Vasopressors and Inotropes in Acute Myocardial Infarction Related Cardiogenic Shock: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Experimental Section
2.1. Selection Criteria
2.2. Search Strategy
2.3. Data Extraction and Quality Assessment
2.4. Data Analysis
3. Results
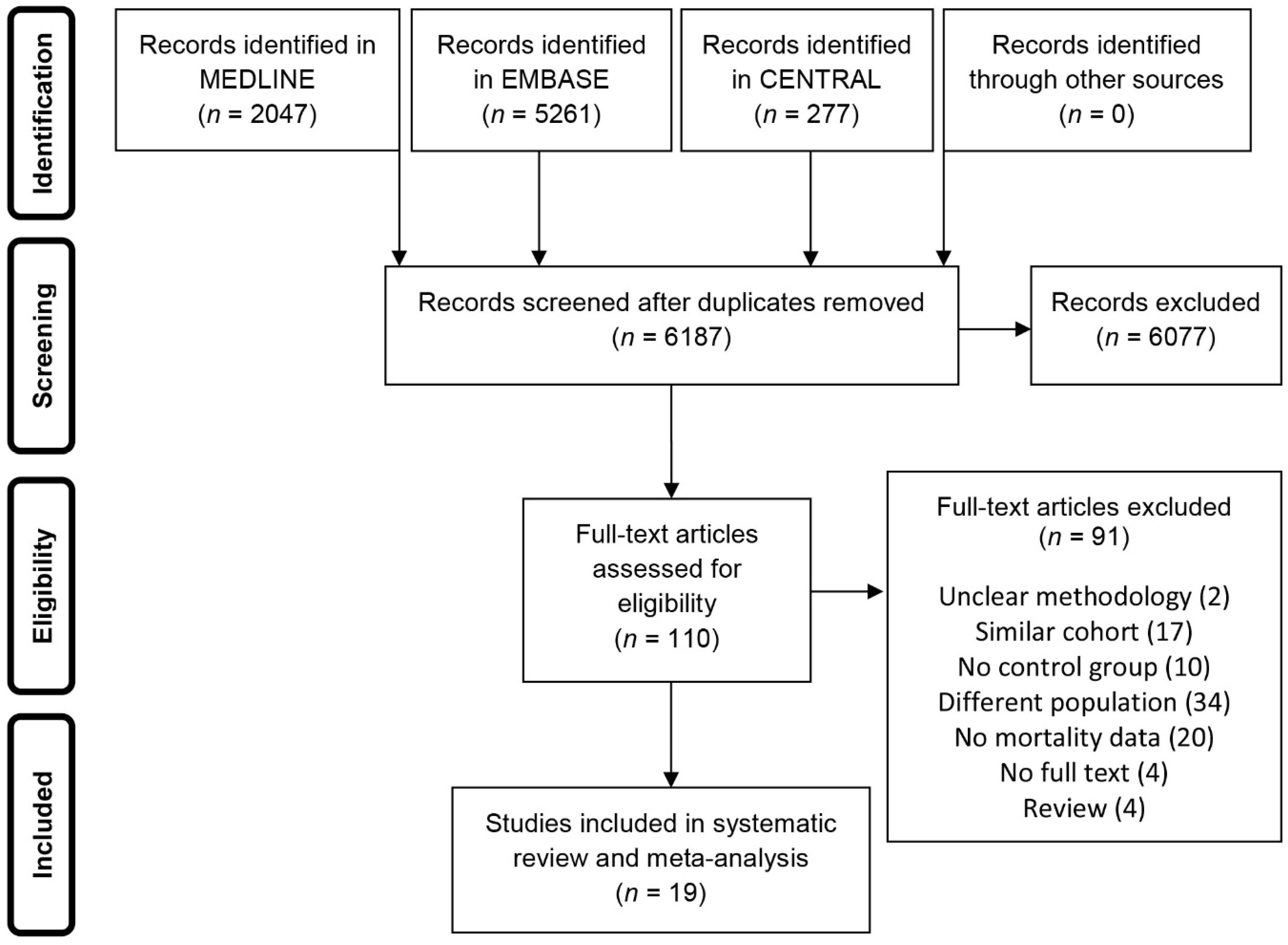
3.1. Search Results
3.2. Study Characteristics
3.3. Participants
3.4. Intervention
3.5. Comparison
3.6. Quality of Studies
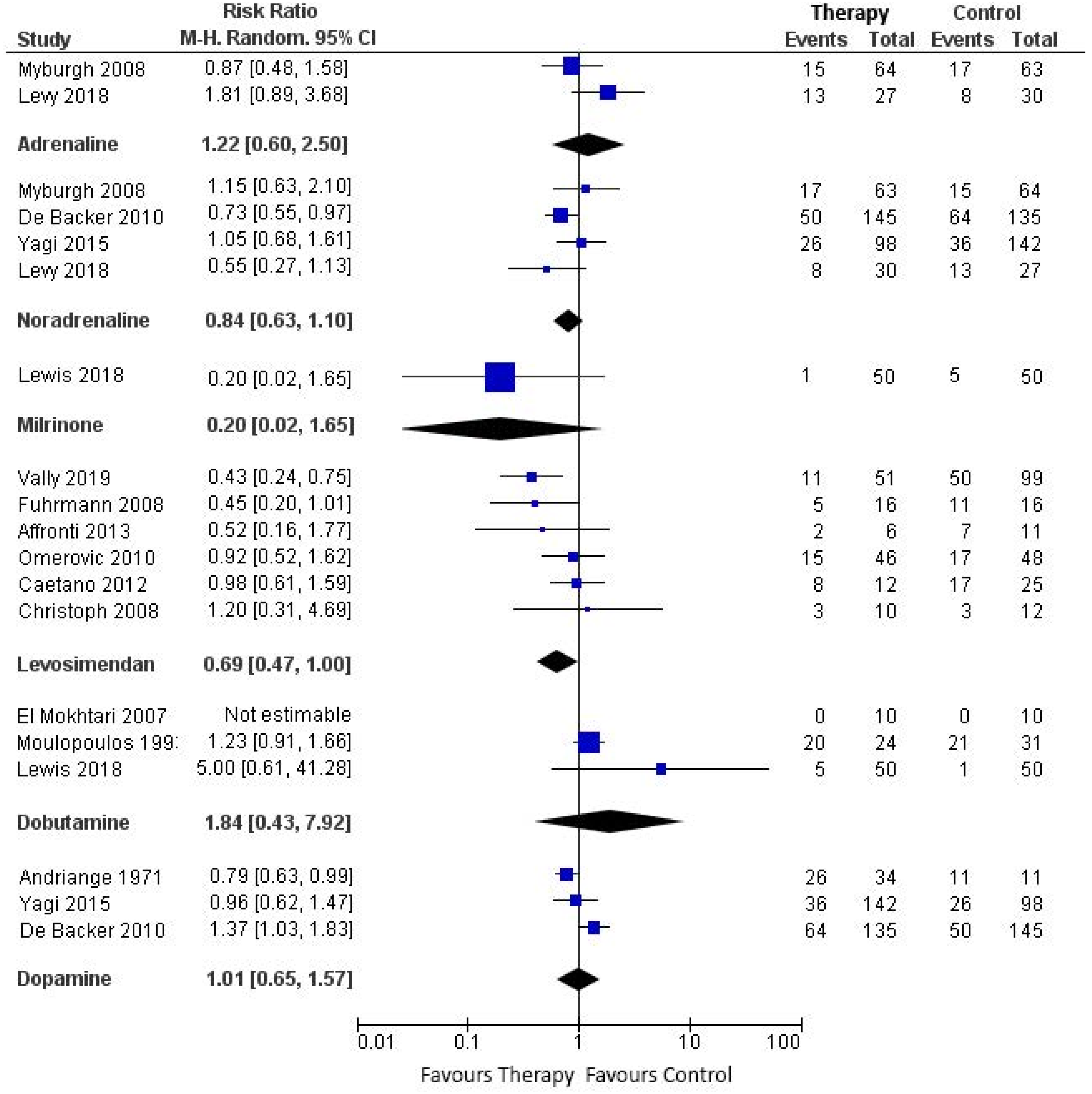
3.7. Mortality Outcomes
3.7.1. Adrenaline vs. Constructed Control
3.7.2. Noradrenaline vs. Constructed Control
3.7.3. Vasopressin vs. Constructed Control
3.7.4. Milrinone vs. Constructed Control
3.7.5. Levosimendan vs. Constructed Control
3.7.6. Dobutamine vs. Constructed Control
3.7.7. Dopamine vs. Constructed Control
3.8. Secondary Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Appendix A. Search strategies
| # | Searches | Results |
| 1 | shock, cardiogenic/ | 7757 |
| 2 | (cardiogen* adj9 shock*).tw,ot,kw,kf. | 10393 |
| 3 | (circulator* adj3 shock*).tw,ot,kf. | 1251 |
| 4 | coron* shock*.tw,ot,kw,kf. | 20 |
| 5 | acute circulatory fail*.tw,ot,kw. | 247 |
| 6 | *shock/dt not (septic or sepsis or bacter*em* or infect* or endotoxin* or heat shock or HSP* or anaphyl* or allergic or vasodilat* or osmotic or h?emorr* or bleeding or toxic or neurogen* or burn* or shock-wave or shock-resistant or hypovolemic or electroconvuls* or distributive shock*).ti. | 711 |
| 7 | ((undifferent* or undiagnos* or different or various or variety or type or types or kind or kinds or forms or states or etiologies) adj2 (shock* not heat shock*)).tw. | 1662 |
| 8 | or/1-7 [I = cardiogenic shock ] | 16778 |
| 9 | myocardial ischemia/ or acute coronary syndrome/ or exp myocardial infarction/ or percutaneous coronary intervention/ or angioplasty, balloon, coronary/ or myocardial revascularization/ or coronary artery bypass/ | 275348 |
| 10 | (((myocard* or heart or card* or ST) adj3 (infarct* or isch?em*)) or (coronary intervent* or STEMI or PCI or angioplast* or post-isch* or postisch* or postinfarct* or post-infarct* or MI or AMI or myocard* revasc* or coronary artery bypass* or CABG or aortocoronary bypass* or coronary bypass*)).tw,ot,kf. | 379295 |
| 11 | 9 or 10 [MI] | 454472 |
| 12 | (shock/ or shock.ti,kw.) not (electric countershock/ or (septic or sepsis or bacter*em* or infect* or endotoxin* or heat shock or HSP* or anaphyl* or allergic or vasodilat* or osmotic or h?emorr* or bleeding or toxic or neurogen* or burn* or shock-wave or shock-resistant or hypovolemic or electroconvuls* or distributive shock*).ti.) [shock general] | 30283 |
| 13 | cardiac output, low/ | 5447 |
| 14 | ((low* or diminish* or decreas* or declin* or reduc* or negligibl* or fall*) adj2 (card* or heart) adj output*).tw,kf. | 8066 |
| 15 | ((low* or diminish* or decreas* or declin* or reduc* or negligibl*) adj output*).tw,kf. | 1988 |
| 16 | cardiac output low.tw,kf,ot. | 51 |
| 17 | (LCOS or COS or LCO).tw,ot,kw. | 17758 |
| 18 | ((instab* or unstab*) adj1 h?emodyn*).tw,kf. | 7625 |
| 19 | or/12-18 [shock, low CO] | 69271 |
| 20 | 11 and 19 [ II = MI + CO ] | 8371 |
| 21 | 8 or 20 [ I II ] | 20946 |
| 22 | (animals/ not humans/) or (porcine or piglet or pig or pigs or rat or rats or dogs or dog or canine).ti. or ph?eochrom*.mp. | 4677715 |
| 23 | (review or editorial).pt. not ((case reports or clinical trial or clinical trial phase iii or clinical trial phase iv or comparative study or controlled clinical trial or evaluation studies or letter or meta analysis or randomized controlled trial).pt. or case-control studies/ or exp cohort studies/ or cross-sectional studies/ or (systematic adj3 (literature or review)).tw,ot,kf.) | 2590121 |
| 24 | 22 or 23 | 7115287 |
| 25 | 21 not 24 [ I II - human not review,editorial] | 16394 |
| 26 | cardiotonic agents/tu, ad | 8559 |
| 27 | catecholamines/ad, tu | 948 |
| 28 | (cardiotonic* or inopressor* or inodilator*).tw,ot,kw. | 2445 |
| 29 | (catecholamines or inotropes or vasopressors or ((catecholamine or inotrop* or vasopressor) adj3 (support or solution* or infusion* or dosing or dose* or dosage* or prescri* or "use" or therap* or treat* or cotreat* or administ* or requir* or need* or superior or first-line or "add" or added or addition or adding or receiv* or receipt or regimen* or alone or combin* or plus or compar* or vs or versus or assigned or allocat* or randomi?ed or effectiveness or efficacy or drug* or agent* or substance* or group))).tw,ot,kf. | 48357 |
| 30 | dopamine/ | 67481 |
| 31 | (dopamin* or hydroxytyramin* or Intropin*).tw,ot,kw. | 145939 |
| 32 | dobutamine/ | 6002 |
| 33 | dobutamin*.tw,ot,kw. | 8454 |
| 34 | noradrenaline/ | 84076 |
| 35 | (norepinephrin* or noradrenalin*).tw,ot,kw. | 92575 |
| 36 | adrenaline/ | 54084 |
| 37 | (epinephrin* or adrenalin*).tw,ot,kw. | 56754 |
| 38 | milrinone/ | 1316 |
| 39 | milrinon*.tw,ot,kw. | 1847 |
| 40 | vasopressins/ | 21322 |
| 41 | vasopressin*.tw,ot,kw. | 33741 |
| 42 | simendan/ | 1042 |
| 43 | (simendan or levosimend*).tw,ot,kw. | 1286 |
| 44 | or/26-43 [ inotropes/vasopressors ] | 378001 |
| 45 | 25 and 44 [ cardiogenic shock + inotropes/vasopressors ] | 2050 |
| 46 | remove duplicates from 45 [ cardiogenic shock + inotropes/vasopressors -deduplicated ] | 2047 |
| # | Searches | Results |
| 1 | cardiogenic shock/ | 24059 |
| 2 | (cardiogen* adj9 shock*).tw,ot,kw. | 18652 |
| 3 | (circulator* adj3 shock*).tw,ot,kw. | 1949 |
| 4 | coron* shock*.tw,ot,kw. | 32 |
| 5 | acute circulatory fail*.tw,ot,kw. | 465 |
| 6 | *Shock/dt not (septic or sepsis or bacter*em* or infect* or endotoxin* or heat shock or HSP* or anaphyl* or allergic or vasodilat* or osmotic or h?emorr* or bleeding or toxic or neurogen* or burn* or shock-wave or shock-resistant or hypovolemic or electroconvuls* or distributive shock*).ti. | 1157 |
| 7 | ((undifferent* or undiagnos* or different or various or variety or type or types or kind or kinds or forms or states or etiologies) adj2 (shock* not heat shock*)).tw. | 2735 |
| 8 | or/1-7 [ I ] | 32877 |
| 9 | heart muscle ischemia/ or heart infarction/ or acute heart infarction/ or anterior myocardial infarction/ or heart infarction size/ or exp heart ventricle infarction/ or non st segment elevation myocardial infarction/ or posterior myocardial infarction/ or st segment elevation myocardial infarction/ or exp percutaneous coronary intervention/ or percutaneous transluminal angioplasty/ or coronary artery bypass graft/ or coronary artery bypass surgery/ | 547773 |
| 10 | (((myocard* or heart or card* or ST) adj3 (infarct* or isch?em*)) or (coronary intervent* or STEMI or PCI or angioplast* or post-isch* or postisch* or postinfarct* or post-infarct* or MI or AMI or myocard* revasc* or coronary artery bypass* or CABG or aortocoronary bypass* or coronary bypass*)).tw,ot,kw. | 572593 |
| 11 | 9 or 10 [MI] | 737611 |
| 12 | (*shock/ or shock.ti.) not (exp heart stimulation/ or (septic or sepsis or bacter*em* or infect* or endotoxin* or heat shock or HSP* or anaphyl* or allergic or vasodilat* or osmotic or h?emorr* or bleeding or toxic or neurogen* or burn* or shock-wave or shock-resistant or hypovolemic or electroconvuls* or distributive shock*).ti.) [shock general] | 32315 |
| 13 | forward heart failure/ | 5518 |
| 14 | ((low* or diminish* or decreas* or declin* or reduc* or negligibl* or fall*) adj2 (card* or heart) adj output*).tw,kw. | 12569 |
| 15 | ((low* or diminish* or decreas* or declin* or reduc* or negligibl*) adj output*).tw,kw. | 2964 |
| 16 | cardiac output low.tw,kw,ot. | 105 |
| 17 | (LCOS or COS or LCO).tw,ot,kw. | 20242 |
| 18 | ((instab* or unstab*) adj1 h?emodyn*).tw,kw. | 12677 |
| 19 | or/12-18 [shock, low CO] | 81903 |
| 20 | 11 and 19 [ II = MI + CO ] | 10001 |
| 21 | 8 or 20 [I II] | 38501 |
| 22 | (book or editorial).pt. or book/ or editorial/ or ((("review" or letter).pt. or "review"/ or letter/) not (meta analysis/ or "systematic review"/ or clinical study/ or case control study/ or exp controlled clinical trial/ or controlled study/ or intervention study/ or longitudinal study/ or major clinical study/ or prospective study/ or retrospective study/ or cohort analysis/ or (systematic adj2 (literature or review)).tw,ot,kw.)) | 3896039 |
| 23 | ((animal/ or animal experiment/ or animal model/ or nonhuman/) not human/) or (porcine or piglet or pig or pigs or rat or rats or dogs or dog or canine).ti. or ph?eochrom*.mp. | 6420601 |
| 24 | 22 or 23 | 10059750 |
| 25 | 21 not 24 [I II - humans not editorials, reviews] | 30861 |
| 26 | *inotropic agent/ or inotropic agent/ae, ct, cb, cm, dt | 6390 |
| 27 | *cardiotonic agent/ or cardiotonic agent/ae, ct, cb, cm, dt | 2726 |
| 28 | catecholamine/ae, ct, cb, cm, dt | 1671 |
| 29 | (cardiotonic* or inopressor* or inodilator*).tw,ot,kw. | 3739 |
| 30 | (catecholamines or inotropes or vasopressors or ((catecholamine or inotrop* or vasopressor) adj3 (support or solution* or infusion* or dosing or dose* or dosage* or prescri* or "use" or therap* or treat* or cotreat* or administ* or requir* or need* or superior or first-line or "add" or added or addition or adding or receiv* or receipt or regimen* or alone or combin* or plus or compar* or vs or versus or assigned or allocat* or randomi?ed or effectiveness or efficacy or drug* or agent* or substance* or group))).tw,ot,kw. | 74053 |
| 31 | dopamine/ not (dopamine/ec not dopamine/ae, cb, cm, dt) | 80557 |
| 32 | (dopamin* or hydroxytyramin* or Intropin*).tw,ot,kw. | 189228 |
| 33 | dobutamine/ not (dobutamine/ec not dobutamine/ae, cb, cm, dt) | 23435 |
| 34 | dobutamin*.tw,ot,kw. | 12411 |
| 35 | noradrenalin/ not (noradrenalin/ec not noradrenalin/ae, cb, cm, dt) | 114540 |
| 36 | (norepinephrin* or noradrenalin*).tw,ot,kw. | 120459 |
| 37 | adrenalin/ not (adrenalin/ec not adrenalin/ae, cb, cm, dt) | 111164 |
| 38 | (epinephrin* or adrenalin*).tw,ot,kw. | 83979 |
| 39 | milrinone/ | 7278 |
| 40 | milrinon*.tw,ot,kw. | 2706 |
| 41 | vasopressin/ not (vasopressin/ec not vasopressin/ad, cb, cm, dt) | 29150 |
| 42 | vasopressin*.tw,ot,kw. | 41607 |
| 43 | simendan/ | 106 |
| 44 | (simendan or levosimend*).tw,ot,kw. | 2165 |
| 45 | or/26-44 [drugs] | 549646 |
| 46 | 25 and 45 [total] | 5721 |
| 47 | remove duplicates from 46 [total hits -deduplicated] | 5640 |
| 48 | (embase or elsevier or canadian).cr. | 26116001 |
| 49 | 47 and 48 [ EMBASE records only] | 5261 |
| ID | Search | Hits |
| #1 | (cardiogen* near/9 shock*):ti,ab,kw | 914 |
| #2 | (circulator* near/3 shock*):ti,ab,kw | 36 |
| #3 | (coron* NEXT shock*):ti,ab,kw | 0 |
| #4 | (acute NEXT circulatory NEXT fail*):ti,ab,kw | 14 |
| #5 | ((undifferent* or undiagnos* or different or various or variety or type or types or kind or kinds or forms or states or etiologies) near/2 shock*):ti,ab not (heat NEXT shock*):ti,ab | 82 |
| #6 | #1 or #2 or #3 or #4 or #5 | 1036 |
| #7 | (((myocard* or heart or card* or ST) near/3 (infarct* or isch*em*)) or ((coronary NEXT intervent*) or STEMI or PCI or angioplast* or (post NEXT isch*) or postisch* or postinfarct* or (post NEXT infarct*) or MI or AMI or (myocard* NEXT revasc*) or (coronary NEXT artery NEXT bypass*) or CABG or (aortocoronary NEXT bypass*) or (coronary NEXT bypass*))) | 57969 |
| #8 | shock:ti,kw not (septic or sepsis or bacter*em* or infect* or endotoxin* or (heat NEXT shock) or HSP* or anaphyl* or allergic or vasodilat* or osmotic or h*emorr* or bleeding or toxic or neurogen* or burn* or (shock NEXT wave) or (shock NEXT resistant) or hypovolemic or (hypo NEXT volemic) or electroconvuls* or (distributive NEXT shock*)):ti | 2559 |
| #9 | ((low* or diminish* or decreas* or declin* or reduc* or negligibl* or fall*) near/2 ((card* NEXT output) OR (heart NEXT output))):ti,ab,kw | 1094 |
| #10 | ((low* or diminish* or decreas* or declin* or reduc* or negligibl*) next output*):ti,ab,kw | 138 |
| #11 | (LCOS or COS or LCO):ti,ab,kw | 312 |
| #12 | ((instab* or unstab*) near/1 h*emodyn*):ti,ab,kw | 633 |
| #13 | #8 or #9 or #10 #11 or #12 | 4238 |
| #14 | #7 and #13 | 1078 |
| #15 | #6 or #14 | 1595 |
| #16 | (cardiotonic* or inopressor* or inodilator* or dopamin* or hydroxytyramin* or Intropin* or dobutamin* or norepinephrin* or noradrenalin* or epinephrin* or adrenalin* or milrinon* or vasopressin* or simendan or levosimend*):ti,ab,kw | 22220 |
| #17 | (catecholamines or inotropes or vasopressors or ((catecholamine or inotrop* or vasopressor) near/3 (support or solution* or infusion* or dosing or dose* or dosage* or prescri* or "use" or therap* or treat* or cotreat* or administ* or requir* or need* or superior or (first NEXT line) or "add" or added or addition or adding or receiv* or receipt or regimen* or alone or combin* or plus or compar* or vs or versus or assigned or allocat* or randomi*ed or effectiveness or efficacy or drug* or agent* or substance* or group))):ti,ab,kw | 4646 |
| #18 | #16 or #17 | 24628 |
| #19 | #15 and #18 | 277 |
References
- Vallabhajosyula, S.; Dunlay, S.M.; Prasad, A.; Kashani, K.; Sakhuja, A.; Gersh, B.J.; Jaffe, A.S.; Holmes, D.R., Jr.; Barsness, G.W. Acute noncardiac organ failure in acute myocardial infarction with cardiogenic shock. J. Am. Coll. Cardiol. 2019, 73, 1781–1791. [Google Scholar] [CrossRef] [PubMed]
- Wayangankar, S.A.; Bangalore, S.; McCoy, L.A.; Jneid, H.; Latif, F.; Karrowni, W.; Charitakis, K.; Feldman, D.N.; Dakik, H.A.; Mauri, L.; et al. Temporal trends and outcomes of patients undergoing percutaneous coronary interventions for cardiogenic shock in the setting of acute myocardial infarction: A report from the CathPCI registry. JACC Cardiovasc. Interv. 2016, 9, 341–351. [Google Scholar] [CrossRef]
- Reynolds, H.R.; Hochman, J.S. Cardiogenic shock: Current concepts and improving outcomes. Circulation 2008, 117, 686–697. [Google Scholar] [CrossRef]
- van Diepen, S.; Katz, J.N.; Albert, N.M.; Henry, T.D.; Jacobs, A.K.; Kapur, N.K.; Kilic, A.; Menon, V.; Ohman, E.M.; Sweitzer, N.K.; et al. Contemporary management of cardiogenic shock: A scientific statement from the american heart association. Circulation 2017, 136, e232–e268. [Google Scholar] [CrossRef]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2017, 39, 119–177. [Google Scholar]
- Berg, D.D.; Bohula, E.A.; Van Diepen, S.; Katz, J.N.; Alviar, C.L.; Baird-Zars, V.M.; Barnett, C.F.; Barsness, G.W.; Burke, J.A.; Cremer, P.C.; et al. Epidemiology of Shock in Contemporary Cardiac Intensive Care Units. Circ. Cardiovasc. Qual. Outcomes 2019, 12, e005618. [Google Scholar] [CrossRef]
- Goldberg, R.J.; Samad, N.A.; Yarzebski, J.; Gurwitz, J.; Bigelow, C.; Gore, J.M. Temporal trends in cardiogenic shock complicating acute myocardial infarction. N. Engl. J. Med. 1999, 340, 1162–1168. [Google Scholar] [CrossRef]
- Hochman, J.S.; Sleeper, L.A.; Webb, J.G.; Sanborn, T.A.A.; White, H.D.; Talley, J.D.; Buller, C.E.; Jacobs, A.K.; Slater, J.N.; Col, J.; et al. Early revascularization in acute myocardial infarction complicated by cardiogenic shock. SHOCK Investigators. Should we emergently revascularize occluded coronaries for cardiogenic shock. N. Engl. J. Med. 1999, 341, 625–634. [Google Scholar] [CrossRef]
- Overgaard, C.B.; Dzavik, V. Inotropes and vasopressors: Review of physiology and clinical use in cardiovascular disease. Circulation 2008, 118, 1047–1056. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.; Altman, D.G.; Gotzsche, P.C.; Juni, P.; Moher, D.; Oxman, A.D.; Savovic, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The cochrane collaboration’s tool for assessing risk of bias in randomised trials. BMJ (Clinical Research Ed) 2011, 343, d5928. [Google Scholar] [CrossRef]
- Stang, A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar] [CrossRef] [PubMed]
- Balshem, H.; Helfand, M.; Schünemann, H.J.; Oxman, A.D.; Kunz, R.; Brozek, J.; Vist, G.E.; Falck-Ytter, Y.; Meerpohl, J.; Norris, S.; et al. GRADE guidelines: 3. Rating the quality of evidence. J. Clin. Epidemiol. 2011, 64, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Levy, B.; Clere-Jehl, R.; Legras, A.; Morichau-Beauchant, T.; Leone, M.; Frederique, G.; Quenot, J.P.; Kimmoun, A.; Cariou, A.; Lassus, J.; et al. Epinephrine versus norepinephrine for cardiogenic shock after acute myocardial infarction. J. Am. Coll. Cardiol. 2018, 72, 173–182. [Google Scholar] [CrossRef] [PubMed]
- Myburgh, J.A.; Higgins, A.; Jovanovska, A.; Lipman, J.; Ramakrishnan, N.; Santamaria, J. Investigators CATS: A comparison of epinephrine and norepinephrine in critically ill patients. Intensive Care Med. 2008, 34, 2226–2234. [Google Scholar] [CrossRef]
- De Backer, D.; Biston, P.; Devriendt, J.; Madl, C.; Chochrad, D.; Aldecoa, C.; Brasseur, A.; Defrance, P.; Gottignies, P.; Vincent, J.L.; et al. Comparison of dopamine and norepinephrine in the treatment of shock. N. Engl. J. Med. 2010, 362, 779–789. [Google Scholar] [CrossRef]
- Samimi-Fard, S.; Garcia-Gonzalez, M.J.; Dominguez-Rodriguez, A.; Abreu-Gonzalez, P. Effects of levosimendan versus dobutamine on long-term survival of patients with cardiogenic shock after primary coronary angioplasty. Int. J. Cardiol. 2008, 127, 284–287. [Google Scholar] [CrossRef]
- Husebye, T.; Eritsland, J.; Muller, C.; Sandvik, L.; Arnesen, H.; Seljeflot, I.; Mangschau, A.; Bjornerheim, R.; Andersen, G.O. Levosimendan in acute heart failure following primary percutaneous coronary intervention-treated acute ST-elevation myocardial infarction. Results from the LEAF trial: A randomized, placebo-controlled study. Eur J. Heart Fail. 2013, 15, 565–572. [Google Scholar] [CrossRef]
- Fuhrmann, J.T.; Schmeisser, A. Levosimendan is superior to enoximone in refractory cardiogenic shock complicating acute myocardial infarction. Crit. Care Med. 2009, 37, 2678–2679. [Google Scholar] [CrossRef]
- Tarvasmaki, T.; Lassus, J.; Varpula, M.; Sionis, A.; Sund, R.; Kober, L.; Spinar, J.; Parissis, J.; Banaszewski, M.; Silva Cardoso, J.; et al. Current real-life use of vasopressors and inotropes in cardiogenic shock - adrenaline use is associated with excess organ injury and mortality. Crit. Care (London, England) 2016, 20, 208. [Google Scholar] [CrossRef]
- Cronin, R.F.; Moore, S.; Marpole, D.G. Shock following myocardial infarction: A clinical survey of 140 cases. Can. Med Assoc. J. 1965, 93, 57–63. [Google Scholar] [PubMed]
- Yagi, T.; Tachibana, E.; Ueki, Y.; Sakamoto, K.; Imamura, H.; Miyamoto, T.; Takahashi, H.; Hanada, H.; Yonemoto, N.; Nagao, K.; et al. The effect of vasopressor agents in the treatment of cardiovascular shock. Circulation 2015, 132 (Suppl. 3), A13004. [Google Scholar]
- Lewis, T.C.; Aberle, C.; Altshuler, D.; Piper, G.L.; Papadopoulos, J. Comparative effectiveness and safety between milrinone or dobutamine as initial inotrope therapy in cardiogenic shock. J. Cardiovasc. Pharmacol. Ther. 2018. [Google Scholar] [CrossRef] [PubMed]
- Vally, S.; Ferdynus, C.; Persichini, R.; Bouchet, B.; Braunberger, E.; Lo Pinto, H.; Martinet, O.; Vandroux, D.; Aujoulat, T.; Allyn, J.; et al. Impact of levosimendan on weaning from peripheral venoarterial extracorporeal membrane oxygenation in intensive care unit. Ann. Intensive Care 2019, 9, 24. [Google Scholar] [CrossRef]
- Affronti, A.; di Bella, I.; Carino, D.; Ragni, T. Levosimendan may improve weaning outcomes in venoarterial ECMO patients. ASAIO J. 2013, 59, 554–557. [Google Scholar] [CrossRef]
- Omerovic, E.; Ramunddal, T.; Albertsson, P.; Holmberg, M.; Hallgren, P.; Boren, J.; Grip, L.; Matejka, G. Levosimendan neither improves nor worsens mortality in patients with cardiogenic shock due to ST-elevation myocardial infarction. Vasc. Health Risk Manag. 2010, 6, 657–663. [Google Scholar] [CrossRef]
- Caetano, F.; Almeida, I.; Silva, J.; Botelho, A.; Mota, P.; Leitao Marques, A. Cardiogenic shock in acute myocardial infarction: Still looking for the best inotrope. Eur. Heart J. Acute Cardiovasc. Care 2012, 1, 28–29. [Google Scholar]
- Christoph, A.; Prondzinsky, R.; Russ, M.; Janusch, M.; Schlitt, A.; Lemm, H.; Reith, S.; Werdan, K.; Buerke, M. Early and sustained haemodynamic improvement with levosimendan compared to intraaortic balloon counterpulsation (IABP) in cardiogenic shock complicating acute myocardial infarction. Acute Card. Care 2008, 10, 49–57. [Google Scholar] [CrossRef]
- Katsytadze, I.; Amosova, E.; Prudkyi, I.; Bogomolets, A.K.O. Long term effects of Levosimendan therapy in patients with cardiogenic shock. Resuscitation 2013, 84, S11. [Google Scholar] [CrossRef]
- El Mokhtari, N.E.; Arlt, A.; Meissner, A.; Lins, M. Inotropic therapy for cardiac low output syndrome: Comparison of hemodynamic effects of dopamine/dobutamine versus dopamine/dopexamine. Eur. J. Med Res. 2007, 12, 563–567. [Google Scholar] [CrossRef]
- Moulopoulos, S.D.; Stamateolopoulos, S.F.; Nanas, J.N.; Kontoyannis, D.A.; Nanas, S.N. Effect of protracted dobutamine infusion on survival of patients in cardiogenic shock treated with intraaortic balloon pumping. Chest 1993, 103, 248–252. [Google Scholar] [CrossRef] [PubMed]
- Andriange, M.; Calay, G.; Gach, J.; Lisin, N. Shock states during myocardial infarct: Treatment of cardiogenic shock with dopamine. Acta Clinica Belgica 1971, 26, 249–261. [Google Scholar] [CrossRef] [PubMed]
- Schumann, J.; Henrich, E.C.; Strobl, H.; Prondzinsky, R.; Weiche, S.; Thiele, H.; Werdan, K.; Frantz, S.; Unverzagt, S. Inotropic agents and vasodilator strategies for the treatment of cardiogenic shock or low cardiac output syndrome. Cochrane Database Syst. Rev. 2018. [Google Scholar] [CrossRef] [PubMed]
- Gamper, G.; Havel, C.; Arrich, J.; Losert, H.; Pace, N.L.; Mullner, M.; Herkner, H. Vasopressors for hypotensive shock. Cochrane Database Syst. Rev. 2016. [Google Scholar] [CrossRef]
- Lamontagne, F.; Richards-Belle, A.; Thomas, K.; Harrison, D.A.; Sadique, M.Z.; Grieve, R.D.; Camsooksai, J.; Darnell, R.; Gordon, A.C.; Henry, D.; et al. Effect of reduced exposure to vasopressors on 90-Day mortality in older critically ill patients with Vasodilatory hypotension: A randomized clinical trial. JAMA 2020, 323, 938–949. [Google Scholar] [CrossRef]
- Ong, M.E.H.; Tiah, L.; Leong, B.S.-H.; Tan, E.C.C.; Ong, V.Y.K.; Tan, E.A.T.; Poh, B.Y.; Pek, P.P.; Chen, Y. A randomised, double-blind, multi-centre trial comparing vasopressin and adrenaline in patients with cardiac arrest presenting to or in the Emergency Department. Resuscitation 2012, 83, 953–960. [Google Scholar] [CrossRef]
- Perkins, G.D.; Ji, C.; Deakin, C.D.; Quinn, T.; Nolan, J.P.; Scomparin, C.; Regan, S.; Long, J.; Slowther, A.; Pocock, H.; et al. A randomized trial of epinephrine in out-of-hospital cardiac arrest. N. Engl. J. Med. 2018, 379, 711–721. [Google Scholar] [CrossRef]
- Olasveengen, T.M.; Sunde, K.; Brunborg, C.; Thowsen, J.; Steen, P.A.; Wik, L. Intravenous drug administration during out-of-hospital cardiac arrest: A randomized trial. JAMA 2009, 302, 2222–2229. [Google Scholar] [CrossRef]

| Study | Year | Country | Center | Setting | Inclusion Period | Follow-up | Overall N | CS N |
|---|---|---|---|---|---|---|---|---|
| Cronin | 1965 | Canada | Single | Retrospective cohort | 1952–1961 | 10 years | 140 | 140 |
| Moulopoulos | 1993 | Greece | Single | Retrospective cohort | 1978–1991 | 1 month | 55 | 55 |
| Andriange | 1971 | Belgium | Single | Retrospective cohort | 1967–1970 | 1 year | 450 | 45 |
| Samimi-Fard | 2007 | Spain | Single | Randomized trial | 2003–2004 | 1 year | 22 | 22 |
| El Mokhtari | 2007 | Germany | Single | Retrospective cohort | - | 1 year | 20 | 20 |
| Fuhrmann | 2008 | Germany | Single | Randomized trial | 2003–2005 | 30 days | 32 | 32 |
| Myburgh | 2008 | Australia | Multi | Randomized trial | 2004–2006 | 90 days | 280 | 128 |
| Christoph | 2008 | Germany | Single | Prospective cohort | 2003–2005 | - | 22 | 22 |
| De Backer | 2010 | Belgium | Multi | Randomized trial | 2003–2007 | 1 year | 1679 | 280 |
| Omerovic | 2010 | Sweden | Single | Prospective cohort | 2004–2006 | 1 year | 94 | 94 |
| Caetano | 2012 | Portugal | - | Retrospective cohort (conference paper) | - | 10.6 ± 10.9 months | 37 | 37 |
| Huseby | 2013 | Norway | Single | Randomized trial | 2006–2010 | 6 months | 61 | 9 |
| Affronti | 2013 | Italy | Single | Retrospective case-control | 2011 | - | 17 | 17 |
| Katsytadze | 2013 | Ukraine | - | Retrospective cohort (conference paper) | - | 1 year | 27 | 27 |
| Yagi | 2015 | Japan | Multi | Prospective cohort (conference paper) | 2012–2014 | 30 days | 979 | 240 |
| Tarvasmaki | 2016 | Finland | Multi | Prospective cohort | 2010–2012 | 90 days | 216 | 216 |
| Levy | 2018 | France | Multi | Randomized trial | 2011–2016 | 60 days | 57 | 57 |
| Vally | 2019 | France | Single | Retrospective cohort | 2010–2017 | 30 days | 150 | 150 |
| Lewis | 2018 | USA | Single | Retrospective cohort | 2013–2015 | In-hospital | 100 | 100 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Karami, M.; Hemradj, V.V.; Ouweneel, D.M.; den Uil, C.A.; Limpens, J.; Otterspoor, L.C.; Vlaar, A.P.; Lagrand, W.K.; Henriques, J.P.S. Vasopressors and Inotropes in Acute Myocardial Infarction Related Cardiogenic Shock: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 2051. https://doi.org/10.3390/jcm9072051
Karami M, Hemradj VV, Ouweneel DM, den Uil CA, Limpens J, Otterspoor LC, Vlaar AP, Lagrand WK, Henriques JPS. Vasopressors and Inotropes in Acute Myocardial Infarction Related Cardiogenic Shock: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2020; 9(7):2051. https://doi.org/10.3390/jcm9072051
Chicago/Turabian StyleKarami, Mina, Veemal V. Hemradj, Dagmar M. Ouweneel, Corstiaan A. den Uil, Jacqueline Limpens, Luuk C. Otterspoor, Alexander P. Vlaar, Wim K. Lagrand, and José P. S. Henriques. 2020. "Vasopressors and Inotropes in Acute Myocardial Infarction Related Cardiogenic Shock: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 9, no. 7: 2051. https://doi.org/10.3390/jcm9072051
APA StyleKarami, M., Hemradj, V. V., Ouweneel, D. M., den Uil, C. A., Limpens, J., Otterspoor, L. C., Vlaar, A. P., Lagrand, W. K., & Henriques, J. P. S. (2020). Vasopressors and Inotropes in Acute Myocardial Infarction Related Cardiogenic Shock: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 9(7), 2051. https://doi.org/10.3390/jcm9072051






