Comprehensive Evaluation of the Oral Health Status, Salivary Gland Function, and Oxidative Stress in the Saliva of Patients with Subacute Phase of Stroke: A Case-Control Study
Abstract
1. Introduction
2. Material and Methods
2.1. Ethical Issues
2.2. Study Participants
2.3. Study Criteria
2.4. Study Group
- Addenbrooke’s Cognitive Examination III (ACE III) was used to differentiate patients with and without cognitive impairment [25].
- The functional independence measure (FIM) was used to explore individual’s physical, psychological and social functioning [26].
- The Barthel Index (BI) was used to measure performance in activities of daily living (ADL) [27].
- The Berg Balance Scale (BBS) was used to determine patient’s ability (or inability) to safely balance during a series of predetermined tasks [28].
2.5. Control Group
2.6. Oral Examination
2.7. Saliva Sampling
2.8. Redox Assays
2.8.1. Salivary Antioxidants
2.8.2. Salivary Redox Status
2.8.3. Salivary Oxidative Stress
2.9. Statistical Analysis
3. Results
3.1. Characteristics of Study and Control Groups
3.2. Oral Health Status
3.3. Salivary Gland Function
3.4. Enzymatic Antioxidants
3.5. Non-Enzymatic Antioxidants
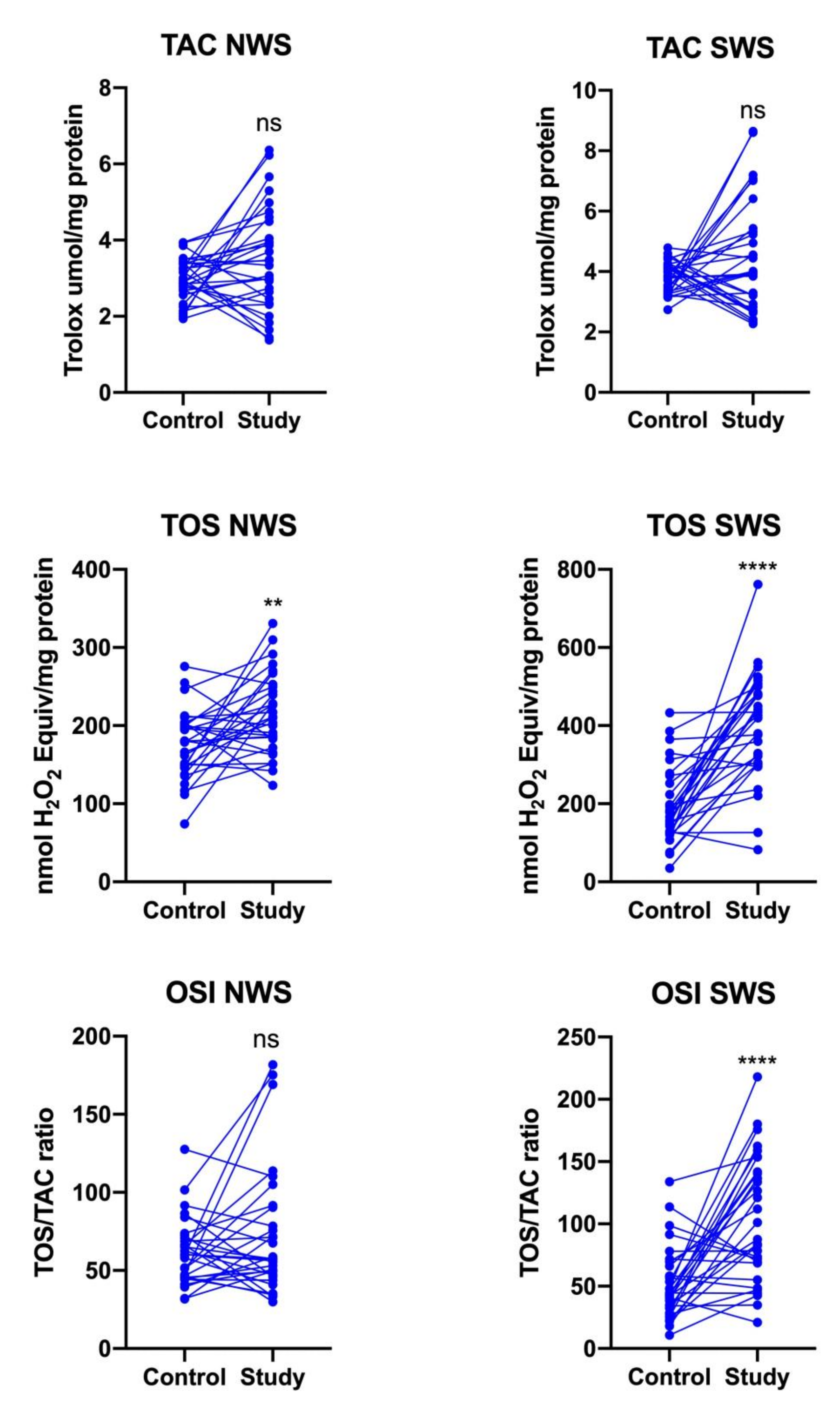
3.6. Redox Status
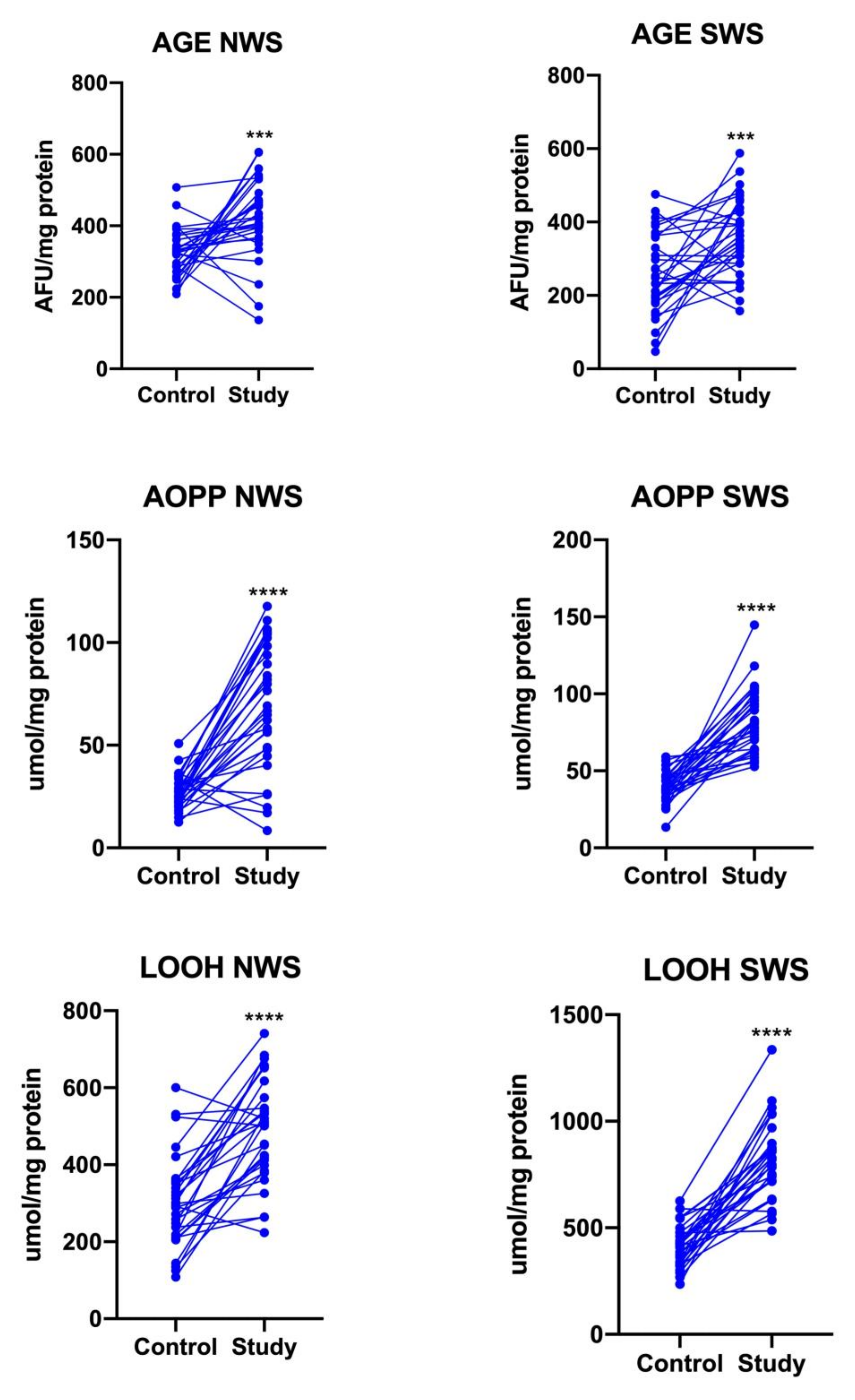
3.7. Oxidative Stress
3.8. Multifactorial Regression
3.9. Correlations
3.10. ROC Analysis
3.11. Supplementary Material
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hankey, G.J. Stroke. Lancet 2017, 389, 641–654. [Google Scholar] [CrossRef]
- Chamorro, Á.; Dirnagl, U.; Urra, X.; Planas, A.M. Neuroprotection in acute stroke: Targeting excitotoxicity, oxidative and nitrosative stress, and inflammation. Lancet Neurol. 2016, 15, 869–881. [Google Scholar] [CrossRef]
- Marzolini, S.; Robertson, A.D.; Oh, P.; Goodman, J.M.; Corbett, D.; Du, X.; MacIntosh, B.J. Aerobic Training and Mobilization Early Post-stroke: Cautions and Considerations. Front. Neurol. 2019, 10, 1187. [Google Scholar] [CrossRef]
- Bernhardt, J.; Hayward, K.S.; Kwakkel, G.; Ward, N.S.; Wolf, S.L.; Borschmann, K.; Krakauer, J.W.; Boyd, L.A.; Carmichael, S.T.; Corbett, D.; et al. Agreed definitions and a shared vision for new standards in stroke recovery research: The Stroke Recovery and Rehabilitation Roundtable taskforce. Int. J. Stroke 2017. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Zeng, F.; Li, Y.X.; Yu, B.L.; Qiu, L.H.; Qin, W.; Li, J.; Zhou, Y.M.; Liang, F.R. Changes of resting cerebral activities in subacute ischemic stroke patients. Neural Regen. Res. 2015. [Google Scholar] [CrossRef]
- Li, P.; Stetler, R.A.; Leak, R.K.; Shi, Y.; Li, Y.; Yu, W.; Bennett, M.V.L.; Chen, J. Oxidative stress and DNA damage after cerebral ischemia: Potential therapeutic targets to repair the genome and improve stroke recovery. Neuropharmacology 2018, 134, 208–217. [Google Scholar] [CrossRef]
- Żukowski, P.; Maciejczyk, M.; Waszkiel, D. Sources of free radicals and oxidative stress in the oral cavity. Arch. Oral Biol. 2018, 92, 8–17. [Google Scholar] [CrossRef]
- Zhao, H.; Han, Z.; Ji, X.; Luo, Y. Epigenetic regulation of oxidative stress in ischemic stroke. Aging Dis. 2016, 7, 295–306. [Google Scholar] [CrossRef]
- Maciejczyk, M.; Żebrowska, E.; Chabowski, A. Insulin Resistance and Oxidative Stress in the Brain: What’s New? Int. J. Mol. Sci. 2019, 20, 874. [Google Scholar] [CrossRef]
- Knaś, M.; Maciejczyk, M.; Waszkiel, D.; Zalewska, A. Oxidative stress and salivary antioxidants. Dent. Med. Probl. 2013, 50, 461–466. [Google Scholar]
- Maciejczyk, M.; Zalewska, A.; Gerreth, K. Salivary Redox Biomarkers in Selected Neurodegenerative Diseases. J. Clin. Med. 2020, 9, 497. [Google Scholar] [CrossRef]
- Milanlioglu, A.; Aslan, M.; Ozkol, H.; Çilingir, V.; Nuri Aydın, M.; Karadas, S. Serum antioxidant enzymes activities and oxidative stress levels in patients with acute ischemic stroke: Influence on neurological status and outcome. Wien. Klin. Wochenschr. 2016. [Google Scholar] [CrossRef]
- Cherubini, A.; Ruggiero, C.; Polidori, M.C.; Mecocci, P. Potential markers of oxidative stress in stroke. Free Radic. Biol. Med. 2005, 39, 841–852. [Google Scholar] [CrossRef] [PubMed]
- Maciejczyk, M.; Szulimowska, J.; Skutnik, A.; Taranta-Janusz, K.; Wasilewska, A.; Wiśniewska, N.; Zalewska, A. Salivary Biomarkers of Oxidative Stress in Children with Chronic Kidney Disease. J. Clin. Med. 2018, 7, 209. [Google Scholar] [CrossRef]
- Maciejczyk, M.; Żukowski, P.; Zalewska, A. Salivary Biomarkers in Kidney Diseases. In Saliva in Health and Disease; Tvarijonaviciute, A., Martínez-Subiela, S., López-Jornet, P., Lamy, E., Eds.; Springer International Publishing: Cham, Switzerland, 2020; pp. 193–219. ISBN 978-3-030-37681-9. [Google Scholar]
- Maciejczyk, M.; Szulimowska, J.; Taranta-Janusz, K.; Werbel, K.; Wasilewska, A.; Zalewska, A. Salivary FRAP as A Marker of Chronic Kidney Disease Progression in Children. Antioxidants 2019, 8, 409. [Google Scholar] [CrossRef]
- Klimiuk, A.; Zalewska, A.; Sawicki, R.; Knapp, M.; Maciejczyk, M. Salivary Oxidative Stress Increases With the Progression of Chronic Heart Failure. J. Clin. Med. 2020, 9, 769. [Google Scholar] [CrossRef] [PubMed]
- Maciejczyk, M.; Taranta-Janusz, K.; Wasilewska, A.; Kossakowska, A.; Zalewska, A. A Case-Control Study of Salivary Redox Homeostasis in Hypertensive Children. Can Salivary Uric Acid be a Marker of Hypertension? J. Clin. Med. 2020, 9, 837. [Google Scholar] [CrossRef] [PubMed]
- Zalewska, A.; Kossakowska, A.; Taranta-Janusz, K.; Zięba, S.; Fejfer, K.; Salamonowicz, M.; Kostecka-Sochoń, P.; Wasilewska, A.; Maciejczyk, M. Dysfunction of Salivary Glands, Disturbances in Salivary Antioxidants and Increased Oxidative Damage in Saliva of Overweight and Obese Adolescents. J. Clin. Med. 2020, 9, 548. [Google Scholar] [CrossRef]
- Fejfer, K.; Buczko, P.; Niczyporuk, M.; Ładny, J.R.; Hady, H.R.; Knaś, M.; Waszkiel, D.; Klimiuk, A.; Zalewska, A.; Maciejczyk, M. Oxidative Modification of Biomolecules in the Nonstimulated and Stimulated Saliva of Patients with Morbid Obesity Treated with Bariatric Surgery. BioMed Res. Int. 2017, 2017. [Google Scholar] [CrossRef] [PubMed]
- Choromańska, M.; Klimiuk, A.; Kostecka-Sochoń, P.; Wilczyńska, K.; Kwiatkowski, M.; Okuniewska, N.; Waszkiewicz, N.; Zalewska, A.; Maciejczyk, M. Antioxidant defence, oxidative stress and oxidative damage in saliva, plasma and erythrocytes of dementia patients. Can salivary AGE be a marker of dementia? Int. J. Mol. Sci. 2017, 18, 2205. [Google Scholar] [CrossRef]
- Klimiuk, A.; Maciejczyk, M.; Choromańska, M.; Fejfer, K.; Waszkiewicz, N.; Zalewska, A. Salivary Redox Biomarkers in Different Stages of Dementia Severity. J. Clin. Med. 2019, 8, 840. [Google Scholar] [CrossRef]
- Kim, H.T.; Park, J.B.; Lee, W.C.; Kim, Y.J.; Lee, Y. Differences in the oral health status and oral hygiene practices according to the extent of post-stroke sequelae. J. Oral Rehabil. 2018. [Google Scholar] [CrossRef] [PubMed]
- Lertpimonchai, A.; Rattanasiri, S.; Arj-Ong Vallibhakara, S.; Attia, J.; Thakkinstian, A. The association between oral hygiene and periodontitis: A systematic review and meta-analysis. Int. Dent. J. 2017, 67, 332–343. [Google Scholar] [CrossRef] [PubMed]
- Matias-Guiu, J.A.; Cortés-Martínez, A.; Valles-Salgado, M.; Rognoni, T.; Fernández-Matarrubia, M.; Moreno-Ramos, T.; Matías-Guiu, J. Addenbrooke’s cognitive examination III: Diagnostic utility for mild cognitive impairment and dementia and correlation with standardized neuropsychological tests. Int. Psychogeriatr. 2017. [Google Scholar] [CrossRef] [PubMed]
- Chumney, D.; Nollinger, K.; Shesko, K.; Skop, K.; Spencer, M.; Newton, R.A. Ability of functional independence measure to accurately predict functional outcome of stroke-specific population: Systematic review. J. Rehabil. Res. Dev. 2010, 47, 17–29. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Unick, J.; Galik, E.; Resnick, B. Barthel Index of Activities of Daily Living. Nurs. Res. 2015. [Google Scholar] [CrossRef] [PubMed]
- Louie, D.R.; Eng, J.J. Berg balance scale score at admission can predict walking suitable for community ambulation at discharge from inpatient stroke rehabilitation. J. Rehabil. Med. 2018. [Google Scholar] [CrossRef]
- Who. Oral Health Surveys—Basic Methofd; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Silness, J.; Löe, H. Periodontal disease in pregnancy II. Correlation between oral hygiene and periodontal condition. Acta Odontol. Scand. 1964, 22, 121–135. [Google Scholar] [CrossRef]
- Skutnik-Radziszewska, A.; Maciejczyk, M.; Flisiak, I.; Kołodziej, J.K.U.; Kotowska-Rodziewicz, A.; Klimiuk, A.; Zalewska, A. Enhanced Inflammation and Nitrosative Stress in the Saliva and Plasma of Patients with Plaque Psoriasis. J. Clin. Med. 2020, 9, 745. [Google Scholar] [CrossRef]
- Toczewska, J.; Konopka, T.; Zalewska, A.; Maciejczyk, M. Nitrosative Stress Biomarkers in the Non-Stimulated and Stimulated Saliva, as well as Gingival Crevicular Fluid of Patients with Periodontitis: Review and Clinical Study. Antioxidants 2020, 9, 259. [Google Scholar] [CrossRef]
- Mansson-Rahemtulla, B.; Baldone, D.C.; Pruitt, K.M.; Rahemtulla, F. Specific assays for peroxidases in human saliva. Arch. Oral Biol. 1986, 31, 661–668. [Google Scholar] [CrossRef]
- Aebi, H. Catalase in vitro. In Methods in Enzymology; Elsevier: Amsterdam, The Netherlands, 1984; Volume 105, pp. 121–126. ISBN 9780121820053. [Google Scholar]
- Misra, H.P.; Fridovich, I. The role of superoxide anion in the autoxidation of epinephrine and a simple assay for superoxide dismutase. J. Biol. Chem. 1972, 247, 3170–3175. [Google Scholar]
- Moron, M.; Depierre, J.; Mannervik, B. Levels of glutathione, glutathione reductase and glutathione S-transferase activities in rat lung and liver. Biochim. Biophys. Acta Gen. Subj. 1979, 582, 67–78. [Google Scholar] [CrossRef]
- Erel, O. A novel automated direct measurement method for total antioxidant capacity using a new generation, more stable ABTS radical cation. Clin. Biochem. 2004, 37, 277–285. [Google Scholar] [CrossRef]
- Erel, O. A new automated colorimetric method for measuring total oxidant status. Clin. Biochem. 2005, 38, 1103–1111. [Google Scholar] [CrossRef] [PubMed]
- Choromańska, B.; Myśliwiec, P.; Łuba, M.; Wojskowicz, P.; Dadan, J.; Myśliwiec, H.; Choromańska, K.; Zalewska, A.; Maciejczyk, M. A Longitudinal Study of the Antioxidant Barrier and Oxidative Stress in Morbidly Obese Patients after Bariatric Surgery. Does the Metabolic Syndrome Affect the Redox Homeostasis of Obese People? J. Clin. Med. 2020, 9, 976. [Google Scholar] [CrossRef] [PubMed]
- Kalousová, M.; Skrha, J.; Zima, T. Advanced glycation end-products and advanced oxidation protein products in patients with diabetes mellitus. Physiol. Res. 2002, 51, 597–604. [Google Scholar]
- Świderska, M.; Maciejczyk, M.; Zalewska, A.; Pogorzelska, J.; Flisiak, R.; Chabowski, A. Oxidative stress biomarkers in the serum and plasma of patients with non-alcoholic fatty liver disease (NAFLD). Can plasma AGE be a marker of NAFLD? Free Radic. Res. 2019. [Google Scholar] [CrossRef]
- Grintzalis, K.; Zisimopoulos, D.; Grune, T.; Weber, D.; Georgiou, C.D. Method for the simultaneous determination of free/protein malondialdehyde and lipid/protein hydroperoxides. Free Radic. Biol. Med. 2013, 59, 27–35. [Google Scholar] [CrossRef]
- Ahmed, N.; de la Torre, B.; Wahlgren, N.G. Salivary Cortisol, a Biological Marker of Stress, Is Positively Associated with 24-Hour Systolic Blood Pressure in Patients with Acute Ischaemic Stroke. Cerebrovasc. Dis. 2004, 18, 206–213. [Google Scholar] [CrossRef]
- Wang, J.; Guan, Q.; Sheng, Y.; Yang, Y.; Guo, L.; Li, W.; Gu, Y.; Han, C. The potential predictive value of salivary cortisol on the occurrence of secondary cognitive impairment after ischemic stroke. Neurosurg. Rev. 2020. [Google Scholar] [CrossRef]
- Al-Rawi, N.H.; Atiyah, K.M. Salivary neuron specific enolase: An indicator for neuronal damage in patients with ischemic stroke and stroke-prone patients. Clin. Chem. Lab. Med. 2009. [Google Scholar] [CrossRef]
- Niimi, M.; Hashimoto, G.; Hara, T.; Yamada, N.; Abo, M.; Fujigasaki, H.; Ide, T. Relationship Between Frequency of Spontaneous Swallowing and Salivary Substance P Level in Patients with Acute Stroke. Dysphagia 2018. [Google Scholar] [CrossRef] [PubMed]
- Kim, I.S.; Han, T.R. Influence of mastication and salivation on swallowing in stroke patients. Arch. Phys. Med. Rehabil. 2005. [Google Scholar] [CrossRef] [PubMed]
- Crack, P.J.; Taylor, J.M. Reactive oxygen species and the modulation of stroke. Free Radic. Biol. Med. 2005, 38, 1433–1444. [Google Scholar] [CrossRef] [PubMed]
- Doyle, K.P.; Simon, R.P.; Stenzel-Poore, M.P. Mechanisms of ischemic brain damage. Neuropharmacology 2008. [Google Scholar] [CrossRef]
- Shirle, R.; Ord, E.N.J.; Work, L.M. Oxidative stress and the use of antioxidants in stroke. Antioxidants 2014, 3, 472–501. [Google Scholar] [CrossRef]
- Miyatani, F.; Kuriyama, N.; Watanabe, I.; Nomura, R.; Nakano, K.; Matsui, D.; Ozaki, E.; Koyama, T.; Nishigaki, M.; Yamamoto, T.; et al. Relationship between Cnm-positive Streptococcus mutans and cerebral microbleeds in humans. Oral Dis. 2015. [Google Scholar] [CrossRef]
- Wang, X.; Michaelis, E.K. Selective Neuronal Vulnerability to Oxidative Stress in the Brain. Front. Aging Neurosci. 2010, 2, 12. [Google Scholar] [CrossRef]
- Battino, M.; Ferreiro, M.S.; Gallardo, I.; Newman, H.N.; Bullon, P. The antioxidant capacity of saliva. J. Clin. Periodontol. 2002, 29, 189–194. [Google Scholar] [CrossRef]
- Sautin, Y.Y.; Johnson, R.J. Uric Acid: The Oxidant-Antioxidant Paradox. Nucleosides Nucleotides Nucleic Acids 2008, 27, 608–619. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Lin, Y.; Liu, Y.; Chen, Y.; Wang, B.; Li, C.; Yan, S.; Wang, Y.; Zhao, W. Serum Uric Acid Levels and Outcomes After Acute Ischemic Stroke. Mol. Neurobiol. 2016. [Google Scholar] [CrossRef] [PubMed]
- Seet, R.C.S.; Kasiman, K.; Gruber, J.; Tang, S.Y.; Wong, M.C.; Chang, H.M.; Chan, Y.H.; Halliwell, B.; Chen, C.P. Is uric acid protective or deleterious in acute ischemic stroke? A prospective cohort study. Atherosclerosis 2010. [Google Scholar] [CrossRef] [PubMed]
- Ott, C.; Jacobs, K.; Haucke, E.; Navarrete Santos, A.; Grune, T.; Simm, A. Role of advanced glycation end products in cellular signaling. Redox Biol. 2014, 2, 411–429. [Google Scholar] [CrossRef]
- Stadtman, E.R.; Levine, R.L. Free radical-mediated oxidation of free amino acids and amino acid residues in proteins. Amino Acids 2003, 25, 207–218. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Schipper, H.M.; Velly, A.M.; Mohit, S.; Gornitsky, M. Salivary biomarkers of oxidative stress: A critical review. Free Radic. Biol. Med. 2015, 85, 95–104. [Google Scholar] [CrossRef]
- Martina, E.; Campanati, A.; Diotallevi, F.; Offidani, A. Saliva and Oral Diseases. J. Clin. Med. 2020, 9, 466. [Google Scholar] [CrossRef]
- Dringen, R. Metabolism and functions of glutathione in brain. Prog. Neurobiol. 2000, 62, 649–671. [Google Scholar] [CrossRef]
- Proctor, G.B.; Carpenter, G.H. Regulation of salivary gland function by autonomic nerves. Auton. Neurosci. 2007, 133, 3–18. [Google Scholar] [CrossRef]
- Carpenter, G.H. The Secretion, Components, and Properties of Saliva. Annu. Rev. Food Sci. Technol. 2013. [Google Scholar] [CrossRef]
- Maciejczyk, M.; Szulimowska, J.; Taranta-Janusz, K.; Wasilewska, A.; Zalewska, A. Salivary Gland Dysfunction, Protein Glycooxidation and Nitrosative Stress in Children with Chronic Kidney Disease. J. Clin. Med. 2020, 9, 1285. [Google Scholar] [CrossRef] [PubMed]
- Károlyházy, K.; Arányi, Z.; Hermann, P.; Vastagh, I.; Márton, K. Oral health status of stroke patients related to residual symptoms: A case-control epidemiological study in Hungary. Oral Heal. Prev. Dent. 2018. [Google Scholar] [CrossRef]
- Nakano, K.; Hokamura, K.; Taniguchi, N.; Wada, K.; Kudo, C.; Nomura, R.; Kojima, A.; Naka, S.; Muranaka, Y.; Thura, M.; et al. The collagen-binding protein of Streptococcus mutans is involved in haemorrhagic stroke. Nat. Commun. 2011. [Google Scholar] [CrossRef]
- Pietropaoli, D.; Monaco, A.; Del Pinto, R.; Cifone, M.G.; Marzo, G.; Giannoni, M. Advanced glycation end products: Possible link between metabolic syndrome and periodontal diseases. Int. J. Immunopathol. Pharmacol. 2012, 25, 9–17. [Google Scholar] [CrossRef] [PubMed]
- Pietropaoli, D.; Tatone, C.; D’Alessandro, A.M.; Monaco, A. Possible involvement of advanced glycation end products in periodontal diseases. Int. J. Immunopathol. Pharmacol. 2010, 23, 683–691. [Google Scholar] [CrossRef] [PubMed]
- Meurman, J.H. A Role for Oral Health Personnel in Stroke Prevention. Compend. Contin. Educ. Dent. 2017, 38, 26–28. [Google Scholar] [PubMed]




| Patients Characteristics | Control n = 30 | Study n = 30 | p-Value | |
|---|---|---|---|---|
| Sex | male n (%) | 18 (60.00) | 18 (60.00) | ns |
| female n (%) | 12 (40.00) | 12 (40.00) | ||
| Age in years | (mean ± SD) | 61.87 ± 11.81 | 61.87 ± 11.81 | ns |
| Education | primary n (%) | 2 (6.67) | 3 (10.00) | ns |
| vocational n (%) | 13 (43.33) | 12 (40.00) | ns | |
| secondary n (%) | 8 (26.67) | 7 (23.33) | ns | |
| university n (%) | 7 (23.33) | 8 (26.67) | ns | |
| Place of residence | urban centre n (%) | 11 (36.67) | 8 (26.67) | ns |
| small town n (%) | 7 (23.33) | 11 (36.67) | ns | |
| rural area or small village n (%) | 12 (40.00) | 11 (36.67) | ns | |
| Houshold member(s) | with family member n (%) | 16 (53.33) | 21 (70.00) | ns |
| none n (%) | 14 (46.67) | 9 (30.00) | ns | |
| Type of stroke | hemorrhagic n (%) | - | 6 (20.00) | nd |
| ischemic n (%) | - | 23 (76.67) | nd | |
| ischemic → hemorrhagic n (%) | - | 1 (3.33) | nd | |
| Time from stroke incident to dental examination and saliva sampling | (mean ± SD) | - | 46.78 ± 4.71 | nd |
| Numbers of strokes in the patient’s life | 1 | - | 26 (86.67) | nd |
| 2 | - | 4 (13.33) | nd | |
| Cognitive and physical functional status | ACE III (mean ± SD) | 97.07 ± 1.26 | 68.80 ± 21.79 | <0.0001 |
| BI (mean ± SD) | 20 ± 0 | 11.10 ± 3.85 | <0.0001 | |
| FIM (mean ± SD) | 125.2 ± 0.66 | 86.73 ± 31.14 | <0.0001 | |
| BBS (mean ± SD) | 55.47 ± 0.5 | 31.03 ± 16.50 | <0.0001 | |
| Other disorders | hypertension n (%) | 20 (66.67) | 22 (73.33) | ns |
| diabetes n (%) | 8 (26.67) | 8 (26.67) | ns | |
| epilepsy n (%) | 3 (10.00) | 3 (10.00) | ns | |
| arteriosclerosis n (%) | 6 (20) | 7 (23.33) | ns | |
| gout n (%) | 1 (3.33) | 2 (6.67) | ns | |
| limb thrombosis n (%) | 2 (6.67) | 2 (6.67) | ns | |
| atrial fibrillation n (%) | 3 (10.00) | 4 (13.33) | ns | |
| Medications | <5 drugs/day n (%) | 11 (36.67) | 12 (40.00) | ns |
| ≥5 drugs/day n (%) | 16 (53.33) | 18 (60.00) | ns | |
| Control n = 30 | Study n = 30 | p-Value | |
|---|---|---|---|
| Caries prevalence (%), i.e., percentage of individuals with DMFT > 0 | 100.00 | 100.00 | ns |
| DT | 3.2 ± 1.2 | 2.50 ± 3.15 | ns |
| MT | 10.5 ± 5.8 | 17.50 ± 11.41 | 0.0038 |
| FT | 8 ± 2.1 | 3.13 ± 4.97 | <0.0001 |
| DMFT | 25 ± 5.3 | 23.13 ± 7.32 | ns |
| <5 | 0 (0.00) | 0 (0.00) | ns |
| 5–9 | 3 (10.00) | 1 (3.33) | ns |
| 10–14 | 1 (3.33) | 3 (10.00) | ns |
| 15–19 | 5 (16.67) | 5 (16.67) | ns |
| 20–25 | 2 (6.66) | 6 (20.00) | ns |
| >25 | 19 (63.33) | 15 (50.00) | ns |
| GI (six completely edentulous patients were excluded from calculations, i.e., n = 24) | 0.74 ± 0.2 | 0.83 ± 0.86 | ns |
| Number of patients without gingivitis n (%) | 15 (50.00) | 8 (33.33) | ns |
| Number of patients with mild gingivitis n (%) | 8 (33.33) | 9 (37.50) | ns |
| Number of patients with moderate gingivitis n (%) | 4 (16.67) | 4 (16.67) | ns |
| Number of patients with severe gingivitis n (%) | 3 (12.50) | 3 (12.50) | ns |
| PlI (six completely edentulous patients were excluded from calculations, i.e., n = 24) | 1.18 ± 0.58 | 1.29 ± 0.98 | ns |
| Number of patients with excellent hygiene n (%) | 15 (50.00) | 4 (16.67) | ns |
| Number of patients with good hygiene n (%) | 9 (37.50) | 9 (37.50) | ns |
| Number of patients with satisfactory hygiene n (%) | 5 (20.83) | 6 (25.00) | ns |
| Number of patients with unsatisfactory hygiene n (%) | 1 (3.33) | 5 (20.83) | <0.0001 |
| Control n = 30 | Study n = 30 | p-Value | |
|---|---|---|---|
| NWS flow rate (mL/min) | 0.33 ± 0.09 | 0.42 ± 0.25 | ns |
| SWS flow rate (mL/min) | 0.91 ± 0.26 | 0.68 ± 0.32 | 0.0036 |
| TP NWS (μg/mL) | 1213 ± 196.4 | 1159 ± 270.1 | ns |
| TP SWS (μg/mL) | 1307 ± 170.4 | 968.2 ± 247 | <0.0001 |
| Dependent Variables | Independent Variables | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Stroke | Gender: Male | Age | ACE III | BI | FIM | BBS | NWS Flow | SWS Flow | |
| Px NWS | 0.019 (−0.011–0.049), p = 0.218 | 0.003 (−0.009–0.016), p = 0.6 | 0 (0–0.001), p = 0.191 | 0 (−0.001–0), p = 0.143 | −0.002 (−0.006–0.001), p = 0.228 | 0 (−0.001–0), p = 0.297 | 0.001 (0–0.002), p = 0.027 * | −0.007 (−0.04–0.027), p = 0.705 | 0.02 (−0.001–0.042), p = 0.07 |
| Px SWS | 0.042 (0.008–0.077), p = 0.021 * | −0.002 (−0.016–0.012), p = 0.784 | 0 (−0.001–0.001), p = 0.822 | 0 (−0.001–0), p = 0.149 | 0 (−0.004–0.005), p = 0.829 | −0.001 (−0.002–0), p = 0.077 | 0.001 (0–0.002), p = 0.106 | 0.033 (−0.006–0.072), p = 0.103 | 0.013 (−0.012–0.038), p = 0.321 |
| CAT NWS | 0.119 (−0.404–0.641), p = 0.658 | −0.071 (−0.286–0.143), p = 0.518 | −0.006 (−0.015–0.003), p = 0.204 | 0.003 (−0.005–0.011), p = 0.482 | −0.062 (−0.125–0.001), p = 0.058 | −0.011 (−0.023–0.001), p = 0.074 | 0.025 (0.007–0.042), p = 0.008 * | −0.166 (−0.758–0.426), p = 0.586 | 0.038 (−0.339–0.415), p = 0.844 |
| CAT SWS | −0.236 (−0.755–0.283), p = 0.377 | −0.01 (−0.223–0.204), p = 0.928 | −0.009 (−0.018–0), p = 0.049 * | −0.006 (−0.014–0.001), p = 0.109 | −0.029 (−0.092–0.033), p = 0.364 | 0.003 (−0.008–0.015), p = 0.58 | −0.015 (−0.032–0.003), p = 0.101 | 0.222 (−0.366–0.811), p = 0.463 | −0.005 (−0.38–0.369), p = 0.979 |
| SOD NWS | 4.192 (−1.469–9.852), p = 0.153 | −1.388 (−3.717–0.94), p = 0.248 | 0.042 (−0.053–0.137), p = 0.39 | 0.02 (−0.065–0.105), p = 0.648 | 0.262 (−0.421–0.945), p = 0.455 | −0.084 (−0.213–0.045), p = 0.209 | 0.11 (−0.079–0.299), p = 0.26 | −0.485 (−6.902–5.933), p = 0.883 | −1.399 (−5.482–2.684), p = 0.505 |
| SOD SWS | −4.672 (−13.971–4.627), p = 0.329 | 3.338 (−0.487–7.164), p = 0.093 | 0.114 (−0.042–0.27), p = 0.157 | 0.02 (−0.119–0.159), p = 0.776 | −0.537 (−1.658–0.584), p = 0.352 | 0.089 (−0.123–0.301), p = 0.415 | −0.044 (−0.354–0.266), p = 0.784 | −6.139 (−16.68–4.403), p = 0.259 | 0.227 (−6.479–6.934), p = 0.947 |
| UA NWS | 5.399 (−12.355–23.153), p = 0.554 | 1.604 (−5.7–8.908), p = 0.669 | 0.112 (−0.186–0.409), p = 0.465 | −0.124 (−0.39–0.142), p = 0.364 | −0.15 (−2.291–1.99), p = 0.891 | 0.162 (−0.243–0.567), p = 0.437 | −0.285 (−0.877–0.307), p = 0.349 | 3.155 (−16.972–23.281), p = 0.76 | −7.858 (−20.662–4.946), p = 0.235 |
| UA SWS | −5.194 (−35.68–25.292), p = 0.74 | 7.91 (−4.632–20.452), p = 0.222 | −0.117 (−0.628–0.394), p = 0.655 | −0.062 (−0.518–0.395), p = 0.792 | −3.226 (−6.902–0.449), p = 0.092 | 0.069 (−0.627–0.765), p = 0.846 | 0.249 (−0.767–1.266), p = 0.633 | 7.454 (−27.106–42.014), p = 0.674 | 6.264 (−15.722–28.251), p = 0.579 |
| GSH NWS | −0.276 (−4.439–3.887), p = 0.897 | −0.073 (−1.786–1.64), p = 0.934 | −0.027 (−0.097–0.043), p = 0.456 | −0.064 (−0.126–0.001), p = 0.05 | 0.189 (−0.313–0.691), p = 0.463 | 0.04 (−0.055–0.135), p = 0.41 | −0.078 (−0.217–0.06), p = 0.273 | 3.333 (−1.387–8.053), p = 0.172 | −0.383 (−3.386–2.619), p = 0.803 |
| GSH SWS | −16.637 (−24.716–8.557), p < 0.001 * | −0.809 (−4.133–2.515), p = 0.635 | 0.061 (−0.074–0.197), p = 0.38 | 0.301 (0.18–0.422), p < 0.001 * | 0.278 (−0.696–1.252), p = 0.579 | −0.004 (−0.188–0.181), p = 0.967 | −0.049 (−0.318–0.221), p = 0.724 | −2.611 (−11.771–6.548), p = 0.579 | −0.747 (−6.574–5.08), p = 0.803 |
| TAC NWS | 0.551 (−0.82–1.923), p = 0.434 | 0.08 (−0.484–0.644), p = 0.783 | 0.011 (−0.012–0.034), p = 0.334 | −0.004 (−0.025–0.016), p = 0.684 | −0.083 (−0.248–0.082), p = 0.33 | −0.013 (−0.045–0.018), p = 0.406 | 0.044 (−0.001–0.09), p = 0.062 | −0.903 (−2.457–0.652), p = 0.261 | 1.099 (0.11–2.088), p = 0.034 * |
| TAC SWS | −0.808 (−2.428–0.812), p = 0.333 | −0.772 (−1.439–0.106), p = 0.028 * | −0.002 (−0.029–0.025), p = 0.903 | 0.005 (−0.019–0.029), p = 0.694 | −0.173 (−0.368–0.022), p = 0.089 | 0.043 (0.006–0.08), p = 0.027 * | −0.076 (−0.13–0.022), p = 0.008 * | 0.113 (−1.724–1.949), p = 0.905 | 0.975 (−0.193–2.144), p = 0.108 |
| TOS NWS | 21.886 (−44.111–87.883), p = 0.519 | −2.844 (−29.996–24.307), p = 0.838 | 0.144 (−0.963–1.25), p = 0.8 | −0.19 (−1.178–0.798), p = 0.708 | −2.317 (−10.275–5.641), p = 0.571 | −0.826 (−2.333–0.68), p = 0.287 | 1.356 (−0.844–3.557), p = 0.233 | −20.546 (−95.364–54.272), p = 0.593 | 25.999 (−21.598–73.596), p = 0.289 |
| TOS SWS | 30.97 (−126.85–188.789), p = 0.702 | 34.294 (−30.633–99.222), p = 0.306 | 1.398 (−1.248–4.045), p = 0.305 | 0.451 (−1.911–2.813), p = 0.71 | −16.533 (−35.562–2.496), p = 0.095 | −0.255 (−3.858–3.347), p = 0.89 | 0.171 (−5.092–5.434), p = 0.95 | 103.489 (−75.423–282.401), p = 0.262 | −106.848 (−220.666–6.971), p = 0.072 |
| OSI NWS | −6.811 (−53.35–39.727), p = 0.775 | −0.109 (−19.255–19.037), p = 0.991 | −0.219 (−1–0.561), p = 0.584 | −0.16 (−0.856–0.537), p = 0.655 | 0.072 (−5.539–5.684), p = 0.98 | 0.092 (−0.971–1.154), p = 0.866 | −0.536 (−2.088–1.015), p = 0.501 | 23.291 (−29.467–76.049), p = 0.391 | −14.16 (−47.723–19.404), p = 0.412 |
| OSI SWS | 32.132 (−20.171–84.434), p = 0.234 | 27.376 (5.858–48.893), p = 0.016 * | 0.294 (−0.583–1.171), p = 0.514 | 0.052 (−0.731–0.834), p = 0.898 | −1.561 (−7.867–4.745), p = 0.63 | −0.932 (−2.126–0.262), p = 0.132 | 1.752 (0.008–3.497), p = 0.054 | 43.924 (−15.369–103.216), p = 0.153 | −43.958 (−81.678–6.238), p = 0.027 * |
| AGE NWS | 2.145 (−124.129–128.42), p = 0.974 | −16.176 (−68.126–35.774), p = 0.544 | −0.115 (−2.232–2.002), p = 0.916 | −1.588 (−3.478–0.301), p = 0.106 | −6.18 (−21.406–9.045), p = 0.43 | 0.936 (−1.946–3.818), p = 0.527 | −1.245 (−5.455–2.966), p = 0.565 | 118.067 (−25.084–261.219), p = 0.112 | 38.166 (−52.903–129.235), p = 0.415 |
| AGE SWS | 149.753 (18.494–281.011), p = 0.03 * | 6.864 (−47.136–60.865), p = 0.804 | 0.414 (−1.787–2.614), p = 0.714 | 0.117 (−1.847–2.081), p = 0.907 | 14.242 (−1.584–30.069), p = 0.084 | −2.386 (−5.382–0.61), p = 0.125 | 0.918 (−3.459–5.295), p = 0.683 | −119.668 (−268.47–29.133), p = 0.121 | −122.463 (−217.127–27.8), p = 0.014 * |
| AOPP NWS | 46.735 (16.635–76.835), p = 0.004 * | 2.443 (−9.94–14.826), p = 0.701 | 0.026 (−0.478–0.531), p = 0.919 | 0.14 (−0.31–0.59), p = 0.545 | 3.003 (−0.626–6.632), p = 0.111 | −0.574 (−1.261–0.113), p = 0.108 | −0.105 (−1.109–0.898), p = 0.838 | −16.026 (−50.148–18.097), p = 0.362 | −11.351 (−33.059–10.357), p = 0.31 |
| AOPP SWS | 47.369 (29.289–65.45), p < 0.001 * | 1.939 (−5.499–9.378), p = 0.612 | −0.024 (−0.327–0.279), p = 0.879 | 0.058 (−0.213–0.328), p = 0.677 | 1.815 (−0.365–3.995), p = 0.109 | −0.043 (−0.456–0.37), p = 0.839 | −0.414 (−1.017–0.188), p = 0.184 | −30.24 (−50.737–9.743), p = 0.006 * | −23.316 (−36.356–10.277), p = 0.001 * |
| LOOH NWS | 163.531 (−17.81–344.873), p = 0.083 | −14.451 (−89.056–60.153), p = 0.706 | 0.488 (−2.552–3.529), p = 0.754 | −0.917 (−3.631–1.796), p = 0.511 | 1.999 (−19.866–23.864), p = 0.858 | 1.785 (−2.354–5.924), p = 0.402 | −3.443 (−9.49–2.604), p = 0.27 | 41.144 (−164.434–246.722), p = 0.697 | −7.547 (−138.33–123.235), p = 0.91 |
| LOOH SWS | 300.808 (128.923–472.693), p = 0.001 * | 27.154 (−43.56–97.868), p = 0.455 | 1.502 (−1.38–4.384), p = 0.312 | −1.306 (−3.878–1.267), p = 0.325 | −11.257 (−31.982–9.468), p = 0.292 | 1.064 (−2.859–4.987), p = 0.597 | 1.491 (−4.241–7.223), p = 0.612 | −89.548 (−284.405–105.31), p = 0.372 | −238.519 (−362.482–114.556), p < 0.001 * |
| ACE III | BI | FIM | BBS | NWS Flow | SWS Flow | ACE III | BI | FIM | BBS | NWS Flow | SWS Flow | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| r-value | p-value | |||||||||||
| Px NWS | −0.13 | −0.26 | −0.15 | 0.05 | −0.15 | 0.27 | 0.52 | 0.17 | 0.44 | 0.80 | 0.44 | 0.15 |
| CAT NWS | 0.04 | −0.43 | −0.28 | −0.03 | −0.07 | 0.07 | 0.83 | 0.02 | 0.15 | 0.90 | 0.71 | 0.73 |
| SOD NWS | 0.04 | 0.04 | −0.09 | 0.05 | −0.03 | −0.34 | 0.85 | 0.82 | 0.63 | 0.80 | 0.89 | 0.06 |
| UA NWS | −0.23 | 0.06 | −0.02 | −0.10 | −0.08 | −0.38 | 0.22 | 0.78 | 0.94 | 0.60 | 0.67 | 0.04 |
| GSH NWS | −0.34 | 0.16 | −0.01 | −0.12 | 0.27 | 0.05 | 0.07 | 0.40 | 0.95 | 0.55 | 0.16 | 0.80 |
| TAC NWS | 0.01 | −0.17 | −0.02 | 0.13 | −0.18 | 0.21 | 0.95 | 0.39 | 0.93 | 0.51 | 0.35 | 0.27 |
| TOS NWS | −0.13 | −0.31 | −0.27 | −0.13 | −0.02 | 0.12 | 0.49 | 0.10 | 0.15 | 0.51 | 0.90 | 0.52 |
| OSI NWS | −0.14 | −0.08 | −0.16 | −0.19 | 0.16 | −0.10 | 0.46 | 0.68 | 0.41 | 0.32 | 0.41 | 0.58 |
| AGE NWS | −0.23 | −0.16 | −0.17 | −0.23 | 0.19 | 0.16 | 0.23 | 0.40 | 0.39 | 0.23 | 0.31 | 0.40 |
| AOPP NWS | −0.16 | −0.09 | −0.32 | −0.27 | −0.16 | −0.29 | 0.41 | 0.63 | 0.09 | 0.15 | 0.41 | 0.12 |
| LOOH NWS | −0.08 | 0.07 | 0.00 | −0.11 | 0.07 | 0.19 | 0.68 | 0.73 | 0.99 | 0.56 | 0.73 | 0.32 |
| Px SWS | −0.24 | −0.21 | −0.29 | −0.18 | 0.23 | 0.11 | 0.22 | 0.28 | 0.12 | 0.34 | 0.23 | 0.58 |
| CAT SWS | −0.36 | −0.35 | −0.41 | −0.45 | 0.10 | 0.05 | 0.05 | 0.07 | 0.03 | 0.01 | 0.61 | 0.81 |
| SOD SWS | 0.08 | −0.02 | 0.13 | 0.14 | −0.31 | −0.11 | 0.70 | 0.93 | 0.50 | 0.48 | 0.10 | 0.58 |
| UA SWS | −0.02 | −0.29 | −0.12 | −0.04 | 0.02 | 0.19 | 0.91 | 0.12 | 0.54 | 0.83 | 0.94 | 0.32 |
| GSH SWS | 0.84 | 0.22 | 0.35 | 0.25 | 0.17 | 0.32 | 0.00 | 0.25 | 0.05 | 0.19 | 0.38 | 0.08 |
| TAC SWS | 0.14 | −0.24 | −0.14 | −0.30 | 0.20 | 0.43 | 0.46 | 0.21 | 0.49 | 0.11 | 0.29 | 0.02 |
| TOS SWS | −0.13 | −0.40 | −0.33 | −0.30 | 0.04 | −0.10 | 0.52 | 0.03 | 0.09 | 0.12 | 0.85 | 0.60 |
| OSI SWS | −0.13 | −0.12 | −0.11 | 0.06 | −0.02 | −0.27 | 0.50 | 0.55 | 0.58 | 0.78 | 0.90 | 0.16 |
| AGE SWS | −0.30 | 0.09 | −0.23 | −0.12 | −0.34 | −0.79 | 0.11 | 0.63 | 0.24 | 0.55 | 0.06 | 0.00 |
| AOPP SWS | −0.26 | 0.16 | −0.07 | −0.10 | −0.47 | −0.76 | 0.17 | 0.41 | 0.74 | 0.60 | 0.01 | 0.00 |
| LOOH SWS | −0.25 | 0.04 | 0.05 | 0.13 | −0.43 | −0.77 | 0.20 | 0.84 | 0.80 | 0.52 | 0.02 | 0.00 |
| AUC | 95% Confidence Interval (CI) | Cut Off | Sensitivity% | 95% CI | Specificity% | 95% CI | |
|---|---|---|---|---|---|---|---|
| Px | 0.8078 | 0.6880 to 0.9276 | >0.03932 | 76.67 | 59.07% to 88.21% | 73.33 | 55.55% to 85.82% |
| CAT | 0.8122 | 0.7003 to 0.9241 | >0.3415 | 76.67 | 59.07% to 88.21% | 70 | 52.12% to 83.34% |
| SOD | 0.6189 | 0.4753 to 0.7625 | >12.88 | 63.33 | 45.51% to 78.13% | 53.33 | 36.14% to 69.77% |
| UA | 0.7611 | 0.6403 to 0.8819 | >55.47 | 70 | 52.12% to 83.34% | 63.33 | 45.51% to 78.13% |
| GSH | 0.5367 | 0.3891 to 0.6843 | >13.22 | 50 | 33.15% to 66.85% | 50 | 33.15% to 66.85% |
| TAC | 0.6144 | 0.4645 to 0.7644 | >3.036 | 56.67 | 39.20% to 72.62% | 56.67 | 39.20% to 72.62% |
| TOS | 0.7222 | 0.5938 to 0.8507 | >189.0 | 63.33 | 45.51% to 78.13% | 60 | 42.32% to 75.41% |
| AGE | 0.8078 | 0.6889 to 0.9267 | >361.7 | 80 | 62.69% to 90.49% | 76.67 | 59.07% to 88.21% |
| AOPP | 0.8711 | 0.7653 to 0.9770 | >32.58 | 83.33 | 66.44% to 92.66% | 76.67 | 59.07% to 88.21% |
| LOOH | 0.8567 | 0.7602 to 0.9531 | >359.5 | 86.67 | 70.32% to 94.69% | 80 | 62.69% to 90.49% |
| AUC | 95% Confidence Interval (CI) | Cut Off | Sensitivity% | 95% CI | Specificity% | 95% CI | |
|---|---|---|---|---|---|---|---|
| Px | 0.9478 | 0.8916 to 1.000 | >0.04009 | 90 | 74.38% to 96.54% | 90 | 74.38% to 96.54% |
| CAT | 0.7578 | 0.6194 to 0.8962 | >0.5207 | 76.67 | 59.07% to 88.21% | 66.67 | 48.78% to 80.77% |
| SOD | 0.6422 | 0.4994 to 0.7850 | <29.16 | 63.33 | 45.51% to 78.13% | 60 | 42.32% to 75.41% |
| UA | 0.6533 | 0.5101 to 0.7966 | >57.45 | 53.33 | 36.14% to 69.77% | 60 | 42.32% to 75.41% |
| GSH | 1 | 1.000 to 1.000 | <42.71 | 100 | 88.65% to 100.0% | 100 | 88.65% to 100.0% |
| TAC | 0.5344 | 0.3747 to 0.6942 | >3.893 | 56.67 | 39.20% to 72.62% | 53.33 | 36.14% to 69.77% |
| TOS | 0.8822 | 0.7934 to 0.9711 | >286.4 | 86.67 | 70.32% to 94.69% | 83.33 | 66.44% to 92.66% |
| AGE | 0.7522 | 0.6300 to 0.8744 | >302.2 | 73.33 | 55.55% to 85.82% | 66.67 | 48.78% to 80.77% |
| AOPP | 0.9911 | 0.9763 to 1.000 | >54.50 | 96.67 | 83.33% to 99.83% | 93.33 | 78.68% to 98.82% |
| LOOH | 0.9833 | 0.9604 to 1.000 | >548.2 | 93.33 | 78.68% to 98.82% | 90 | 74.38% to 96.54% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gerreth, P.; Maciejczyk, M.; Zalewska, A.; Gerreth, K.; Hojan, K. Comprehensive Evaluation of the Oral Health Status, Salivary Gland Function, and Oxidative Stress in the Saliva of Patients with Subacute Phase of Stroke: A Case-Control Study. J. Clin. Med. 2020, 9, 2252. https://doi.org/10.3390/jcm9072252
Gerreth P, Maciejczyk M, Zalewska A, Gerreth K, Hojan K. Comprehensive Evaluation of the Oral Health Status, Salivary Gland Function, and Oxidative Stress in the Saliva of Patients with Subacute Phase of Stroke: A Case-Control Study. Journal of Clinical Medicine. 2020; 9(7):2252. https://doi.org/10.3390/jcm9072252
Chicago/Turabian StyleGerreth, Piotr, Mateusz Maciejczyk, Anna Zalewska, Karolina Gerreth, and Katarzyna Hojan. 2020. "Comprehensive Evaluation of the Oral Health Status, Salivary Gland Function, and Oxidative Stress in the Saliva of Patients with Subacute Phase of Stroke: A Case-Control Study" Journal of Clinical Medicine 9, no. 7: 2252. https://doi.org/10.3390/jcm9072252
APA StyleGerreth, P., Maciejczyk, M., Zalewska, A., Gerreth, K., & Hojan, K. (2020). Comprehensive Evaluation of the Oral Health Status, Salivary Gland Function, and Oxidative Stress in the Saliva of Patients with Subacute Phase of Stroke: A Case-Control Study. Journal of Clinical Medicine, 9(7), 2252. https://doi.org/10.3390/jcm9072252








