Mental Disorders, Musculoskeletal Disorders and Income-Driven Patterns: Evidence from the Global Burden of Disease Study 2017
Abstract
1. Introduction
2. Methods
2.1. Geography and Metrics
2.2. Mental Disorders and Musculoskeletal Disorders
2.3. Mortality and Causes of Death
2.4. Nonfatal Health Loss as Expressed by Years Lived with Disability (YLDs)
2.5. Disability-Adjusted Life-Years (DALYs)
2.6. Assessment of Socioeconomic Factors and Health System Performance
2.7. Statistical Analysis
2.7.1. Correlation Analysis
2.7.2. Linear Mixed Model Analysis
3. Results
3.1. Trends in DALYs Due to Mental and MSK Disorders and Annualized Rates of Change (ARC) between 1990 and 2017
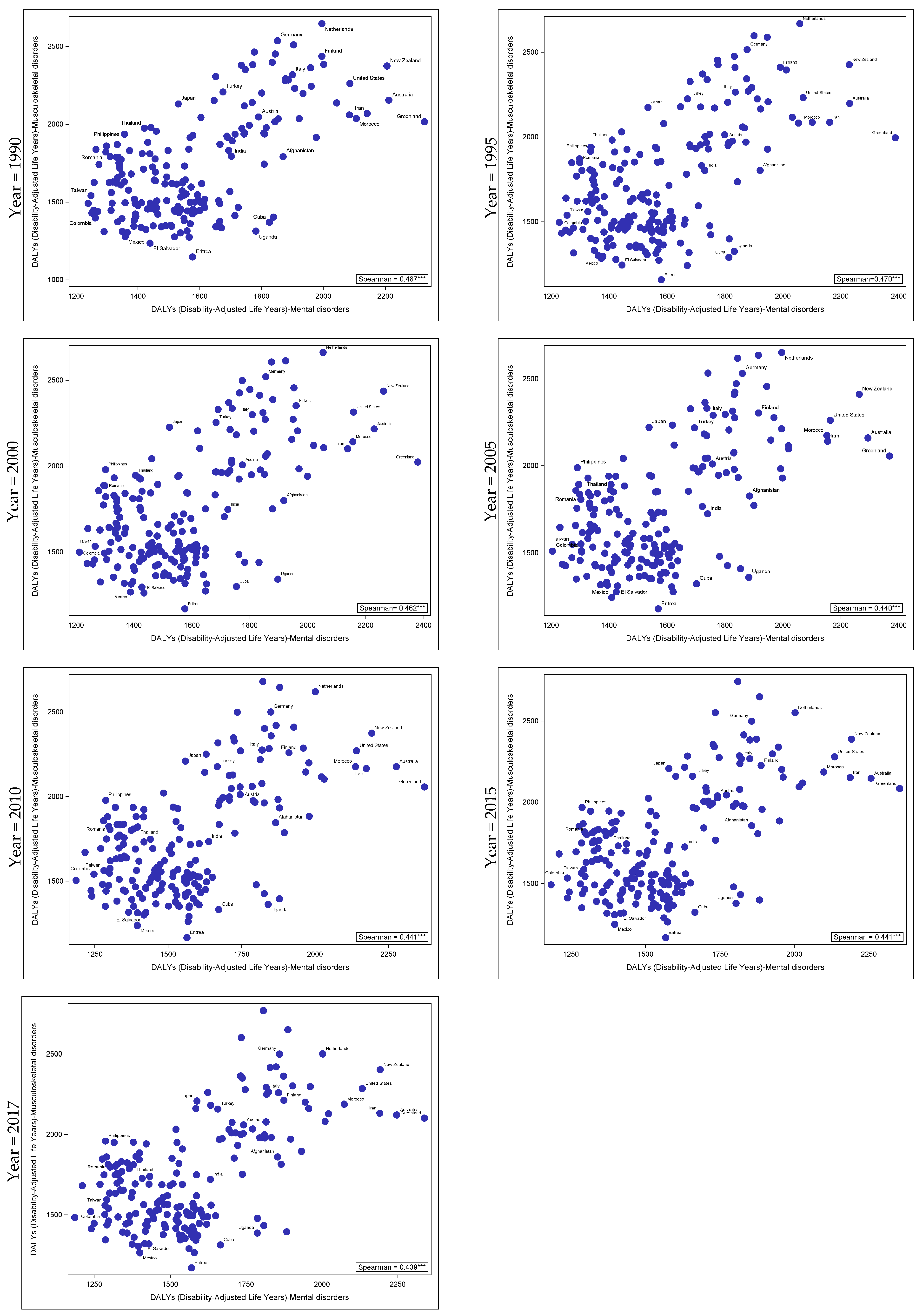
3.2. Correlation Trends in DALYs Attributed to Mental and MSK Disorders between 1990 and 2017
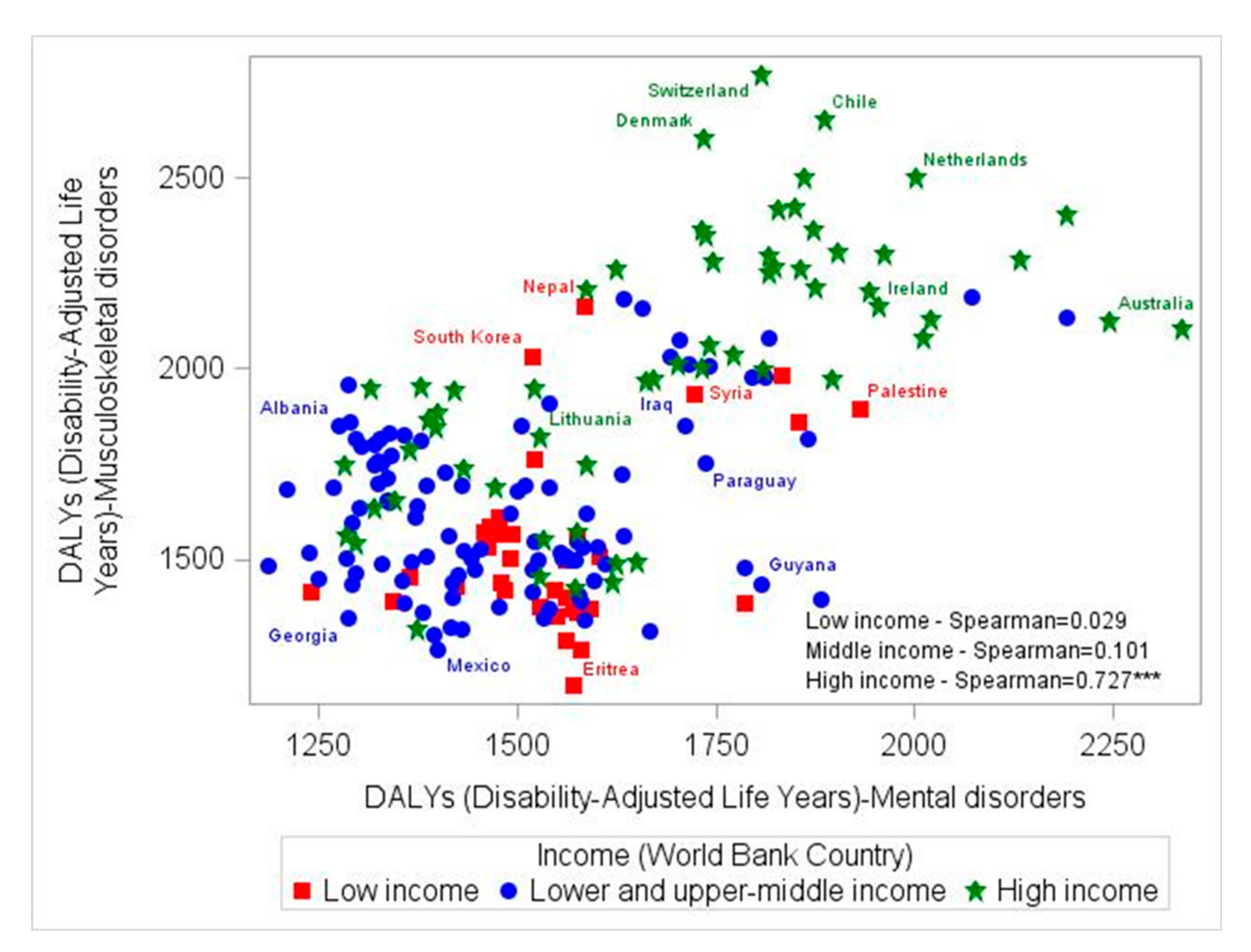
3.3. Correlation Trends in DALYs Attributed to Mental and MSK Disorders between 1990 and 2017, by Country-Income Level
3.4. Correlation Trends in YLDs Attributed to Mental and MSK Disorders between 1990 and 2017, in Both Sexes, by Males and Females and by Country-Income Level
4. Discussion
5. Strengths and Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Steel, Z.; Marnane, C.; Iranpour, C.; Chey, T.; Jackson, J.W.; Patel, V.; Silove, D. The global prevalence of common mental disorders: A systematic review and meta-analysis 1980–2013. Int. J. Epidemiol. 2014, 43, 476–493. [Google Scholar] [CrossRef] [PubMed]
- Phyomaung, P.P.; Dubowitz, J.; Cicuttini, F.M.; Fernando, S.; Wluka, A.E.; Raaijmaakers, P.; Wang, Y.; Urquhart, D.M. Are depression, anxiety and poor mental health risk factors for knee pain? A systematic review. BMC Musculoskelet. Disord. 2014, 15, 10. [Google Scholar] [CrossRef] [PubMed]
- Del Campo, M.T.; Romo, P.E.; de la Hoz, R.E.; Villamor, J.M.; Mahíllo-Fernández, I. Anxiety and depression predict musculoskeletal disorders in health care workers. Arch. Environ. Occup. Health 2017, 72, 39–44. [Google Scholar] [CrossRef] [PubMed]
- Crofford, L.J. Psychological Aspects of Chronic Musculoskeletal Pain. Best Pract. Res. Clin. Rheumatol. 2015, 29, 147–155. [Google Scholar] [CrossRef]
- Williams, A.; Kamper, S.J.; Wiggers, J.H.; O’Brien, K.M.; Lee, H.; Wolfenden, L.; Yoong, S.L.; Robson, E.; McAuley, J.H.; Hartvigsen, J.; et al. Musculoskeletal conditions may increase the risk of chronic disease: A systematic review and meta-analysis of cohort studies. BMC Med. 2018, 16, 167. [Google Scholar] [CrossRef]
- Roux, C.; Guillemin, F.; Boini, S.; Longuetaud, F.; Arnault, N.; Hercberg, S.; Briancon, S. Impact of musculoskeletal disorders on quality of life: An inception cohort study. Ann. Rheum. Dis. 2005, 64, 606–611. [Google Scholar] [CrossRef]
- Evans, S.; Banerjee, S.; Leese, M.; Huxley, P. The impact of mental illness on quality of life: A comparison of severe mental illness, common mental disorder and healthy population samples. Qual. Life Res. 2007, 16, 17–29. [Google Scholar] [CrossRef]
- Härter, M.; Woll, S.; Reuter, K.; Wunsch, A.; Bengel, J. Recognition of psychiatric disorders in musculoskeletal and cardiovascular rehabilitation patients. Arch. Phys. Med. Rehabil. 2004, 85, 1192–1197. [Google Scholar] [CrossRef]
- Australian Institute of Health and Welfare. When Musculoskeletal Conditions and Mental Disorders Occur Together. AIHW Bulletin No. 80. 2010. Available online: https://www.aihw.gov.au/getmedia/dc68198e-f447-40e8-90ed-b7b92266a0c6/11155.pdf.aspx?inline=true (accessed on 5 January 2020).
- GBD 2017 Causes of Death Collaborators. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef]
- Briggs, A.M.; Woolf, A.D.; Dreinhöfer, K.; Homb, N.; Hoy, D.G.; Kopansky-Giles, D.; Åkesson, K.; March, L. Reducing the global burden of musculoskeletal conditions. Bull. World Health Organ. 2018, 96, 366–368. [Google Scholar] [CrossRef]
- Duffield, S.J.; Ellis, B.M.; Goodson, N.; Walker-Bone, K.; Conaghan, P.G.; Margham, T.; Loftis, T. The contribution of musculoskeletal disorders in multimorbidity: Implications for practice and policy. Best Pract. Res. Clin. Rheumatol. 2017, 31, 129–144. [Google Scholar] [CrossRef] [PubMed]
- GBD 2017 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1859–1922. [Google Scholar] [CrossRef]
- Ashnagar, M.; Sartang, A.G.; Habibi, E. Assessment Mental Health and Musculoskeletal Disorders among Military Personnel in Bandar Abbas (Iran) in 2016. Iran. J. Health Saf. Environ. 2017, 4, 752–757. [Google Scholar]
- Stubbs, B.; Veronese, N.; Vancampfort, D.; Thompson, T.; Kohler, C.; Schofield, P.; Solmi, M.; Mugisha, J.; Kahl, K.G.; Pillinger, T.; et al. Lifetime self-reported arthritis is associated with elevated levels of mental health burden: A multi-national cross sectional study across 46 low- and middle-income countries. Sci. Rep. 2017, 7, 7138. [Google Scholar] [CrossRef]
- Choong, P.; Brooks, P. Achievements during the Bone and Joint Decade 2000-2010. Best Pract. Res. Clin. Rheumatol. 2012, 26, 173–181. [Google Scholar] [CrossRef]
- Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [CrossRef]
- GATHER. Available online: http://gather-statement.org/ (accessed on 29 July 2018).
- GBD 2017 Mortality Collaborators Global, regional, and national age-sex-specific mortality and life expectancy, 1950-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1684–1735. [CrossRef]
- An Integrative Metaregression Framework for Descriptive Epidemiology av Abraham D Flaxman, Theo Vos, Christopher J L Murray (Bok). Available online: https://www.bokus.com/bok/9780295991849/an-integrative-metaregression-framework-for-descriptive-epidemiology/ (accessed on 29 July 2018).
- GBD 2017 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef]
- Barber, R.M.; Fullman, N.; Sorensen, R.J.D.; Bollyky, T.; McKee, M.; Nolte, E.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; et al. Healthcare Access and Quality Index based on mortality from causes amenable to personal health care in 195 countries and territories, 1990–2015: A novel analysis from the Global Burden of Disease Study 2015. Lancet 2017, 390, 231–266. [Google Scholar] [CrossRef]
- New Country Classifications by Income Level: 2018–2019. Available online: https://blogs.worldbank.org/opendata/new-country-classifications-income-level-2018-2019 (accessed on 19 June 2019).
- Akoglu, H. User’s guide to correlation coefficients. Turk. J. Emerg Med. 2018, 18, 91–93. [Google Scholar] [CrossRef]
- Caballero, F.F.; Soulis, G.; Engchuan, W.; Sánchez-Niubó, A.; Arndt, H.; Ayuso-Mateos, J.L.; Haro, J.M.; Chatterji, S.; Panagiotakos, D.B. Advanced analytical methodologies for measuring healthy ageing and its determinants, using factor analysis and machine learning techniques: The ATHLOS project. Sci. Rep. 2017, 7, 43955. [Google Scholar] [CrossRef] [PubMed]
- Hooten, W.M. Chronic Pain and Mental Health Disorders: Shared Neural Mechanisms, Epidemiology, and Treatment. Mayo Clin. Proc. 2016, 91, 955–970. [Google Scholar] [CrossRef] [PubMed]
- Arnow, B.A.; Hunkeler, E.M.; Blasey, C.M.; Lee, J.; Constantino, M.J.; Fireman, B.; Kraemer, H.C.; Dea, R.; Robinson, R.; Hayward, C. Comorbid depression, chronic pain, and disability in primary care. Psychosom. Med. 2006, 68, 262–268. [Google Scholar] [CrossRef]
- Blozik, E.; Laptinskaya, D.; Herrmann-Lingen, C.; Schaefer, H.; Kochen, M.M.; Himmel, W.; Scherer, M. Depression and anxiety as major determinants of neck pain: A cross-sectional study in general practice. BMC Musculoskelet. Disord. 2009, 10, 13. [Google Scholar] [CrossRef] [PubMed]
- Stray, L.L.; Kristensen, Ø.; Lomeland, M.; Skorstad, M.; Stray, T.; Tønnessen, F.E. Motor regulation problems and pain in adults diagnosed with ADHD. Behav. Brain Funct. 2013, 9, 18. [Google Scholar] [CrossRef]
- Guy, J.A.; Knight, L.M.; Wang, Y.; Jerrell, J.M. Factors Associated With Musculoskeletal Injuries in Children and Adolescents With Attention-Deficit/Hyperactivity Disorder. Prim. Care Companion CNS Disord. 2016, 18. [Google Scholar] [CrossRef] [PubMed]
- Nakua, E.K.; Otupiri, E.; Dzomeku, V.M.; Owusu-Dabo, E.; Agyei-Baffour, P.; Yawson, A.E.; Folson, G.; Hewlett, S. Gender disparities of chronic musculoskeletal disorder burden in the elderly Ghanaian population: Study on global ageing and adult health (SAGE WAVE 1). BMC Musculoskelet. Disord. 2015, 16. [Google Scholar] [CrossRef]
- Miller, A.E.J.; MacDougall, J.D.; Tarnopolsky, M.A.; Sale, D.G. Gender differences in strength and muscle fiber characteristics. Europ. J. Appl. Physiol. 1993, 66, 254–262. [Google Scholar] [CrossRef]
- Maletic, V.; Raison, C.L. Neurobiology of depression, fibromyalgia and neuropathic pain. Front. Biosci. (Landmark Ed.) 2009, 14, 5291–5338. [Google Scholar] [CrossRef]
- Ross, R.L.; Jones, K.D.; Bennett, R.M.; Ward, R.L.; Druker, B.J.; Wood, L.J. Preliminary Evidence of Increased Pain and Elevated Cytokines in Fibromyalgia Patients with Defective Growth Hormone Response to Exercise. Open Immunol. J. 2010, 3, 9–18. [Google Scholar] [CrossRef]
- Derry, H.M.; Padin, A.C.; Kuo, J.L.; Hughes, S.; Kiecolt-Glaser, J.K. Sex Differences in Depression: Does Inflammation Play a Role? Curr. Psychiatry Rep. 2015, 17, 78. [Google Scholar] [CrossRef] [PubMed]
- Treaster, D.E.; Burr, D. Gender differences in prevalence of upper extremity musculoskeletal disorders. Ergonomics 2004, 47, 495–526. [Google Scholar] [CrossRef] [PubMed]
- Rebello, G. Musculoskeletal Disorders. In The Massachusetts General Hospital Guide to Medical Care in Patients with Autism Spectrum Disorder; Hazen, E.P., McDougle, C.J., Eds.; Current Clinical Psychiatry; Springer International Publishing: Cham, Switzerland, 2018; pp. 207–213. ISBN 978-3-319-94458-6. [Google Scholar]
- Brooks Holliday, S.; Ewing, B.A.; Storholm, E.D.; Parast, L.; D’Amico, E.J. Gender Differences in the Association between Conduct Disorder and Risky Sexual Behavior. J. Adolesc. 2017, 56, 75–83. [Google Scholar] [CrossRef]
- Yazdi, M.; Karimi Zeverdegani, S.; MollaAghaBabaee, A.H. Association of derived patterns of musculoskeletal disorders with psychological problems: A latent class analysis. Environ. Health Prev. Med. 2019, 24, 34. [Google Scholar] [CrossRef] [PubMed]
- Nerurkar, L.; Siebert, S.; McInnes, I.B.; Cavanagh, J. Rheumatoid arthritis and depression: An inflammatory perspective. Lancet Psychiatry 2019, 6, 164–173. [Google Scholar] [CrossRef]
- White, R.; Jain, S.; Giurgi-Oncu, C. Counterflows for mental well-being: What high-income countries can learn from low and middle-income countries. Int. Rev. Psychiatry 2014, 26, 602–606. [Google Scholar] [CrossRef]
- Foreman, K.J.; Marquez, N.; Dolgert, A.; Fukutaki, K.; Fullman, N.; McGaughey, M.; Pletcher, M.A.; Smith, A.E.; Tang, K.; Yuan, C.-W.; et al. Forecasting life expectancy, years of life lost, and all-cause and cause-specific mortality for 250 causes of death: Reference and alternative scenarios for 2016-40 for 195 countries and territories. Lancet 2018, 392, 2052–2090. [Google Scholar] [CrossRef]


| Mental Disorders | Definition/Estimation | Musculoskeletal Disorders | Definition/Estimation |
|---|---|---|---|
| aMeAD | the sum of DALYs attributed to total mental disorders (MDT) minus DALYs attributed to anxiety and depressive disorders | Rheumatoid arthritis | GBD original definition |
| Depressive disorders | the sum of DALYs for major depressive disorders and dysthymia | Osteoarthritis | GBD original definition |
| Major depressive disorders | GBD original definition | Low back pain disorders | GBD original definition |
| Anxiety disorders | GBD original definition | Neck pain disorders | GBD original definition |
| Attention deficit/hyperactivity disorder | GBD original definition | Gout disorders | GBD original definition |
| Idiopathic developmental intellectual disability | GBD original definition | Other musculoskeletal disorders | GBD original definition |
| Anorexia or bulimia nervosa (eating disorders) | the sum of DALYs attributed to anorexia or bulimia nervosa | - | - |
| Other mental disorders | GBD original definition | - | - |
| Schizophrenia | GBD original definition | - | - |
| Dysthymia | GBD original definition | - | - |
| Bipolar disorders | GBD original definition | - | - |
| Autism disorders | GBD original definition | - | - |
| Conduct disorders | GBD original definition | - | - |
| Other Disorders | Mental Disorders Sub-Categories | ||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year | Neoplasms | CVD | NeuroD | Injuries | MDT | aMeAD | Depressive Disorders | MDD | Dysthymia | Bipolar | Anxiety | EatingD | Autism Disorders | ADHD | Conduct Disorder | IDID | OMD | SZA | |
| MSK | 1990 | 0.105 | −0.089 | 0.038 | −0.319 | 0.487 | 0.630 | 0.144 | 0.051 | 0.339 | 0.276 | 0.548 | 0.461 | 0.130 | −0.303 | −0.002 | 0.073 | 0.470 | 0.602 |
| 1995 | 0.054 | −0.176 | 0.002 | −0.391 | 0.470 | 0.613 | 0.120 | 0.038 | 0.320 | 0.286 | 0.530 | 0.472 | 0.136 | −0.301 | 0.014 | 0.042 | 0.495 | 0.582 | |
| 2000 | 0.009 | −0.239 | −0.002 | −0.381 | 0.462 | 0.589 | 0.126 | 0.044 | 0.302 | 0.284 | 0.522 | 0.477 | 0.149 | −0.280 | 0.010 | 0.009 | 0.488 | 0.569 | |
| 2005 | −0.008 | −0.255 | 0.028 | −0.390 | 0.440 | 0.573 | 0.114 | 0.033 | 0.309 | 0.272 | 0.511 | 0.466 | 0.154 | −0.290 | 0.037 | 0.023 | 0.474 | 0.559 | |
| 2010 | −0.045 | −0.277 | 0.056 | −0.444 | 0.441 | 0.570 | 0.108 | 0.028 | 0.315 | 0.269 | 0.513 | 0.462 | 0.151 | −0.297 | 0.023 | 0.038 | 0.456 | 0.549 | |
| 2015 | −0.124 | −0.303 | 0.047 | −0.417 | 0.441 | 0.565 | 0.104 | 0.023 | 0.322 | 0.272 | 0.506 | 0.457 | 0.159 | −0.304 | 0.025 | 0.076 | 0.452 | 0.539 | |
| 2017 | −0.134 | −0.307 | 0.041 | −0.442 | 0.439 | 0.563 | 0.104 | 0.017 | 0.320 | 0.272 | 0.503 | 0.451 | 0.166 | −0.305 | 0.023 | 0.090 | 0.448 | 0.533 | |
| Other Disorders | Mental Disorders Sub-Categories | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year | Gender | Neoplasms | CVD | NeuroD | Injuries | MDT | aMeAD | Depressive Disorders | MDD | Dysthymia | Bipolar | Anxiety | EatingD | Autism Disorders | ADHD | Conduct Disorder | IDID | OMD | SZA | |
| MSK | 1990 | Females | −0.112 | −0.279 | 0.169 | −0.301 | 0.448 | 0.646 | 0.175 | 0.058 | 0.442 | 0.329 | 0.552 | 0.522 | −0.094 | −0.441 | −0.267 | 0.066 | 0.242 | 0.694 |
| 1995 | −0.139 | −0.318 | 0.154 | −0.339 | 0.439 | 0.637 | 0.148 | 0.034 | 0.440 | 0.336 | 0.548 | 0.533 | −0.089 | −0.427 | −0.269 | 0.042 | 0.275 | 0.674 | ||
| 2000 | −0.209 | −0.366 | 0.155 | −0.339 | 0.439 | 0.619 | 0.136 | 0.040 | 0.440 | 0.334 | 0.543 | 0.543 | −0.083 | −0.399 | −0.272 | 0.005 | 0.268 | 0.671 | ||
| 2005 | −0.240 | −0.357 | 0.200 | −0.330 | 0.434 | 0.600 | 0.140 | 0.041 | 0.445 | 0.318 | 0.530 | 0.529 | −0.079 | −0.399 | −0.284 | 0.015 | 0.239 | 0.661 | ||
| 2010 | −0.255 | −0.382 | 0.212 | −0.370 | 0.437 | 0.595 | 0.136 | 0.038 | 0.427 | 0.322 | 0.545 | 0.532 | −0.086 | −0.394 | −0.272 | 0.055 | 0.212 | 0.657 | ||
| 2015 | −0.281 | −0.393 | 0.199 | −0.355 | 0.432 | 0.584 | 0.130 | 0.031 | 0.427 | 0.322 | 0.546 | 0.530 | −0.081 | −0.400 | −0.281 | 0.092 | 0.202 | 0.652 | ||
| 2017 | −0.280 | −0.397 | 0.196 | −0.364 | 0.429 | 0.582 | 0.130 | 0.032 | 0.429 | 0.323 | 0.544 | 0.528 | −0.073 | −0.393 | −0.282 | 0.114 | 0.190 | 0.650 | ||
| MSK | 1990 | Males | 0.258 | 0.084 | −0.026 | −0.277 | 0.500 | 0.482 | 0.175 | 0.146 | 0.198 | 0.145 | 0.522 | 0.366 | 0.243 | −0.250 | 0.215 | 0.083 | 0.195 | 0.384 |
| 1995 | 0.218 | −0.022 | −0.045 | −0.356 | 0.485 | 0.467 | 0.154 | 0.127 | 0.178 | 0.161 | 0.523 | 0.364 | 0.236 | −0.248 | 0.223 | 0.050 | 0.218 | 0.376 | ||
| 2000 | 0.195 | −0.115 | −0.037 | −0.333 | 0.479 | 0.440 | 0.151 | 0.128 | 0.146 | 0.169 | 0.524 | 0.363 | 0.257 | −0.213 | 0.236 | 0.021 | 0.202 | 0.338 | ||
| 2005 | 0.133 | −0.155 | −0.033 | −0.354 | 0.463 | 0.431 | 0.139 | 0.111 | 0.158 | 0.153 | 0.519 | 0.353 | 0.252 | −0.219 | 0.263 | 0.044 | 0.191 | 0.324 | ||
| 2010 | 0.099 | −0.193 | −0.004 | −0.420 | 0.449 | 0.424 | 0.119 | 0.093 | 0.174 | 0.150 | 0.525 | 0.339 | 0.254 | −0.221 | 0.275 | 0.053 | 0.172 | 0.308 | ||
| 2015 | 0.015 | −0.230 | −0.010 | −0.400 | 0.440 | 0.422 | 0.108 | 0.082 | 0.172 | 0.150 | 0.516 | 0.336 | 0.272 | −0.229 | 0.288 | 0.073 | 0.155 | 0.286 | ||
| 2017 | 0.004 | −0.245 | −0.024 | −0.426 | 0.438 | 0.423 | 0.107 | 0.079 | 0.169 | 0.154 | 0.513 | 0.334 | 0.281 | −0.223 | 0.287 | 0.082 | 0.146 | 0.277 | ||
| Other Disorders | Mental Disorders Sub-Categories | |||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Year | Income Categories | Neoplasms | CVD | NeuroD | Injuries | MDT | aMeAD | Depressive Disorders | MDD | Dysthymia | Bipolar | Anxiety | EatingD | Autism Disorders | ADHD | Conduct Disorder | IDID | OMD | SZA | |
| MSK | 1990 | Low income | −0.401 | 0.120 | −0.035 | −0.065 | 0.162 | 0.375 | −0.062 | −0.063 | −0.404 | 0.299 | 0.201 | 0.442 | −0.414 | −0.293 | 0.224 | 0.095 | 0.092 | 0.490 |
| 1995 | −0.490 | −0.024 | −0.191 | −0.236 | 0.085 | 0.368 | −0.127 | −0.128 | −0.450 | 0.315 | 0.162 | 0.426 | −0.365 | 0.243 | 0.273 | 0.073 | 0.151 | 0.509 | ||
| 2000 | −0.422 | 0.013 | −0.063 | −0.208 | 0.066 | 0.494 | −0.096 | −0.097 | −0.446 | 0.340 | 0.163 | 0.417 | −0.348 | −0.234 | 0.260 | 0.093 | 0.229 | 0.569 | ||
| 2005 | −0.291 | 0.151 | 0.191 | −0.099 | 0.058 | 0.522 | −0.075 | −0.083 | −0.373 | 0.316 | 0.097 | 0.399 | −0.347 | −0.283 | 0.238 | 0.203 | 0.195 | 0.547 | ||
| 2010 | −0.315 | 0.187 | 0.275 | −0.201 | 0.088 | 0.465 | −0.033 | −0.062 | −0.397 | 0.274 | 0.061 | 0.414 | −0.377 | −0.338 | 0.182 | 0.155 | 0.054 | 0.524 | ||
| 2015 | −0.364 | 0.157 | 0.332 | 0.032 | 0.058 | 0.462 | −0.063 | −0.064 | −0.360 | 0.246 | 0.001 | 0.365 | −0.396 | −0.394 | 0.210 | 0.185 | 0.007 | 0.497 | ||
| 2017 | −0.392 | 0.128 | 0.327 | −0.082 | 0.029 | 0.445 | −0.051 | −0.059 | −0.334 | 0.234 | −0.014 | 0.330 | −0.356 | −0.378 | 0.230 | 0.149 | −0.035 | 0.502 | ||
| MSK | 1990 | Lower and upper-middle income | 0.037 | 0.400 | 0.192 | −0.034 | 0.175 | 0.214 | 0.064 | −0.035 | 0.273 | −0.171 | 0.333 | −0.263 | −0.541 | −0.259 | 0.026 | 0.561 | −0.002 | 0.333 |
| 1995 | −0.007 | 0.339 | 0.180 | −0.084 | 0.143 | 0.189 | 0.037 | −0.045 | 0.237 | −0.148 | 0.323 | −0.230 | −0.524 | −0.254 | 0.003 | 0.582 | 0.084 | 0.314 | ||
| 2000 | −0.056 | 0.247 | 0.147 | −0.091 | 0.139 | 0.162 | 0.039 | −0.046 | 0.203 | −0.124 | 0.319 | −0.194 | −0.500 | −0.213 | 0.005 | 0.559 | 0.071 | 0.299 | ||
| 2005 | −0.085 | 0.232 | 0.118 | −0.133 | 0.115 | 0.123 | 0.022 | −0.056 | 0.212 | −0.129 | 0.316 | −0.201 | −0.499 | −0.229 | 0.007 | 0.562 | 0.051 | 0.308 | ||
| 2010 | −0.067 | 0.221 | 0.143 | −0.199 | 0.108 | 0.120 | 0.009 | −0.067 | 0.226 | −0.117 | 0.323 | −0.210 | −0.508 | −0.235 | −0.005 | 0.578 | 0.042 | 0.305 | ||
| 2015 | −0.083 | 0.195 | 0.105 | −0.186 | 0.103 | 0.101 | −0.009 | −0.075 | 0.226 | −0.105 | 0.333 | −0.217 | −0.507 | −0.238 | 0.002 | 0.595 | 0.047 | 0.291 | ||
| 2017 | −0.091 | 0.205 | 0.111 | −0.191 | 0.101 | 0.082 | −0.007 | −0.079 | 0.223 | −0.103 | 0.327 | −0.232 | −0.510 | −0.240 | −0.003 | 0.587 | 0.033 | 0.272 | ||
| MSK | 1990 | High income | 0.111 | −0.457 | 0.418 | −0.288 | 0.735 | 0.719 | 0.506 | 0.376 | 0.504 | 0.345 | 0.656 | 0.652 | 0.670 | −0.241 | 0.061 | 0.214 | 0.565 | 0.391 |
| 1995 | 0.083 | −0.514 | 0.390 | −0.313 | 0.750 | 0.694 | 0.516 | 0.413 | 0.492 | 0.344 | 0.643 | 0.630 | 0.651 | −0.233 | 0.121 | 0.202 | 0.523 | 0.373 | ||
| 2000 | −0.042 | −0.488 | 0.380 | −0.321 | 0.741 | 0.680 | 0.521 | 0.421 | 0.462 | 0.331 | 0.642 | 0.623 | 0.637 | −0.238 | 0.142 | 0.184 | 0.505 | 0.355 | ||
| 2005 | −0.116 | −0.550 | 0.373 | −0.415 | 0.723 | 0.661 | 0.567 | 0.453 | 0.480 | 0.316 | 0.625 | 0.594 | 0.643 | −0.235 | 0.154 | 0.173 | 0.493 | 0.339 | ||
| 2010 | −0.151 | −0.568 | 0.385 | −0.447 | 0.726 | 0.648 | 0.566 | 0.470 | 0.478 | 0.304 | 0.650 | 0.582 | 0.640 | −0.235 | 0.146 | 0.140 | 0.499 | 0.325 | ||
| 2015 | −0.206 | −0.592 | 0.372 | −0.453 | 0.723 | 0.658 | 0.564 | 0.456 | 0.495 | 0.316 | 0.649 | 0.608 | 0.660 | −0.224 | 0.157 | 0.173 | 0.482 | 0.328 | ||
| 2017 | −0.206 | −0.594 | 0.384 | −0.485 | 0.727 | 0.670 | 0.566 | 0.437 | 0.496 | 0.317 | 0.667 | 0.608 | 0.669 | −0.230 | 0.135 | 0.207 | 0.498 | 0.329 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tyrovolas, S.; Moneta, V.; Giné Vázquez, I.; Koyanagi, A.; Abduljabbar, A.S.; Haro, J.M. Mental Disorders, Musculoskeletal Disorders and Income-Driven Patterns: Evidence from the Global Burden of Disease Study 2017. J. Clin. Med. 2020, 9, 2189. https://doi.org/10.3390/jcm9072189
Tyrovolas S, Moneta V, Giné Vázquez I, Koyanagi A, Abduljabbar AS, Haro JM. Mental Disorders, Musculoskeletal Disorders and Income-Driven Patterns: Evidence from the Global Burden of Disease Study 2017. Journal of Clinical Medicine. 2020; 9(7):2189. https://doi.org/10.3390/jcm9072189
Chicago/Turabian StyleTyrovolas, Stefanos, Victoria Moneta, Iago Giné Vázquez, Ai Koyanagi, Adel S. Abduljabbar, and Josep Maria Haro. 2020. "Mental Disorders, Musculoskeletal Disorders and Income-Driven Patterns: Evidence from the Global Burden of Disease Study 2017" Journal of Clinical Medicine 9, no. 7: 2189. https://doi.org/10.3390/jcm9072189
APA StyleTyrovolas, S., Moneta, V., Giné Vázquez, I., Koyanagi, A., Abduljabbar, A. S., & Haro, J. M. (2020). Mental Disorders, Musculoskeletal Disorders and Income-Driven Patterns: Evidence from the Global Burden of Disease Study 2017. Journal of Clinical Medicine, 9(7), 2189. https://doi.org/10.3390/jcm9072189






