Sacubitril/Valsartan Improves Autonomic Function and Cardiopulmonary Parameters in Patients with Heart Failure with Reduced Ejection Fraction
Abstract
:1. Introduction
2. Experimental Section
2.1. Study Population
2.2. Laboratory Measurements
2.3. Doppler Echocardiography
2.4. Cardiopulmonary Exercise Stress Testing
2.5. Statistics
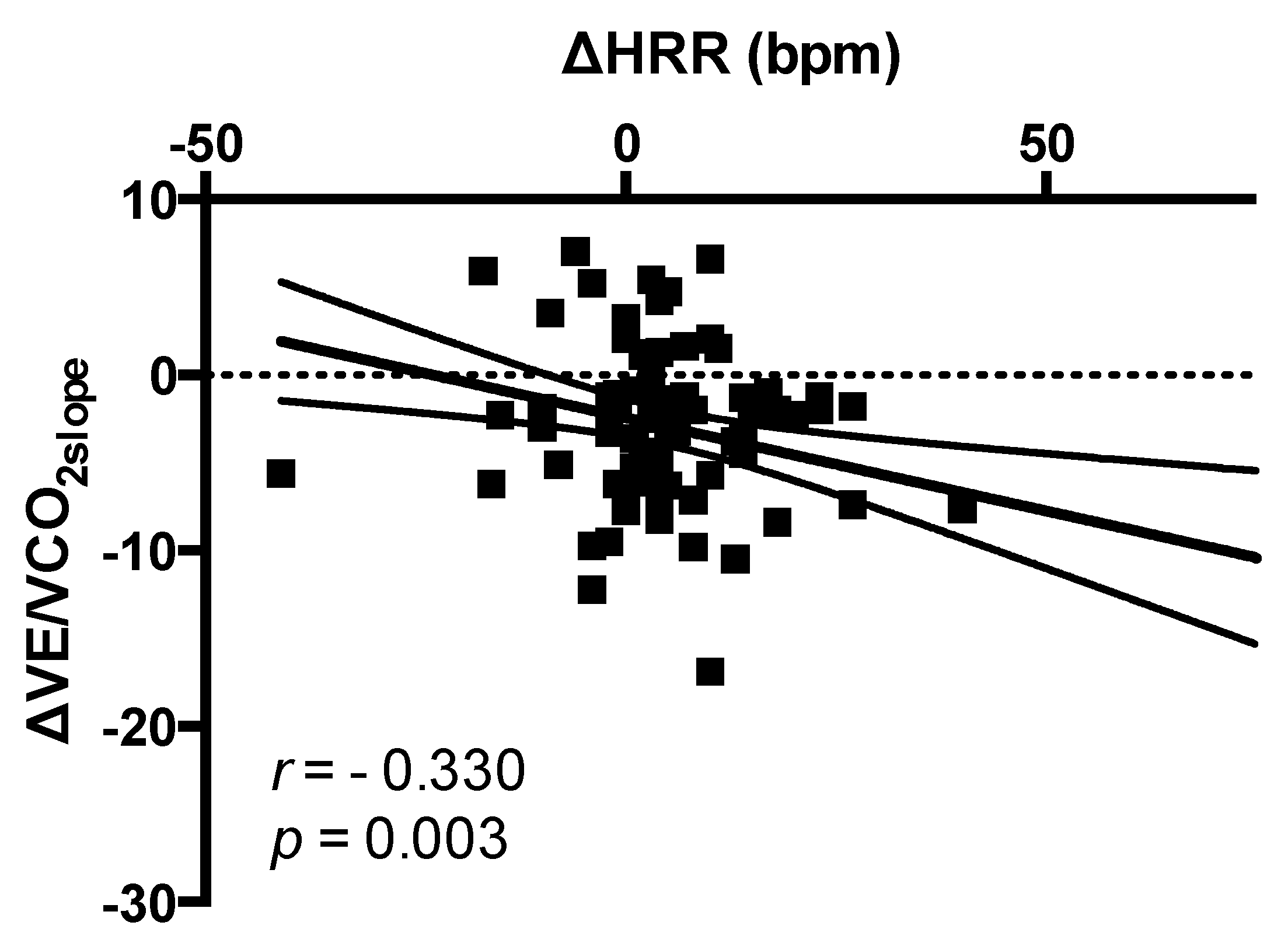
3. Results
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- Peçanha, T.; Silva-Júnior, N.D.; Forjaz, C.L. Heart rate recovery: Autonomic determinants, methods of assessment and association with mortality and cardiovascular diseases. Clin. Physiol. Funct. Imag. 2014, 34, 327–339. [Google Scholar] [CrossRef] [PubMed]
- Peçanha, T.; Bartels, R.; Brito, L.C.; Paula-Ribeiro, M.; Oliveira, R.S.; Goldberger, J.J. Methods of assessment of the post-exercise cardiac autonomic recovery: A methodological review. Int. J. Cardiol. 2017, 227, 795–802. [Google Scholar] [CrossRef] [PubMed]
- Coote, J.H. Recovery of heart rate following intense dynamic exercise. Exp. Physiol. 2010, 95, 431–440. [Google Scholar] [CrossRef] [PubMed]
- Goldberger, J.J.; Johnson, N.P.; Subacius, H.; Ng, J.; Greenland, P. Comparison of the physiologic and prognostic implications of the heart rate versus the RR interval. Heart Rhythm 2014, 11, 1925–1933. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kannankeril, P.J.; Le, F.K.; Kadish, A.H.; Goldberger, J.J. Parasympathetic effects on heart rate recovery after exercise. J. Investig. Med. 2004, 52, 394–401. [Google Scholar] [CrossRef]
- Dewland, T.A.; Androne, A.S.; Lee, F.A.; Lampert, R.J.; Katz, S.D. Effect of acetylcholinesterase inhibition with pyridostig-mine on cardiac parasympathetic function in sedentary adults and trained athletes. Am. J. Physiol. Heart Circ. Physiol. 2007, 293, 86–92. [Google Scholar] [CrossRef] [Green Version]
- Pepper, G.S.; Lee, R.W. Sympathetic activation in heart failure and its treatment with beta-blockade. Arch. Intern. Med. 1999, 159, 225–234. [Google Scholar] [CrossRef]
- Rengo, G.; Galasso, G.; Femminella, G.D.A.; Parisi, V.; Zincarelli, C.; Pagano, G.; De Lucia, C.; Cannavo, A.; Liccardo, D.; Marciano, C.; et al. Reduction of lymphocyte G protein-coupled receptor kinase-2 (GRK2) after exercise training predicts survival in patients with heart failure. Eur. J. Prev. Cardiol. 2014, 21, 4–11. [Google Scholar] [CrossRef]
- Rengo, G.; Parisi, V.; Femminella, G.D.A.; Pagano, G.; de Lucia, C.; Cannavo, A.; Liccardo, D.; Giallauria, F.; Scala, O.; Zincarelli, C.; et al. Molecular aspects of the cardioprotective effect of exercise in the elderly. Aging Clin. Exp. Res. 2013, 25, 487–497. [Google Scholar] [CrossRef] [Green Version]
- McMurray, J.J.; Packer, M.; Desai, A.S.; Gong, J.; Lefkowitz, M.P.; Rizkala, A.R.; Rouleau, J.L.; Shi, V.C.; Solomon, S.D.; Swedberg, K.; et al. Angiotensin-neprilysin inhibition versus enalapril in heart failure. N. Engl. J. Med. 2014, 371, 993–1004. [Google Scholar] [CrossRef] [Green Version]
- Malfatto, G.; Ravaro, S.; Caravita, S.; Baratto, C.; Sorropago, A.; Giglio, A.; Tomaselli, M.; Parati, G.; Villani, A. Improvement of functional capacity in sacubitril-valsartan treated patients assessed by cardiopulmonary exercise test. Acta Cardiol. 2019, 2, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Vitale, G.; Romano, G.; Di Franco, A.; Caccamo, G.; Nugara, C.; Ajello, L.; Storniolo, S.; Sarullo, S.; Agnese, V.; Giallauria, F.; et al. Early Effects of Sacubitril/Valsartan on Exercise Tolerance in Patients with Heart Failure with Reduced Ejection Fraction. J. Clin. Med. 2019, 8, 262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lau, C.W.; Martens, P.; Lambeets, S.; Dupont, M.; Mullens, W. Effects of sacubitril/valsartan on functional status and exercise capacity in real-world patients. Acta Cardiol. 2019, 74, 405–412. [Google Scholar] [CrossRef] [PubMed]
- Sgorbini, L.; Rossetti, A.; Galati, A. Sacubitril/Valsartan: Effect on Walking Test and Physical Capability. Cardiology 2017, 138 (Suppl. 1), 17–20. [Google Scholar] [CrossRef] [Green Version]
- Ambrosetti, M.; Abreu, A.; Corrà, U.; Davos, C.H.; Hansen, D.; Frederix, I.; Iliou, M.C.; Pedretti, R.F.; Schmid, J.P.; Vigorito, C.; et al. Secondary prevention through comprehensive cardiovascular rehabilitation: From knowledge to implementation, 2020 update, A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 2020, 30, 2047487320913379. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; Gonzalez-Juanately, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. ESC Scientific Document Group, 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar]
- Giallauria, F.; Cirillo, P.; Lucci, R.; Pacileo, M.; De Lorenzo, A.; D’Agostino, M.; Moschella, S.; Psaroudaki, M.; Del Forno, D.; Orio, F.; et al. Left ventricular remodelling in patients with moderate systolic dysfunction after myocardial infarction: Favourable effects of exercise training and predictive role of N-terminal pro-brain natriuretic peptide. Eur. J. Cardiovasc. Prev. Rehabil. 2008, 15, 113–118. [Google Scholar] [CrossRef]
- Giallauria, F.; Lucci, R.; De Lorenzo, A.; D’Agostino, M.; Del Forno, D.; Vigorito, C. Favourable effects of exercise training on N-terminal pro-brain natriuretic peptide plasma levels in elderly patients after acute myocardial infarction. Age Ageing 2006, 35, 601–607. [Google Scholar] [CrossRef] [Green Version]
- Lang, R.M.; Bierig, M.; Devereux, R.B.; Flachskampf, F.A.; Foster, E.; Pellikka, P.A.; Picard, M.H.; Roman, M.J.; Seward, J.; Shanewise, J.; et al. Recommendations for chamber quantification. Eur. J. Echocardiogr. 2006, 7, 79–108. [Google Scholar] [CrossRef]
- Tsang, T.S.; Abharayatna, W.P.; Barnes, M.E.; Miyasaka, Y.; Gersh, B.J.; Bailey, K.R.; Cha, S.S.; Seward, J.B. Prediction of cardiovascular outcomes with left atrial size. J. Am. Coll. Cardiol. 2006, 47, 1018–1023. [Google Scholar] [CrossRef] [Green Version]
- Giallauria, F.; Galizia, G.; Lucci, R.; D’Agostino, M.; Vitelli, A.; Maresca, L.; Orio, F.; Vigorito, C. Favourable effects of exercise-based cardiac rehabilitation after acute myocardial infarction on left atrial remodeling. Int. J. Cardiol. 2009, 136, 300–306. [Google Scholar] [CrossRef] [PubMed]
- Quinones, M.A.; Otto, C.M.; Stoddard, M.; Waggoner, A.; Zoghbi, W.A.; Doppler Quantification Task Force of the Nomenclature and Standards Committee of the American Society of Echocardiography. Recommendations for quantification of Doppler echocardiography: A report from the Doppler Quantification Task Force of the Nomenclature and Standards Committee of the American Society of Echocardiography. J. Am. Soc. Echocardiogr. 2002, 15, 167–184. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia, M.J.; Thomas, J.D.; Klein, A.L. New Doppler echocardiographic applications for the study of diastolic function. J. Am. Coll. Cardiol. 1998, 32, 865–875. [Google Scholar] [CrossRef] [Green Version]
- Wassermann, K.; Hansen, J.E.; Sue, D.Y.; Whipp, B.J. Normal values. In Principles of Exercise Testing and Interpretation; Wassermann, K., Hansen, J.E., Sue, D.Y., Whipp, B.J., Eds.; Lea & Febiger: Philadelphia, PA, USA, 2004; Volume 1987, pp. 72–85. [Google Scholar]
- Beaver, W.L.; Wasserman, K.; Whipps, B.J. A new method for detecting anaerobic threshold by gas exchange. J. Appl. Physiol. 1986, 60, 2020–2027. [Google Scholar] [CrossRef]
- Corrà, U.; Giordano, A.; Bosimini, E.; Mezzani, A.; Piepoli, M.; Coats, A.J.; Giannuzzi, P. Oscillatory ventilation during exercise in patients with chronic heart failure: Clinical correlates and prognostic implications. Chest 2002, 121, 1572–1580. [Google Scholar] [CrossRef] [Green Version]
- Giallauria, F.; Lucci, R.; Pietrosante, M.; De Lorenzo, A.; Gargiulo, G.; D’Agostino, M.; Gerundo, G.; Abete, P.; Rengo, F.; Vigorito, C. Exercise-based Cardiac Rehabilitation improves Heart Rate Recovery in Elderly Patients after Acute Myocardial Infarction. J. Gerontol. Ser. A Biol. Sci. Med. Sci. 2006, 61, 713–717. [Google Scholar] [CrossRef] [Green Version]
- Giallauria, F.; De Lorenzo, A.; Pilerci, F.; Manakos, A.; Lucci, R.; Psaroudaki, M.; D’Agostino, M.; Del Forno, D.; Vigorito, C. Long-Term Effects of Cardiac Rehabilitation On End-Exercise Heart Rate Recovery After Myocardial Infarction. Eur. J. Cardiovasc. Prev. Rehabil. 2006, 13, 544–550. [Google Scholar] [CrossRef]
- Pearson, M.J.; Smart, N.A. Exercise therapy and autonomic function in heart failure patients: A systematic review and meta-analysis. Heart Fail. Rev. 2018, 23, 91–108. [Google Scholar] [CrossRef]
- Manresa-Rocamora, A.; Ribeiro, F.; Sarabia, J.M.; Íbias, J.; Oliveira, N.L.; Vera-Garcia, F.J.; Moya-Ramón, M. Exercise-based cardiac rehabilitation and parasympathetic function in patients with coronary artery disease: A systematic review and meta-analysis. Clin. Anton. Res. 2020. [Google Scholar] [CrossRef]
- Tang, Y.D.; Dewland, T.A.; Wencker, D.; Katz, S.D. Post-exercise heart rate recovery independently predicts mortality risk in patients with chronic heart failure. J. Card. Fail. 2009, 15, 850–855. [Google Scholar] [CrossRef] [Green Version]
- Sheppard, R.J.; Racine, N.; Roof, A.; Ducharme, A.; Blanchet, M.; White, M. Heart rate recovery—A potential marker of clinical outcomes in heart failure patients receiving beta-blocker therapy. Can. J. Cardiol. 2007, 23, 1135–1138. [Google Scholar] [CrossRef] [Green Version]
- Cahalin, L.P.; Forman, D.E.; Chase, P.; Guazzi, M.; Myers, J.; Bensimhon, D.; Peberdy, M.A.; Ashley, E.; West, E.; Arena, R. The prognostic significance of heart rate recovery is not dependent upon maximal effort in patients with heart failure. Int. J. Cardiol. 2013, 168, 1496–1501. [Google Scholar] [CrossRef] [PubMed]
- Hajdusek, P.; Kotrc, M.; Kautzner, J.; Melenovsky, V.; Benesova, E.; Jarolim, P.; Benes, J. Heart rate response to exercise in heart failure patients: The prognostic role of metabolic-chronotropic relation and heart rate recovery. Int. J. Cardiol. 2017, 228, 588–593. [Google Scholar] [CrossRef] [PubMed]
- Toska, K.; Eriksen, M. Peripheral vasoconstriction shortly after onset of moderate exercise in human. J. Appl. Physiol. 1994, 77, 1519–1525. [Google Scholar] [CrossRef]
- Walgenbach, S.C.; Donald, D.E. Inhibition by carotid baroreflex of exercise-induced increases in arterial pressure. Circ. Res. 1983, 52, 253–262. [Google Scholar] [CrossRef] [Green Version]
- Imai, K.; Sato, H.; Hori, M.; Kusuoka, H.; Ozaki, H.; Yokoyama, H. Vagally mediated heart rate recovery after exercise is accelerated in athletes but blunted in patients with chronic heart failure. J. Am. Coll. Cardiol. 1994, 24, 1529–1535. [Google Scholar] [CrossRef] [Green Version]
- Giallauria, F.; Cirillo, P.; Lucci, R.; Pacileo, M.; D’Agostino, M.; Maietta, P.; Vitelli, A.; Chiariello, M.; Vigorito, C. Autonomic Dysfunction is associated with High Mobility Group Box-1 Levels in Patients after Acute Myocardial Infarction. Atherosclerosis 2010, 208, 280–284. [Google Scholar] [CrossRef] [Green Version]
- Frangogiannis, N.G.; Smith, C.W.; Entman, M.L. The inflammatory response in myocardial infarction. Cardiovasc. Res. 2002, 53, 31–47. [Google Scholar]
- Cole, C.R.; Blackstone, E.H.; Pashkow, F.J.; Snader, C.E.; Lauer, M.S. Heart-rate recovery immediately after exercise as a predictor of mortality. N. Engl. J. Med. 1999, 341, 1351–1357. [Google Scholar] [CrossRef]
- Nishime, E.O.; Cole, C.R.; Blackstone, E.H.; Pashkow, F.J.; Lauer, M.S. Heart-rate recovery and treadmill exercise score as a predictors of mortality in patients referred for exercise ECG. JAMA 2000, 284, 1392–1398. [Google Scholar] [CrossRef]
- Watanabe, J.; Thamilarasan, M.; Blackstone, E.H.; Thomas, J.D.; Lauer, M.S. Heart rate recovery immediately after treadmill exercise and left ventricular systolic dysfunction as predictors of mortality. Circulation 2001, 104, 1911–1916. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vivekananthan, D.P.; Blackstone, E.H.; Pothier, C.E.; Lauer, M.S. Heart rate recovery after exercise is a predictor of mortality, independent of the angiographic severity of coronary disease. J. Am. Coll. Cardiol. 2003, 42, 831–838. [Google Scholar] [CrossRef]
- von Lueder, T.G.; Wang, B.H.; Kompa, A.R.; Huang, L.; Webb, R.; Jordaan, P.; Atar, D.; Krum, H. Angiotensin receptor neprilysin inhibitor LCZ696 attenuates cardiac remodeling and dysfunction after myocardial infarction by reducing cardiac fibrosis and hypertrophy. Circ. Heart Fail. 2015, 8, 71–78. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Suematsu, Y.; Jing, W.; Nunes, A.; Kashyap, M.L.; Khazaeli, M.; Vaziri, N.D.; Moradi, H. LCZ696 (Sacubitril/Valsartan), an Angiotensin-Receptor Neprilysin Inhibitor, Attenuates Cardiac Hypertrophy, Fibrosis, and Vasculopathy in a Rat Model of Chronic Kidney Disease. J. Card. Fail. 2018, 24, 266–275. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Baseline | 12-Month Follow-Up | ||
|---|---|---|---|
| Age (Years) | 57.9 ± 9.6 | ||
| Gender (Male) (%) | 87 | ||
| BMI (kg/m2) | 28.3 ± 4.5 | 28.2 ± 4.6 | 0.935 |
| NT-proBNP (pg/mL) | 1443.2 ± 1323 | 1041.2 ± 1171.3 | 0.015 |
| eGFR (MDRD) (mL/min/1.73 m2) | 73.1 ± 36.3 | 76.8 ± 38.8 | 0.518 |
| Haemoglobin (g/dL) | 12.8 ± 1.4 | 14.2 ± 2.5 | 0.388 |
| Na+ (mEq/L) | 139.2 ± 2.6 | 140 ± 2.3 | 0.06 |
| K+ (mEq/L) | 4.2 ± 0.5 | 4.3 ± 0.5 | 0.691 |
| SBP (mmHg) | 117.1 ± 16.9 | 102.9 ± 13.4 | <0.0001 |
| DBP (mmHg) | 71.8 ± 9.7 | 64.2 ± 6.9 | <0.0001 |
| HR (bpm) | 68.2 ± 11.5 | 67.1 ± 8.9 | 0.435 |
| NYHA Class I | 5 (4%) | 15 (11.4%) ** | <0.0001 |
| NYHA Class II | 82 (62%) | 104 (77.2%) | |
| NYHA Class III | 46 (34%) | 15 (11.4%) | |
| NYHA Class IV | |||
| Pacemaker (n,%) | 6 (4.5%) | ||
| CRT (n,%) | 23 (17%) | ||
| PMK-ICD (n,%) | 102 (76%) | ||
| Hypertension (n,%) | 72 (54%) | ||
| Diabetes (n,%) | 45 (34%) | ||
| Dyslipidemia (n,%) | 78 (59%) | ||
| Atrial Fibrillation (n,%) | 22 (16%) | ||
| COPD (n,%) | 21 (16%) | ||
| Active Smokers | 58 (44%) | ||
| Drug therapy | |||
| Beta-Blockers (n,%) | 125 (93%) | 125 (93%) | 1.00 |
| ACE-Inhibitors * (n,%) | 81 (60%) | ||
| ARBs * (n,%) | 29 (21%) | ||
| Loop Diuretics (n,%) | 111 (83%) | 103 (77%) | 0.04 |
| Loop Diuretics Dose (mg/day) | 87 ± 105 | 80 ± 97 | 0.586 |
| MRA (n,%) | 110 (82%) | 109 (81%) | 0.533 |
| MRA dose (mg/day) | 26 ± 12 | 24 ± 9 | 0.174 |
| Ivabradine (n,%) | 25 (19%) | 25 (19%) | 1.00 |
| Statin (n,%) | 97 (72%) | 95 (70%) | 1.00 |
| ARNI1 (n,%) | 90 (67.2%) | 39 (29.1%) ** | <0.0001 |
| ARNI2 (n,%) | 40 (31.3%) | 48 (35.8%) | |
| ARNI3 (n,%) | 2 (1.5%) | 47 (35.1%) |
| ARNI1 | ARNI2 | ARNI3 | ||||
|---|---|---|---|---|---|---|
| Baseline (n = 90) | 12-Month Follow-Up (n = 39) | Baseline (n = 40) | 12-Month Follow-Up (n = 48) | Baseline (n = 2) | 12-Month Follow-Up (n = 47) | |
| Age (Years) | 58 ± 9 | 59 ± 9 | 57.8 ± 10.8 | 58.3 ± 11.0 | 55.5 ± 13.4 | 56.7 ± 8.4 |
| BMI (kg/m2) | 27.2 ± 3.9 | 26.9 ± 4.0 | 30.4 ± 5.1 | 28.8 ± 4.7 | 31.4 ± 2.3 | 28.6 ± 4.9 |
| NT-proBNP (pg/mL) | 1450.15 ± 1466.52 | 1343.55 ± 1373.42 | 1390.70 ± 991.90 | 1151.68 ± 1303.11 | 2146 ± 11.49 | 673.3 ± 704.7 * |
| eGFR (MDRD) (mL/min/1.73 m2) | 73.3 ± 39.2 | 69.3 ± 23.7 | 72.5 ± 31.1 | 82.2 ± 55.0 | 77.5 ± 15.9 | 75.6 ± 13.9 |
| Haemoglobin (g/dL) | 13.0 ± 1.6 | 14.2 ± 2.5 | 12.0 ± 1.1 | 12.8 ± 1.4 | 12.3 ± 1.8 | 12.7 ± 1.6 |
| Na+ (mEq/L) | 139.2 ± 2.6 | 139.8 ± 3.2 | 139.5 ± 2.6 | 140.1 ± 1.8 | 136 ± 0.3 | 140.4 ± 2.2 |
| K+ (mEq/L) | 4.2 ± 0.43 | 4.4 ± 0.60 | 4.3 ± 0.54 | 4.2 ± 0.36 | 4.5 ± 0.32 | 4.3 ± 0.53 |
| SBP (mmHg) | 114.9 ± 14.5 | 96.9 ± 11.5 * | 121.8 ± 20.2 | 102.9 ± 12.0 * | 122.5 ± 31.8 | 107.9 ± 14.5 |
| DBP (mmHg) | 71.3 ± 9.6 | 62.4 ± 6.7 * | 72.7 ± 10.2 | 63.9 ± 6.6 * | 77.5 ± 3.5 | 65.9 ± 7.2 * |
| HR (bpm) | 67.8 ± 10.5 | 67.3 ± 7.016 | 68.0 ± 12.5 | 67.4 ± 8.6 | 86.5 ± 26.2 | 66.6 ± 10.9 * |
| Doppler-Echocardiography Parameters | Baseline | 12-Month Follow-Up | p-Value |
|---|---|---|---|
| LVEDD (mm) | 63.1 ± 6.7 | 63.6 ± 6.5 | 0.701 |
| LVEDV (mL) | 216.2 ± 56.3 | 208.7 ± 59.1 | 0.482 |
| LVEDVi (mL/m2) | 112.2 ± 27.9 | 112.9 ± 25.8 | 0.897 |
| LVEF (%) | 28 ± 5.8 | 31.8 ± 7.3 | <0.0001 |
| LAV (mL) | 96.7 ± 35.8 | 86.1 ± 29.3 | 0.098 |
| LAVi (mL/m2) | 49.6 ± 17.9 | 45.6 ± 14.7 | 0.226 |
| E-Wave (cm/s) | 0.92 ± 0.43 | 0.85 ± 0.42 | 0.434 |
| A-Wave (cm/s) | 0.67 ± 0.31 | 0.79 ± 0.31 | 0.094 |
| E/A Ratio | 1.53 ± 1.4 | 1.01 ± 0.74 | 0.02 |
| Deceleration Time (ms) | 175.9 ± 53.8 | 197.2 ± 59.4 | 0.113 |
| E’ (cm/s) | 0.05 ± 0.02 | 0.06 ± 0.02 | 0.047 |
| E/E’ ratio | 15.1 ± 6.8 | 13.4 ± 7.0 | 0.298 |
| TAPSE (mm) | 19.5 ± 4.2 | 19.3 ± 3.9 | 0.398 |
| ARNI1 | ARNI2 | ARNI3 | ||||
|---|---|---|---|---|---|---|
| Baseline (n = 90) | 12-Month Follow-Up (n = 39) | Baseline (n = 40) | 12-Month Follow-Up (n = 48) | Baseline (n = 2) | 12-Month Follow-Up (n = 47) | |
| LVEDD (mm) | 62.8 ± 6.4 | 64.3 ± 6.1 | 63.8 ± 7.7 | 65.1 ± 5.4 | 68.0 ± 2.8 | 61.4 ± 7.6 |
| LVEDV (mL) | 210.9 ± 57.7 | 210.7 ± 53.1 | 224.3 ± 51.5 | 213.6 ± 67.2 | 281.0 ± 41 | 203.3 ± 64.1 |
| LVEDVi (mL/m2) | 112.7 ± 28.4 | 110.9 ± 25.7 | 107.9 ± 26.6 | 115.9 ± 21.4 | 140.5 ± 13.4 | 113.9 ± 29.9 |
| LVEF (%) | 28.4 ± 6.2 | 29.2 ± 7.2 | 27.4 ± 6.4 | 32.1 ± 6.5 * | 28.2 ± 4.9 | 33.8 ± 8.0 |
| LAV (mL) | 92.7 ± 35.0 | 90.8 ± 27.6 | 106.4 ± 38.4 | 86.7 ± 37.1 | 107.0 ± 18.4 | 79.8 ± 27.4 |
| LAVi (mL/m2) | 49.1 ± 19.2 | 48.9 ± 16.3 | 50.9 ± 14.7 | 44.3 ± 14.4 | 53 ± 4.2 | 41.6 ± 12.6 |
| E-Wave (cm/s) | 0.90 ± 0.43 | 0.97 ± 0.46 | 1.01 ± 0.44 | 0.8 ± 0.23 | 0.65 ± 0.03 | 0.72 ± 0.45 |
| A-Wave (cm/s) | 0.64 ± 0.30 | 0.71 ± 0.28 | 0.75 ± 0.33 | 0.85 ± 0.42 | 0.85 ± 0.04 | 0.83 ± 0.22 |
| E/A Ratio | 1.6 ± 1.5 | 1.36 ± 1.44 | 0.89 ± 0.55 | 0.94 ± 0.31 | 0.76 ± 0.035 | 0.87 ± 0.34 |
| Deceleration Time (ms) | 172.5 ± 55.1 | 191.8 ± 55.9 | 193.2 ± 47.1 | 185.0 ± 55.9 | 143.5 ± 61.5 | 212.4 ± 67.9 |
| E’ (cm/s) | 0.05 ± 0.02 | 0.06 ± 0.01 | 0.06 ± 0.01 | 0.06 ± 0.02 | 0.05 ± 0.01 | 0.06 ± 0.02 |
| E/E’ ratio | 15.2 ± 7.5 | 13.2 ± 4.6 | 15.3 ± 4.6 | 13.5 ± 5.7 | 13.3 ± 3.3 | 13.6 ± 10.4 |
| TAPSE (mm) | 19.0 ± 4.1 | 17.6 ± 3.1 | 20.8 ± 4.7 | 19.6 ± 3.3 | 18.5 ± 0.7 | 20.0 ± 3.3 |
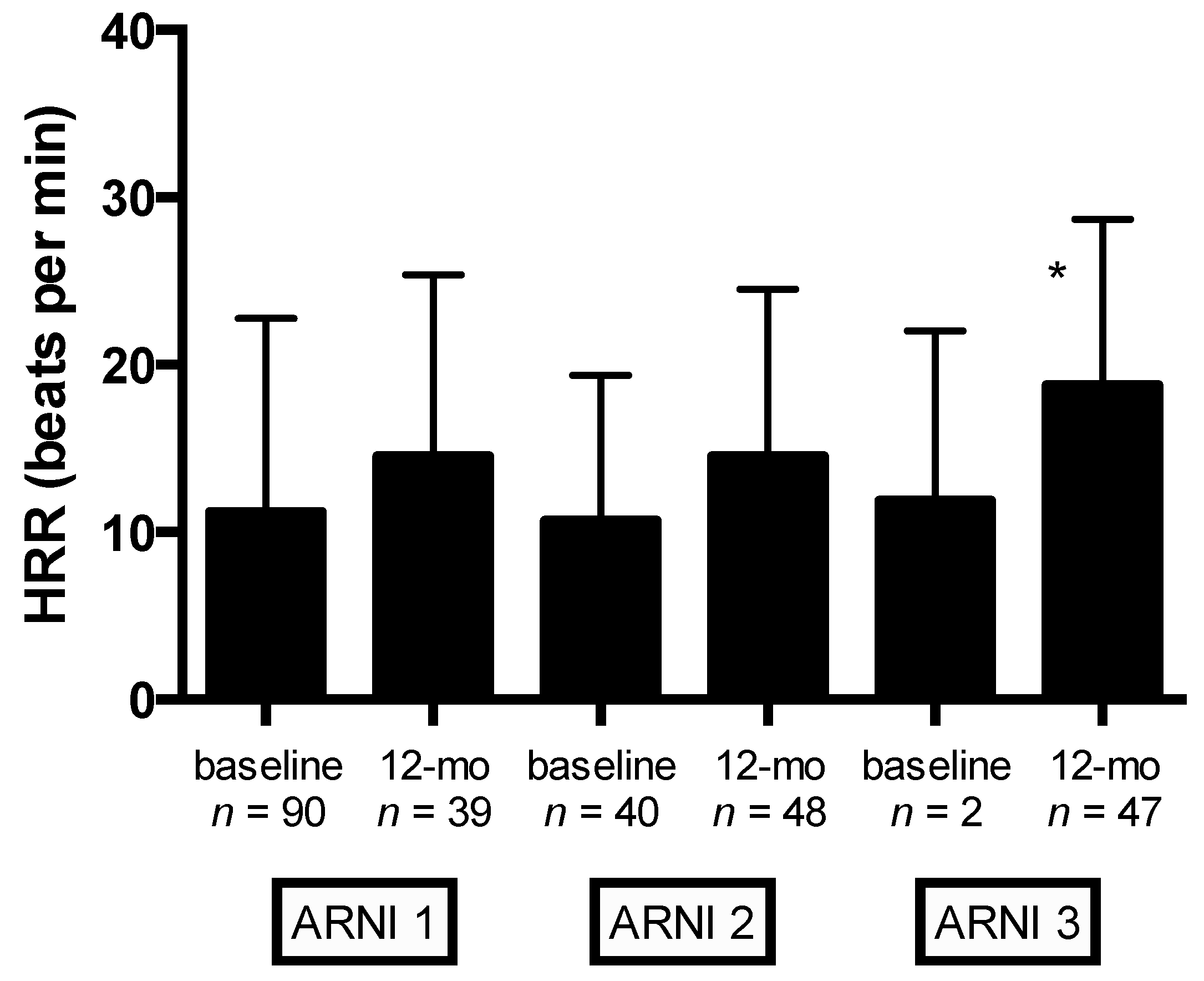
| CPET Parameters | Baseline | 12-Month Follow-Up | p Value |
|---|---|---|---|
| VO2peak (mL/kg/min) | 15.3 ± 3.7 | 17.8 ± 4.2 | <0.0001 |
| Predicted VO2peak (%) | 56.4 ± 13.9 | 64.8 ± 17.8 | <0.0001 |
| Watt Max (W) | 72.8 ± 25.1 | 90.5 ± 28.1 | <0.0001 |
| VE/VCO2slope | 33.4 ± 6.2 | 30.3 ± 6.5 | <0.0001 |
| RER | 1.14 ± 0.12 | 1.14 ± 0.15 | 0.836 |
| HR Rest (bpm) | 72.4 ± 10.8 | 68.9 ± 12.1 | 0.329 |
| HR Peak (bpm) | 106.6 ± 18.2 | 110.9 ± 20.6 | 0.001 |
| HRR (bpm) | 11.4 ± 9.5 | 17.4 ± 15.1 | 0.004 |
| AT-VO2 (mL/kg/min) | 11.4 ± 2.9 | 12.1 ± 3.6 | 0.015 |
| AT-VO2 (%) | 40.9 ± 11.5 | 55.5 ± 84.6 | 0.173 |
| AT-Watt (W) | 56.1 ± 24.8 | 58.5 ± 22.1 | 0.536 |
| O2-Pulse (mL/beat) | 11.4 ± 3 | 13.7 ± 4.6 | <0.0001 |
| ΔVO2/Δwork (mL/min/watt) | 9.2 ± 1.6 | 10.2 ± 1.5 | <0.0001 |
| Peak Ventilation (L/min) | 48.1 ± 12.3 | 61.4 ± 18.9 | <0.0001 |
| TIDAL Volume (mL/kg) | 1.5 ± 0.38 | 2.2 ± 3.7 | 0.114 |
| Respiratory Rate (breaths/min) | 30.8 ± 6.3 | 33.6 ± 7.4 | <0.0001 |
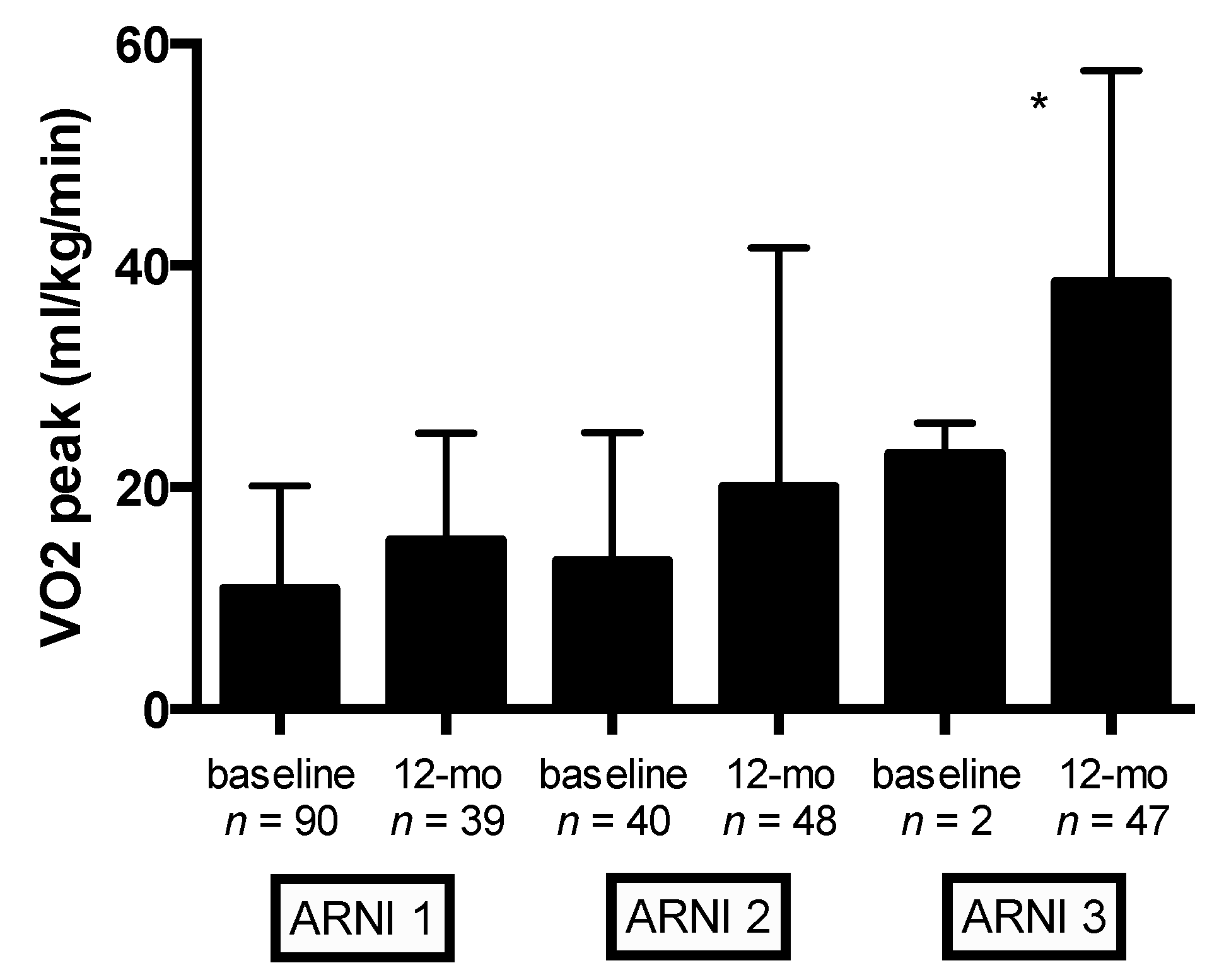
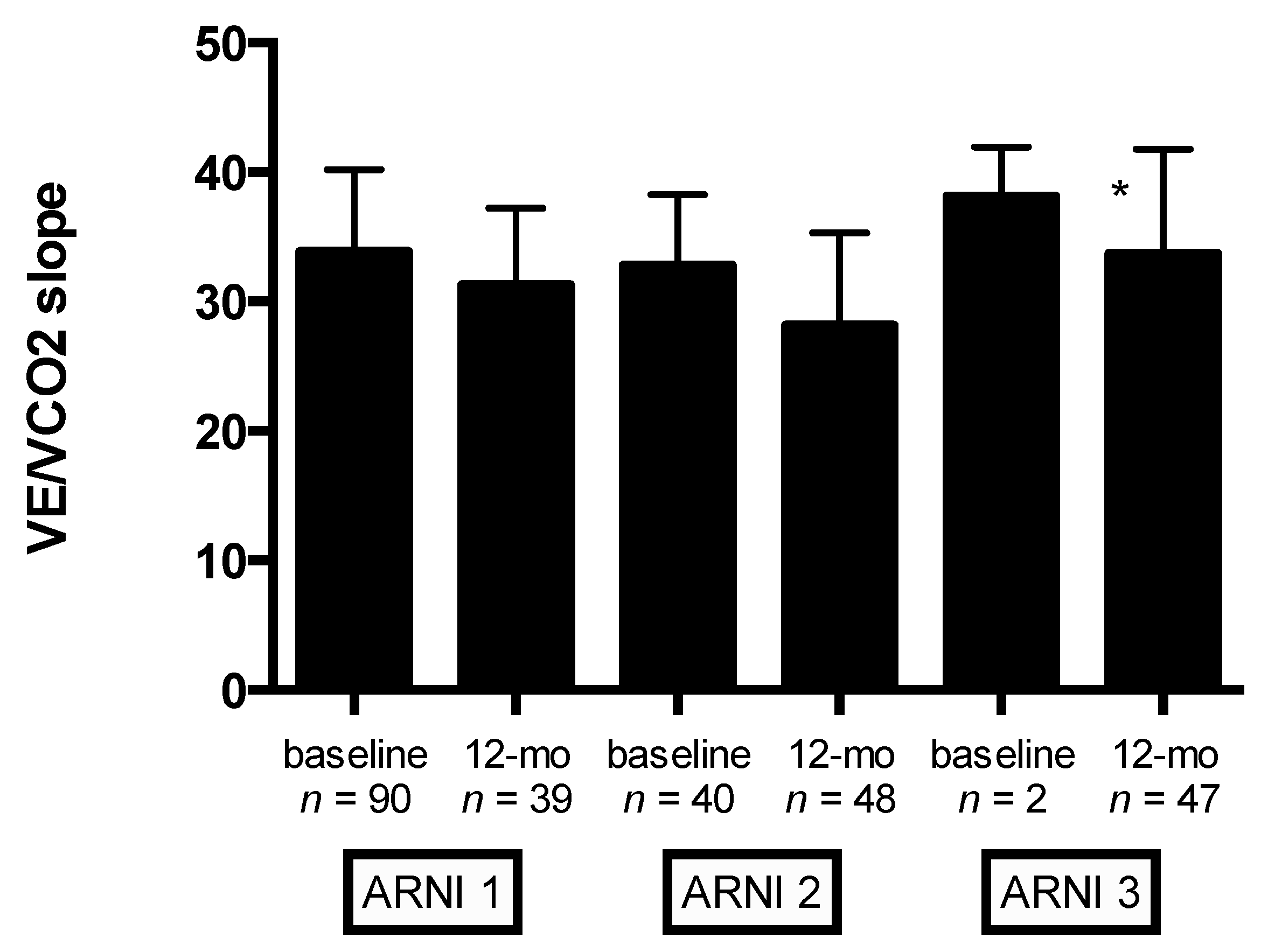
| ARNI1 | ARNI2 | ARNI3 | ||||
|---|---|---|---|---|---|---|
| Baseline (n = 90) | 12-Month Follow-Up (n = 39) | Baseline (n = 40) | 12-Month Follow-Up (n = 48) | Baseline (n = 2) | 12-Month Follow-Up (n = 47) | |
| VO2peak (mL/kg/min) | 15.3 ± 3.7 | 16.5 ± 4.2 | 14.8 ± 3.6 | 17.5 ± 4.7 ** | 14.2 ± 2.7 | 18.9 ± 4.7 |
| Predicted VO2peak (%) | 56.4 ± 13.9 | 62.5 ± 14.4 * | 54.0 ± 14.5 | 65.4 ± 16.0 ** | 50.5 ± 21.9 | 68.7 ± 19.1 |
| Watt Max (W) | 72.8 ± 25.1 | 80.6 ± 31.6 | 78.2 ± 24.9 | 86.8 ± 28.9 | 63.0 ± 7.0 | 102.8 ± 30.7 |
| VE/VCO2slope | 33.4 ± 6.2 | 32.2 ± 5.9 | 32.3 ± 5.6 | 31.3 ± 7.1 | 38.1 ± 3.8 | 28.9 ± 5.2 ** |
| RER | 1.14 ± 0.12 | 1.13 ± 0.09 | 1.13 ± 0.07 | 1.16 ± 0.11 | 1.07 ± 0.10 | 1.15 ± 0.10 |
| HR Rest (bpm) | 72.4 ± 10.8 | 68.7 ± 7.2 | 70.9 ± 10.9 | 68.3 ± 9.1 | 80.5 ± 27.6 | 69.4 ± 10.1 |
| HR Peak (bpm) | 106.6 ± 18.2 | 106.7 ± 19.9 | 106.3 ± 19.3 | 110.3 ± 15.9 | 126.0 ± 26.9 | 115.1 ± 22.1 |
| HRR (bpm) | 11.4 ± 9.5 | 14.1 ± 10.9 | 12.2 ± 11.2 | 15.0 ± 9.9 | 23.0 ± 2.8 | 18.7 ± 10.0 |
| AT-VO2 (mL/kg/min) | 11.4 ± 2.9 | 12.3 ± 2.9 | 11.4 ± 2.3 | 12.2 ± 3.7 | 10.9 ± 2.7 | 13.0 ± 2.9 |
| AT-VO2 (%) | 40.9 ± 11.5 | 45.7 ± 13.5 | 46.0 ± 13.4 | 45.8 ± 13.4 | 41.0 ± 11.3 | 50.2 ± 12.5 ** |
| AT-Watt (W) | 56.1 ± 24.8 | 57.2 ± 25.6 | 59.5 ± 19.7 | 55.1 ± 19.2 | 48.0 ± 21.3 | 67.3 ± 22.9 ** |
| O2-Pulse (mL/beat) | 11.4 ± 3.0 | 12.2 ± 3.5 | 12.6 ± 3.2 | 13.2 ± 3.8 | 10.2 ± 2.4 | 14.4 ± 3.8 * |
| ΔVO2/Δwork (mL/min/watt) | 9.2 ± 1.6 | 9.6 ± 1.8 | 9.0 ± 1.7 | 10.1 ± 1.5 ** | 9.5 ± 0.6 | 10.1 ± 1.5 |
| Peak Ventilation (L/min) | 45.8 ± 10.6 | 55.0 ± 17.9 ** | 52.7 ± 14.7 | 56.4 ± 15.0 | 47.2 ± 9.5 | 63.6 ± 18.8 ** |
| TIDAL volume (mL/kg) | 1.5 ± 0.38 | 1.7 ± 0.56 * | 1.7 ± 0.47 | 1.6 ± 0.44 | 1.6 ± 0.17 | 1.9 ± 0.5 |
| Respiratory Rate (breaths/min) | 30.8 ± 6.3 | 33.2 ± 6.9 | 31.7 ± 6.5 | 34.7 ± 6.0 * | 30.0 ± 2.8 | 32.9 ± 7.0 ** |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Giallauria, F.; Vitale, G.; Pacileo, M.; Di Lorenzo, A.; Oliviero, A.; Passaro, F.; Calce, R.; Parlato, A.; Testa, C.; D’Ambrosio, G.; et al. Sacubitril/Valsartan Improves Autonomic Function and Cardiopulmonary Parameters in Patients with Heart Failure with Reduced Ejection Fraction. J. Clin. Med. 2020, 9, 1897. https://doi.org/10.3390/jcm9061897
Giallauria F, Vitale G, Pacileo M, Di Lorenzo A, Oliviero A, Passaro F, Calce R, Parlato A, Testa C, D’Ambrosio G, et al. Sacubitril/Valsartan Improves Autonomic Function and Cardiopulmonary Parameters in Patients with Heart Failure with Reduced Ejection Fraction. Journal of Clinical Medicine. 2020; 9(6):1897. https://doi.org/10.3390/jcm9061897
Chicago/Turabian StyleGiallauria, Francesco, Giuseppe Vitale, Mario Pacileo, Anna Di Lorenzo, Alessandro Oliviero, Francesco Passaro, Roberta Calce, Alessandro Parlato, Crescenzo Testa, Giuseppe D’Ambrosio, and et al. 2020. "Sacubitril/Valsartan Improves Autonomic Function and Cardiopulmonary Parameters in Patients with Heart Failure with Reduced Ejection Fraction" Journal of Clinical Medicine 9, no. 6: 1897. https://doi.org/10.3390/jcm9061897
APA StyleGiallauria, F., Vitale, G., Pacileo, M., Di Lorenzo, A., Oliviero, A., Passaro, F., Calce, R., Parlato, A., Testa, C., D’Ambrosio, G., Romano, G., Clemenza, F., Sarullo, S., Venturini, E., Gentile, M., Nugara, C., Iannuzzo, G., D’Andrea, A., Vigorito, C., & Sarullo, F. M. (2020). Sacubitril/Valsartan Improves Autonomic Function and Cardiopulmonary Parameters in Patients with Heart Failure with Reduced Ejection Fraction. Journal of Clinical Medicine, 9(6), 1897. https://doi.org/10.3390/jcm9061897









