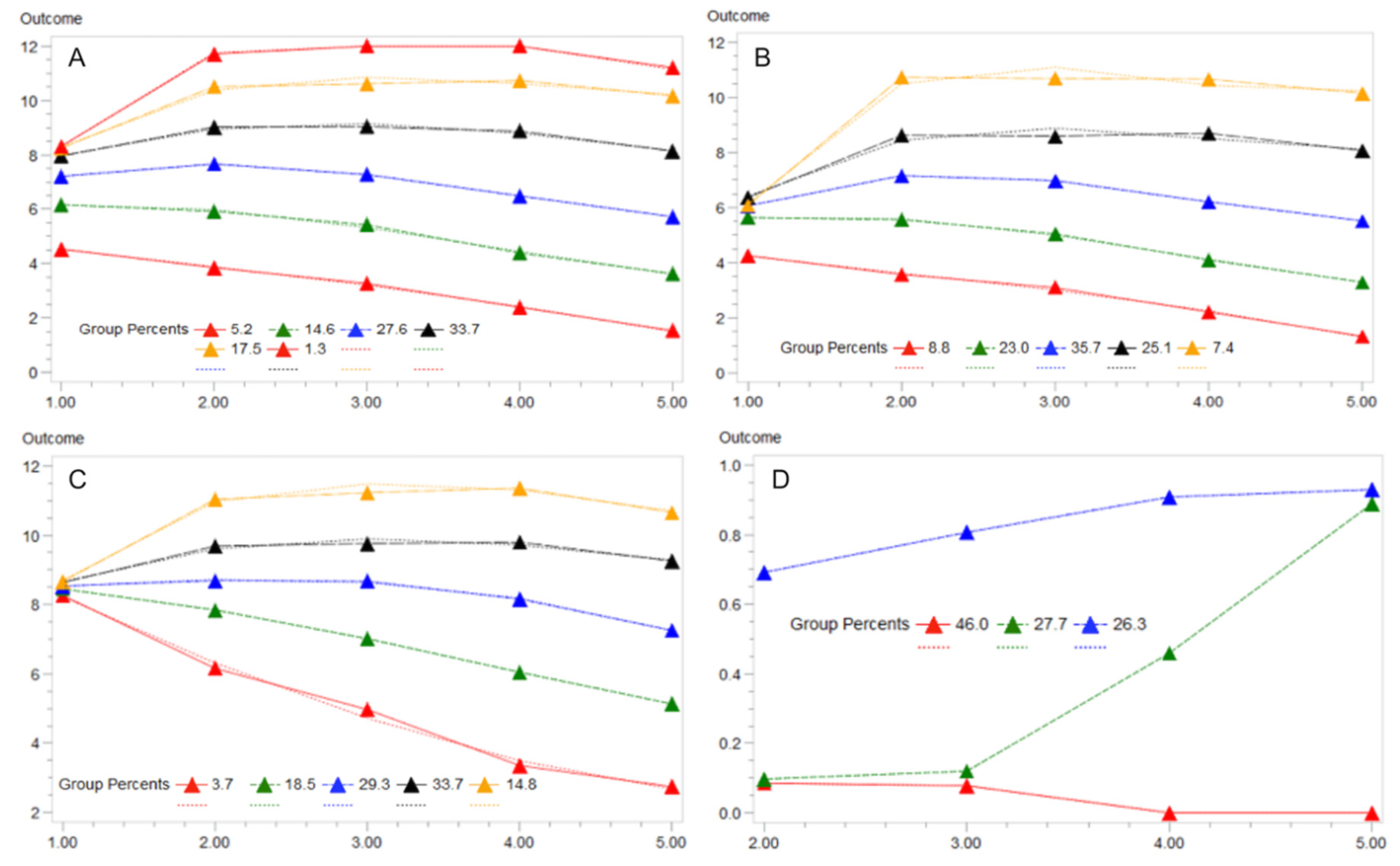
2.4. Group-Based Trajectory Modeling
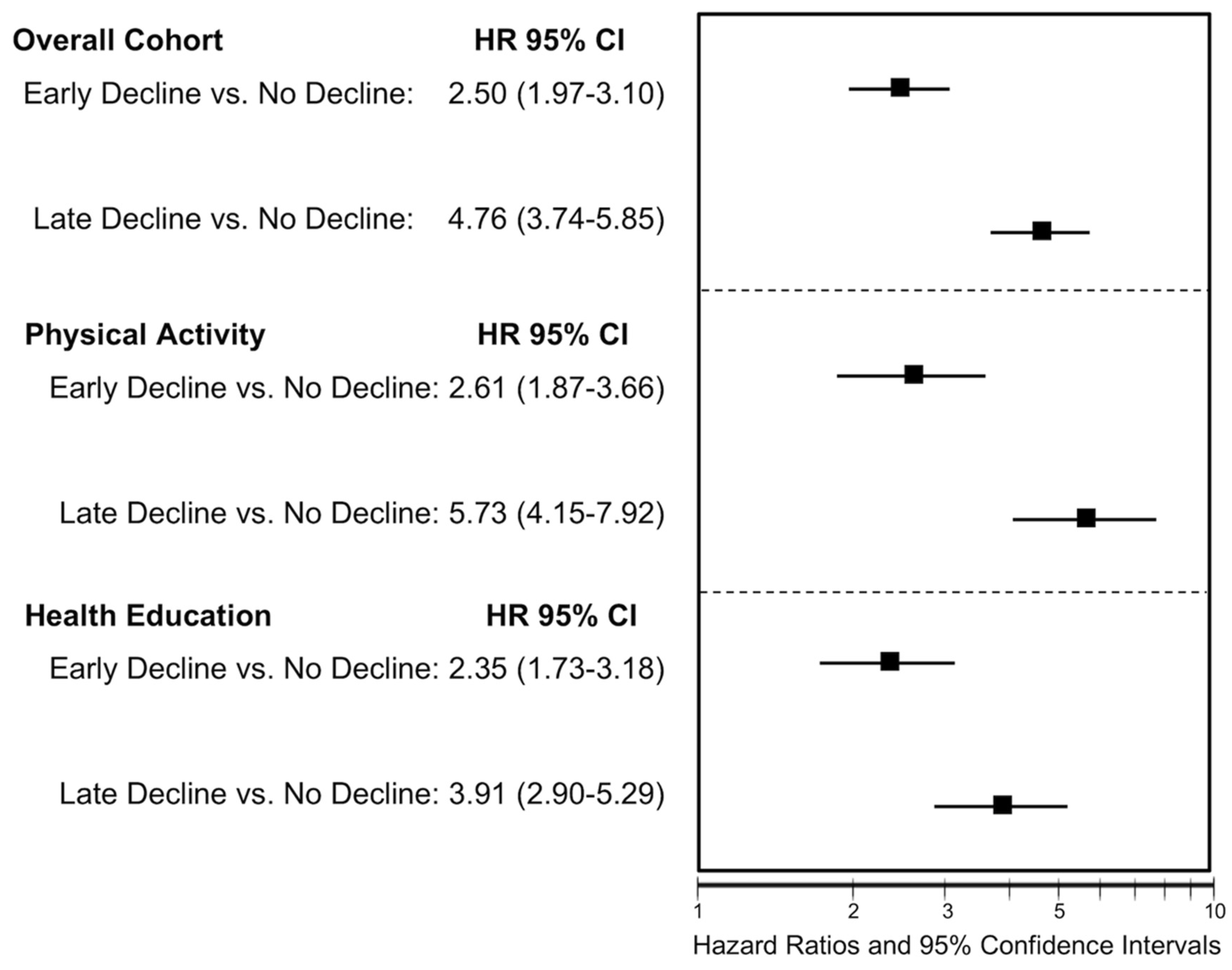
3. Results
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Guralnik, J.M.; Simonsick, E.M.; Ferrucci, L.; Glynn, R.J.; Berkman, L.F.; Blazer, D.G.; Scherr, P.A.; Wallace, R.B. A Short Physical Performance Battery Assessing Lower Extremity Function: Association with Self-Reported Disability and Prediction of Mortality and Nursing Home Admission. J. Gerontol. 1994, 49, M85–M94. [Google Scholar] [CrossRef] [PubMed]
- Santanasto, A.J.; Glynn, N.W.; Lovato, L.C.; Blair, S.N.; Fielding, R.A.; Gill, T.M.; Guralnik, J.M.; Hsu, F.-C.; King, A.C.; Strotmeyer, E.S.; et al. Effect of Physical Activity versus Health Education on Physical Function, Grip Strength and Mobility. J. Am. Geriatr. Soc. 2017, 65, 1427–1433. [Google Scholar] [CrossRef]
- Bean, J.F.; Kiely, D.K.; LaRose, S.; Goldstein, R.; Frontera, W.R.; Leveille, S. Are changes in leg power responsible for clinically meaningful improvements in mobility in older adults? J. Am. Geriatr. Soc. 2010, 58, 2363–2368. [Google Scholar] [CrossRef] [PubMed]
- Legrand, D.; Vaes, B.; Mathei, C.; Adriaensen, W.; Van Pottelbergh, G.; Degryse, J.-M. Muscle Strength and Physical Performance as Predictors of Mortality, Hospitalization, and Disability in the Oldest Old. J. Am. Geriatr. Soc. 2014, 62, 1030–1038. [Google Scholar] [CrossRef] [PubMed]
- Volpato, S.; Cavalieri, M.; Sioulis, F.; Guerra, G.; Maraldi, C.; Zuliani, G.; Fellin, R.; Guralnik, J.M. Predictive Value of the Short Physical Performance Battery Following Hospitalization in Older Patients. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2010, 66A, 89–96. [Google Scholar] [CrossRef] [PubMed]
- Pavasini, R.; Guralnik, J.; Brown, J.C.; Di Bari, M.; Cesari, M.; Landi, F.; Vaes, B.; Legrand, D.; Verghese, J.; Wang, C.; et al. Short Physical Performance Battery and all-cause mortality: Systematic review and meta-analysis. BMC Med. 2016, 14, 215. [Google Scholar] [CrossRef] [PubMed]
- Perera, S.; Mody, S.H.; Woodman, R.C.; Studenski, S.A. Meaningful Change and Responsiveness in Common Physical Performance Measures in Older Adults. J. Am. Geriatr. Soc. 2006, 54, 743–749. [Google Scholar] [CrossRef]
- Pahor, M.; Guralnik, J.M.; Ambrosius, W.T.; Blair, S.; Bonds, D.E.; Church, T.S.; Espeland, M.A.; Fielding, R.A.; Gill, T.M.; Groessl, E.J.; et al. Effect of structured physical activity on prevention of major mobility disability in older adults: The LIFE study randomized clinical trial. J. Am. Med. Assoc. 2014, 311, 2387–2396. [Google Scholar] [CrossRef]
- Fielding, R.A.; Rejeski, W.J.; Blair, S.; Church, T.; Espeland, M.A.; Gill, T.M.; Guralnik, J.M.; Hsu, F.-C.; Katula, J.; King, A.C.; et al. The Lifestyle Interventions and Independence for Elders Study: Design and Methods. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2011, 66, 1226–1237. [Google Scholar] [CrossRef]
- Layne, A.S.; Hsu, F.-C.; Blair, S.N.; Chen, S.-H.; Dungan, J.; Fielding, R.A.; Glynn, N.W.; Hajduk, A.M.; King, A.C.; Manini, T.M.; et al. Predictors of Change in Physical Function in Older Adults in Response to Long-Term, Structured Physical Activity: The LIFE Study. Arch. Phys. Med. Rehabil. 2017, 98, 11–24. [Google Scholar] [CrossRef]
- Nagin, D.S.; Odgers, C.L. Group-Based Trajectory Modeling in Clinical Research. Annu. Rev. Clin. Psychol. 2010, 6, 109–138. [Google Scholar] [CrossRef] [PubMed]
- White, D.K.; Neogi, T.; Nevitt, M.C.; Peloquin, C.E.; Zhu, Y.; Boudreau, R.; Cauley, J.A.; Ferrucci, L.; Harris, T.B.; Satterfield, S.M.; et al. Trajectories of Gait Speed Predict Mortality in Well-Functioning Older Adults: The Health, Aging and Body Composition Study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2012, 68, 456–464. [Google Scholar] [CrossRef] [PubMed]
- Laddu, D.R.; Parimi, N.; Cauley, J.A.; Cawthon, P.M.; Ensrud, K.E.; Orwoll, E.; Stefanick, M.; Langsetmo, L. Osteoporotic Fractures in Men (MrOS) Study Research Group; for the Osteoporotic Fractures in Men (MrOS) Study Research Group The Association Between Trajectories of Physical Activity and All-Cause and Cause-Specific Mortality. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2018, 73, 1708–1713. [Google Scholar] [CrossRef]
- Han, L.; Gill, T.M.; Jones, B.L.; Allore, H. Cognitive Aging Trajectories and Burdens of Disability, Hospitalization and Nursing Home Admission Among Community-living Older Persons. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2015, 71, 766–771. [Google Scholar] [CrossRef] [PubMed]
- De La Fuente, J.; Caballero, F.F.; Sanchez-Niubo, A.; Panagiotakos, D.B.; Prina, A.M.; Arndt, H.; Haro, J.M.; Chatterji, S.; Ayuso-Mateos, J.L.; Prina, M.A. Determinants of Health Trajectories in England and the United States: An Approach to Identify Different Patterns of Healthy Aging. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2018, 73, 1512–1518. [Google Scholar] [CrossRef] [PubMed]
- Marsh, A.P.; Lovato, L.C.; Glynn, N.W.; Kennedy, K.; Castro, C.; Domanchuk, K.; McDavitt, E.; Rodate, R.; Marsiske, M.; McGloin, J.; et al. Lifestyle interventions and independence for elders study: Recruitment and baseline characteristics. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2013, 68, 1549–1558. [Google Scholar] [CrossRef]
- Rejeski, W.J.; Axtell, R.; Fielding, R.; Katula, J.; King, A.C.; Manini, T.M.; Marsh, A.P.; Pahor, M.; Rego, A.; Tudor-Locke, C.; et al. Promoting physical activity for elders with compromised function: The lifestyle Interventions and Independence for elders (LIFE) study physical activity intervention. Clin. Interv. Aging 2013, 8, 1119–1131. [Google Scholar] [CrossRef] [PubMed]
- Jones, B.L.; Nagin, D.S.; Roeder, K. A SAS Procedure Based on Mixture Models for Estimating Developmental Trajectories. Sociol. Methods Res. 2001, 29, 374–393. [Google Scholar] [CrossRef]
- Pahor, M.; Guralnik, J.M.; Anton, S.D.; Ambrosius, W.T.; Blair, S.N.; Church, T.S.; Espeland, M.A.; Fielding, R.A.; Gill, T.M.; Glynn, N.W.; et al. Impact and Lessons From the Lifestyle Interventions and Independence for Elders (LIFE) Clinical Trials of Physical Activity to Prevent Mobility Disability. J. Am. Geriatr. Soc. 2020, 68, 872–881. [Google Scholar] [CrossRef]
- Resnick, B.; Boltz, M. The Impact of Psychological Status, Social Well-Being, and Physical Function on Healthcare Utilization. J. Am. Geriatr. Soc. 2020, 68, 241–243. [Google Scholar] [CrossRef]
- Riebe, D.; Franklin, B.A.; Thompson, P.D.; Garber, C.E.; Whitfield, G.P.; Magal, M.; Pescatello, L.S. Updating ACSM’s Recommendations for Exercise Preparticipation Health Screening. Med. Sci. Sports Exerc. 2015, 47, 2473–2479. [Google Scholar] [CrossRef] [PubMed]
- Cheng, Y.; Goodin, A.J.; Pahor, M.; Manini, T.; Brown, J.D. Healthcare Utilization and Physical Functioning in Older Adults in the United States. J. Am. Geriatr. Soc. 2019, 68, 266–271. [Google Scholar] [CrossRef] [PubMed]
- Brown, J.D.; Wang, C.Y.; Groessl, E.J.; Pahor, M.; Manini, T. Three-year post-intervention follow-up comparison of healthcare resource utilization and costs in the Lifestyle Interventions and Independence for Elders (LIFE) Study. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2020. [Google Scholar] [CrossRef]
| Characteristics | Group Membership | ||
|---|---|---|---|
| Group 1: No Decline | Group 2: Early Decline | Group 3: Late Decline | |
| n = 752 (46.0%) | n = 453 (27.7%) | n = 430 (26.3%) | |
| Physical activity intervention (n (%)] | 379 (50.4%) | 231 (51%) | 208 (48.5%) |
| Age, mean (SD) | 78 (5.0) | 79.4 (5.2) | 80.1 (5.3) |
| Female sex (n (%)] | 526 (70%) | 306 (67.6%) | 266 (61.9%) |
| Race (n (%)) | |||
| White | 543 (72.2%) | 356 (78.6%) | 343 (79.8%) |
| Black | 147 (19.5%) | 73 (16.1%) | 66 (15.3%) |
| Other | 62 (8.3%) | 24 (5.3%) | 21 (4.9%) |
| Education, ≥high school (n (%)] | 492 (65.5%) | 315 (69.5%) | 293 (68.2%) |
| BMI, kg/m2 (mean (SD)] | 30.3 (5.9) | 30.5 (5.8) | 29.6 (6.3) |
| Physical functioning assessments | |||
| SPPB ≤ 7 b (n (%)) | 333 (44.2%) | 221 (48.8%) | 176 (40.9%) |
| Gait speed, m/s (mean (SD)) | 0.8 (0.2) | 0.8 (0.2) | 0.8 (0.2) |
| Grip Strength, kg (mean (SD)) | 24.6 (10.4) | 23.1 (8.9) | 22.7 (9) |
| CHAMPS Score (range 0–120) a (mean (SD)) | 16.9 (32.5) | 17 (33.4) | 17.4 (33.5) |
| PAT-D (range 1–5) b (mean (SD)) | 1.4 (0.4) | 1.4 (0.4) | 1.5 (0.4) |
| Cognitive functioning assessments | |||
| 3MSE (range 0–100) a (mean (SD)) | 92 (5.2) | 91.7 (5.4) | 90.8 (5.6) |
| PSQI (range 0–21) b (mean (SD)) | 5.9 (3.8) | 6 (3.7) | 6 (3.8) |
| MATS score (range 30–80) a (mean (SD)) | 55.1 (7.9) | 52.4 (7.7) | 52.2 (8) |
| Smoking (n (%)) | |||
| Never | 405 (53.8%) | 241 (53.1%) | 218 (50.6%) |
| Former | 320 (42.6%) | 204 (45%) | 198 (46.1%) |
| Current | 27 (3.6%) | 9 (1.9%) | 14 (3.3%) |
| CVD (n (%)) | 205 (27.3%) | 139 (30.8%) | 146 (33.9%) |
| Diabetes (n (%)) | 199 (26.5%) | 133 (29.3%) | 126 (29.4%) |
| Heart attack (n (%)) | 69 (9.2%) | 46 (10.1%) | 42 (9.9%) |
| Heart failure (n (%)) | 39 (5.2%) | 34 (7.5%) | 23 (5.4%) |
| Metabolic Syndrome (n (%)) | 365 (48.5%) | 242 (53.3%) | 207 (48.1%) |
| Hypertension (n (%)) | 522 (69.5%) | 321 (70.9%) | 302 (70.1%) |
| Arthritis (n (%)) | 150 (19.9%) | 75 (16.6%) | 91 (21.2%) |
| Chronic lung disease (n (%)) | 133 (17.7%) | 77 (17.1%) | 71 (16.5%) |
| Self-Rated Health (good, very good, or excellent) (n (%)) | 462 (61.4%) | 294 (65%) | 296 (68.8%) |
| Characteristics | Group Membership Comparisons | ||
|---|---|---|---|
| Late Decline (Group 2) vs. No Decline (Group 1) 1 | Early Decline (Group 3) vs. No Decline (Group 1) 2 | Early Decline vs. Late Decline 3 | |
| Physical activity intervention | 1.05 (0.80–1.37) | 0.84 (0.64–1.11) | 0.96 (0.74–1.26) |
| Age | 1.05 (1.02–1.08) * | 1.07 (1.03–1.10) * | 0.98 (0.93–1.02) |
| Female sex | 0.66 (0.44–0.98) * | 0.39 (0.26–0.59) * | 2.13 (1.13–4.02) * |
| Race | |||
| White | 0.65 (0.31–1.35) | 0.9 (0.42–1.9) | 1.20 (0.62–2.32) |
| Black | Reference | Reference | Reference |
| Other | 1.29 (0.87–1.93) | 1.63 (1.06–2.51) * | 1.55 (0.51–4.71) |
| Education, ≥high school | 1.34 (0.99–1.81) | 1.29 (0.94–1.77) | 0.89 (0.57–1.40) |
| BMI | 1.01 (0.99–1.04) | 0.98 (0.96–1.01) | 1.00 (0.96–1.05) |
| MATS score | 0.95 (0.93–0.98) * | 0.95 (0.93–0.97) * | 1.02 (0.99–1.06) |
| Gait speed (m/s) | 1.4 (0.49–3.97) | 1.22 (0.41–3.6) | 2.50 (0.57–11.0) |
| Grip Strength | 0.99 (0.97–1.01) | 0.97 (0.95–0.99) * | 0.99 (0.96–1.02) |
| PAT-D | 1.1 (0.7–1.71) | 1.53 (0.98–2.4) | 0.87 (0.45–1.69) |
| 3MSE | 0.98 (0.95–1.00) | 0.95 (0.92–0.97) * | 1.03 (0.98–1.07) |
| PSQI | 1.01 (0.97–1.04) | 0.99 (0.95–1.03) | 1.05 (0.99–1.11) |
| CHAMPS Score | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) |
| SPPB ≤ 7 | 1.14 (1.04–1.25) * | 1.32 (1.19–1.46) * | 1.08 (0.66–1.76) |
| Smoking | |||
| Never | Reference | Reference | Reference |
| Former | 1.06 (0.8–1.4) | 1.16 (0.86–1.56) | 0.85 (0.55–1.32) |
| Current | 0.44 (0.17–1.14) | 1.1 (0.51–2.41) | 3.19 (1.14–8.96) * |
| CVD | 1.1 (0.79–1.55) | 1.16 (0.82–1.64) | 0.92 (0.55–1.52) |
| Diabetes | 0.99 (0.71–1.39) | 1.22 (0.87–1.72) | 0.86 (0.53–1.39) |
| Heart attack | 0.78 (0.45–1.33) | 0.71 (0.41–1.24) | 1.93 (0.92–4.08) |
| Heart failure | 1.19 (0.63–2.23) | 0.87 (0.44–1.72) | 0.91 (0.34–2.46) |
| Metabolic Syndrome | 1.11 (0.8–1.54) | 1.14 (0.81–1.61) | 0.98 (0.80–1.23) |
| Hypertension | 0.95 (0.69–1.32) | 1.05 (0.75–1.47) | 0.90 (0.80–1.05) |
| Arthritis | 0.69 (0.48–1.01) | 1.03 (0.72–1.48) | 1.12 (0.65–1.94) |
| Chronic lung disease | 0.92 (0.64–1.32) | 0.71 (0.48–1.05) | 1.04 (0.60–1.81) |
| Self-Rated Health (>Good) | 1.94 (1.01–3.74) * | 1.71 (0.84–3.47) | 1.13 (0.98–1.30) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brown, J.D.; Lo-Ciganic, W.-H.; Shao, H.; Pahor, M.; Manini, T.M. Trajectories of Short Physical Performance Battery Are Strongly Associated with Future Major Mobility Disability: Results from the LIFE Study. J. Clin. Med. 2020, 9, 2332. https://doi.org/10.3390/jcm9082332
Brown JD, Lo-Ciganic W-H, Shao H, Pahor M, Manini TM. Trajectories of Short Physical Performance Battery Are Strongly Associated with Future Major Mobility Disability: Results from the LIFE Study. Journal of Clinical Medicine. 2020; 9(8):2332. https://doi.org/10.3390/jcm9082332
Chicago/Turabian StyleBrown, Joshua D., Wei-Hsuan Lo-Ciganic, Hui Shao, Marco Pahor, and Todd M. Manini. 2020. "Trajectories of Short Physical Performance Battery Are Strongly Associated with Future Major Mobility Disability: Results from the LIFE Study" Journal of Clinical Medicine 9, no. 8: 2332. https://doi.org/10.3390/jcm9082332
APA StyleBrown, J. D., Lo-Ciganic, W.-H., Shao, H., Pahor, M., & Manini, T. M. (2020). Trajectories of Short Physical Performance Battery Are Strongly Associated with Future Major Mobility Disability: Results from the LIFE Study. Journal of Clinical Medicine, 9(8), 2332. https://doi.org/10.3390/jcm9082332






