Estimated Population Prevalence of Heart Failure with Reduced Ejection Fraction in Spain, According to DAPA-HF Study Criteria
Abstract
1. Introduction
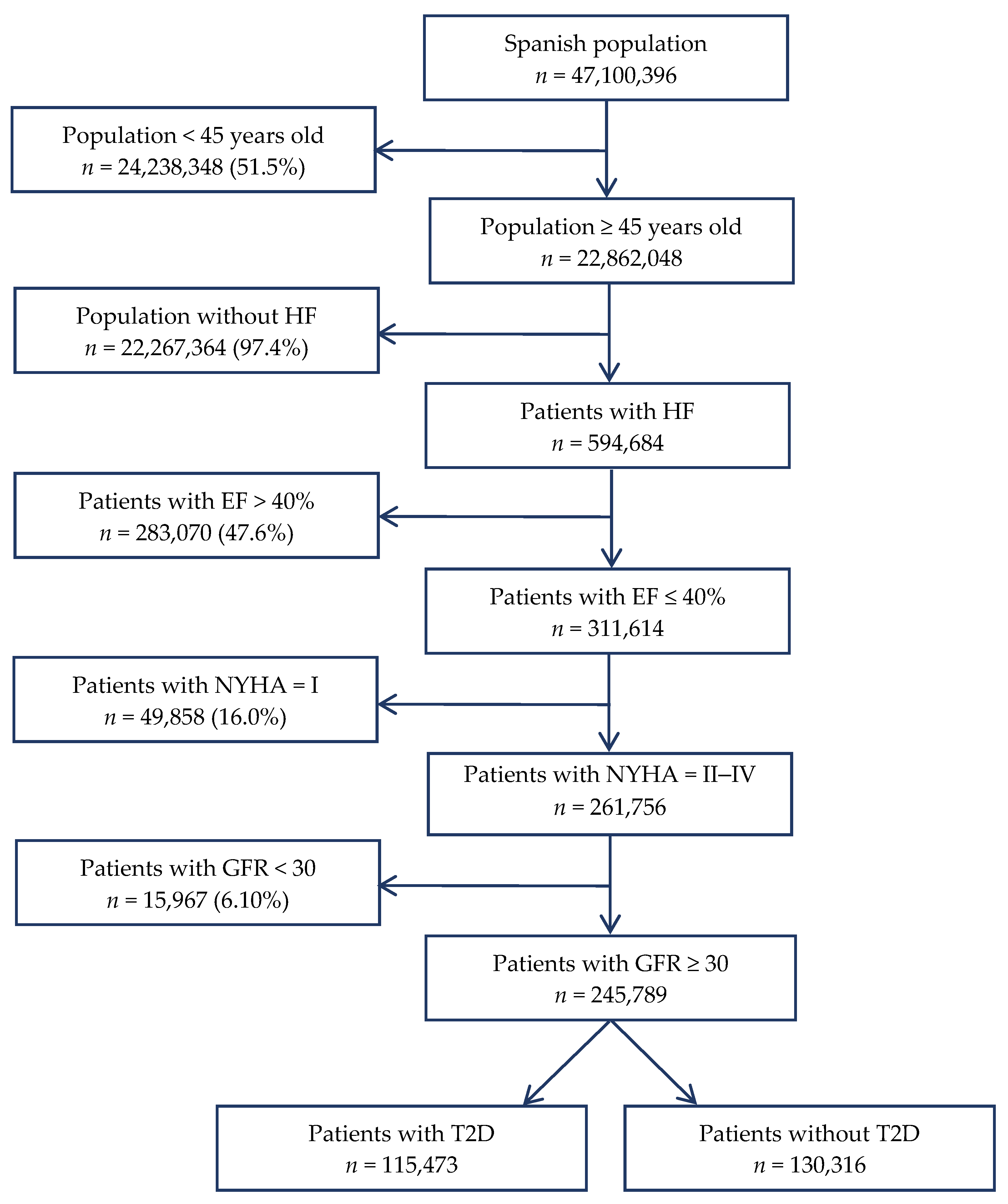
2. Materials and Methods
2.1. Study Design and Population
2.2. Estimation of Population Prevalence and Number of Patients with Heart Failure in Spain
2.3. Estimation of Ejection Fraction ≤ 40% and New York Heart Association Functional Class II–IV Prevalence in the Heart Failure Population in Spain
- RICA (National Registry for Heart Failure), carried out in internal medicine units in 52 public and private hospitals [27];
- REDINSCOR (Spanish Network for Heart Failure), carried out in HF units in 18 hospitals [27];
- BADAPIC (Database of Patients with Heart Failure), involving 62 centres with specific HF units or clinics [6];
- INCA (Heart Failure Study), involving 415 primary care physicians and 93 cardiologists [7];
- EPISERVE (Heart Failure in Outpatients), carried out by 181 primary care physicians, 172 cardiologists, and 154 internal medicine physicians [28];
- GALICAP (Galician Study of Heart Failure in Primary Care), involving 149 primary care physicians distributed in eight areas of Galicia [29].
2.4. Estimation of Glomerular Filtration Rate ≥ 30 mL/min/1.73 m² Prevalence in the Heart Failure Population in Spain
2.5. Estimation of Type 2 Diabetes Mellitus Prevalence in the Heart Failure Population in Spain
2.6. Statistical Analysis
3. Results
3.1. Estimation of Population Prevalence and Number of Patients with Heart Failure in Spain
3.2. Estimation of Ejection Fraction ≤ 40% and New York Heart Association Functional Class II–IV Prevalence in the Heart Failure Population in Spain
3.3. Estimation of Glomerular Filtration Rate ≥ 30 mL/min/1.73 m² Prevalence in the Heart Failure Population in Spain
3.4. Estimation of Type 2 Diabetes Mellitus Prevalence in the Heart Failure Population in Spain
4. Discussion
4.1. Main Findings
4.2. Reliability of Prevalence Estimates
4.3. Potential Translational Perspective
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.; Coats, A.; Falk, V.; González-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC)Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [CrossRef] [PubMed]
- Heidenreich, P.A.; Albert, N.M.; Allen, L.A.; Bluemke, D.A.; Butler, J.; Fonarow, G.C.; Ikonomidis, J.S.; Khavjou, O.; Konstam, M.A.; Maddox, T.M.; et al. Forecasting the impact of heart failure in the United States: A policy statement from the American Heart Association. Circ. Hear. Fail. 2013, 6, 606–619. [Google Scholar] [CrossRef]
- Carlisle, M.A.; Fudim, M.; Devore, A.D.; Piccini, J.P. Heart Failure and Atrial Fibrillation, Like Fire and Fury. JACC: Hear. Fail. 2019, 7, 447–456. [Google Scholar] [CrossRef] [PubMed]
- National Statistics Institute. INEbase. Deaths according to Causes by Sex and Age Group. Available online: https://www.ine.es/jaxiT3/Datos.htm?t=7947#!tabs-tabla (accessed on 18 March 2020).
- Chioncel, O.; Lainscak, M.; Seferovic, P.M.; Anker, S.; Crespo-Leiro, M.G.; Harjola, V.-P.; Parissis, J.; Laroche, C.; Piepoli, M.; Fonseca, C.; et al. Epidemiology and one-year outcomes in patients with chronic heart failure and preserved, mid-range and reduced ejection fraction: An analysis of the ESC Heart Failure Long-Term Registry. Eur. J. Hear. Fail. 2017, 19, 1574–1585. [Google Scholar] [CrossRef] [PubMed]
- Jiménez-Navarro, M.; Castillo, J.; Marrero, M.A.R.; Anguita-Sánchez, M. Influence of Gender on Long-term Prognosis of Patients With Chronic Heart Failure Seen in Heart Failure Clinics. Clin. Cardiol. 2010, 33, E13–E18. [Google Scholar] [CrossRef] [PubMed]
- Otero, B.; Permanyer-Miralda, G.; Cuixart, C.B.; Costa, J.A.; Blázquez, E.S.; INCA investigators. Clinical profile and management patterns in outpatients with heart failure in Spain: INCA study. Aten. Primaria 2009, 41, 394–401. [Google Scholar] [CrossRef]
- Lupón, J.; Díez-López, C.; De Antonio, M.; Domingo, M.; Zamora, E.; Moliner, P.; González, B.; Santesmases, J.; Troya, M.I.; Bayés-Genís, A. Recovered heart failure with reduced ejection fraction and outcomes: A prospective study. Eur. J. Hear. Fail. 2017, 19, 1615–1623. [Google Scholar] [CrossRef] [PubMed]
- Delgado, J.F.; Oliva, J.; Llano, M.; Pascual-Figal, D.A.; Grillo, J.J.; Comin-Colet, J.; Díaz, B.; De La Concha, L.M.; Martí, B.; Peña, L.M.; et al. Health Care and Nonhealth Care Costs in the Treatment of Patients with Symptomatic Chronic Heart Failure in Spain. Rev. Esp. Cardiol. (Eng. Ed.) 2014, 67, 643–650. [Google Scholar] [CrossRef]
- Oliva, J.; Jorgensen, N.; Barrios, J.M.R. Carga socioeconómica de la insuficiencia cardíaca: Revisión de los estudios de coste de la enfermedad. Pharm. Span. Res. Artic. 2010, 7, 68–79. [Google Scholar] [CrossRef]
- Farré, N.; Vela, E.; Cleries, M.; Bustins, M.; Cainzos-Achirica, M.; Enjuanes, C.; Moliner, P.; Ruiz, S.; Rotellar, J.M.V.; Lupón, J. Medical resource use and expenditure in patients with chronic heart failure: A population-based analysis of 88 195 patients. Eur. J. Hear. Fail. 2016, 18, 1132–1140. [Google Scholar] [CrossRef]
- Roux, J.A.F.-L.; Comin, J.; Pedro-Botet, J.; Benaiges, D.; Dou, J.P.-D.; Chillarón, J.J.; Goday, A.; Bruguera, J.; Cano-Perez, J.F. Seven-year mortality in heart failure patients with undiagnosed diabetes: An observational study. Cardiovasc. Diabetol. 2011, 10, 39. [Google Scholar] [CrossRef] [PubMed]
- Alcober-Morte, L.; Barrio-Ruiz, C.; Parellada-Esquius, N.; Subirana, I.; Comín-Colet, J.; Grau, M.; Dégano, I.R.; Cainzos-Achirica, M.; Cunillera-Puértolas, O.; Cobo-Guerrero, S.; et al. Heart failure admission across glomerular filtration rate categories in a community cohort of 125,053 individuals over 60 years of age. Hypertens. Res. 2019, 42, 2013–2020. [Google Scholar] [CrossRef]
- Farré, N.; Vela, E.; Clèries, M.; Bustins, M.; Cainzos-Achirica, M.; Enjuanes, C.; Moliner, P.; Ruiz, S.; Rotellar, J.M.V.; Comín-Colet, J. Real world heart failure epidemiology and outcome: A population-based analysis of 88,195 patients. PLoS ONE 2017, 12, e0172745. [Google Scholar] [CrossRef]
- Sánchez, M.A.; Leiro, M.G.C.; Galván, E.D.T.; Jiménez-Navarro, M.; Alonso-Pulpón, L.; García, J.M.; on behalf of the PRICE study investigators. Prevalence of heart failure in the Spanish general population aged over 45 years. The PRICE Study. Rev. Esp. Cardiol. 2008, 61, 1041–1049. [Google Scholar] [CrossRef]
- Cortina, A.; Reguero, J.; Segovia, E.; Lambert, J.L.R.; Cortina, R.; Arias, J.C.; Vara, J.; Torre, F. Prevalence of heart failure in Asturias (a region in the North of Spain). Am. J. Cardiol. 2001, 87, 1417–1419. [Google Scholar] [CrossRef]
- Ohlmeier, C.; Mikolajczyk, R.; Frick, J.; Prütz, F.; Haverkamp, W.; Garbe, E. Incidence, prevalence and 1-year all-cause mortality of heart failure in Germany: A study based on electronic healthcare data of more than six million persons. Clin. Res. Cardiol. 2015, 104, 688–696. [Google Scholar] [CrossRef] [PubMed]
- Parén, P.; Schaufelberger, M.; Björck, L.; Lappas, G.; Fu, M.; Rosengren, A. Trends in prevalence from 1990 to 2007 of patients hospitalized with heart failure in Sweden. Eur. J. Hear. Fail. 2014, 16, 737–742. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; de Ferranti, S.; Després, J.P.; Fullerton, H.J.; Howard, V.J.; et al. Heart disease and stroke statistics--2015 update: A report from the American Heart Association. Circulation 2015, 131, e29–e322. [Google Scholar] [CrossRef] [PubMed]
- Taylor, C.; Ordóñez-Mena, J.M.; Roalfe, A.K.; Lay-Flurrie, S.; Jones, N.; Marshall, T.; Hobbs, F.D.R. Trends in survival after a diagnosis of heart failure in the United Kingdom 2000-2017: Population based cohort study. BMJ 2019, 364, l223. [Google Scholar] [CrossRef]
- Baglioni, P.; Wiviott, S.D.; Raz, I.; Sabatine, M.S.; Akinci, B. Dapagliflozin and Cardiovascular Outcomes in Type 2 Diabetes. N. Engl. J. Med. 2019, 380, 1880–1881. [Google Scholar] [CrossRef]
- McMurray, J.; Solomon, S.D.; Inzucchi, S.E.; Køber, L.; Kosiborod, M.N.; Martinez, F.A.; Ponikowski, P.; Sabatine, M.S.; Anand, I.S.; Bělohlávek, J.; et al. Dapagliflozin in Patients with Heart Failure and Reduced Ejection Fraction. N. Engl. J. Med. 2019, 381, 1995–2008. [Google Scholar] [CrossRef]
- Crespo-Leiro, M.G.; Barge-Caballero, E.; Segovia-Cubero, J.; González-Costello, J.; López-Fernández, S.; García-Pinilla, J.M.; Almenar-Bonet, L.; De Juan-Bagudá, J.; Roig-Minguell, E.; Bayés-Genís, A.; et al. Hyperkalemia in heart failure patients in Spain and its impact on guidelines and recommendations: ESC-EORP-HFA Heart Failure Long-Term Registry. Rev. Esp. Cardiol. (Eng. Ed.) 2020, 73, 313–323. [Google Scholar] [CrossRef]
- Hernáez, Á.; Delgado, J.F.; Cinca, J.; Fernández-Avilés, F.; Marrugat, J. Prevalence and incidence of hyperkalaemia in the Spanish population with heart failure with reduced ejection fraction: A systematic review and populational relevance. Rev. Clin. Esp. 2018, 218, 253–260. [Google Scholar] [CrossRef]
- McMurray, J.J.; DeMets, D.L.; Inzucchi, S.E.; Køber, L.; Kosiborod, M.N.; Langkilde, A.M.; Martinez, F.A.; Bengtsson, O.; Ponikowski, P.; Sabatine, M.S.; et al. A trial to evaluate the effect of the sodium–glucose co-transporter 2 inhibitor dapagliflozin on morbidity and mortality in patients with heart failure and reduced left ventricular ejection fraction (DAPA-HF). Eur. J. Hear. Fail. 2019, 21, 665–675. [Google Scholar] [CrossRef]
- National Statistics Institute. INEbase. Resident Population by Date, Sex, Age Group and Nationality. Available online: https://www.ine.es/jaxiT3/Tabla.htm?t=9683&L=0 (accessed on 5 February 2020).
- Álvarez-García, J.; Salamanca-Bautista, P.; Ferrero-Gregori, A.; Montero-Pérez-Barquero, M.; Puig, T.; Aramburu-Bodas, Ó.; Vázquez, R.; Formiga, F.; Delgado, J.; Delgado, J.F.; et al. Prognostic Impact of Physician Specialty on the Prognosis of Outpatients With Heart Failure: Propensity Matched Analysis of the REDINSCOR and RICA Registries. Rev. Esp. Cardiol. (Eng. Ed.) 2017, 70, 347–354. [Google Scholar] [CrossRef]
- González-Juanatey, J.R.; Ezquerra, E.A.; Martínez-Sellés, M.; Gutiérrez, P.C.; Nocito, A.D.S.; Fradera, I.Z. Heart failure in outpatients: Comorbidities and management by different specialists. The EPISERVE Study. Rev. Esp. Cardiol. 2008, 61, 611–619. [Google Scholar] [CrossRef]
- Otero-Raviña, F.; Grigorian-Shamagian, L.; Fransi-Galiana, L.; Názara-Otero, C.; Fernández-Villaverde, J.M.; Del Alamo-Alonso, A.; Nieto-Pol, E.; De Santiago-Boullón, M.; López-Rodríguez, I.; Cardona-Vidal, J.M.; et al. Galician study of heart failure in primary care (GALICAP Study). Rev. Esp. Cardiol. 2007, 60, 373–383. [Google Scholar] [CrossRef] [PubMed]
- Pascual-Figal, D.A.; Ferrero-Gregori, A.; Otero, I.G.; Vazquez-Garcia, R.; Delgado, J.F.; Álvarez-García, J.; Gimeno, J.R.; Worner-Diz, F.; Bardají, A.; Alonso-Pulpon, L.; et al. Mid-range left ventricular ejection fraction: Clinical profile and cause of death in ambulatory patients with chronic heart failure. Int. J. Cardiol. 2017, 240, 265–270. [Google Scholar] [CrossRef] [PubMed]
- Murphy, N.F.; Simpson, C.R.; McAlister, F.A.; Stewart, S.; MacIntyre, K.; Kirkpatrick, M.; Chalmers, J.; Redpath, A.; Capewell, S.; McMurray, J.J. National survey of the prevalence, incidence, primary care burden, and treatment of heart failure in Scotland. Heart 2004, 90, 1129–1136. [Google Scholar] [CrossRef] [PubMed]
- Bleumink, G.S.; Knetsch, A.M.; Sturkenboom, M.C.J.M.; Straus, S.; Hofman, A.; Deckers, J.W.; Witteman, J.C.; Stricker, B.H. Quantifying the heart failure epidemic: Prevalence, incidence rate, lifetime risk and prognosis of heart failure The Rotterdam Study. Eur. Hear. J. 2004, 25, 1614–1619. [Google Scholar] [CrossRef] [PubMed]
- Ceia, F.; Fonseca, C.; Mota, T.; Morais, H.; Matias, F.; De Sousa, A.; Oliveira, A.G.; on behalf of the EPICA Investigators. Prevalence of chronic heart failure in Southwestern Europe: The EPICA study. Eur. J. Hear. Fail. 2002, 4, 531–539. [Google Scholar] [CrossRef]
- Zinman, B.; Wanner, C.; Lachin, J.M.; Fitchett, D.; Bluhmki, E.; Hantel, S.; Mattheus, M.; Devins, T.; Johansen, O.E.; Woerle, H.J.; et al. Empagliflozin, Cardiovascular Outcomes, and Mortality in Type 2 Diabetes. N. Engl. J. Med. 2015, 373, 2117–2128. [Google Scholar] [CrossRef] [PubMed]
- Neal, B.; Perkovic, V.; Mahaffey, K.W.; De Zeeuw, D.; Fulcher, G.; Erondu, N.; Shaw, W.; Law, G.; Desai, M.; Matthews, D.R.; et al. Canagliflozin and Cardiovascular and Renal Events in Type 2 Diabetes. N. Engl. J. Med. 2017, 377, 644–657. [Google Scholar] [CrossRef] [PubMed]
- Figtree, G.A.; Rådholm, K.; Barrett, T.D.; Perkovic, V.; Mahaffey, K.W.; De Zeeuw, D.; Fulcher, G.; Matthews, D.R.; Shaw, W.; Neal, B. Effects of Canagliflozin on Heart Failure Outcomes Associated With Preserved and Reduced Ejection Fraction in Type 2 Diabetes Mellitus. Circulation 2019, 139, 2591–2593. [Google Scholar] [CrossRef]
- Kato, E.T.; Silverman, M.G.; Mosenzon, O.; Zelniker, T.A.; Cahn, A.; Furtado, R.H.M.; Kuder, J.; Murphy, S.A.; Bhatt, D.L.; Leiter, L.A.; et al. Effect of Dapagliflozin on Heart Failure and Mortality in Type 2 Diabetes Mellitus. Circulation 2019, 139, 2528–2536. [Google Scholar] [CrossRef]
- Crespo-Leiro, M.G.; Anker, S.; Maggioni, A.P.; Coats, A.J.; Filippatos, G.; Ruschitzka, F.; Ferrari, R.; Piepoli, M.; Delgado, J.F.; Metra, M.; et al. European Society of Cardiology Heart Failure Long-Term Registry (ESC-HF-LT): 1-year follow-up outcomes and differences across regions. Eur. J. Hear. Fail. 2016, 18, 613–625. [Google Scholar] [CrossRef] [PubMed]
- De Frutos, F.; Mirabet, S.; Ortega-Paz, L.; Buera, I.; Darnés, S.; Farré, N.; Perez, B.; Adeliño, R.; Bascompte, R.; Pérez-Rodón, J.; et al. Management of Heart Failure with Reduced Ejection Fraction after ESC 2016 Heart Failure Guidelines: The Linx Registry. ESC Hear. Fail. 2020, 7, 26–36. [Google Scholar] [CrossRef]
| Inclusion Criteria |
| (1) Provision of signed informed consent prior to any study specific procedures |
| (2) Men or women, aged ≥18 years at the time of consent |
| (3) Diagnosis of HF with left ventricular EF ≤ 40%, which has been present for at least 12 months prior to enrolment |
| (4) Diagnosis of symptomatic HF (NYHA functional class II–IV), within the previous 2 months |
| (5) Optimally treated with pharmacological and/or device therapy for HF |
| (6) NT-proBNP ≥ 600 pg/mL (or if hospitalised for HF within the previous 12 months, NT-proBNP ≥ 400 pg/mL) at enrolment. Patients with atrial fibrillation or atrial flutter must have a level ≥900 pg/mL, irrespective of history of HF hospitalization |
| Exclusion Criteria |
| (1) Treatment with SGLT2 inhibitors within 8 weeks prior to enrolment, or previous intolerance of an SGLT2 inhibitor |
| (2) Diagnosis of type 1 diabetes mellitus |
| (3) Symptomatic hypotension or systolic blood pressure <95 mmHg |
| (4) Recent worsening HF or other cardiovascular events or procedures |
| (5) Severe (GFR < 30 mL/min/1.73m² by CKD-EPI equation), unstable, or rapidly progressing renal disease at the time of randomization |
| (6) Other conditions likely to prevent patient participation in the trial or greatly limit life expectancy |
| Year of Publication | Country/Region | Study Population | Age, Years (SD) | Women,% | Age Group Prevalence, By Years | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | 45–54 | 55–64 | 65–74 | ≥75 | ||||||||
| Farré et al. [14] | 2017 | Catalonia | 88,195 | 77 (12) | 55.0% | 2.70% | 0.30% | 0.90% | 2.50% | 8.80% | ||
| Anguita et al. [15] | 2008 | Spain | 1776 | 64 (12) | 55.9% | 6.80% | 1.30% | 5.50% | 8.00% | 16.1% | ||
| 40–49 | 50–59 | 60–69 | 70–79 | ≥80 | ||||||||
| Cortina et al. [16] | 2001 | Asturias | 391 | 60 (13) | 53.6% | 5.00% | <1.00% | 2.00% | 5.00% | 13.0% | 18.0% | |
| 0–49 | 50–59 | 60–69 | 70–79 | 80–89 | ≥90 | |||||||
| Ohlmeier et al. [17] | 2015 | Germany | 6,284,194 | 39 (21) | 48.2% | 1.70% | 0.10% | 1.28% | 3.88% | 10.8% | 25.9% | 45.7% |
| 19–54 | 55–64 | 65–74 | 75–84 | 85–99 | ||||||||
| Parén et al. [18] | 2014 | Sweden | 144,925 | - | 48.9% | 1.99% | 0.13% | 1.06% | 3.20% | 9.23% | 20.4% | |
| 45–64 | 65–74 | ≥75 | ||||||||||
| Murphy et al. [31] | 2004 | Scotland | 307,741 | - | 50.6% | 0.71% | 0.38% | 2.30% | 6.53% | |||
| 55–64 | 65–74 | 75–84 | ≥85 | |||||||||
| Bleumink et al. [32] | 2004 | Rotterdam | 7983 | 70 (10) | 61.0% | 6.70% | - | 0.90% | 4.00% | 9.70% | 17.4% | |
| 25–49 | 50–59 | 60–69 | 70–79 | ≥80 | ||||||||
| Ceia et al. [33] | 2002 | Portugal | 5434 | 68 (15) | 62.7% | 4.36% | 1.36% | 2.93% | 7.63% | 12.7% | 16.1% | |
| Study | Year of Publication | Study Population | Age, Years (SD) | Women, % | Type of Heart Failure | Geographical Area | Specialty | Reduced EF | NYHA Class II–IV |
|---|---|---|---|---|---|---|---|---|---|
| RICA [27] | 2017 | 1396 | 79 (8) | 54.0% | chronic | Spain | Internal medicine | 39.5% | 80.2% |
| REDINSCOR [27] | 2017 | 2150 | 70 (10) | 31.0% | chronic | Spain | Cardiology | 79.6% | 100% ¹ |
| BADAPIC [6] | 2010 | 4720 | 65 (12) | 29.0% | chronic | Spain | Cardiology | 63.4% | 100% ¹ |
| INCA [7] | 2009 | 2161 | 71 (11) | 44.4% | chronic | Spain | Primary care and cardiology | 38.3% | 84.0% |
| EPISERVE [28] | 2008 | 2249 | 72 (10) | 45.0% | - | Spain, except La Rioja | Primary care, cardiology, and internal medicine | 55.0% | 90.4% |
| GALICAP [29] | 2007 | 1195 | 76 (10) | 52.1% | - | Galicia | Primary care | 38.6% | 81.5% |
| Mean | 52.4% | 84.0% | |||||||
| General Population (by Age Group) | Heart Failure Prevalence (by Age Group) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | 45–54 | 55–64 | 65–74 | Total | 45–54 | 55–64 | 65–74 | 75+ | ||
| Autonomous Communities | 0.30% | 0.90% | 2.50% | 8.80% | ||||||
| Andalucía | 3,895,025 | 1,341,487 | 1,093,149 | 770,187 | 690,202 | 93,855 | 4024 | 9838 | 19,255 | 60,738 |
| Aragón | 674,882 | 207,355 | 180,224 | 136,185 | 151,118 | 18,947 | 622 | 1622 | 3405 | 13,298 |
| Principado de Asturias | 589,263 | 164,027 | 161,384 | 131,949 | 131,903 | 16,851 | 492 | 1452 | 3299 | 11,607 |
| Illes Balears | 529,589 | 194,110 | 145,007 | 103,545 | 86,927 | 12,126 | 582 | 1305 | 2589 | 7650 |
| Canarias | 1,048,012 | 390,823 | 293,621 | 199,438 | 164,130 | 23,244 | 1172 | 2643 | 4986 | 14,443 |
| Cantabria | 307,255 | 93,358 | 85,403 | 65,351 | 63,143 | 8239 | 280 | 769 | 1634 | 5557 |
| Castilla y León | 1,347,618 | 376,632 | 361,698 | 275,863 | 333,425 | 40,623 | 1130 | 3255 | 6897 | 29,341 |
| Castilla-La Mancha | 974,147 | 320,338 | 265,833 | 180,457 | 207,519 | 26,127 | 961 | 2392 | 4511 | 18,262 |
| Catalunya | 3,593,591 | 1,188,206 | 946,935 | 738,057 | 720,393 | 93,933 | 3565 | 8522 | 18,451 | 63,395 |
| Comunitat Valenciana | 2,437,743 | 799,940 | 658,274 | 508,440 | 471,089 | 62,491 | 2400 | 5924 | 12,711 | 41,456 |
| Extremadura | 537,686 | 166,131 | 151,011 | 104,505 | 116,039 | 14,682 | 498 | 1359 | 2613 | 10,211 |
| Galicia | 1,484,698 | 424,418 | 377,370 | 322,257 | 360,653 | 44,463 | 1273 | 3396 | 8056 | 31,737 |
| Comunidad de Madrid | 3,099,482 | 1,074,013 | 826,152 | 609,975 | 589,342 | 77,769 | 3222 | 7435 | 15,249 | 51,862 |
| Región de Murcia | 648,115 | 234,820 | 176,760 | 123,046 | 113,489 | 15,358 | 704 | 1591 | 3076 | 9987 |
| Comunidad Foral de Navarra | 317,203 | 102,519 | 84,911 | 64,649 | 65,124 | 8419 | 308 | 764 | 1616 | 5731 |
| País Vasco | 1,156,253 | 347,445 | 312,977 | 247,706 | 248,125 | 31,887 | 1042 | 2817 | 6193 | 21,835 |
| La Rioja | 158,846 | 49,143 | 43,080 | 32,058 | 34,565 | 4378 | 147 | 388 | 801 | 3042 |
| Ciudad Autónoma de Ceuta | 32,632 | 12,059 | 10,246 | 5676 | 4651 | 680 | 36 | 92 | 142 | 409 |
| Ciudad Autónoma de Melilla | 30,008 | 11,057 | 9737 | 5077 | 4137 | 612 | 33 | 88 | 127 | 364 |
| All Communities | 22,862,048 | 7,497,881 | 6,183,772 | 4,624,421 | 4,555,974 | 594,684 | 22,494 | 55,654 | 115,611 | 400,926 |
| 95% CI | 22,852,679–22,871,420 | 7,492,516–7,503,249 | 6,178,900–6,188,647 | 4,620,208–4,628,637 | 4,551,792–4,560,158 | 593,175–596,196 | 22,202–22,789 | 55,194–56,117 | 114,947–116,278 | 399,687–402,168 |
| Heart Failure + Ejection Fraction ≤ 40% (by Age Group) | Heart Failure + Ejection Fraction ≤ 40% + NYHA Class II–IV (by Age Group) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | 45–54 | 55–64 | 65–74 | 75+ | Total | 45–54 | 55–64 | 65–74 | 75+ | |
| Autonomous Communities | 52.4% | 52.4% | 52.4% | 52.4% | 84.0% | 84.0% | 84.0% | 84.0% | ||
| Andalucía | 49,180 | 2109 | 5155 | 10,089 | 31,827 | 41,311 | 1771 | 4330 | 8475 | 26,734 |
| Aragón | 9928 | 326 | 850 | 1784 | 6968 | 8340 | 274 | 714 | 1499 | 5853 |
| Principado de Asturias | 8830 | 258 | 761 | 1729 | 6082 | 7417 | 217 | 639 | 1452 | 5109 |
| Illes Balears | 6354 | 305 | 684 | 1356 | 4008 | 5337 | 256 | 574 | 1139 | 3367 |
| Canarias | 12,180 | 614 | 1385 | 2613 | 7568 | 10,231 | 516 | 1163 | 2195 | 6357 |
| Cantabria | 4317 | 147 | 403 | 856 | 2912 | 3627 | 123 | 338 | 719 | 2446 |
| Castilla y León | 21,287 | 592 | 1706 | 3614 | 15,375 | 17,881 | 497 | 1433 | 3036 | 12,915 |
| Castilla-La Mancha | 13,690 | 504 | 1254 | 2364 | 9569 | 11,500 | 423 | 1053 | 1986 | 8038 |
| Catalunya | 49,221 | 1868 | 4466 | 9669 | 33,219 | 41,346 | 1569 | 3751 | 8122 | 27,904 |
| Comunitat Valenciana | 32,745 | 1258 | 3104 | 6661 | 21,723 | 27,506 | 1056 | 2608 | 5595 | 18,247 |
| Extremadura | 7693 | 261 | 712 | 1369 | 5351 | 6462 | 219 | 598 | 1150 | 4495 |
| Galicia | 23,299 | 667 | 1780 | 4222 | 16,630 | 19,571 | 560 | 1495 | 3546 | 13,970 |
| Comunidad de Madrid | 40,751 | 1688 | 3896 | 7991 | 27,176 | 34,231 | 1418 | 3273 | 6712 | 22,828 |
| Región de Murcia | 8048 | 369 | 834 | 1612 | 5233 | 6760 | 310 | 700 | 1354 | 4396 |
| Comunidad Foral de Navarra | 4411 | 161 | 400 | 847 | 3003 | 3706 | 135 | 336 | 711 | 2523 |
| País Vasco | 16,709 | 546 | 1476 | 3245 | 11,442 | 14,035 | 459 | 1240 | 2726 | 9611 |
| La Rioja | 2294 | 77 | 203 | 420 | 1594 | 1927 | 65 | 171 | 353 | 1339 |
| Ciudad Autónoma de Ceuta | 356 | 19 | 48 | 74 | 214 | 299 | 16 | 41 | 62 | 180 |
| Ciudad Autónoma de Melilla | 321 | 17 | 46 | 67 | 191 | 269 | 15 | 39 | 56 | 160 |
| All Communities | 311,614 | 11,787 | 29,163 | 60,580 | 210,085 | 261,756 | 9901 | 24,497 | 50,887 | 176,471 |
| 95% CI | 310,522–312,709 | 11,576–12,001 | 28,830–29,499 | 60,100– 61,063 | 209,189–210,984 | 260,755–262,760 | 9708–10,097 | 24,192–24,805 | 50,447–51,330 | 175,650–177,295 |
| HF + EF ≤ 40% + NYHA Class II–IV + GFR ≥ 30 (by Age Group) | |||||
|---|---|---|---|---|---|
| Total | 45–54 | 55–64 | 65–74 | 75+ | |
| Autonomous Communities | 93.9% | 93.9% | 93.9% | 93.9% | |
| Andalucía | 38,791 | 1663 | 4066 | 7958 | 25,104 |
| Aragón | 7831 | 257 | 670 | 1407 | 5496 |
| Principado de Asturias | 6965 | 203 | 600 | 1363 | 4797 |
| Illes Balears | 5012 | 241 | 539 | 1070 | 3162 |
| Canarias | 9607 | 485 | 1092 | 2061 | 5970 |
| Cantabria | 3405 | 116 | 318 | 675 | 2297 |
| Castilla y León | 16,790 | 467 | 1345 | 2850 | 12,127 |
| Castilla-La Mancha | 10,798 | 397 | 989 | 1865 | 7548 |
| Catalunya | 38,823 | 1473 | 3522 | 7626 | 26,202 |
| Comunitat Valenciana | 25,828 | 992 | 2449 | 5254 | 17,134 |
| Extremadura | 6068 | 206 | 562 | 1080 | 4220 |
| Galicia | 18,377 | 526 | 1404 | 3330 | 13,117 |
| Comunidad de Madrid | 32,143 | 1332 | 3073 | 6303 | 21,435 |
| Región de Murcia | 6348 | 291 | 658 | 1271 | 4128 |
| Comunidad Foral de Navarra | 3480 | 127 | 316 | 668 | 2369 |
| País Vasco | 13,179 | 431 | 1164 | 2559 | 9025 |
| La Rioja | 1810 | 61 | 160 | 331 | 1257 |
| Ciudad Autónoma de Ceuta | 281 | 15 | 38 | 59 | 169 |
| Ciudad Autónoma de Melilla | 253 | 14 | 36 | 52 | 150 |
| All Communities | 245,789 | 9297 | 23,002 | 47,783 | 165,707 |
| 95% CI | 244,819–246,762 | 9,110–9,487 | 22,707–23,300 | 47,357–48,212 | 164,911–166,506 |
| HF + EF ≤ 40% + NYHA Class II–IV + GFR ≥ 30 + Diabetes (by Age Group) | HF + EF ≤ 40% + NYHA Class II–IV + GFR ≥ 30 (No Diabetes) (by Age Group) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | 45–54 | 55–64 | 65–74 | 75+ | Total | 45–54 | 55–64 | 65–74 | 75+ | |
| Autonomous Communities | 28.7% | 40.7% | 49.2% | 48.2% | 71.3% | 59.3% | 50.8% | 51.8% | ||
| Andalucía | 18,157 | 478 | 1654 | 3914 | 12,111 | 20,634 | 1185 | 2412 | 4044 | 12,993 |
| Aragón | 3690 | 74 | 273 | 692 | 2652 | 4141 | 183 | 398 | 715 | 2845 |
| Principado de Asturias | 3288 | 58 | 244 | 671 | 2314 | 3677 | 145 | 356 | 693 | 2483 |
| Illes Balears | 2340 | 69 | 219 | 526 | 1525 | 2672 | 172 | 320 | 544 | 1636 |
| Canarias | 4477 | 139 | 444 | 1014 | 2880 | 5130 | 345 | 648 | 1047 | 3090 |
| Cantabria | 1603 | 33 | 129 | 332 | 1108 | 1803 | 82 | 188 | 343 | 1189 |
| Castilla y León | 7934 | 134 | 547 | 1402 | 5851 | 8856 | 333 | 798 | 1448 | 6277 |
| Castilla-La Mancha | 5075 | 114 | 402 | 917 | 3641 | 5724 | 283 | 587 | 947 | 3906 |
| Catalunya | 18,248 | 423 | 1433 | 3751 | 12,641 | 20,576 | 1050 | 2090 | 3875 | 13,561 |
| Comunitat Valenciana | 12,131 | 285 | 996 | 2584 | 8266 | 13,697 | 707 | 1453 | 2670 | 8868 |
| Extremadura | 2855 | 59 | 228 | 531 | 2036 | 3213 | 147 | 333 | 549 | 2184 |
| Galicia | 8688 | 151 | 571 | 1638 | 6328 | 9689 | 375 | 833 | 1692 | 6789 |
| Comunidad de Madrid | 15,074 | 383 | 1250 | 3100 | 10,341 | 17,069 | 949 | 1823 | 3203 | 11,094 |
| Región de Murcia | 2968 | 84 | 267 | 625 | 1991 | 3380 | 207 | 390 | 646 | 2136 |
| Comunidad Foral de Navarra | 1636 | 37 | 128 | 329 | 1143 | 1843 | 91 | 187 | 339 | 1226 |
| País Vasco | 6210 | 124 | 473 | 1259 | 4,354 | 6969 | 307 | 691 | 1301 | 4671 |
| La Rioja | 852 | 18 | 65 | 163 | 607 | 957 | 43 | 95 | 168 | 651 |
| Ciudad Autónoma de Ceuta | 130 | 4 | 16 | 29 | 82 | 151 | 11 | 23 | 30 | 88 |
| Ciudad Autónoma de Melilla | 117 | 4 | 15 | 26 | 73 | 136 | 10 | 21 | 27 | 78 |
| All Communities | 115,473 | 2672 | 9355 | 23,503 | 79,943 | 130,316 | 6625 | 13,647 | 24,280 | 85,764 |
| 95% CI | 114,809–116,140 | 2573–2774 | 9167–9546 | 23,205–23,804 | 79,391–80,498 | 129,610–131,025 | 6467–6786 | 13,420–13,877 | 23,977–24,586 | 85,192–86,339 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Camps-Vilaró, A.; Delgado-Jiménez, J.F.; Farré, N.; Tizón-Marcos, H.; Álvarez-García, J.; Cinca, J.; Dégano, I.R.; Marrugat, J. Estimated Population Prevalence of Heart Failure with Reduced Ejection Fraction in Spain, According to DAPA-HF Study Criteria. J. Clin. Med. 2020, 9, 2089. https://doi.org/10.3390/jcm9072089
Camps-Vilaró A, Delgado-Jiménez JF, Farré N, Tizón-Marcos H, Álvarez-García J, Cinca J, Dégano IR, Marrugat J. Estimated Population Prevalence of Heart Failure with Reduced Ejection Fraction in Spain, According to DAPA-HF Study Criteria. Journal of Clinical Medicine. 2020; 9(7):2089. https://doi.org/10.3390/jcm9072089
Chicago/Turabian StyleCamps-Vilaró, Anna, Juan F. Delgado-Jiménez, Núria Farré, Helena Tizón-Marcos, Jesús Álvarez-García, Juan Cinca, Irene R. Dégano, and Jaume Marrugat. 2020. "Estimated Population Prevalence of Heart Failure with Reduced Ejection Fraction in Spain, According to DAPA-HF Study Criteria" Journal of Clinical Medicine 9, no. 7: 2089. https://doi.org/10.3390/jcm9072089
APA StyleCamps-Vilaró, A., Delgado-Jiménez, J. F., Farré, N., Tizón-Marcos, H., Álvarez-García, J., Cinca, J., Dégano, I. R., & Marrugat, J. (2020). Estimated Population Prevalence of Heart Failure with Reduced Ejection Fraction in Spain, According to DAPA-HF Study Criteria. Journal of Clinical Medicine, 9(7), 2089. https://doi.org/10.3390/jcm9072089






