Multidimensional Evaluation of Continuous Positive Airway Pressure (CPAP) Treatment for Sleep Apnea in Different Clusters of Couples
Abstract
1. Introduction
2. Methods
2.1. Study Participants
2.2. Assessments
2.3. CPAP Prescription, Initiation and Follow-Up
2.4. Statistical Analysis
3. Results
3.1. Patient and Couple Cluster Characteristics
3.2. Cluster Analysis
3.3. Baseline Couple Cluster Data
3.3.1. Baseline Epworth Sleepiness Score
3.3.2. Baseline Quebec Sleep Questionnaire Score
3.3.3. Baseline Quality Marriage Index
3.4. Impact of Couple Clusters on CPAP Adherence and Questionnaires
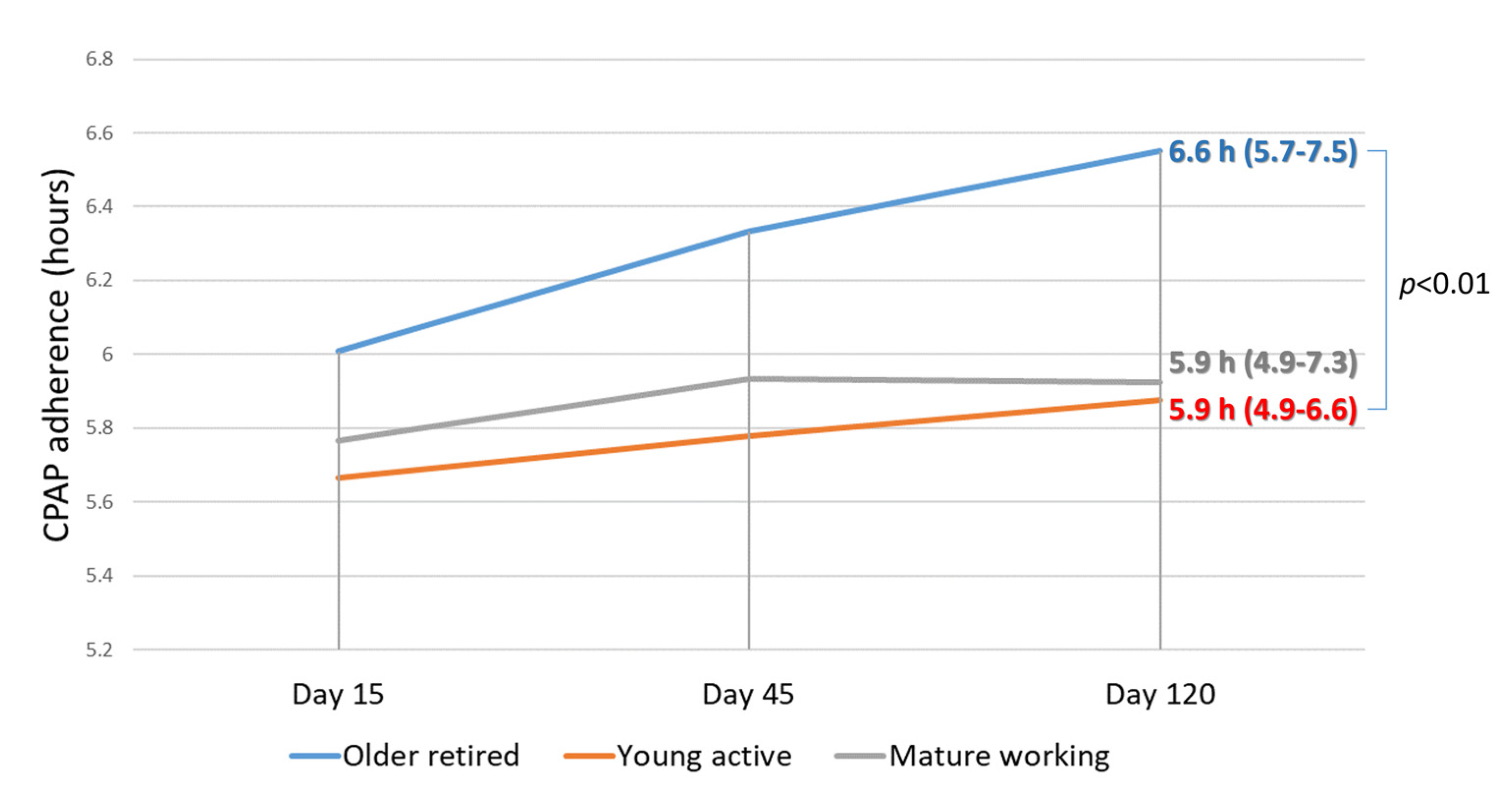
3.4.1. CPAP adherence
3.4.2. Epworth Sleepiness Score
3.4.3. Quebec Sleep Questionnaire Score
3.4.4. Dyadic Adjustment Scale
3.4.5. Quality of Marriage Index
3.4.6. Spouse’s Sleep Quality
3.4.7. Spousal Involvement
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Benjafield, A.V.; Ayas, N.T.; Eastwood, P.R.; Heinzer, R.; Ip, M.S.M.; Morrell, M.J.; Nunez, C.M.; Patel, S.R.; Penzel, T.; Pépin, J.L.D.; et al. Estimation of the global prevalence and burden of obstructive sleep apnoea: A literature-based analysis. Lancet Respir. Med. 2019, 7, 687–698. [Google Scholar] [CrossRef]
- Levy, P.A.; Kohler, M.; McNicholas, W.T.; Barbé, F.; McEvoy, R.D.; Somers, V.K.; Lavie, L.; Pépin, J.L. Obstructive sleep apnoea syndrome. Nat. Rev. Dis. Primers 2015, 1, 15015. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Zhou, Z.; McEvoy, R.D.; Anderson, C.S.; Rodgers, A.; Perkovic, V.; Neal, B. Association of positive airway pressure with cardiovascular events and death in adults with sleep apnea: A systematic review and meta-analysis. JAMA 2017, 318, 156–166. [Google Scholar] [CrossRef] [PubMed]
- Cistulli, P.A.; Armitstead, J.; Pepin, J.L.; Woehrle, H.; Nunez, C.M.; Benjafield, A.; Malhotra, A. Short-term CPAP adherence in obstructive sleep apnea: A big data analysis using real world data. Sleep Med. 2019, 59, 114–116. [Google Scholar] [CrossRef] [PubMed]
- Baratta, F.; Pastori, D.; Bucci, T.; Fabiani, M.; Fabiani, V.; Brunori, M.; Loffredo, L.; Lillo, R.; Pannitteri, G.; Angelico, F.; et al. Long-term prediction of adherence to continuous positive air pressure therapy for the treatment of moderate/severe obstructive sleep apnea syndrome. Sleep Med. 2018, 43, 66–70. [Google Scholar] [CrossRef] [PubMed]
- Chai-Coetzer, C.L.; Luo, Y.M.; Antic, N.A.; Zhang, X.L.; Chen, B.Y.; He, Q.Y.; Heeley, E.; Huang, S.G.; Anderson, C.S.; Zhong, N.S.; et al. Predictors of long-term adherence to continuous positive airway pressure therapy in patients with obstructive sleep apnea and cardiovascular disease in the save study. Sleep 2013, 36, 1929–1937. [Google Scholar] [CrossRef] [PubMed]
- Weaver, T.E.; Grunstein, R.R. Adherence to continuous positive airway pressure therapy. Proc. Am. Thorac. Soc. 2008, 5, 173–178. [Google Scholar] [CrossRef]
- Diaz-Abad, M.; Chatila, W.; Lammi, M.R.; Swift, I.; D’Alonzo, G.E.; Krachman, S.L. Determinants of CPAP adherence in hispanics with obstructive sleep apnea. Sleep Disord. 2014, 2014, 6. [Google Scholar] [CrossRef]
- Salepci, B.; Caglayan, B.; Kiral, N.; Sarac, G.; Fidan, A.; Torun, E.; Comert, S.S.; Gungor, G.A. CPAP Adherence of Patients With Obstructive Sleep Apnea. Respir. Care 2013, 58, 1467–1473. [Google Scholar] [CrossRef]
- Weaver, T.E.; Maislin, G.; Dinges, D.F.; Bloxham, T.; George, C.F.P.; Greenberg, H.; Kader, G.; Mahowald, M.; Younger, J.; Pack, A.I. Relationship between hours of cpap use and achieving normal levels of sleepiness and daily functioning. Sleep 2007, 30, 711–719. [Google Scholar] [CrossRef]
- Berg, C.A.; Upchurch, R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychol. Bull. 2007, 133, 920–954. [Google Scholar] [CrossRef] [PubMed]
- Broström, A.; Nilsen, P.; Johansson, P.; Ulander, M.; Strömberg, A.; Svanborg, E.; Fridlund, B. Putative facilitators and barriers for adherence to CPAP treatment in patients with obstructive sleep apnea syndrome: A qualitative content analysis. Sleep Med. 2010, 11, 126–130. [Google Scholar] [CrossRef] [PubMed]
- Gentina, T.; Bailly, S.; Jounieaux, F.; Verkindre, C.; Broussier, P.M.; Guffroy, D.; Prigent, A.; Gres, J.J.; Kabbani, J.; Kedziora, L.; et al. Marital quality, partner’s engagement and continuous positive airway pressure adherence in obstructive sleep apnea. Sleep Med. 2019, 55, 56–61. [Google Scholar] [CrossRef] [PubMed]
- Merenda, A.; Miano, P. Co-parental couples and new families: A study of the primary triad. Procedia Soc. Behav. Sci. 2015, 174, 1107–1110. [Google Scholar] [CrossRef]
- Berry, R.B.; Budhiraja, R.; Gottlieb, D.J.; Gozal, D.; Iber, C.; Kapur, V.; Marcus, C.L.; Mehra, R.; Parthasarathy, S.; Quan, S.F.; et al. Rules for scoring respiratory events in sleep: Update of the 2007 AASM manual for the scoring of sleep and associated events. J. Clin. Sleep Med. 2012, 8, 597–619. [Google Scholar] [CrossRef]
- Lacasse, Y.; Bureau, M.P.; Series, F. A new standardised and self-administered quality of life questionnaire specific to obstructive sleep apnoea. Thorax 2004, 59, 494–499. [Google Scholar] [CrossRef]
- Norton, R. Measuring marital quality: A critical look at the dependent variable. J. Marriage Fam. 1983, 45, 141–151. [Google Scholar] [CrossRef]
- Carey, M.P.; Spector, I.P.; Lantinga, L.J.; Krauss, D.J. Reliability of the dyadic adjustment scale. Psychol. Assess. 1993, 15, 238–240. [Google Scholar] [CrossRef]
- Lewis, K.E.; Seale, L.; Bartle, I.E.; Watkins, A.J.; Ebden, P. Early predictors of CPAP use for the treatment of obstructive sleep apnea. Sleep 2004, 27, 134–138. [Google Scholar] [CrossRef]
- Baron, K.G.; Smith, T.W.; Berg, C.; Czajkowski, L.A.; Gunn, H.; Jones, C.R. Spousal involvement in CPAP adherence among patients with obstructive sleep apnea. Sleep Breath. 2010, 15, 525–534. [Google Scholar] [CrossRef]
- Wiese, H.J.; Boethel, C.; Phillips, B.; Wilson, J.F.; Peters, J.; Viggiano, T. CPAP compliance: Video education may help! Sleep Med. 2005, 6, 171–174. [Google Scholar] [CrossRef]
- Hagenaars, J.A.; McCutcheon, A.L. Applied Latent Class. Analysis; Cambridge University Press: Cambridge, UK, 2002. [Google Scholar]
- Marbac, M.; Sedki, M. VarSelLCM: An R/C++ package for variable selection in model-based clustering of mixed-data with missing values. Bioinformatics 2019, 35, 1255–1257. [Google Scholar] [CrossRef] [PubMed]
- Sin, D.; Mayers, I.; Man, G.C.W.; Pawluk, L. Long-term compliance rates to continuous positive airway pressure in obstructive sleep apnea. Chest 2002, 121, 430–435. [Google Scholar] [CrossRef] [PubMed]
- Batool-Anwar, S.; Baldwin, C.M.; Fass, S.; Quan, S.F. Role of spousal involvement in continuous positive airway pressure (CPAP) adherence in patients with obstructive sleep apnea (OSA). Southwest J. Pulm. Crit. Care 2017, 14, 213–227. [Google Scholar] [CrossRef]
- McArdle, N.; Kingshott, R.; Engleman, H.M.; Mackay, T.W.; Douglas, N.J. Partners of patients with sleep apnoea/hypopnoea syndrome: Effect of CPAP treatment on sleep quality and quality of life. Thorax 2001, 56, 513–518. [Google Scholar] [CrossRef] [PubMed]
- Crook, S.; Sievi, N.A.; Bloch, K.E.; Stradling, J.R.; Frei, A.; Puhan, M.A.; Kohler, M. Minimum important difference of the Epworth Sleepiness Scale in obstructive sleep apnoea: Estimation from three randomised controlled trials. Thorax 2019, 74, 390–396. [Google Scholar] [CrossRef]
- Baron, K.G.; Gunn, H.E.; Czajkowski, L.A.; Smith, T.W.; Jones, C.R. Spousal involvement in CPAP: Does pressure help? J. Clin. Sleep Med. 2012, 8, 147–153. [Google Scholar] [CrossRef][Green Version]
- Hoy, C.J.; Vennelle, M.; Kingshott, R.N.; Engleman, H.M.; Douglas, N.J. Can intensive support improve continuous positive airway pressure use in patients with the sleep apnea/hypopnea syndrome? Am. J. Respir. Crit. Care Med. 1999, 159, 1096–1100. [Google Scholar] [CrossRef]
- Weaver, T.E. Novel aspects of CPAP treatment and interventions to improve CPAP adherence. J. Clin. Med. 2019, 8, 2220. [Google Scholar] [CrossRef]
- Parthasarathy, S.; Wendel, C.; Haynes, P.L.; Atwood, C.; Kuna, S. A pilot study of CPAP adherence promotion by peer buddies with sleep apnea. J. Clin. Sleep Med. 2013, 9, 543–550. [Google Scholar] [CrossRef]
- McFadyen, T.A.; Espie, C.A.; McArdle, N.; Douglas, N.J.; Engleman, H.M. Controlled, prospective trial of psychosocial function before and after continuous positive airway pressure therapy. Eur. Respir. J. 2001, 18, 996–1002. [Google Scholar] [CrossRef] [PubMed]
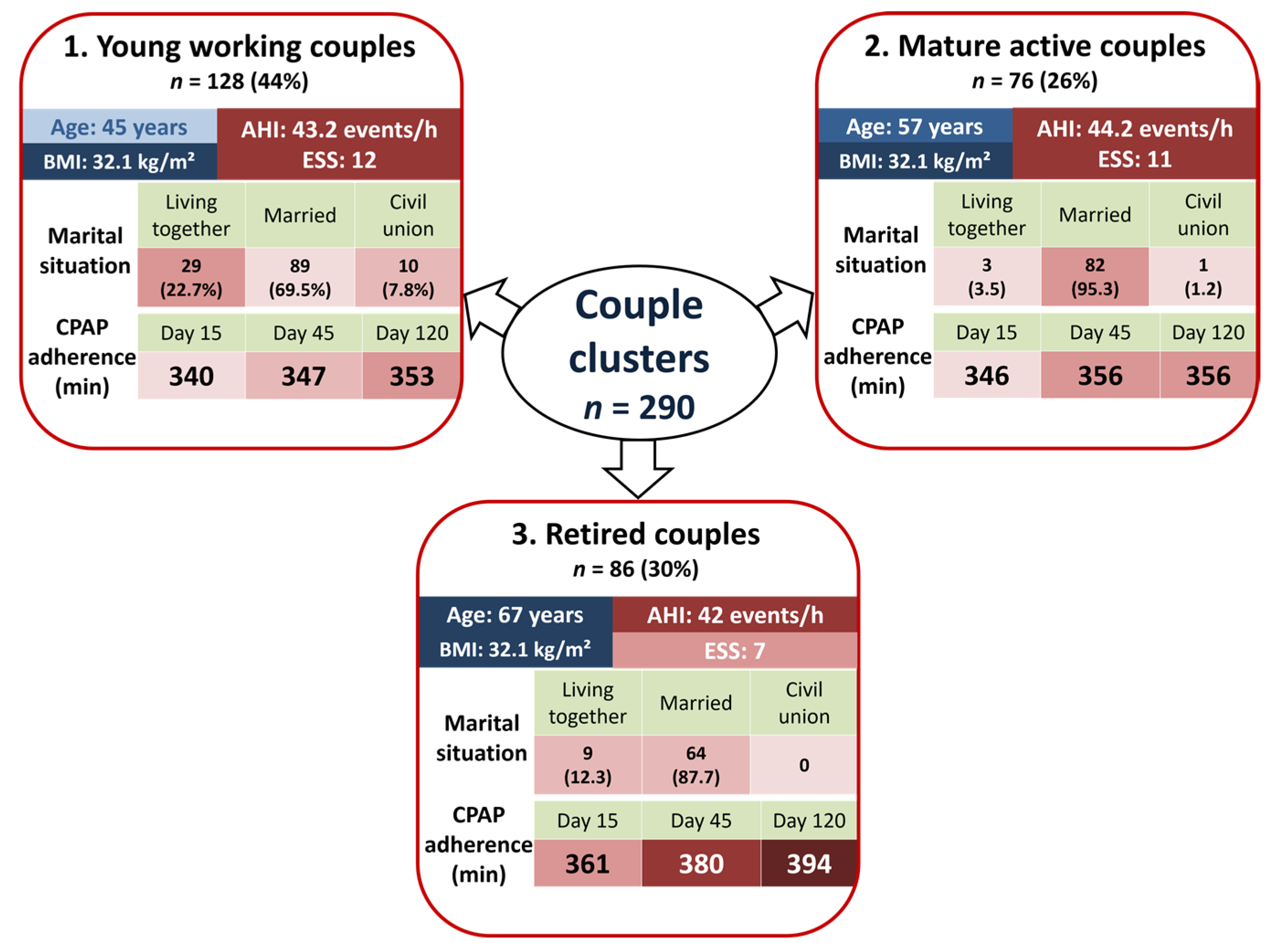
| Variables | Class 1: Older Retired Couples n = 76 (26%) | Class 2: Young Working Couples n = 128 (44%) | Class 3: Mature Active Couples n = 86 (30%) | Overall p-Value |
|---|---|---|---|---|
| Age (year) | 67 (63–71) | 45 (40–49) | 57 (54–59) | <0.01 |
| Gender (male) | 60 (80) | 102 (79.7) | 62 (72.1) | 0.36 |
| BMI (kg/m2) | 32.1 (27.6–35.7) | 32.1 (28.9–35.8) | 32.1 (27.7–37.4) | 0.81 |
| AHI (events/h) | 42 (34.7–52) | 43.2 (33–60.1) | 44.2 (32–57) | 0.89 |
| Epworth score | 7 (5–12) | 12 (8–16) | 11 (7–15) | <0.01 |
| Orofacial CPAP mask (%) | 21 (28) | 24 (19.5) | 18 (21.4) | 0.37 |
| APAP (%) | 70 (94.6) | 120 (95.2) | 77 (89.5) | 0.23 |
| Variables | Variable Items | Class 1: Older Retired Couples n = 76 (26%) | Class 2: Young Working Couples n = 128 (44%) | Class 3: Mature Active Couples n = 86 (30%) | Overall p-Value |
|---|---|---|---|---|---|
| Marital situation | Living together | 9 (12.3) | 29 (22.7) | 3 (3.5) | <0.01 |
| Married | 64 (87.7) | 89 (69.5) | 82 (95.3) | ||
| Civil union | 0 (0) | 10 (7.8) | 1 (1.2) | ||
| Children at home | Yes | 11 (15.3) | 106 (83.5) | 37 (43.5) | <0.01 |
| Same bedtime | Yes | 39 (54.9) | 60 (47.2) | 55 (64) | 0.06 |
| Separate bedroom | Yes | 22 (29.7) | 40 (31.7) | 18 (21.7) | 0.27 |
| Size of mattress | >140 cm | 31 (46.3) | 79 (63.7) | 46 (59.7) | 0.06 |
| Number of years together | 10 to 30 years | 13 (19.4) | 72 (58.5) | 25 (29.4) | <0.01 |
| <10 years | 2 (3) | 51 (41.5) | 5 (5.9) | ||
| >30 years | 52 (77.6) | 0 (0) | 55 (64.7) | ||
| Professional activity | Both working | 0 (0) | 96 (75) | 43 (53.1) | <0.01 |
| No one working | 73 (97.3) | 0 (0) | 1 (1.2) | ||
| One is working | 2 (2.7) | 32 (25) | 37 (45.7) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mendelson, M.; Gentina, T.; Gentina, E.; Tamisier, R.; Pépin, J.-L.; Bailly, S. Multidimensional Evaluation of Continuous Positive Airway Pressure (CPAP) Treatment for Sleep Apnea in Different Clusters of Couples. J. Clin. Med. 2020, 9, 1658. https://doi.org/10.3390/jcm9061658
Mendelson M, Gentina T, Gentina E, Tamisier R, Pépin J-L, Bailly S. Multidimensional Evaluation of Continuous Positive Airway Pressure (CPAP) Treatment for Sleep Apnea in Different Clusters of Couples. Journal of Clinical Medicine. 2020; 9(6):1658. https://doi.org/10.3390/jcm9061658
Chicago/Turabian StyleMendelson, Monique, Thibaut Gentina, Elodie Gentina, Renaud Tamisier, Jean-Louis Pépin, and Sébastien Bailly. 2020. "Multidimensional Evaluation of Continuous Positive Airway Pressure (CPAP) Treatment for Sleep Apnea in Different Clusters of Couples" Journal of Clinical Medicine 9, no. 6: 1658. https://doi.org/10.3390/jcm9061658
APA StyleMendelson, M., Gentina, T., Gentina, E., Tamisier, R., Pépin, J.-L., & Bailly, S. (2020). Multidimensional Evaluation of Continuous Positive Airway Pressure (CPAP) Treatment for Sleep Apnea in Different Clusters of Couples. Journal of Clinical Medicine, 9(6), 1658. https://doi.org/10.3390/jcm9061658






