Using Bayesian Networks to Predict Long-Term Health-Related Quality of Life and Comorbidity after Bariatric Surgery: A Study Based on the Scandinavian Obesity Surgery Registry
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects and Variables
2.2. Statistical Methods
2.3. Model Training and Validation
2.4. Software and Hardware
3. Results
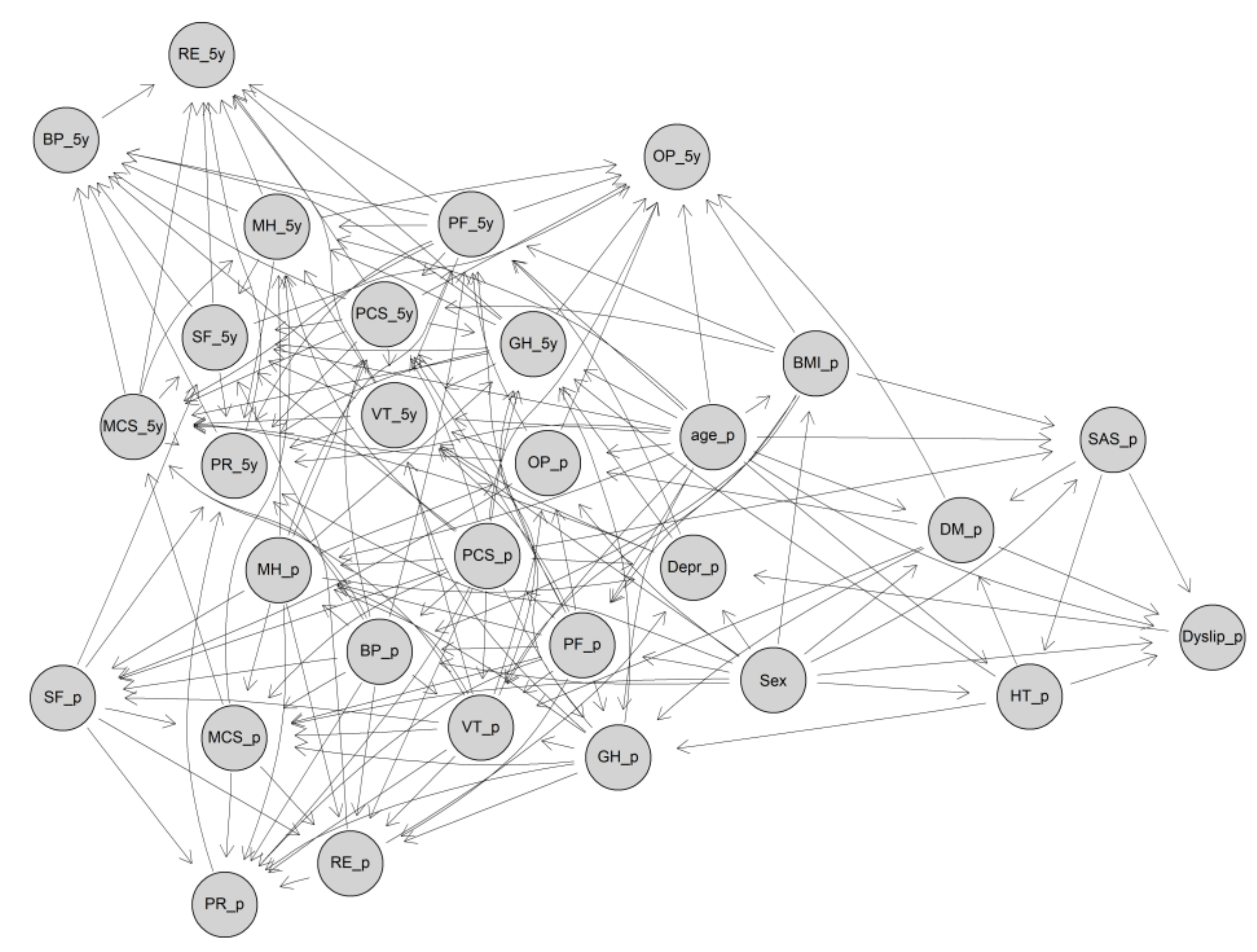
3.1. Structure of the GBN
3.2. Performance of the GBN in the Validation Dataset
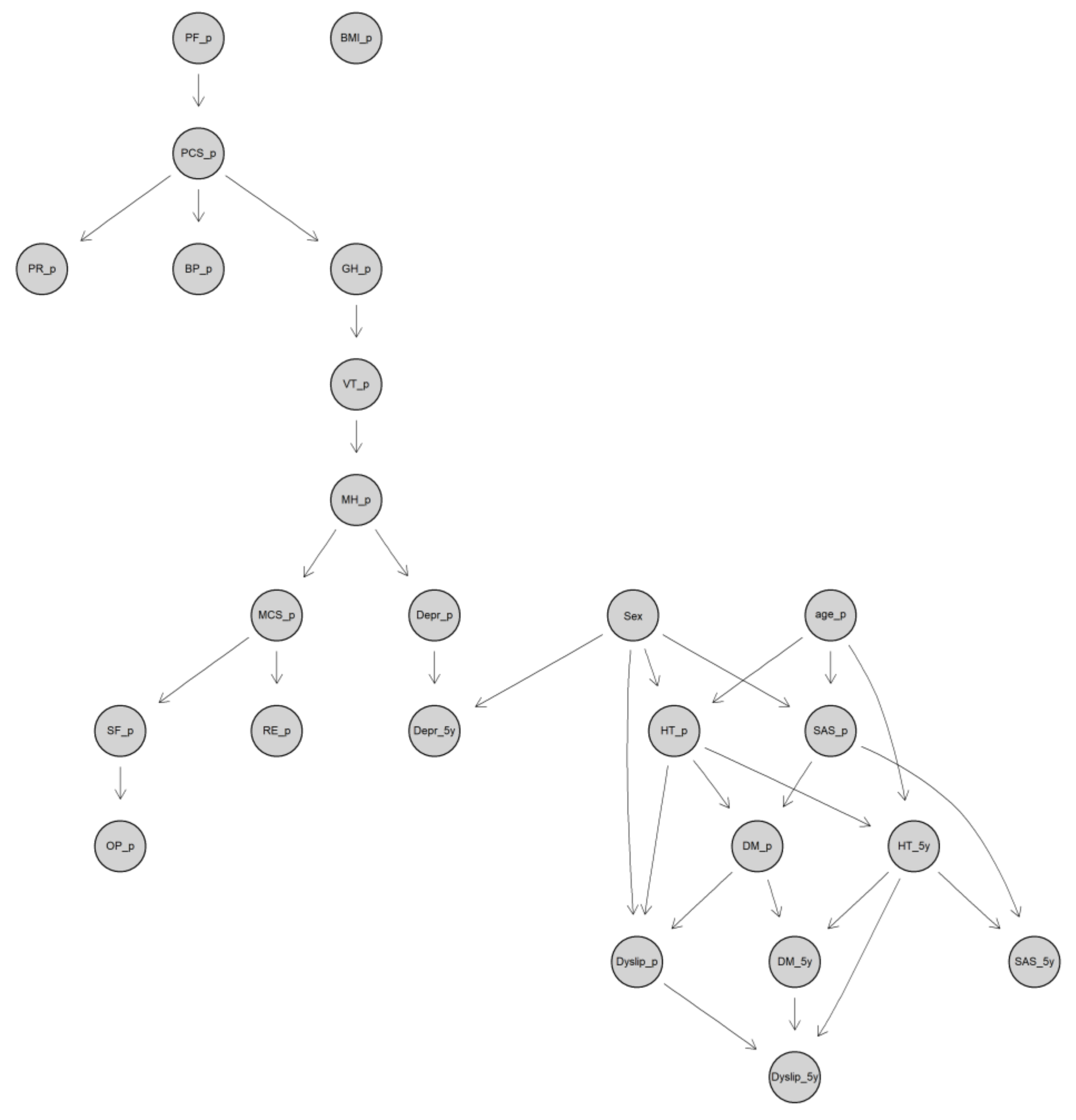
3.3. Structure of the DBN
3.4. Performance of the DBN in the Validation Dataset
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Arroyo-Johnson, C.; Mincey, K.D. Obesity Epidemiology Worldwide. Gastroenterol. Clin. N. Am. 2016, 45, 571–579. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.Y.; Hung, C.K.; Chang, Y.Y.; Tai, C.M.; Lin, J.T.; Wang, J.D. Health-related quality of life in adult patients with morbid obesity coming for bariatric surgery. Obes. Surg. 2010, 20, 1121–1127. [Google Scholar] [CrossRef] [PubMed]
- Kolotkin, R.L.; Crosby, R.D.; Williams, G.R. Health-related quality of life varies among obese subgroups. Obes. Res. 2002, 10, 748–756. [Google Scholar] [CrossRef] [PubMed]
- White, M.A.; O’Neil, P.M.; Kolotkin, R.L.; Byrne, T.K. Gender, race, and obesity-related quality of life at extreme levels of obesity. Obes. Res. 2004, 12, 949–955. [Google Scholar] [CrossRef] [PubMed]
- Angrisani, L.; Santonicola, A.; Iovino, P.; Formisano, G.; Buchwald, H.; Scopinaro, N. Bariatric Surgery Worldwide 2013. Obes. Surg. 2015, 25, 1822–1832. [Google Scholar] [CrossRef] [PubMed]
- Welbourn, R.; Pournaras, D.J.; Dixon, J.; Higa, K.; Kinsman, R.; Ottosson, J.; Ramos, A.; van Wagensveld, B.; Walton, P.; Weiner, R.; et al. Bariatric Surgery Worldwide: Baseline Demographic Description and One-Year Outcomes from the Second IFSO Global Registry Report 2013-2015. Obes. Surg. 2018, 28, 313–322. [Google Scholar] [CrossRef] [PubMed]
- Andersen, J.R.; Aasprang, A.; Karlsen, T.I.; Natvig, G.K.; Vage, V.; Kolotkin, R.L. Health-related quality of life after bariatric surgery: A systematic review of prospective long-term studies. Surg. Obes. Relat. Dis. 2015, 11, 466–473. [Google Scholar] [CrossRef] [PubMed]
- Kalarchian, M.A.; Marcus, M.D.; Courcoulas, A.P.; Cheng, Y.; Levine, M.D. Self-report of gastrointestinal side effects after bariatric surgery. Surg. Obes. Relat. Dis. 2014, 10, 1202–1207. [Google Scholar] [CrossRef]
- O’Brien, P.E. Bariatric surgery: Mechanisms, indications and outcomes. J. Gastroenterol. Hepatol. 2010, 25, 1358–1365. [Google Scholar] [CrossRef]
- Balsiger, B.M.; Murr, M.M.; Poggio, J.L.; Sarr, M.G. Bariatric surgery. Surgery for weight control in patients with morbid obesity. Med. Clin. N. Am. 2000, 84, 477–489. [Google Scholar] [CrossRef]
- Peterhansel, C.; Nagl, M.; Wagner, B.; Dietrich, A.; Kersting, A. Predictors of Changes in Health-Related Quality of Life 6 and 12 months After a Bariatric Procedure. Obes. Surg. 2017, 27, 2120–2128. [Google Scholar] [CrossRef] [PubMed]
- Khandalavala, B.N.; Geske, J.; Nirmalraj, M.; Koran-Scholl, J.B.; Neumann-Potash, L.; McBride, C.L. Predictors of Health-Related Quality of Life After Bariatric Surgery. Obes. Surg. 2015, 25, 2302–2305. [Google Scholar] [CrossRef] [PubMed]
- Wimmelmann, C.L.; Dela, F.; Mortensen, E.L. Psychological predictors of mental health and health-related quality of life after bariatric surgery: A review of the recent research. Obes. Res. Clin. Pract. 2014, 8, e314–e324. [Google Scholar] [CrossRef] [PubMed]
- Janik, M.R.; Rogula, T.; Bielecka, I.; Kwiatkowski, A.; Pasnik, K. Quality of Life and Bariatric Surgery: Cross-Sectional Study and Analysis of Factors Influencing Outcome. Obes. Surg. 2016, 26, 2849–2855. [Google Scholar] [CrossRef]
- Cao, Y.; Raoof, M.; Montgomery, S.; Ottosson, J.; Naslund, I. Predicting Long-Term Health-Related Quality of Life after Bariatric Surgery Using a Conventional Neural Network: A Study Based on the Scandinavian Obesity Surgery Registry. J. Clin. Med. 2019, 8, 2149. [Google Scholar] [CrossRef]
- Raoof, M.; Szabo, E.; Karlsson, J.; Näslund, E.; Cao, Y.; Näslund, I. Improvements of health-related quality of life five years after gastric bypass. What is important besides weight loss? A study from Scandinavian Obesity Surgery Register. Surg. Obes. Relat. Dis. 2020, in press. [Google Scholar] [CrossRef]
- Cao, Y.; Montgomery, S.; Ottosson, J.; Naslund, E.; Stenberg, E. Deep Learning Neural Networks to Predict Serious Complications After Bariatric Surgery: Analysis of Scandinavian Obesity Surgery Registry Data. JMIR Med. Inform. 2020, 8, e15992. [Google Scholar] [CrossRef]
- Hedenbro, J.L.; Naslund, E.; Boman, L.; Lundegardh, G.; Bylund, A.; Ekelund, M.; Laurenius, A.; Moller, P.; Olbers, T.; Sundbom, M.; et al. Formation of the Scandinavian Obesity Surgery Registry, SOReg. Obes. Surg. 2015, 25, 1893–1900. [Google Scholar] [CrossRef]
- Gerber, P.; Anderin, C.; Szabo, E.; Naslund, I.; Thorell, A. Impact of age on risk of complications after gastric bypass: A cohort study from the Scandinavian Obesity Surgery Registry (SOReg). Surg. Obes. Relat. Dis. 2018, 14, 437–442. [Google Scholar] [CrossRef] [PubMed]
- Stenberg, E.; Cao, Y.; Szabo, E.; Naslund, E.; Naslund, I.; Ottosson, J. Risk Prediction Model for Severe Postoperative Complication in Bariatric Surgery. Obes. Surg. 2018. [Google Scholar] [CrossRef] [PubMed]
- Tao, W.; Holmberg, D.; Naslund, E.; Naslund, I.; Mattsson, F.; Lagergren, J.; Ljung, R. Validation of Obesity Surgery Data in the Swedish National Patient Registry and Scandinavian Obesity Registry (SOReg). Obes. Surg. 2016, 26, 1750–1756. [Google Scholar] [CrossRef]
- Hays, R.D.; Morales, L.S. The RAND-36 measure of health-related quality of life. Ann. Med. 2001, 33, 350–357. [Google Scholar] [CrossRef]
- Karlsson, J.; Taft, C.; Sjostrom, L.; Torgerson, J.S.; Sullivan, M. Psychosocial functioning in the obese before and after weight reduction: Construct validity and responsiveness of the Obesity-related Problems scale. Int. J. Obes. 2003, 27, 617–630. [Google Scholar] [CrossRef] [PubMed]
- Ben-Gal, I. Bayesian Networks; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2008; Volume 1. [Google Scholar]
- Scutari, M.; Denis, J.-B. Bayesian Networks: With Examples in R; Chapman and Hall/CRC: Boca Raton, FL, USA, 2014. [Google Scholar]
- Nagarajan, R.; Scutari, M.; Lèbre, S. Bayesian Networks in r: With Applications in Systems Biology; Springer: London, UK, 2013; Volume 48. [Google Scholar]
- Grzegorczyk, M. An introduction to Gaussian Bayesian networks. Methods Mol. Biol. 2010, 662, 121–147. [Google Scholar] [CrossRef] [PubMed]
- Pozzi, M.; Der Kiureghian, A. Gaussian Bayesian network for reliability analysis of a system of bridges. In Proceedings of the 11th International Conference on Structural Safety and Reliability, New York, NY, USA, 16 June 2013. [Google Scholar]
- Weitzen, S.; Lapane, K.L.; Toledano, A.Y.; Hume, A.L.; Mor, V. Principles for modeling propensity scores in medical research: A systematic literature review. Pharmacoepidemiol. Drug Saf. 2004, 13, 841–853. [Google Scholar] [CrossRef] [PubMed]
- Hartemink, A.J. Principled Computational Methods for the Validation Discovery of Genetic Regulatory Networks; Massachusetts Institute of Technology: Cambridge, MA, USA, 2001. [Google Scholar]
- Sachs, K.; Perez, O.; Pe’er, D.; Lauffenburger, D.A.; Nolan, G.P. Causal protein-signaling networks derived from multiparameter single-cell data. Science 2005, 308, 523–529. [Google Scholar] [CrossRef]
- Caruana, R.; Niculescu-Mizil, A. Data mining in metric space: An empirical analysis of supervised learning performance criteria. In Proceedings of the Tenth ACM SIGKDD International Conference on Knowledge Discovery and Data Mining, Seattle, WA, USA, 22–25 August 2004; pp. 69–78. [Google Scholar]
- Cao, Y.; Fang, X.; Ottosson, J.; Naslund, E.; Stenberg, E. A Comparative Study of Machine Learning Algorithms in Predicting Severe Complications after Bariatric Surgery. J. Clin. Med. 2019, 8, 668. [Google Scholar] [CrossRef]
- Mandrekar, J.N. Receiver operating characteristic curve in diagnostic test assessment. J. Thorac. Oncol. 2010, 5, 1315–1316. [Google Scholar] [CrossRef]
- Marzban, C. The ROC curve and the area under it as performance measures. Weather Forecast. 2004, 19, 1106–1114. [Google Scholar] [CrossRef]
- Scutari, M. Learning Bayesian Networks with the bnlearn R Package. J. Stat. Softw 2010, 35, 1–22. [Google Scholar] [CrossRef]
- Kammerdiner, A.R.; Gupal, A.M.; Pardalos, P.M. Application of Bayesian networks and data mining to biomedical problems. AIP Conf. Proc. 2007, 953, 132. [Google Scholar]
- Lucas, P.J. Biomedical applications of Bayesian networks. In Advances in Probabilistic Graphical Models; Springer: Berlin/Heidelberg, Germany, 2007; pp. 333–358. [Google Scholar]
- Pearl, J. Probabilistic Reasoning in Intelligent Systems: Networks of Plausible Inference; Elsevier: Amsterdam, The Netherlands, 2014. [Google Scholar]
- Mani, S.; Valtorta, M.; McDermott, S. Building Bayesian network models in medicine: The MENTOR experience. Appl. Intell. 2005, 22, 93–108. [Google Scholar] [CrossRef]
- Blaine, B. Does depression cause obesity? A meta-analysis of longitudinal studies of depression and weight control. J. Health Psychol. 2008, 13, 1190–1197. [Google Scholar] [CrossRef]
- Hyttinen, A.; Eberhardt, F.; Hoyer, P.O. Learning linear cyclic causal models with latent variables. J. Mach. Learn. Res. 2012, 13, 3387–3439. [Google Scholar]
- Neville, J.; Jensen, D. Relational dependency networks. J. Mach. Learn. Res. 2007, 8, 653–692. [Google Scholar]
- Pontiroli, A.E.; Fossati, A.; Vedani, P.; Fiorilli, M.; Folli, F.; Paganelli, M.; Marchi, M.; Maffei, C. Post-surgery adherence to scheduled visits and compliance, more than personality disorders, predict outcome of bariatric restrictive surgery in morbidly obese patients. Obes. Surg. 2007, 17, 1492–1497. [Google Scholar] [CrossRef]
- Tsushima, W.T.; Bridenstine, M.P.; Balfour, J.F. MMPI-2 scores in the outcome prediction of gastric bypass surgery. Obes. Surg. 2004, 14, 528–532. [Google Scholar] [CrossRef]
- Finks, J.F.; Kole, K.L.; Yenumula, P.R.; English, W.J.; Krause, K.R.; Carlin, A.M.; Genaw, J.A.; Banerjee, M.; Birkmeyer, J.D.; Birkmeyer, N.J.; et al. Predicting risk for serious complications with bariatric surgery: Results from the Michigan Bariatric Surgery Collaborative. Ann. Surg. 2011, 254, 633–640. [Google Scholar] [CrossRef]
- Hayes, M.T.; Hunt, L.A.; Foo, J.; Tychinskaya, Y.; Stubbs, R.S. A model for predicting the resolution of type 2 diabetes in severely obese subjects following Roux-en Y gastric bypass surgery. Obes. Surg. 2011, 21, 910–916. [Google Scholar] [CrossRef] [PubMed]
- Cruz, M.R.; Martins, C.; Dias, J.; Pinto, J.S. A validation of an intelligent decision-making support system for the nutrition diagnosis of bariatric surgery patients. JMIR Med. Inform. 2014, 2, e8. [Google Scholar] [CrossRef]
- Susser, M. What Is a Cause and How Do We Know One-a Grammar for Pragmatic Epidemiology. Am. J. Epidemiol. 1991, 133, 635–648. [Google Scholar] [CrossRef]
- Karhausen, L.R. On the Logic of Causal Inference. Am. J. Epidemiol. 1987, 126, 556–557. [Google Scholar] [CrossRef] [PubMed]
- Li, J.; Shi, J.J.; Satz, D. Modeling and analysis of disease and risk factors through learning Bayesian networks from observational data. Qual. Reliab. Eng. Int. 2008, 24, 291–302. [Google Scholar] [CrossRef]
- Nguefack-Tsague, G. Using bayesian networks to model hierarchical relationships in epidemiological studies. Epidemiol. Health 2011, 33, e2011006. [Google Scholar] [CrossRef]
- Moffa, G.; Catone, G.; Kuipers, J.; Kuipers, E.; Freeman, D.; Marwaha, S.; Lennox, B.R.; Broome, M.R.; Bebbington, P. Using Directed Acyclic Graphs in Epidemiological Research in Psychosis: An Analysis of the Role of Bullying in Psychosis. Schizophr. Bull. 2017, 43, 1273–1279. [Google Scholar] [CrossRef] [PubMed]
- Hess, R.; Thurston, R.C.; Hays, R.D.; Chang, C.C.; Dillon, S.N.; Ness, R.B.; Bryce, C.L.; Kapoor, W.N.; Matthews, K.A. The impact of menopause on health-related quality of life: Results from the STRIDE longitudinal study. Qual. Life Res. 2012, 21, 535–544. [Google Scholar] [CrossRef] [PubMed]

| Preoperative | 5-Year Postoperative | |
|---|---|---|
| Age (year) | 42.7 ± 11.0 | 47.7 ± 11.0 |
| BMI (kg/m2) | 42.3 ± 5.2 | 30.3 ± 5.2 |
| Female | 5154 (78.8%) | 5154 (78.8%) |
| SAS | 668 (10.2%) | 188 (2.9%) |
| Hypertension | 1817 (27.8%)) | 1420 (21.7%) |
| T2D | 973 (14.9%) | 452 (6.9%) |
| Depression | 855 (13.1%) | 1162 (17.8%) |
| Dyslipidemia | 732 (11.2%) | 429 (6.6%) |
| PF | 61.7 ± 21.9 | 84.2 ± 20.7 |
| RP | 60.3 ± 38.9 | 77.9 ± 36.5 |
| BP | 56.0 ± 26.9 | 65.2 ± 30.7 |
| GH | 58.2 ± 21.4 | 68.1 ± 24.7 |
| VT | 47.4 ± 23.0 | 54.5 ± 26.9 |
| SF | 74.9 ± 26.1 | 79.6 ± 26.4 |
| RE | 76.0 ± 36.2 | 76.9 ± 37.8 |
| MH | 71.5 ± 19.4 | 72.0 ± 23.0 |
| PCS | 38.3 ± 10.7 | 47.6 ± 11.1 |
| MCS | 46.8 ± 11.7 | 44.6 ± 13.8 |
| OP | 61.0 ± 26.4 | 25.6 ± 27.4 |
| HRQoL Scores | GBN | CNN | Linear Regression |
|---|---|---|---|
| PF | 0.0335 | 0.0350 | 0.0343 |
| RP | 0.1166 | 0.1324 | 0.1211 |
| BP | 0.0813 | 0.0898 | 0.0772 |
| GH | 0.0499 | 0.0618 | 0.0508 |
| VT | 0.0590 | 0.0914 | 0.0625 |
| SF | 0.0599 | 0.0995 | 0.0588 |
| RE | 0.1230 | 0.2118 | 0.1269 |
| MH | 0.0436 | 0.0807 | 0.0416 |
| PCS | 0.0196 | 0.0333 | 0.0219 |
| MCS | 0.0356 | 0.0584 | 0.0305 |
| OP | 0.0597 | 0.0750 | 0.0608 |
| Comorbidity | DBN | MLR | ||||||
|---|---|---|---|---|---|---|---|---|
| Sen | Spe | Acc | AUC (95% CI) | Sen | Spe | Acc | AUC (95% CI) | |
| SAS | 0.64 | 0.92 | 0.91 | 0.83 (0.76, 0.91) | 0.90 | 0.73 | 0.73 | 0.90 (0.86, 0.94) |
| Hypertension | 0.83 | 0.83 | 0.84 | 0.89 (0.87, 0.91) | 0.73 | 0.67 | 0.68 | 0.76 (0.73, 0.79) |
| T2D | 0.96 | 0.89 | 0.90 | 0.94 (0.92, 0.96) | 0.78 | 0.68 | 0.69 | 0.76 (0.72, 0.81) |
| Depression | 0.51 | 0.95 | 0.87 | 0.75 (0.72, 0.78) | 0.66 | 0.55 | 0.57 | 0.61 (0.67, 0.65) |
| Dyslipidemia | 0.78 | 0.91 | 0.90 | 0.92 (0.88, 0.95) | 0.76 | 0.67 | 0.68 | 0.77 (0.74, 0.82) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cao, Y.; Raoof, M.; Szabo, E.; Ottosson, J.; Näslund, I. Using Bayesian Networks to Predict Long-Term Health-Related Quality of Life and Comorbidity after Bariatric Surgery: A Study Based on the Scandinavian Obesity Surgery Registry. J. Clin. Med. 2020, 9, 1895. https://doi.org/10.3390/jcm9061895
Cao Y, Raoof M, Szabo E, Ottosson J, Näslund I. Using Bayesian Networks to Predict Long-Term Health-Related Quality of Life and Comorbidity after Bariatric Surgery: A Study Based on the Scandinavian Obesity Surgery Registry. Journal of Clinical Medicine. 2020; 9(6):1895. https://doi.org/10.3390/jcm9061895
Chicago/Turabian StyleCao, Yang, Mustafa Raoof, Eva Szabo, Johan Ottosson, and Ingmar Näslund. 2020. "Using Bayesian Networks to Predict Long-Term Health-Related Quality of Life and Comorbidity after Bariatric Surgery: A Study Based on the Scandinavian Obesity Surgery Registry" Journal of Clinical Medicine 9, no. 6: 1895. https://doi.org/10.3390/jcm9061895
APA StyleCao, Y., Raoof, M., Szabo, E., Ottosson, J., & Näslund, I. (2020). Using Bayesian Networks to Predict Long-Term Health-Related Quality of Life and Comorbidity after Bariatric Surgery: A Study Based on the Scandinavian Obesity Surgery Registry. Journal of Clinical Medicine, 9(6), 1895. https://doi.org/10.3390/jcm9061895





