Sequential Strategy Including FFRCT Plus Stress-CTP Impacts on Management of Patients with Stable Chest Pain: The Stress-CTP RIPCORD Study
Abstract
1. Introduction
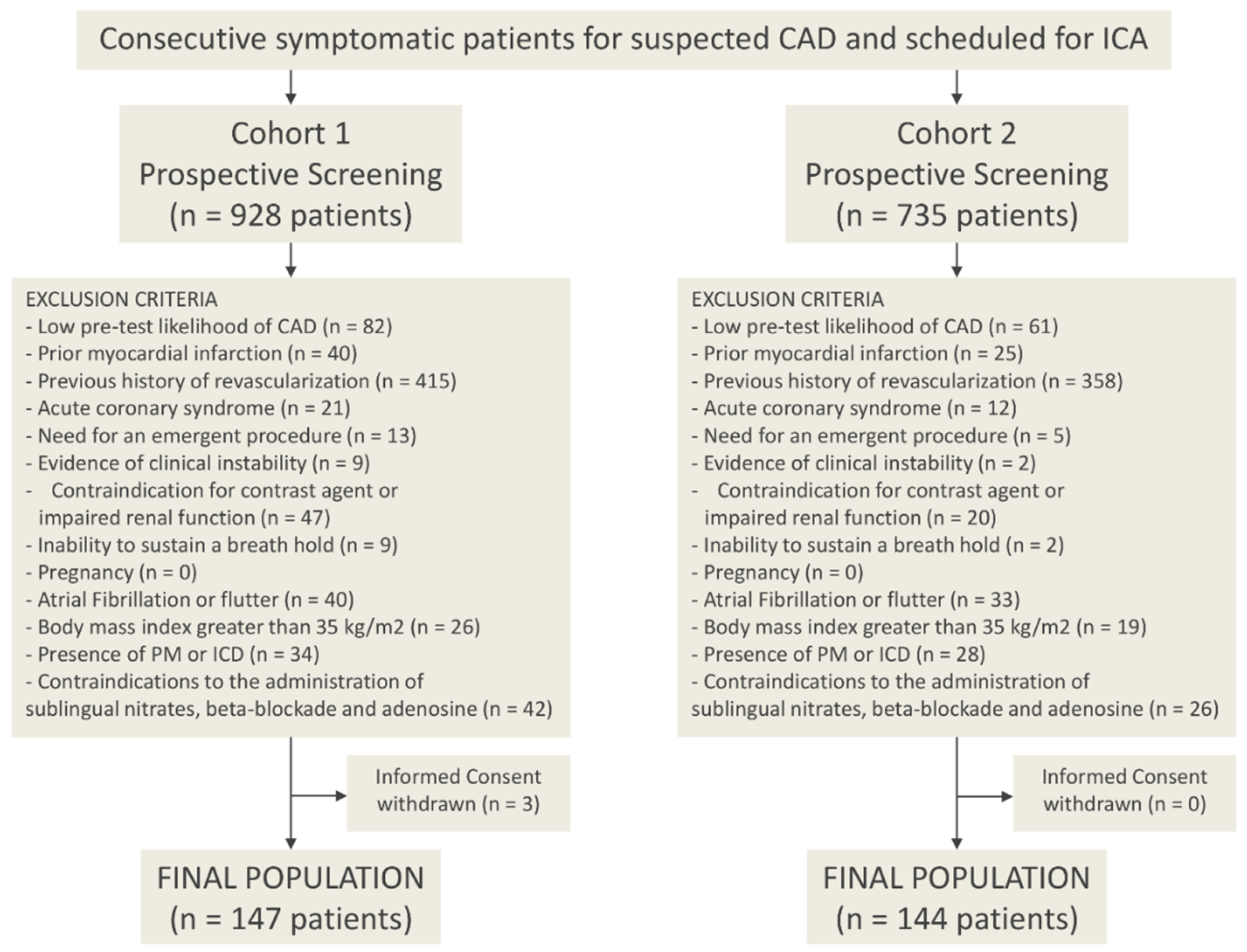
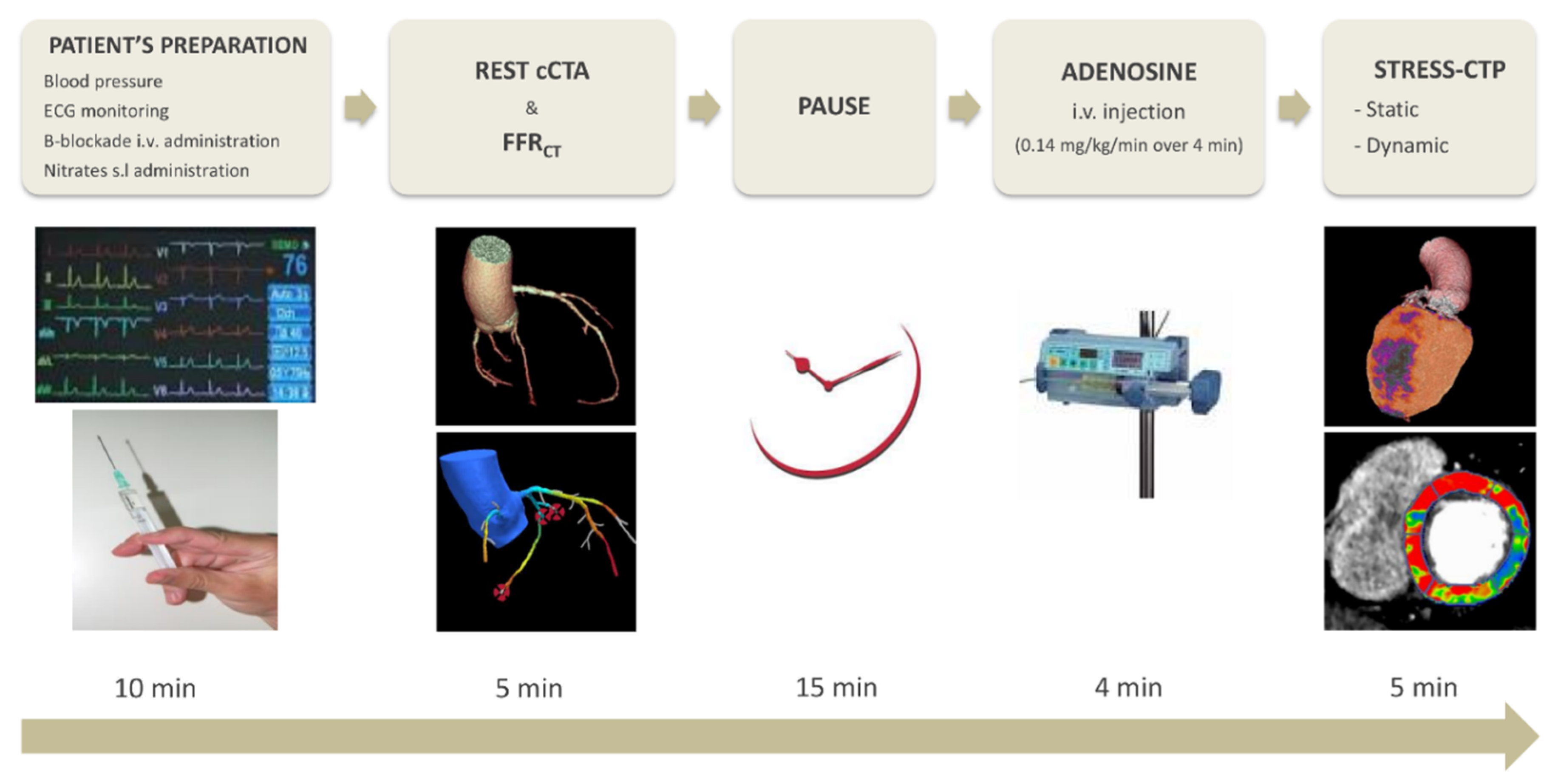
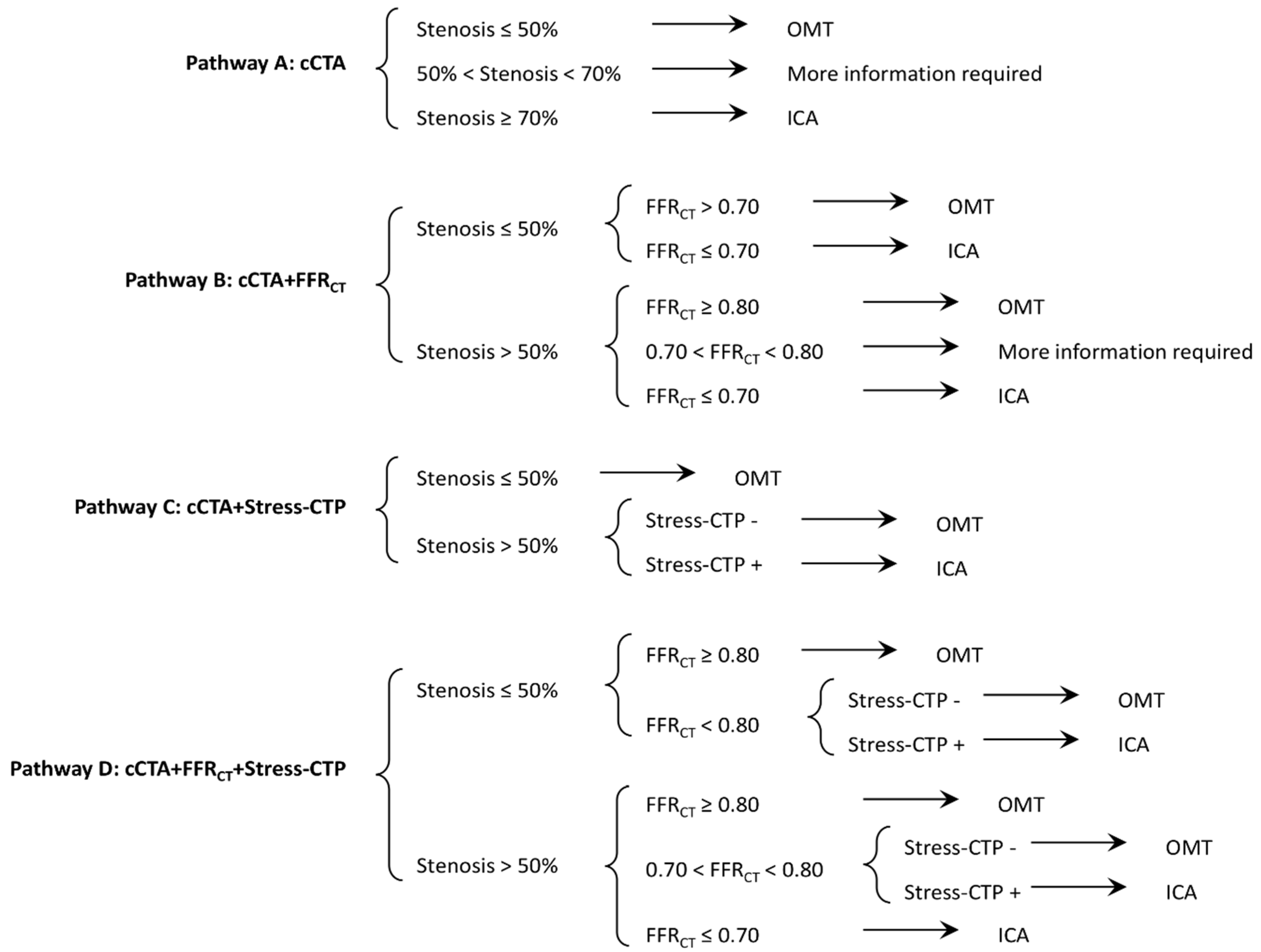
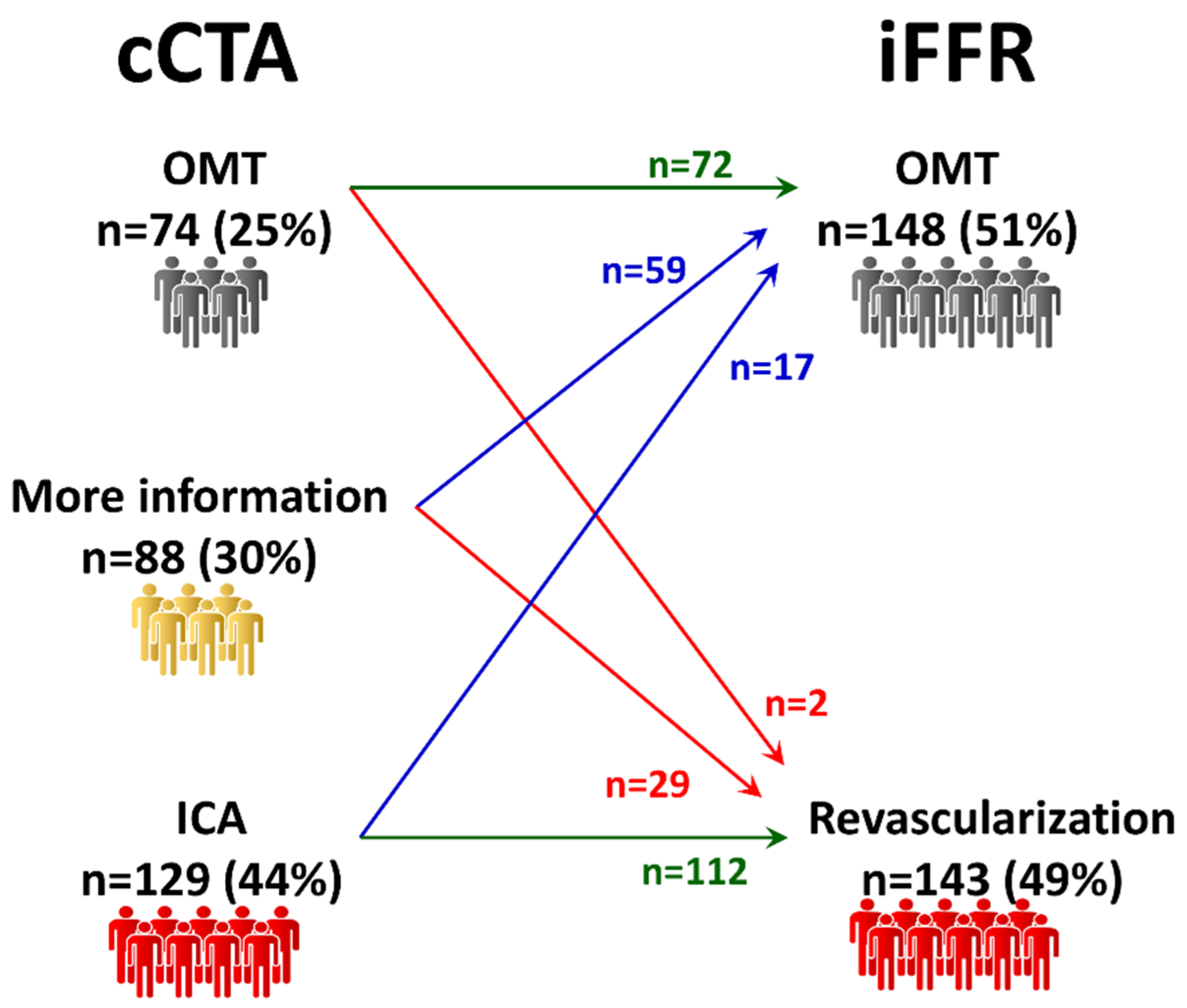
2. Experimental Methods
- (a)
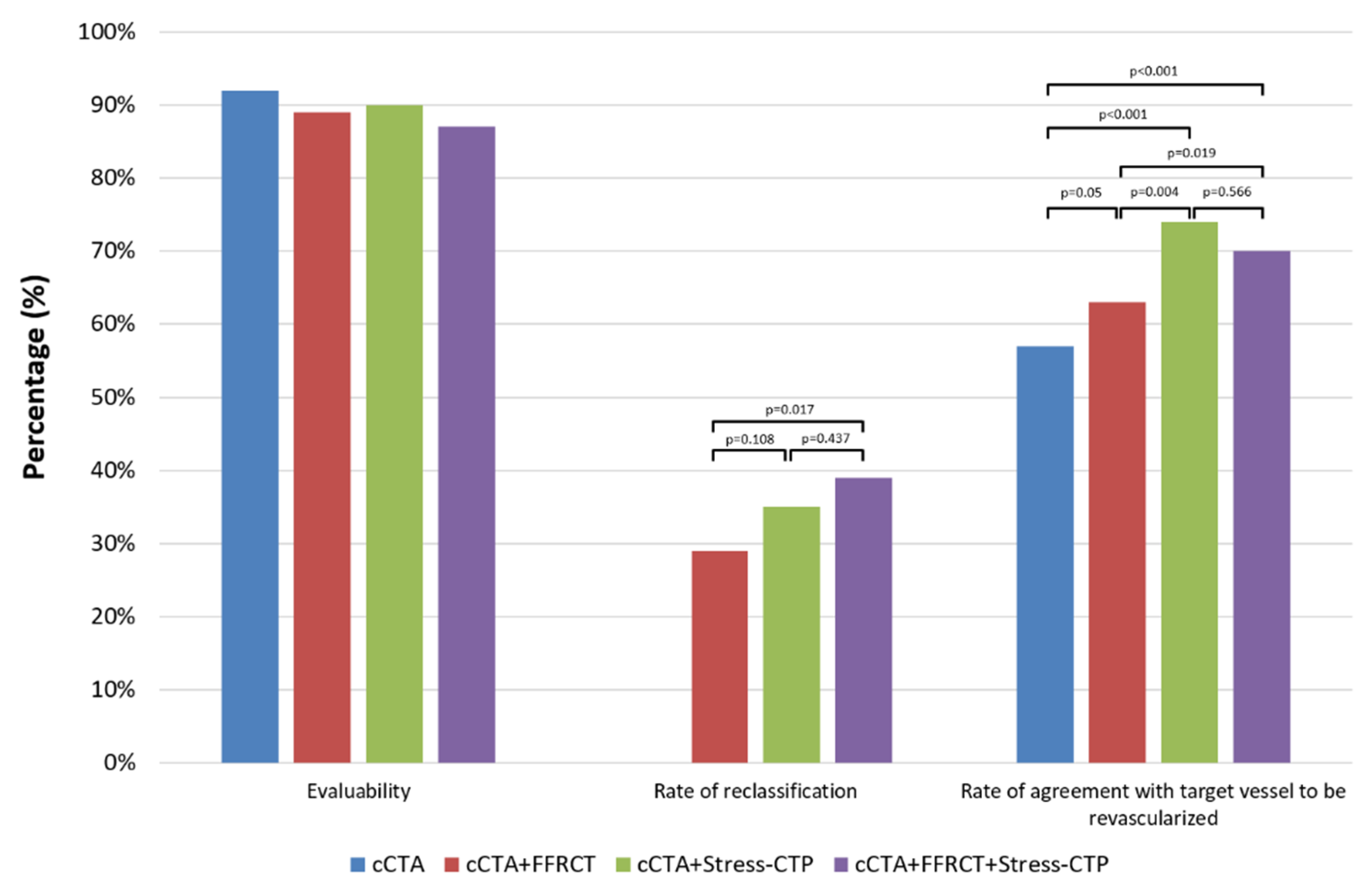
- Overall evaluability, defined as the ratio between the number of patients in which the strategy information was applied to the total number of patients
- (b)
- Rate of reclassification, defined as the ratio between the number of patients who underwent a different management as compared to the initial decision to the total number of patients
- (c)
- Rate of agreement on the vessels to be revascularized, defined as the ratio between the number of patients in which the vessel to be revascularized matched the final decision to the total number of patients
- (d)
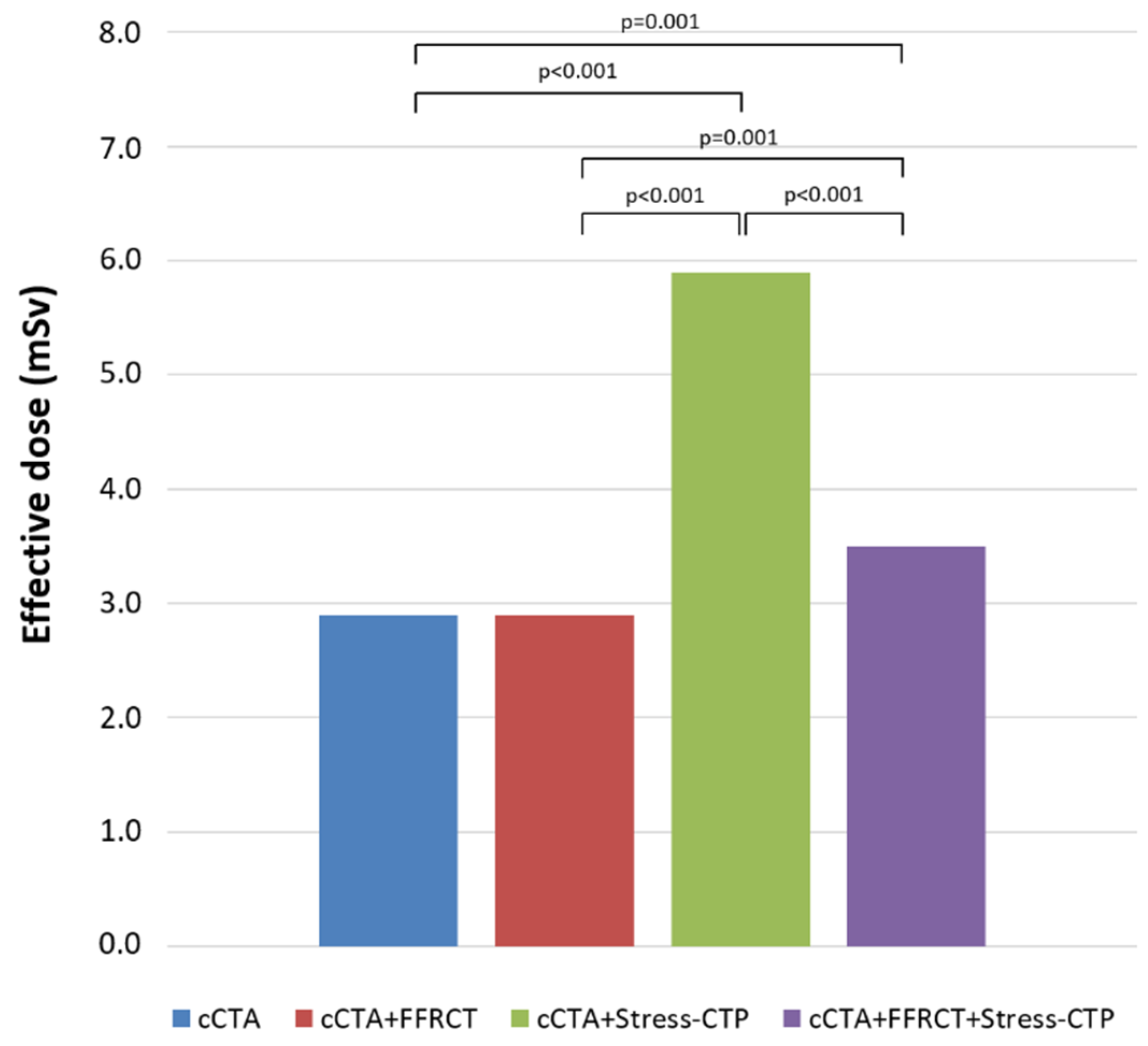
- Cumulative effective dose (ED), defined as the cumulative radiation exposure of the strategy.
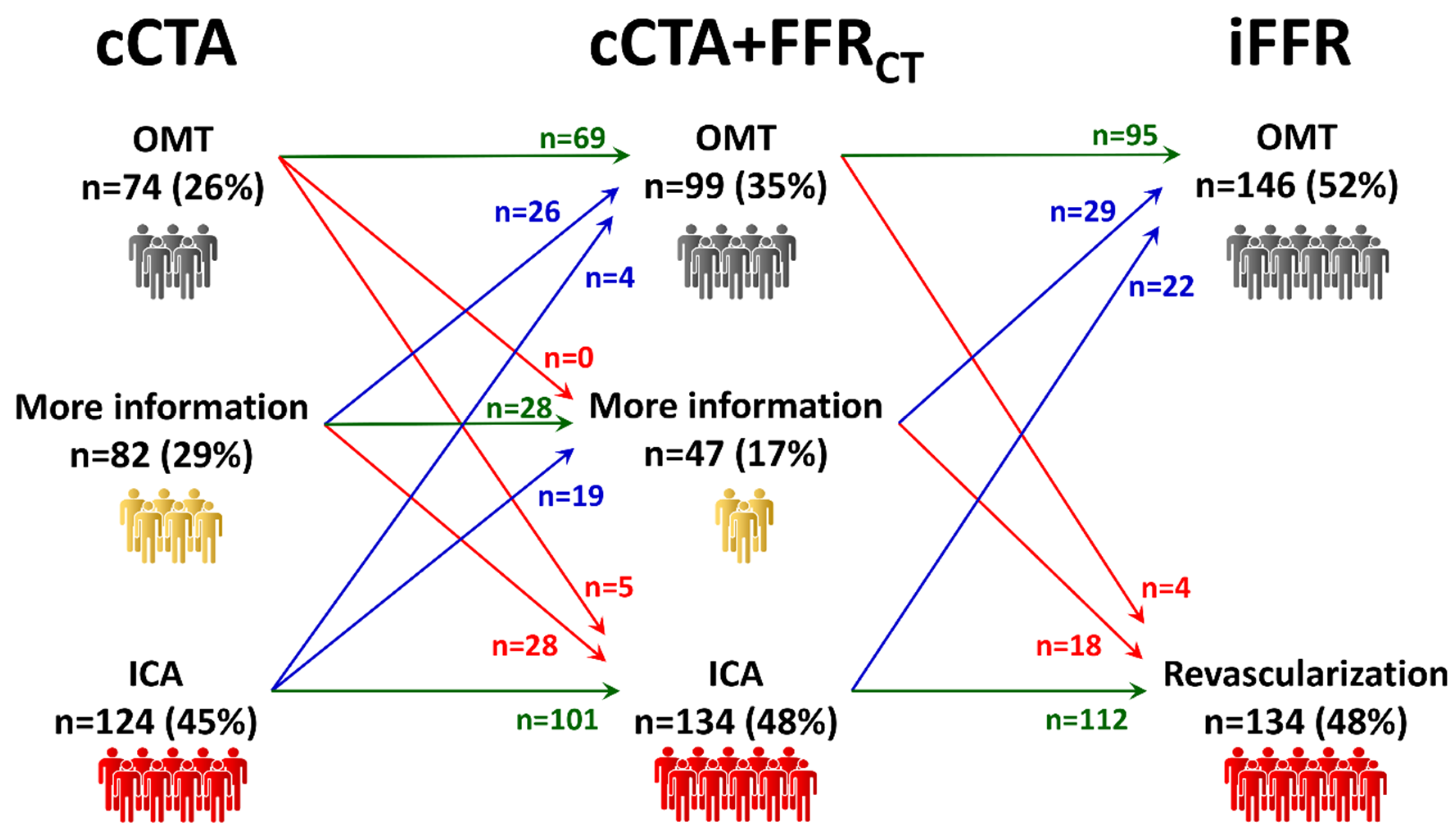
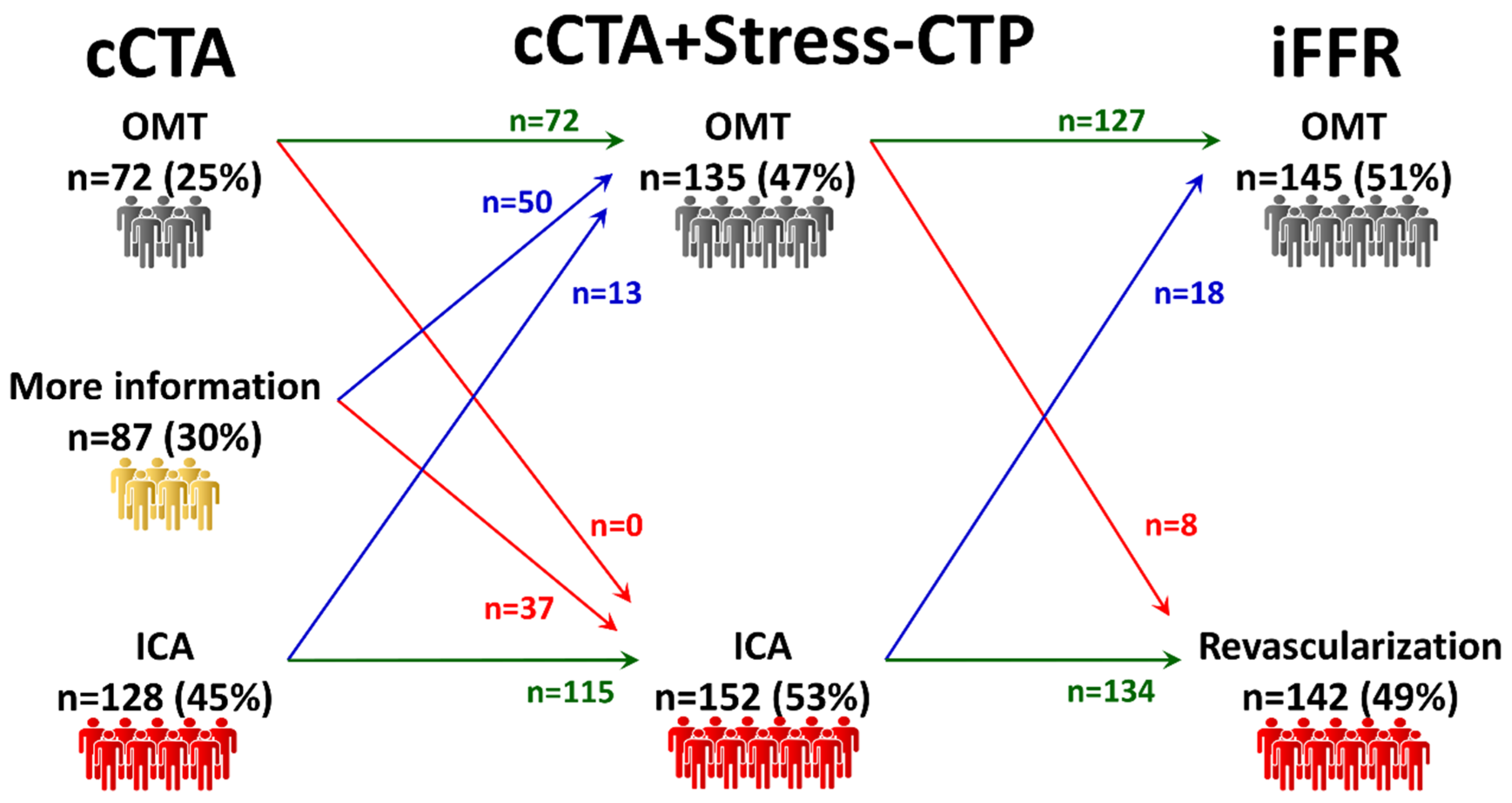
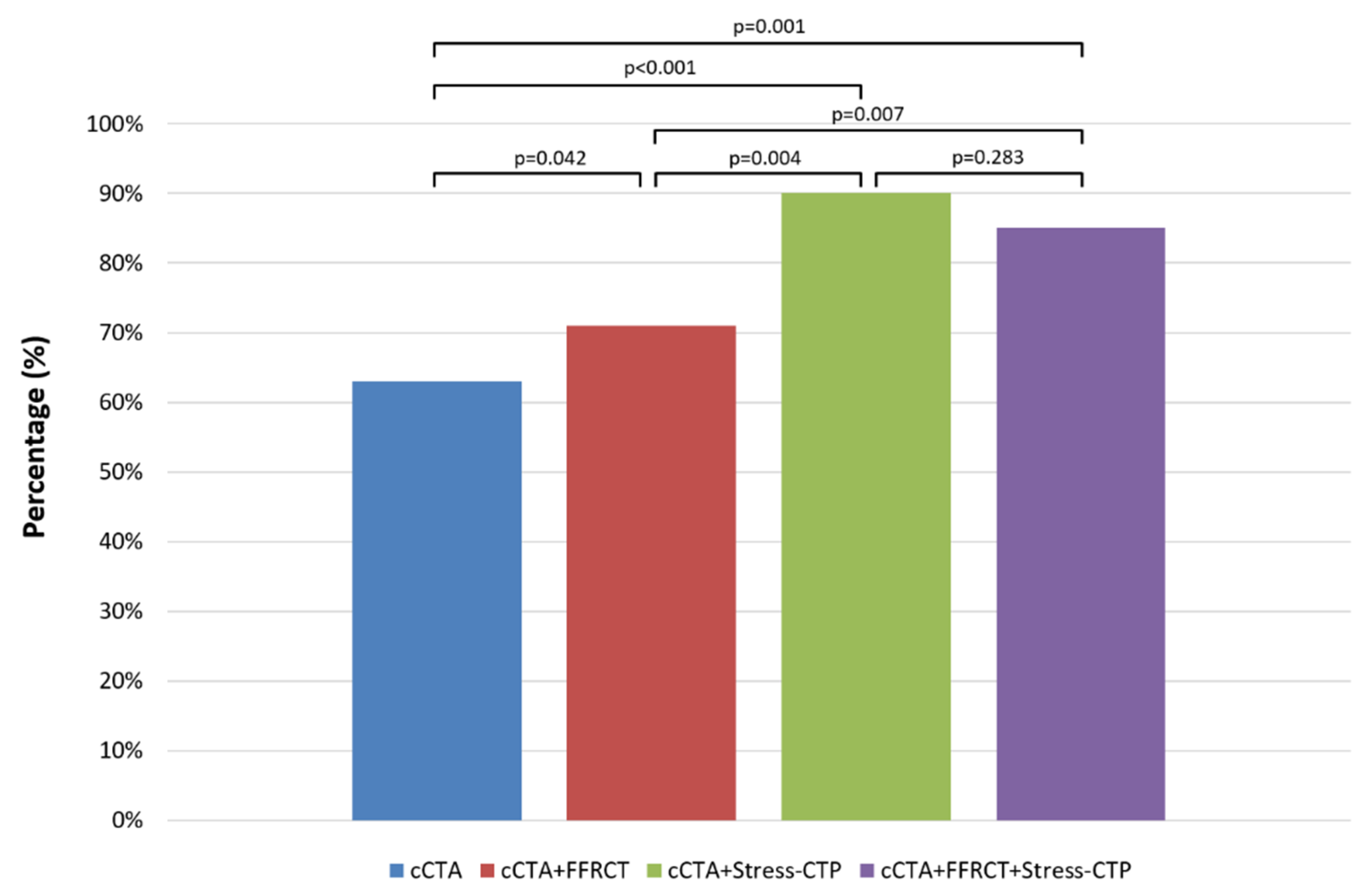
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
Appendix B
References
- Pontone, G.; Andreini, D.; Quaglia, C.; Ballerini, G.; Nobili, E.; Pepi, M. Accuracy of multidetector spiral computed tomography in detecting significant coronary stenosis in patient populations with differing pre-test probabilities of disease. Clin. Radiol. 2007, 62, 978–985. [Google Scholar] [CrossRef] [PubMed]
- Min, J.K.; Dunning, A.; Lin, F.Y.; Achenbach, S.; Al-Mallah, M.; Budoff, M.J.; Cademartiri, F.; Callister, T.Q.; Chang, H.J.; Cheng, V.; et al. Age- and sex-related differences in all-cause mortality risk based on coronary computed tomography angiography findings results from the International Multicenter CONFIRM (Coronary CT Angiography Evaluation for Clinical Outcomes: An International Multicenter Registry) of 23,854 patients without known coronary artery disease. J. Am. Coll. Cardiol. 2011, 58, 849–860. [Google Scholar] [CrossRef]
- Pontone, G.; Andreini, D.; Bartorelli, A.L.; Bertella, E.; Cortinovis, S.; Mushtaq, S.; Foti, C.; Annoni, A.; Formenti, A.; Baggiano, A.; et al. A long-term prognostic value of CT angiography and exercise ECG in patients with suspected CAD. JACC Cardiovasc. Imaging 2013, 6, 641–650. [Google Scholar] [CrossRef][Green Version]
- Investigators, S.-H.; Newby, D.E.; Adamson, P.D.; Berry, C.; Boon, N.A.; Dweck, M.R.; Flather, M.; Forbes, J.; Hunter, A.; Lewis, S.; et al. Coronary CT Angiography and 5-Year Risk of Myocardial Infarction. N. Engl. J. Med. 2018, 379, 924–933. [Google Scholar] [CrossRef]
- Pontone, G.; Bertella, E.; Mushtaq, S.; Loguercio, M.; Cortinovis, S.; Baggiano, A.; Conte, E.; Annoni, A.; Formenti, A.; Beltrama, V.; et al. Coronary artery disease: Diagnostic accuracy of CT coronary angiography--a comparison of high and standard spatial resolution scanning. Radiology 2014, 271, 688–694. [Google Scholar] [CrossRef]
- Dewey, M.; Vavere, A.L.; Arbab-Zadeh, A.; Miller, J.M.; Sara, L.; Cox, C.; Gottlieb, I.; Yoshioka, K.; Paul, N.; Hoe, J.; et al. Patient characteristics as predictors of image quality and diagnostic accuracy of MDCT compared with conventional coronary angiography for detecting coronary artery stenoses: CORE-64 Multicenter International Trial. AJR Am. J. Roentgenol. 2010, 194, 93–102. [Google Scholar] [CrossRef] [PubMed]
- Rossi, A.; Merkus, D.; Klotz, E.; Mollet, N.; de Feyter, P.J.; Krestin, G.P. Stress myocardial perfusion: Imaging with multidetector CT. Radiology 2014, 270, 25–46. [Google Scholar] [CrossRef] [PubMed]
- Pontone, G.; Andreini, D.; Guaricci, A.I.; Baggiano, A.; Fazzari, F.; Guglielmo, M.; Muscogiuri, G.; Berzovini, C.M.; Pasquini, A.; Mushtaq, S.; et al. Incremental Diagnostic Value of Stress Computed Tomography Myocardial Perfusion With Whole-Heart Coverage CT Scanner in Intermediate- to High-Risk Symptomatic Patients Suspected of Coronary Artery Disease. JACC Cardiovasc. Imaging 2019, 12, 338–349. [Google Scholar] [CrossRef]
- Fairbairn, T.A.; Nieman, K.; Akasaka, T.; Norgaard, B.L.; Berman, D.S.; Raff, G.; Hurwitz-Koweek, L.M.; Pontone, G.; Kawasaki, T.; Sand, N.P.; et al. Real-world clinical utility and impact on clinical decision-making of coronary computed tomography angiography-derived fractional flow reserve: Lessons from the ADVANCE Registry. Eur. Heart J. 2018, 39, 3701–3711. [Google Scholar] [CrossRef]
- Rossi, A.; Wragg, A.; Klotz, E.; Pirro, F.; Moon, J.C.; Nieman, K.; Pugliese, F. Dynamic Computed Tomography Myocardial Perfusion Imaging: Comparison of Clinical Analysis Methods for the Detection of Vessel-Specific Ischemia. Circ. Cardiovasc. Imaging 2017, 10, e005505. [Google Scholar] [CrossRef] [PubMed]
- Pontone, G.; Andreini, D.; Guaricci, A.I.; Guglielmo, M.; Baggiano, A.; Muscogiuri, G.; Fusini, L.; Soldi, M.; Fazzari, F.; Berzovini, C.; et al. Quantitative vs. qualitative evaluation of static stress computed tomography perfusion to detect haemodynamically significant coronary artery disease. Eur. Heart J. Cardiovasc. Imaging 2018, 19, 1244–1252. [Google Scholar] [CrossRef] [PubMed]
- Pontone, G.; Baggiano, A.; Andreini, D.; Guaricci, A.I.; Guglielmo, M.; Muscogiuri, G.; Fusini, L.; Soldi, M.; Del Torto, A.; Mushtaq, S.; et al. Diagnostic accuracy of simultaneous evaluation of coronary arteries and myocardial perfusion with single stress cardiac computed tomography acquisition compared to invasive coronary angiography plus invasive fractional flow reserve. Int. J. Cardiol. 2018, 273, 263–268. [Google Scholar] [CrossRef] [PubMed]
- Douglas, P.S.; Pontone, G.; Hlatky, M.A.; Patel, M.R.; Norgaard, B.L.; Byrne, R.A.; Curzen, N.; Purcell, I.; Gutberlet, M.; Rioufol, G.; et al. Clinical outcomes of fractional flow reserve by computed tomographic angiography-guided diagnostic strategies vs. usual care in patients with suspected coronary artery disease: The prospective longitudinal trial of FFR(CT): Outcome and resource impacts study. Eur. Heart J. 2015, 36, 3359–3367. [Google Scholar] [CrossRef]
- Collet, C.; Onuma, Y.; Andreini, D.; Sonck, J.; Pompilio, G.; Mushtaq, S.; La Meir, M.; Miyazaki, Y.; de Mey, J.; Gaemperli, O.; et al. Coronary computed tomography angiography for heart team decision-making in multivessel coronary artery disease. Eur. Heart J. 2018, 39, 3689–3698. [Google Scholar] [CrossRef]
- Pontone, G.; Baggiano, A.; Andreini, D.; Guaricci, A.I.; Guglielmo, M.; Muscogiuri, G.; Fusini, L.; Fazzari, F.; Mushtaq, S.; Conte, E.; et al. Stress Computed Tomography Perfusion Versus Fractional Flow Reserve CT Derived in Suspected Coronary Artery Disease: The PERFECTION Study. JACC Cardiovasc. Imaging 2019, 12, 1487–1497. [Google Scholar] [CrossRef]
- Coenen, A.; Rossi, A.; Lubbers, M.M.; Kurata, A.; Kono, A.K.; Chelu, R.G.; Segreto, S.; Dijkshoorn, M.L.; Wragg, A.; van Geuns, R.M.; et al. Integrating CT Myocardial Perfusion and CT-FFR in the Work-Up of Coronary Artery Disease. JACC Cardiovasc. Imaging 2017, 10, 760–770. [Google Scholar] [CrossRef]
- Curzen, N.; Rana, O.; Nicholas, Z.; Golledge, P.; Zaman, A.; Oldroyd, K.; Hanratty, C.; Banning, A.; Wheatcroft, S.; Hobson, A.; et al. Does routine pressure wire assessment influence management strategy at coronary angiography for diagnosis of chest pain?: The RIPCORD study. Circ. Cardiovasc. Interv. 2014, 7, 248–255. [Google Scholar] [CrossRef]
- Curzen, N.P.; Nolan, J.; Zaman, A.G.; Norgaard, B.L.; Rajani, R. Does the Routine Availability of CT-Derived FFR Influence Management of Patients With Stable Chest Pain Compared to CT Angiography Alone?: The FFRCT RIPCORD Study. JACC Cardiovasc. Imaging 2016, 9, 1188–1194. [Google Scholar] [CrossRef]
- Pontone, G.; Andreini, D.; Guaricci, A.I.; Guglielmo, M.; Mushtaq, S.; Baggiano, A.; Beltrama, V.; Trabattoni, D.; Ferrari, C.; Calligaris, G.; et al. Rationale and design of the PERFECTION (comparison between stress cardiac computed tomography PERfusion versus Fractional flow rEserve measured by Computed Tomography angiography In the evaluation of suspected cOroNary artery disease) prospective study. J. Cardiovasc. Comput. Tomogr. 2016, 10, 330–334. [Google Scholar] [CrossRef]
- The SCOT-HEART investigators. CT coronary angiography in patients with suspected angina due to coronary heart disease (SCOT-HEART): An open-label, parallel-group, multicentre trial. Lancet 2015, 385, 2383–2391. [Google Scholar] [CrossRef]
- Nielsen, L.H.; Botker, H.E.; Sorensen, H.T.; Schmidt, M.; Pedersen, L.; Sand, N.P.; Jensen, J.M.; Steffensen, F.H.; Tilsted, H.H.; Bottcher, M.; et al. Prognostic assessment of stable coronary artery disease as determined by coronary computed tomography angiography: A Danish multicentre cohort study. Eur. Heart J. 2017, 38, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Norgaard, B.L.; Leipsic, J.; Gaur, S.; Seneviratne, S.; Ko, B.S.; Ito, H.; Jensen, J.M.; Mauri, L.; De Bruyne, B.; Bezerra, H.; et al. Diagnostic performance of noninvasive fractional flow reserve derived from coronary computed tomography angiography in suspected coronary artery disease: The NXT trial (Analysis of Coronary Blood Flow Using CT Angiography: Next Steps). J. Am. Coll. Cardiol. 2014, 63, 1145–1155. [Google Scholar] [CrossRef] [PubMed]
- Douglas, P.S.; De Bruyne, B.; Pontone, G.; Patel, M.R.; Norgaard, B.L.; Byrne, R.A.; Curzen, N.; Purcell, I.; Gutberlet, M.; Rioufol, G.; et al. 1-Year Outcomes of FFRCT-Guided Care in Patients With Suspected Coronary Disease: The PLATFORM Study. J. Am. Coll. Cardiol. 2016, 68, 435–445. [Google Scholar] [CrossRef]
- Patel, M.R.; Norgaard, B.L.; Fairbairn, T.A.; Nieman, K.; Akasaka, T.; Berman, D.S.; Raff, G.L.; Hurwitz Koweek, L.M.; Pontone, G.; Kawasaki, T.; et al. 1-Year Impact on Medical Practice and Clinical Outcomes of FFRCT: The ADVANCE Registry. JACC Cardiovasc. Imaging 2020, 13, 97–105. [Google Scholar] [CrossRef]
- Norgaard, B.L.; Hjort, J.; Gaur, S.; Hansson, N.; Botker, H.E.; Leipsic, J.; Mathiassen, O.N.; Grove, E.L.; Pedersen, K.; Christiansen, E.H.; et al. Clinical Use of Coronary CTA-Derived FFR for Decision-Making in Stable CAD. JACC Cardiovasc. Imaging 2017, 10, 541–550. [Google Scholar] [CrossRef] [PubMed]
- Wong, D.T.; Ko, B.S.; Cameron, J.D.; Leong, D.P.; Leung, M.C.; Malaiapan, Y.; Nerlekar, N.; Crossett, M.; Troupis, J.; Meredith, I.T.; et al. Comparison of diagnostic accuracy of combined assessment using adenosine stress computed tomography perfusion + computed tomography angiography with transluminal attenuation gradient + computed tomography angiography against invasive fractional flow reserve. J. Am. Coll. Cardiol. 2014, 63, 1904–1912. [Google Scholar] [CrossRef]
- Pontone, G.; Baggiano, A.; Andreini, D.; Guaricci, A.I.; Guglielmo, M.; Muscogiuri, G.; Fusini, L.; Soldi, M.; Del Torto, A.; Mushtaq, S.; et al. Dynamic Stress Computed Tomography Perfusion With a Whole-Heart Coverage Scanner in Addition to Coronary Computed Tomography Angiography and Fractional Flow Reserve Computed Tomography Derived. JACC Cardiovasc. Imaging 2019, 10, 2460–2471. [Google Scholar] [CrossRef] [PubMed]
- Pontone, G.; De Cecco, C.; Baggiano, A.; Guaricci, A.I.; Guglielmo, M.; Leiner, T.; Lima, J.; Maurovich-Horvat, P.; Muscogiuri, G.; Nance, J.W.; et al. Design of CTP-PRO study (impact of stress Cardiac computed Tomography myocardial Perfusion on downstream resources and PROgnosis in patients with suspected or known coronary artery disease: A multicenter international study). Int. J. Cardiol. 2019, 292, 253–257. [Google Scholar] [CrossRef]


| Baseline Characteristics | |
| Number, n | 291 |
| Age, years (mean ± SD) | 65 ± 9 |
| Male, n (%) | 222 (76) |
| BMI, kg/m2 (mean ± SD) | 26.7 ± 4.2 |
| Risk Factors | |
| Hypertension, n (%) | 214 (74) |
| Smoker, n (%) | 93 (32) |
| Hyperlipidaemia, n (%) | 189 (65) |
| Diabetes, n (%) | 55 (19) |
| Family History, n (%) | 179 (62) |
| Symptoms | |
| Typical angina, n (%) | 218 (75) |
| Atypical angina, n (%) | 73 (25) |
| Pre-test likelihood of CAD, % (mean ± SD) | 65 ± 15 |
| Reasons for invasive coronary angiography | |
| Symptoms, n (%) | 147 (50) |
| Positive exercise-EKG, n (%) | 79 (27) |
| Positive stress echocardiography, n (%) | 11 (4) |
| Positive single photon emission computed tomography, n (%) | 49 (17) |
| Positive stress cardiac magnetic resonance, n (%) | 5 (2) |
| cCTA scan protocol, REST | |
| HR before scanning, bpm (mean ± SD) | 69 ± 11 |
| β-blocker, n (%) | 161 (55) |
| β-blocker dosage, mg (mean ± SD) | 10 ± 5 |
| HR during scanning, bpm (mean ± SD) | 62 ± 9 |
| Dose length product, mGy-cm (mean ± SD) | 204 ± 92 |
| Effective dose, mSv (mean ± SD) | 2.9 ± 1.3 |
| cCTA scan protocol, STRESS | |
| HR during scanning, bpm (mean ± SD) | 81 ± 15 |
| Effective dose for Static CTP, mSv (mean ± SD) | 2.6 ± 1.0 |
| Effective dose for Dynamic CTP, mSv (mean ± SD) | 5.4 ± 0.6 |
| Prevalence of obstructive CAD (≥50%) at ICA | |
| No disease, n (%) | 97 (33) |
| One-vessel disease, n (%) | 98 (34) |
| Two-vessels disease, n (%) | 50 (17) |
| Three-vessels disease, n (%) | 46 (16) |
| Prevalence of functionally significant CAD * | 143 (49) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baggiano, A.; Fusini, L.; Del Torto, A.; Vivona, P.; Guglielmo, M.; Muscogiuri, G.; Soldi, M.; Martini, C.; Fraschini, E.; Rabbat, M.G.; et al. Sequential Strategy Including FFRCT Plus Stress-CTP Impacts on Management of Patients with Stable Chest Pain: The Stress-CTP RIPCORD Study. J. Clin. Med. 2020, 9, 2147. https://doi.org/10.3390/jcm9072147
Baggiano A, Fusini L, Del Torto A, Vivona P, Guglielmo M, Muscogiuri G, Soldi M, Martini C, Fraschini E, Rabbat MG, et al. Sequential Strategy Including FFRCT Plus Stress-CTP Impacts on Management of Patients with Stable Chest Pain: The Stress-CTP RIPCORD Study. Journal of Clinical Medicine. 2020; 9(7):2147. https://doi.org/10.3390/jcm9072147
Chicago/Turabian StyleBaggiano, Andrea, Laura Fusini, Alberico Del Torto, Patrizia Vivona, Marco Guglielmo, Giuseppe Muscogiuri, Margherita Soldi, Chiara Martini, Enrico Fraschini, Mark G. Rabbat, and et al. 2020. "Sequential Strategy Including FFRCT Plus Stress-CTP Impacts on Management of Patients with Stable Chest Pain: The Stress-CTP RIPCORD Study" Journal of Clinical Medicine 9, no. 7: 2147. https://doi.org/10.3390/jcm9072147
APA StyleBaggiano, A., Fusini, L., Del Torto, A., Vivona, P., Guglielmo, M., Muscogiuri, G., Soldi, M., Martini, C., Fraschini, E., Rabbat, M. G., Baessato, F., Cicala, G., Danza, M. L., Cavaliere, A., Loffreno, A., Palmisano, V., Ricci, F., Rizzon, G., Tonet, E., ... Pontone, G. (2020). Sequential Strategy Including FFRCT Plus Stress-CTP Impacts on Management of Patients with Stable Chest Pain: The Stress-CTP RIPCORD Study. Journal of Clinical Medicine, 9(7), 2147. https://doi.org/10.3390/jcm9072147
















