Intra-Abdominal Nocardiosis—Case Report and Review of the Literature
Abstract
1. Introduction
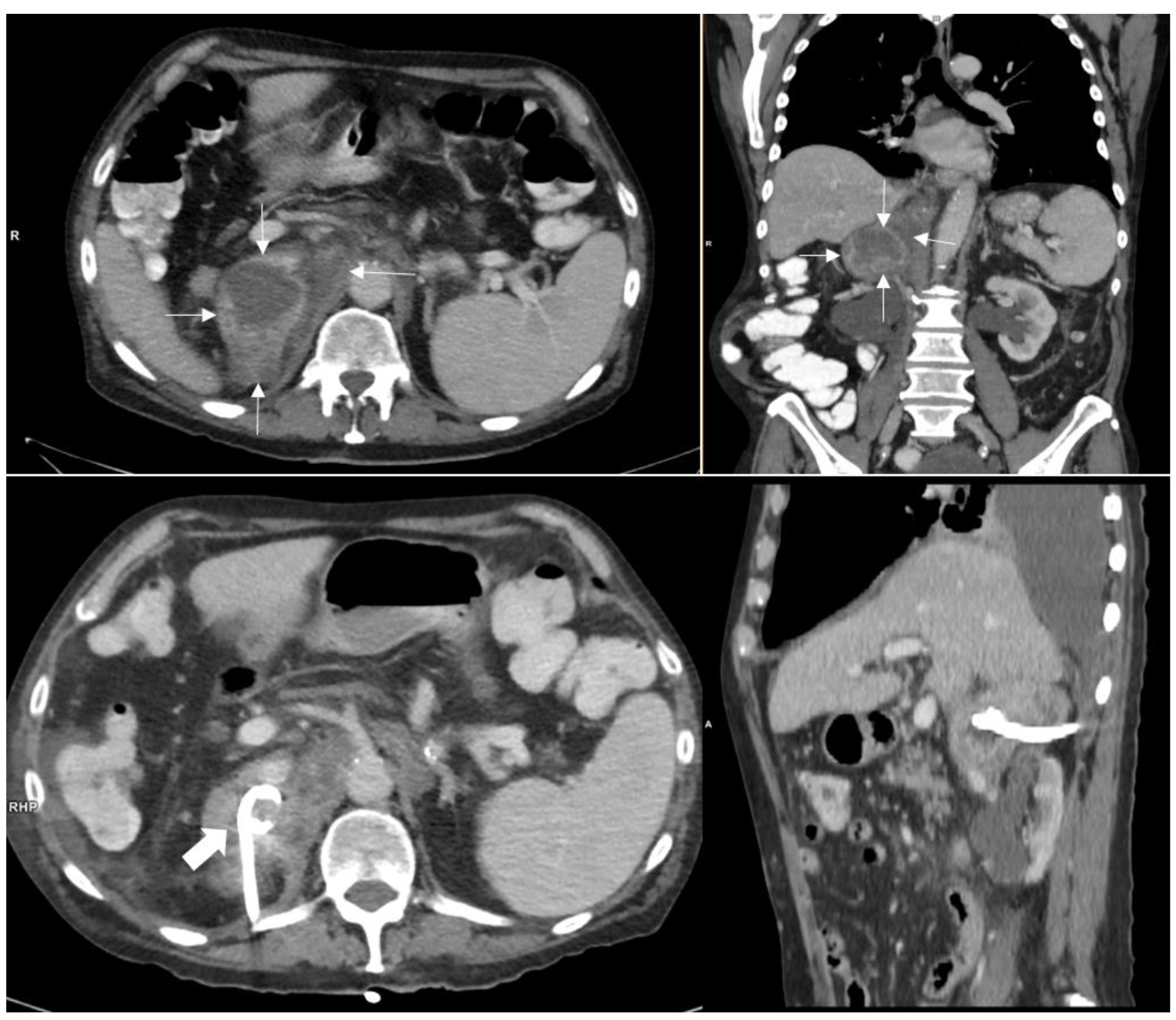
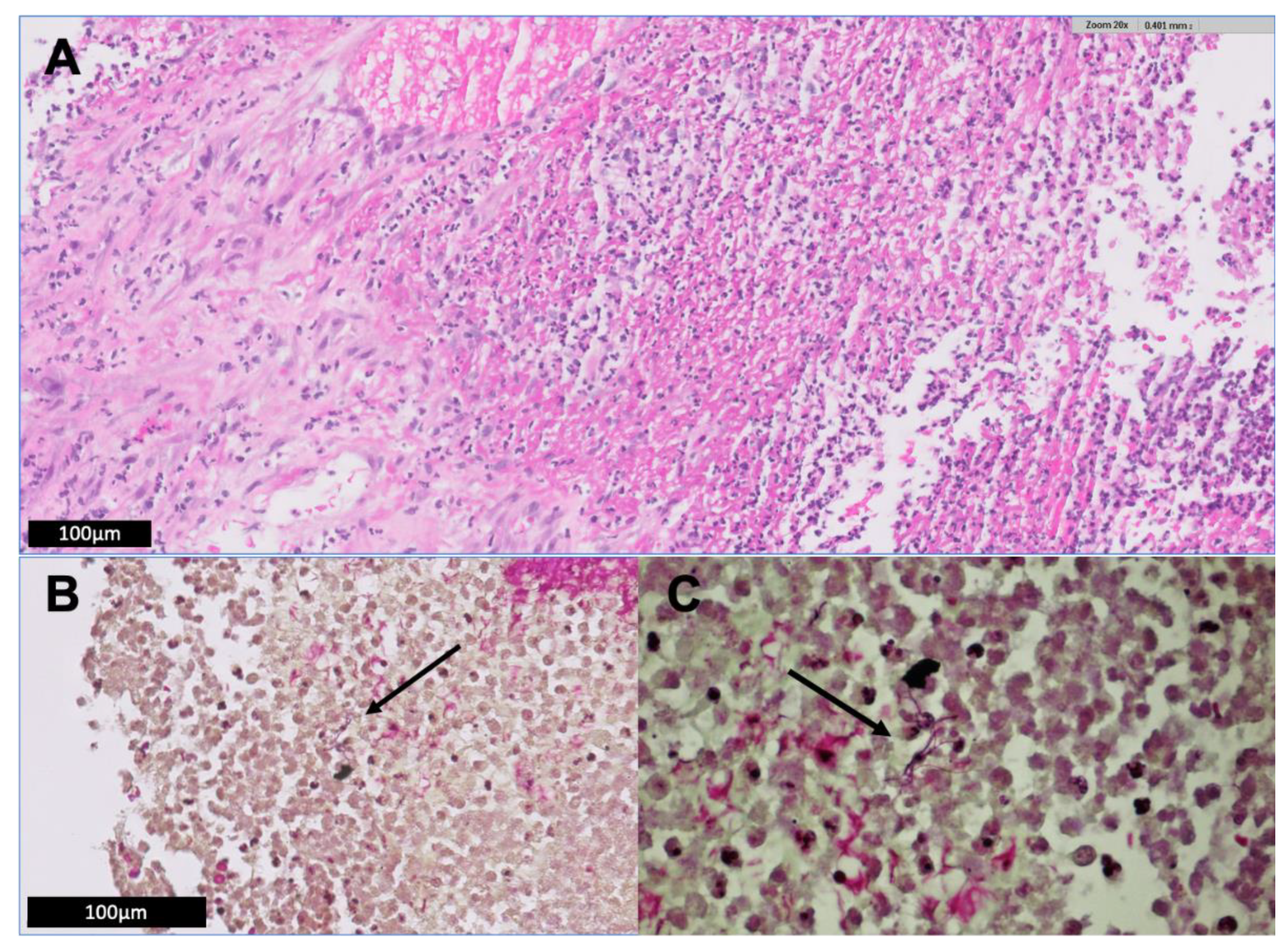
2. Illustrative Case Report
3. Methods
4. Literature Review and Discussion
4.1. Route of Nocardia acquisition
4.2. Infection Due to Nocardia Paucivorans
4.3. Abdominal/Retroperitoneal Infection Due to Nocardia Species
4.4. Peritoneal Dialysis-Related Nocardia Peritonitis
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Brown-Elliott, B.A.; Brown, J.M.; Conville, P.S.; Wallace, R.J., Jr. Clinical and laboratory features of the Nocardia spp. based on current molecular taxonomy. Clin. Microbiol. Rev. 2006, 19, 259–282. [Google Scholar] [CrossRef] [PubMed]
- Biswas Roy, S.; Ross, M.D.; Patil, P.D.; Trepeta, R.; Bremner, R.M.; Panchabhai, T.S. Primary Nocardia Infection Causing a Fluorodeoxyglucose-Avid Right Renal Mass in a Redo Lung Transplant Recipient. Case Rep. Transplant. 2018, 2018, 9752860. [Google Scholar] [CrossRef] [PubMed]
- Aliaga, L.; Fatoul, G.; Guirao, E.; Pena, A.; Rodriguez-Granger, J.; Cobo, F. Nocardia paucivorans brain abscess. Clinical and microbiological characteristics. IDCases 2018, 13, e00422. [Google Scholar] [CrossRef] [PubMed]
- Shimizu, Y.; Tsuchiya, K.; Fujisawa, H. Nocardia paucivorans cerebellar abscess: Surgical and pharmacotherapy. Surg. Neurol. Int. 2019, 10, 22. [Google Scholar] [CrossRef]
- Chong, Y.L.; Green, J.A.; Toh, K.L.; Tan, J.K. Laparoscopic drainage of nocardial adrenal abscess in an HIV positive patient. Int. J. Urol. 2004, 11, 547–549. [Google Scholar] [CrossRef]
- Al-Tawfiq, J.A.; Al-Khatti, A.A. Disseminated systemic Nocardia farcinica infection complicating alefacept and infliximab therapy in a patient with severe psoriasis. Int. J. Infect. Dis. 2010, 14, e153–e157. [Google Scholar] [CrossRef][Green Version]
- Lerner, P.I. Nocardiosis. Clin. Infect. Dis. 1996, 22, 891–903; quiz 904–905. [Google Scholar] [CrossRef]
- Kendrick-Jones, J.; Ratanjee, S.K.; Taylor, S.L.; Marshall, M.R. Nocardia asteroides peritoneal dialysis-related peritonitis: A case of successful treatment and return to peritoneal dialysis. Nephrol. Dial. Transplant. 2008, 23, 2693–2694. [Google Scholar] [CrossRef]
- Lovett, I.S.; Houang, E.T.; Burge, S.; Turner-Warwick, M.; Thompson, F.D.; Harrison, A.R.; Joekes, A.M.; Parkinson, M.C. An outbreak of Nocardia asteroides infection in a renal transplant unit. Q. J. Med. 1981, 50, 123–135. [Google Scholar]
- Salfield, S.A.; Duerden, B.I.; Dickson, J.A.; Milner, R.D. Abdominal nocardiosis in a Sudanese girl. Eur. J. Pediatr. 1983, 140, 135–137. [Google Scholar] [CrossRef]
- Meier, B.; Metzger, U.; Muller, F.; Siegenthaler, W.; Luthy, R. Successful treatment of a pancreatic Nocardia asteroides abscess with amikacin and surgical drainage. Antimicrob. Agents Chemother. 1986, 29, 150–151. [Google Scholar] [CrossRef]
- Kim, J.; Minamoto, G.Y.; Grieco, M.H. Nocardial infection as a complication of AIDS: Report of six cases and review. Rev. Infect. Dis. 1991, 13, 624–629. [Google Scholar] [CrossRef]
- Bocchetti, M.; Muzj, A.; Gargiulo, F.; Cipullo, P.; Amato, G. A case of abdominal aortic aneurysm infected by Nocardia asteroides. Biomed. Pharmacother. 1996, 50, 36. [Google Scholar] [CrossRef]
- Smit, L.H.; Leemans, R.; Overbeek, B.P. Nocardia farcinica as the causative agent in a primary psoas abscess in a previously healthy cattle inspector. Clin. Microbiol. Infect. 2003, 9, 445–448. [Google Scholar] [CrossRef][Green Version]
- Saeed, S.; Varela, J.E.; Nelson, R.L.; Blend, M.J. An unusual case of intraabdominal nocardia abscess detected by Tc-99m HMPAO-labeled WBC study. Clin. Nucl. Med. 2004, 29, 270–271. [Google Scholar] [CrossRef]
- Cassar, C.L. Nocardia sepsis in a multigravida with systemic lupus erythematosus and autoimmune hepatitis. Anaesth. Intensive Care 2007, 35, 601–604. [Google Scholar] [CrossRef] [PubMed]
- Chedid, M.B.; Chedid, M.F.; Porto, N.S.; Severo, C.B.; Severo, L.C. Nocardial infections: Report of 22 cases. Rev. Inst. Med. Trop. Sao Paulo 2007, 49, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Pai, K.; Rao, L. Isolated renal nocardiosis in a patient with AIDS: Unusual presentation. Indian J. Urol. 2009, 25, 395–397. [Google Scholar] [CrossRef] [PubMed]
- Patil, R.N.; Bafna, U.D.; Pallavi, V.R.; Rathod, P.S. Successful Intra-peritoneal Antibiotic Therapy for Primary Abdominal Nocardiosis in an Immunocompetent Young Female Masquerading as Carcinoma Ovary. Online J. Health Allied Sci. 2011, 10, 11. [Google Scholar]
- De Montmollin, E.; Corcos, O.; Noussair, L.; Leflon-Guibout, V.; Belmatoug, N.; Joly, F.; Lefort, A. Retroperitoneal abscesses due to Nocardia farcinica: Report of two cases in patients with malnutrition. Infection 2012, 40, 93–96. [Google Scholar] [CrossRef] [PubMed]
- Kamyab, A.; Fakhoury, J.D.; Sutkowski, R.; Drelichman, E.; Jacobs, M.J. Fulminant colitis secondary to nocardiosis. Int. J. Colorectal. Dis. 2012, 27, 841–842. [Google Scholar] [CrossRef] [PubMed]
- Naha, K.; Dasari, S.; Vivek, G.; Prabhu, M. Primary abdominal nocardiosis masquerading as tubercular pelvic inflammatory disease in an immunocompetent individual. BMJ Case Rep. 2013, 2013. [Google Scholar] [CrossRef]
- Hanchanale, P.; Jain, M.; Varghese, J.; V, J.; Rela, M. Nocardia liver abscess post liver transplantation-A rare presentation. Transpl. Infect. Dis. 2017, 19, e12670. [Google Scholar] [CrossRef]
- David Turer, B.G.; Raghavendran, K. Fulminant Nocardia Colitis: A Case Report. Surgical Infect. Case Rep. 2016, 1, 69–71. [Google Scholar] [CrossRef]
- Singh, S.; Verma, Y.; Pandey, P.; Singh, U.B. Granulomatous hepatitis by Nocardia species: An unusual case. Int. J. Infect. Dis. 2019, 81, 97–99. [Google Scholar] [CrossRef]
- Acharya, R.; Amin, K.; Rajderkar, D.; Washam, M.; Pekkucuksen, N.; Mannemuddhu, S.; Upadhyay, K. Isolated abdominal nocardiosis in a pediatric renal transplant recipient. Pediatr. Transplant. 2019, 23, e13392. [Google Scholar] [CrossRef] [PubMed]
- Idriss, Z.H.; Cunningham, R.J.; Wilfert, C.M. Nocardiosis in children: Report of three cases and review of the literature. Pediatrics 1975, 55, 479–484. [Google Scholar] [PubMed]
- Chulay, J.D.; Lankerani, M.R. Splenic abscess. Report of 10 cases and review of the literature. Am. J. Med. 1976, 61, 513–522. [Google Scholar] [CrossRef]
- Sandre, R.M.; Summerbell, R.C. Disseminated Nocardia otitidiscaviarum in a patient with AIDS. Can. J. Infect. Dis. 1997, 8, 347–350. [Google Scholar] [CrossRef]
- Midiri, M.; Finazzo, M.; Bartolotta, T.V.; Maria, M.D. Nocardial adrenal abscess: CT and MR findings. Eur. Radiol. 1998, 8, 466–468. [Google Scholar] [CrossRef]
- Indumathi, V.A.; Shivakumar, A.N.S. Disseminated nocardiosis in an elderly patient presenting with prolonged pyrexia: Diagnosis by thyroid abscess culture. Indian J. Med. Microbiol. 2007, 25, 294–296. [Google Scholar] [CrossRef][Green Version]
- Jimenez-Galanes Marchan, S.; Meneu Díaz, J.C.; Caso Maestro, O.; Perez Saborido, B.; Moreno Elola-Olaso, A.; Abradelo Usera, M.; Fundora Suarez, Y.; Gimeno Calvo, A.; Moreno Molinero, V.; Garcia Reyne, A. Disseminated nocardiosis: A rare infectious complication following Non-heart-beating donor liver transplantation. Transplant. Proc. 2009, 41, 2495–2497. [Google Scholar] [CrossRef]
- Arora, G.; Friedman, M.; Macdermott, R.P. Disseminated Nocardia nova infection. South Med. J. 2010, 103, 1269–1271. [Google Scholar] [CrossRef] [PubMed]
- John, M.A.; Madiba, T.E.; Mahabeer, P.; Naidoo, K.; Sturm, A.W. Disseminated nocardiosis masquerading as abdominal tuberculosis. S. Afr. J. Surg. 2004, 42, 17–19. [Google Scholar]
- Hu, Y.; Zheng, D.; Takizawa, K.; Mikami, Y.; Dai, L.; Yazawa, K.; Fukushima, K.; Lu, C.; Xi, L. Systemic nocardiosis caused by Nocardia concava in China. Med. Mycol. 2011, 49, 662–666. [Google Scholar] [PubMed]
- Xu, J.; Yachnis, A.T.; Malaty, I. An independent elderly woman with rapid onset of coma. JAMA Neurol. 2014, 71, 1043–1047. [Google Scholar] [CrossRef] [PubMed]
- Piau, C.; Kerjouan, M.; Le Mouel, M.; Patrat-Delon, S.; Henaux, P.L.; Brun, V.; Morin, M.P.; Gautier, P.; Rodriguez-Nava, V.; Kayal, S. First case of disseminated infection with Nocardia cerradoensis in a human. J. Clin. Microbiol. 2015, 53, 1034–1037. [Google Scholar] [CrossRef][Green Version]
- Lim, M.Y.; Alker, A.P.; Califano, S.; Trembath, D.G.; Alby, K.; Gilligan, P.H.; Jamieson, K.; Serody, J.S.; Shea, T.C. Concurrent Disseminated Nocardiosis and GI Mucormycosis in a Stem-Cell Transplantation Recipient. J. Clin. Oncol. 2016, 34, e84–e86. [Google Scholar] [CrossRef]
- Senard, O.; Blanot, S.; Jouvion, G.; Rodriguez-Nava, V.; Lortholary, O.; Join-Lambert, O.; Toubiana, J. Fulminant Nocardiosis Due to a Multidrug-Resistant Isolate in a 12-Year-Old Immunocompetent Child. Pediatrics 2018, 141, e20163131. [Google Scholar] [CrossRef]
- Jiang, Y.; Huang, A.; Fang, Q. Disseminated nocardiosis caused by. Exp. Ther. Med. 2016, 12, 3339–3346. [Google Scholar] [CrossRef]
- Bonacini, M.; Walden, J.M. Nocardia brasiliensis peritonitis in a patient with AIDS. Am. J. Gastroenterol. 1990, 85, 1432–1433. [Google Scholar]
- Schlebusch, S.; Nimmo, G.; Carter, R. Bowel abscess with Nocardia veterana associated with colon carcinoma. Pathology 2010, 42, 306–307. [Google Scholar] [CrossRef] [PubMed]
- Arfania, D.; Everett, E.D.; Nolph, K.D.; Rubin, J. Uncommon causes of peritonitis in patients undergoing peritoneal dialysis. Arch. Intern. Med. 1981, 141, 61–64. [Google Scholar] [CrossRef] [PubMed]
- Chan, D.T.; Cheng, I.K.; Chan, P.C.; Mok, K.Y. Nocardia peritonitis complicating continuous ambulatory peritoneal dialysis. Perit. Dial. Int. 1990, 10, 99. [Google Scholar] [CrossRef] [PubMed]
- Kaczmarski, E.B.; Wilkie, M.; Thornhill, C.; Oppenheim, B.A.; Ackrill, P. Problems encountered in diagnosis of Nocardia asteroides peritonitis complicating CAPD. Perit. Dial. Int. 1990, 10, 106. [Google Scholar] [CrossRef]
- Lopes, J.O.; Alves, S.H.; Benevenga, J.P.; Salla, A.; Tatsch, I. Nocardia asteroides peritonitis during continuous ambulatory peritoneal dialysis. Rev. Inst. Med. Trop. Sao Paulo 1993, 35, 377–379. [Google Scholar] [CrossRef]
- Recule, C.; Milongo, R.; Boiron, P.; Croize, J. Nocardia peritonitis complicating CAPD. Perit. Dial. Int. 1994, 14, 297–298. [Google Scholar]
- Dwyer, K.M. Nocardia peritonitis and abdominal abscess complicating continuous ambulatory peritoneal dialysis. Nephrology 2001, 263–265. [Google Scholar] [CrossRef]
- Chu, K.H.; Fung, K.S.; Tsang, W.K.; Chan, H.W.; Tong, K.L. Nocardia peritonitis: Satisfactory response to intraperitoneal trimethoprim-sulfamethoxazole. Perit. Dial. Int. 2003, 23, 197–198. [Google Scholar] [CrossRef]
- Ortiz, A.M.; Rabagliati, R.; Machuca, E. Successful treatment of Nocardia asteroides peritonitis in a patient undergoing automated peritoneal dialysis and receiving immunosuppressive therapy. Adv. Perit. Dial. 2005, 21, 66–68. [Google Scholar]
- Li, S.Y.; Yu, K.W.; Yang, W.C.; Chen, T.W.; Lin, C.C. Nocardia peritonitis—A case report and literature review. Perit. Dial. Int. 2008, 28, 544–547. [Google Scholar] [CrossRef] [PubMed]
- Prasad, N.; Suresh, J.K.; Gupta, A.; Prasad, K.N.; Sharma, R.K. Nocardia asteroides peritonitis in peritoneal dialysis patients: Case report and review of the literature. Indian J. Nephrol. 2011, 21, 276–279. [Google Scholar] [CrossRef] [PubMed]
- El-Naggari, M.; El Nour, I.; Al-Nabhani, D.; Al Muharrmi, Z.; Gaafar, H.; Abdelmogheth, A.A. Nocardia asteroides peritoneal dialysis-related peritonitis: First case in pediatrics, treated with protracted linezolid. J. Infect. Public Health 2016, 9, 192–197. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bosshard, P.P.; Abels, S.; Zbinden, R.; Böttger, E.C.; Altwegg, M. Ribosomal DNA sequencing for identification of aerobic gram-positive rods in the clinical laboratory (an 18-month evaluation). J. Clin. Microbiol. 2003, 41, 4134–4140. [Google Scholar] [CrossRef]
- Wayne, P. Performance Standards for Susceptibility Testing of Mycobacteria, Nocardia spp., and other Aerobic Actinomycetes, 1st ed.; CLSI supplement M62, ed.; Clinical and Laboratory Standards Institute: Wayne, NY, USA, 2018. [Google Scholar]
- Hammoud, M.; Kraft, C.; Pulst-Korenberg, J.; Chenoweth, C.; Gregg, K.S. Disseminated Nocardia paucivorans infection in an immunocompetent host. Infection 2014, 42, 917–920. [Google Scholar] [CrossRef] [PubMed]
- Minero, M.V.; Marin, M.; Cercenado, E.; Rabadan, P.M.; Bouza, E.; Munoz, P. Nocardiosis at the turn of the century. Medicine (Baltimore) 2009, 88, 250–261. [Google Scholar] [CrossRef]
- Yassin, A.F.; Rainey, F.A.; Burghardt, J.; Brzezinka, H.; Mauch, M.; Schaal, K.P. Nocardia paucivorans sp. nov. Int. J. Syst. Evol. Microbiol. 2000, 50 Pt 2, 803–809. [Google Scholar] [CrossRef][Green Version]
- Wellinghausen, N.; Pietzcker, T.; Kern, W.V.; Essig, A.; Marre, R. Expanded spectrum of Nocardia species causing clinical nocardiosis detected by molecular methods. Int. J. Med. Microbiol. 2002, 292, 277–282. [Google Scholar] [CrossRef]
- Eisenblatter, M.; Disko, U.; Stoltenburg-Didinger, G.; Scherubl, H.; Schaal, K.P.; Roth, A.; Ignatius, R.; Zeitz, M.; Hahn, H.; Wagner, J. Isolation of Nocardia paucivorans from the cerebrospinal fluid of a patient with relapse of cerebral nocardiosis. J. Clin. Microbiol. 2002, 40, 3532–3534. [Google Scholar] [CrossRef]
- Wegerle, S.; Markus, A.; Weber, N.; Steffen, H.; King, B.; Eder, W.; Philipp, E.; Morresi-Hauff, A.; Haussinger, K.; Hoffmann, H. Pulmonary nocardiosis with trimethoprime/sulphamethoxazole-resistant Nocardia paucivorans in a patient with no signs of immunosuppression. Pneumologie 2007, 61, 46–51. [Google Scholar] [CrossRef]
- Khan, S.H.; Sanche, S.E.; Robinson, C.A.; Pirouzmand, F. N. paucivorans infection presenting as a brain abscess. Can. J. Neurol. Sci. 2006, 33, 426–427. [Google Scholar] [CrossRef] [PubMed]
- Gray, T.J.; Serisier, D.J.; Gilpin, C.M.; Coulter, C.; Bowler, S.J.; McCormack, J.G. Nocardia paucivorans—A cause of disseminated nocardiosis. J. Infect. 2007, 54, e95–e98. [Google Scholar] [CrossRef] [PubMed]
- Monticelli, J.; Luzzati, R.; Maurel, C.; Rosin, C.; Valentinotti, R.; Farina, C. Brain Abscesses Caused by Nocardia paucivorans in a Multiple Myeloma Patient Treated with Lenalidomide and Dexamethasone: A Case Report and Review of Literature. Mediterr. J. Hematol. Infect. Dis. 2015, 7, e2015011. [Google Scholar] [CrossRef] [PubMed]
- Delavari, N.; Than, K.D.; Chen, K.S.; McKeever, P.E.; Wang, A.C.; Pandey, A.S. Resolution of innumerable cerebral Nocardia paucivorans abscesses after medical management. J. Clin. Neurosci. 2016, 27, 175–177. [Google Scholar] [CrossRef] [PubMed]
- Rafiei, N.; Peri, A.M.; Righi, E.; Harris, P.; Paterson, D.L. Central nervous system nocardiosis in Queensland: A report of 20 cases and review of the literature. Medicine (Baltimore) 2016, 95, e5255. [Google Scholar] [CrossRef]
- Schiaroli, E.; Pasticci, M.B.; De Carolis, E.; Mello, E.; Pallotto, C.; Leli, C.; De Socio, G.V.; Baldelli, F.; Sanguinetti, M.; Mencacci, A. Diagnosis of Nocardia paucivorans central nervous system infection by DNA sequencing from paraffin-embedded tissue. Infez. Med. 2016, 24, 147–152. [Google Scholar]
- Samuel, D.M.G.; Matta, M.; Podgore, J.K. Nocardia Paucivorans Empyema in a Patient with Suspected Silicosis. Am. J. Respir. Crit. Care Med. 2018, 2018, 197. [Google Scholar]
- Wilson, J.W. Nocardiosis: Updates and clinical overview. Mayo Clin. Proc. 2012, 87, 403–407. [Google Scholar] [CrossRef]
| Case n°/Reference | Year ** | Age | Sex | Site | Immune Status | Therapy Regimen | Therapy Duration | Outcome |
|---|---|---|---|---|---|---|---|---|
| 1 [58] | 2000 | 51 | M | Sputum | Chronic lung disease | NR | NR | NR |
| 2 [59] | 2002 | 40 | F | Brain abscess | NR | NR | NR | NR |
| 3 [60] | 2002 | 63 | M | Brain abscess | Low CD4+ count of unknown origin | Cef, Amp, Amk, Mer, Levo, Mino | >6 months | survived |
| 4 [61] | 2006 | 54 | M | Sputum, BAL, lung biopsy | Immunocompetent | TMP/SMX, A/clav, Cip | 6 months | NR |
| 5 [62] | 2006 | 63 | M | Brain abscess | Immunocompetent | Surgical resection, TMP/SMX | 3 months | survived |
| 6 [63] | 2007 | 52 | M | Lung abscess | NR | NR | NR | died |
| 7 [63] | 2007 | 55 | M | Brain abscess | NR | NR | NR | NR |
| 8 [63] | 2007 | NR | M | Pleural fluid | NR | NR | NR | NR |
| 9 [63] | 2007 | 44 | M | Mediastinal lymph node | NR | NR | NR | NR |
| 10 [63] | 2007 | 78 | F | Lung abscess | Chronic lung disease | NR | NR | NR |
| 11 [63] | 2007 | 50 | F | Sputum | NR | NR | NR | NR |
| 12 [63] | 2007 | 41 | M | Brain abscess | Hodgkin’s lymphoma | NR | NR | NR |
| 13 [63] | 2007 | 53 | M | Lung abscess | NR | NR | NR | NR |
| 14 [63] | 2007 | 58 | F | Brain abscess | Corticosteroid therapy | NR | NR | NR |
| 15 [63] | 2007 | 66 | F | Sputum | NR | NR | NR | NR |
| 16 [63] | 2007 | 54 | M | Endocarditis, brain abscess, | NR | NR | NR | NR |
| skin abscess | ||||||||
| 17 [63] | 2007 | 65 | F | Sputum | NR | NR | NR | NR |
| 18 [63] | 2007 | 72 | F | Lung abscess | Corticosteroid therapy | NR | NR | NR |
| 19 [63] | 2007 | 66 | M | Brain abscess | Immunosuppression * | NR | NR | NR |
| 20 [63] | 2007 | 74 | M | BAL fluid | NR | NR | NR | NR |
| 21 [63] | 2007 | NR | M | Sputum | NR | NR | NR | NR |
| 22 [63] | 2007 | 74 | M | Skin abscess | NR | NR | NR | NR |
| 23 [63] | 2007 | 57 | M | Brain abscess, pneumonia | NR | NR | NR | NR |
| 24 [63] | 2007 | 80 | M | Lung, skin | NR | NR | NR | NR |
| 25 [63] | 2007 | 62 | M | Skin | Immunocompetent | NR | NR | NR |
| 26 [63] | 2007 | 87 | M | Sputum | NR | NR | NR | NR |
| 27 [63] | 2007 | 77 | F | BAL fluid | Immunocompetent | NR | NR | NR |
| 28 [63] | 2007 | 50 | M | Sputum | Lung cancer | NR | NR | NR |
| 29 [63] | 2007 | 67 | M | Brain abscess | Diabetes mellitus | NR | NR | NR |
| 30 [63] | 2007 | 67 | M | Sputum | Immunocompetent | NR | NR | NR |
| 31 [63] | 2007 | 47 | F | Sputum | NR | NR | NR | NR |
| 32 [63] | 2007 | 66 | F | Sputum | Previous lung infection | NR | NR | NR |
| 33 [63] | 2007 | 46 | M | Sputum | Immunocompetent | NR | NR | NR |
| 34 [63] | 2007 | 79 | M | Pleural fluid | Corticosteroid therapy | NR | NR | NR |
| 35 [63] | 2007 | 76 | M | Pleural fluid | Immunocompetent | NR | NR | NR |
| 36 [63] | 2007 | 61 | M | Skin abscess | NR | NR | NR | NR |
| 37 [63] | 2007 | 60 | M | Blood | Chemotherapy | NR | NR | NR |
| 38 [63] | 2007 | 53 | M | BAL fluid and skin lesion | Smoking and other drug abuse, Hepatitis C | Tica/clav, Rox, TMP/SMX | 12 months | survived |
| 39 [56] | 2014 | 50 | M | M. iliopsoas, brain, lung, | Smoking and other drug abuse | TMP/SMX, Imi, Mox | 12 months | survived |
| mediastinal lymph nodes | ||||||||
| 40 [64] | 2015 | 70 | M | Brain abscesses | Multiple Myeloma under chemotherapy | TMP/SMX, Mer, Cip | 12 months | survived |
| 41 [65] | 2016 | 50 | M | Brain abscesses | Smoking and other drug abuse | TMP/SMX, Imi, Line, Mox | 12 months | survived |
| 42 [66] | 2016 | 80 | F | Brain and lung abscess | Immunocompetent | Surgical resection, TMP/SMX, Cef | 9 months | survived |
| 43 [66] | 2016 | 50 | M | Spinal cord, lung | Alcohol abuse | Surgical resection, TMP/SMX, Mer, Cef | 9 months | survived |
| 44 [66] | 2016 | 59 | M | Brain and lung abscess | Immunocompetent | TMP/SMX, Mer | 12 months | survived |
| 45 [67] | 2016 | 54 | M | Brain abscess | Immunocompetent | Cef, Met, Mer, Line, Imi, Van, Rif, TMP/SMX | 21 weeks | survived |
| 46 [3] | 2018 | 61 | M | Brain abscess | Myasthenia gravis, corticosteroid therapy | TMP/SMX, Cef, Met, Line, Levo | 11 months | survived |
| 47 [2] | 2018 | 66 | F | Renal abscess | Post Lung Transplantation | TMP/SMX, Imi | 9–12 months | survived |
| 48 [68] | 2018 | 42 | M | Lung empyema | Suspected silicosis | TMP/SMX | NR | survived |
| 49 [4] | 2019 | 52 | F | Brain abscess | Immunocompetent | Surgical resection, Cef, TMP/SMX, Levo | 13 months | survived |
| 50 [present report] | 81 | M | Abscess in right adrenal loge | B-Cell Lymphoma, Hypogammaglobulinemia | Surgical resection, A/clav, TMP/SMX, Amk, Cef, Mino, Cip | 6 months | survived |
| Case n°/Reference | Year ** | Age | Sex | Species | Site | Immune Status | Therapy Regimen | Therapy Duration | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| 1 [28] | 1976 | 49 | F | NR | Spleen abscess | Immunocompetent | Sulfisoxazole | NR | survived |
| 2 [9] | 1981 | 26 | F | N. asteroides | Perirenal area * | Post renal transplant | Sulphatriad, fusidic acid | NR | survived |
| 3 [10] | 1983 | 11 | F | N. asteroides | Liver and kidney abscesses | Immunocompetent | Surgical resection, Amk, TMP/SMX, Sulphadimidine | 12 weeks | survived |
| 4 [11] | 1986 | 76 | M | N. asteroides | Pancreas abscess | Immunocompetent | Surgical resection, A/clav, Amk, Orn, TMP/SMX | NR | survived |
| 5 [41] | 1990 | 19 | M | N. brasiliensis | Cholecystitis and Peritonitis | AIDS | NR | 7 days | died |
| 6 [12] | 1991 | 38 | M | N. asteroides | Left suprarenal abscess | AIDS | Surgical resection | NR | died |
| 7 [13] | 1996 | 67 | M | N. asteroides | Abdominal aortic aneurysm | Immunocompetent | TMP/SMX, Amk | NR | survived |
| 8 [14] | 2003 | 42 | M | N. farcinica | Psoas abscess | Immunocompetent | TMP/SMX | 11 months | survived |
| 9 [15] | 2004 | 37 | F | NR | Abdominal abscess | M. Crohn | NR | NR | NR |
| 10 [5] | 2004 | 34 | M | N. asteroides | Left Adrenal abscess | AIDS | Surgical resection, TMP/SMX, Cef | NR | survived |
| 11 [16] | 2007 | 25 | F | NR | Bilateral kidney abscesses | Corticosteroids and Azathioprin for SLE | Methylprednisolone | NR | died |
| 12 [17] | 2007 | 44 | F | NR | Jejunum | Post liver transplant | Surgical resection, Imi, Van | NR | died |
| 13 [18] | 2009 | 55 | M | NR | Kidney abscess | AIDS | Surgical resection | NR | NR |
| 14 [42] | 2010 | 83 | F | N. veterana | Bowel abscess | Colon cancer | Surgical resection, Cef, Gen, Met, TMP/SMX | NR | survived |
| 15 [19] | 2011 | 32 | F | NR | Bilateral abscesses of ovaries and fallopian tubes, omentum | Immunocompetent | Surgical resection, Mino, TMP/SMX, Amk, Line, Cip | 6 Months | survived |
| 16 [20] | 2012 | 59 | F | N. farcinica | Right adrenal compartment | Chronic hepatitis C, post treatment for lymphoma | Amk, Cefu, TMP/SMX | 4 months | died |
| 17 [21] | 2012 | 54 | F | NR | Colon | Immunocompetent | Surgical resection, antibiotics not specified | NR | survived |
| 18 [22] | 2013 | 30 | F | NR | Left adnexal collection * | Immunocompetent | TMP/SMX, Amk | 6 months | survived |
| 19 [24] | 2016 | 58 | F | N. farcinica | Colon, blood | TNFa-antagonist for M. Crohn | Van, Met, Imi, Amk, TMP/SMX | 12 months | survived |
| 20 [23] | 2017 | 59 | M | N. farcinica | Liver abscess | Post liver transplant | TMP/SMX, Amk, Imi | NR | survived |
| 21 [2] | 2018 | 63 | F | N. paucivorans | Renal abscess | Post lung transplant | Surgical resection, Imi, TMP/SMX | 9–12 months | NR |
| 22 [25] | 2019 | 63 | M | N. farcinica | Liver (hepatitis) | Immunocompetent | TMP/SMX, Amk | 4 weeks | died |
| 23 [26] | 2019 | 11 | F | N. farcinica | Abdominal abscesses | Post renal transplant | TMP/SMX, Mer, Imi, Cila, Line | NR | NR |
| 24 [present report] | 81 | M | N. paucivorans | Right adrenal space | B-Cell Lymphoma, Hypogammaglobulinemia | Surgical resection, A/clav, TMP/SMX, Amk, Cef, Mino, Cip | 6 months | survived |
| Case n°/Reference | Year ** | Age | Sex | Species | Site | Immune Status | Therapy Regimen | Therapy Duration | Outcome |
|---|---|---|---|---|---|---|---|---|---|
| 1 [27] | 1975 | 13 | M | N. asteroides | Lungs, liver, pancreas, lymph nodes | Immunocompetent | Surgical resection, sulphadiazine, sulfisoxazole | 6 months | NR |
| 2 [29] | 1997 | 59 | M | N. otitidiscaviarum | Thoracoabdominal abscess, lung | HIV positive | Surgical drainage, TMP/SMX, Amk, Cefotaxime | NR | survived |
| 3 [30] | 1998 | 49 | F | N. asteroides | Left adrenal abscess, spleen, lung | chronic steroids for RA | Surgical resection | NR | survived |
| 4 [34] | 2004 | 32 | M | N. brasiliensis | Lung, intestines | AIDS | Surgical resection | NR | died |
| 5 [17] | 2007 | 30 | M | N. asteroides | Lung, pleura, abdomen * | Post kidney transplant, chemotherapy, corticosteroids | NR | NR | survived |
| 6 [31] | 2007 | 67 | M | N. asteroides | Pancreas, omentum, brain, lungs, thyroid | Chronic steroids for Still’s disease | Mer, Amk, TMP/SMX | NR | died |
| 7 [32] | 2009 | 69 | M | N. farcinica | Adrenal glands, brain, lung, skin, muscle | Post liver transplant | TMP/SMX | 7 months | survived |
| 8 [6] | 2010 | 66 | F | N. farcinica | Brain, bilateral adrenal abscesses, abdominal lymph nodes | aTNF-therapy for Psoriasis | Van, Amp, Mer, Voriconazole, TMP/SMX, Line | 2.5 months | died |
| 9 [33] | 2010 | 61 | F | N. nova | Lung, skin, kidney, pancreas, brain | Chronic steroids and Azathioprine for ulcerative colitis | TMP/SMX | 1 year | survived |
| 10 [35] | 2011 | 42 | M | N. concava | Lung, liver | Chronic steroids for polychondritis | Sulphadiazine, Van, Imi, Cip, Amk | 25 days | died |
| 11 [20] | 2012 | 68 | F | N. farcinica | Right kidney abscess, brain abscess, lung | Anorexia nervosa | Cef, Erythromycin, TMP/SMX, Amk, Imi, Cip | 65 days | died |
| 12 [36] | 2014 | 75 | M | N. farcinica | Kidney, liver, spleen, lung, brain | Immunocompetent | Mer, Van, Cefepime, Doxycycline, Acilovir | 3 days | died |
| 13 [37] | 2015 | 59 | F | N. cerradoensis | Brain, skin, retroperitoneum, lung | Post renal transplant | Mer, Amk | 3 months | survived |
| 14 [40] | 2016 | 37 | M | N. otitidiscaviarum | Subcutaneous soft tissue, liver, lung | Immunocompetent | Cef, TMP/SMX, Mino | NR | survived |
| 15 [38] | 2016 | 58 | M | N. nova | Lung, ileum | B-cell Non-Hodgkin lymphoma | TMP/SMX, Imi | 11 months | died |
| 16 [39] | 2018 | 12 | M | N. elegans/aobensis/ africana complex | Kidney, lung, brain | Immunocompetent | Pip/Taz, Amk, Imi, Cip | 6 days | died |
| Case n°/Reference | Year ** | Age | Sex | Species | Cause of ESRD | Therapy Regimen | Therapy Duration | Outcome | Catheter Removal |
|---|---|---|---|---|---|---|---|---|---|
| 1 [43] | 1981 | 70 | M | N. asteroides | CIN | Ceph, Sulf | 6 weeks | survived | No |
| 2 [44] | 1990 | 60 | M | NR | PCKD | Ofl, Tob, Ceph, Van, Azt, TMP/SMX | 8 weeks | survived | No |
| 3 [45] | 1990 | 58 | F | N. asteroides | NR | Ceft, Net, Van, TMP/SMX | NR | survived | Yes |
| 4 [46] | 1993 | 38 | M | N. asteroides | SLE | Ceph, TMP/SMX | 4 weeks | died | No |
| 5 [47] | 1994 | 80 | M | N. nova | NR | TMP/SMX | 3 weeks | survived | Yes |
| 6 [48] | 2001 | 32 | M | N. nova | Type 1 DM | TMP/SMX, Imi | 4 months | survived | Yes |
| 7 [49] | 2003 | 68 | F | N. nova | Unknown | Cefa, Net, Ceft, Amk, Imi, TMP/SMX, Cef | 2 weeks | died | No |
| 8 [50] | 2005 | 35 | M | N. asteroides | CBUS | Van, Ceft, TMP/SMX, Amk, Cefu | 19 weeks | survived | No |
| 9 [51] | 2008 | 75 | M | NR | Type 2 DM | Van, TMP/SMX | 11 weeks | survived | Yes |
| 10 [8] | 2008 | 66 | M | N. asteroides | Type 2 DM | Cefa, Gen TMP/SMX | 12 months | survived | Yes |
| 11 [52] | 2011 | 57 | M | N. asteroides | Type 2 DM | Van, Ceft, TMP/SMX, Cef, Cip | 2 weeks | died | Yes |
| 12 [53] | 2016 | 13 | F | N. asteroides | DGS | Van, Cip, Ceft, Line | 8 months | survived | Yes |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tramèr, L.; Mertz, K.D.; Huegli, R.; Hinic, V.; Jost, L.; Burkhalter, F.; Wirz, S.; Tarr, P.E. Intra-Abdominal Nocardiosis—Case Report and Review of the Literature. J. Clin. Med. 2020, 9, 2141. https://doi.org/10.3390/jcm9072141
Tramèr L, Mertz KD, Huegli R, Hinic V, Jost L, Burkhalter F, Wirz S, Tarr PE. Intra-Abdominal Nocardiosis—Case Report and Review of the Literature. Journal of Clinical Medicine. 2020; 9(7):2141. https://doi.org/10.3390/jcm9072141
Chicago/Turabian StyleTramèr, Lucas, Kirsten D. Mertz, Rolf Huegli, Vladimira Hinic, Lorenz Jost, Felix Burkhalter, Sebastian Wirz, and Philip E. Tarr. 2020. "Intra-Abdominal Nocardiosis—Case Report and Review of the Literature" Journal of Clinical Medicine 9, no. 7: 2141. https://doi.org/10.3390/jcm9072141
APA StyleTramèr, L., Mertz, K. D., Huegli, R., Hinic, V., Jost, L., Burkhalter, F., Wirz, S., & Tarr, P. E. (2020). Intra-Abdominal Nocardiosis—Case Report and Review of the Literature. Journal of Clinical Medicine, 9(7), 2141. https://doi.org/10.3390/jcm9072141





