Total Hip Arthroplasty Using Imageless Computer-Assisted Navigation—2-Year Follow-Up of a Prospective Randomized Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Patients
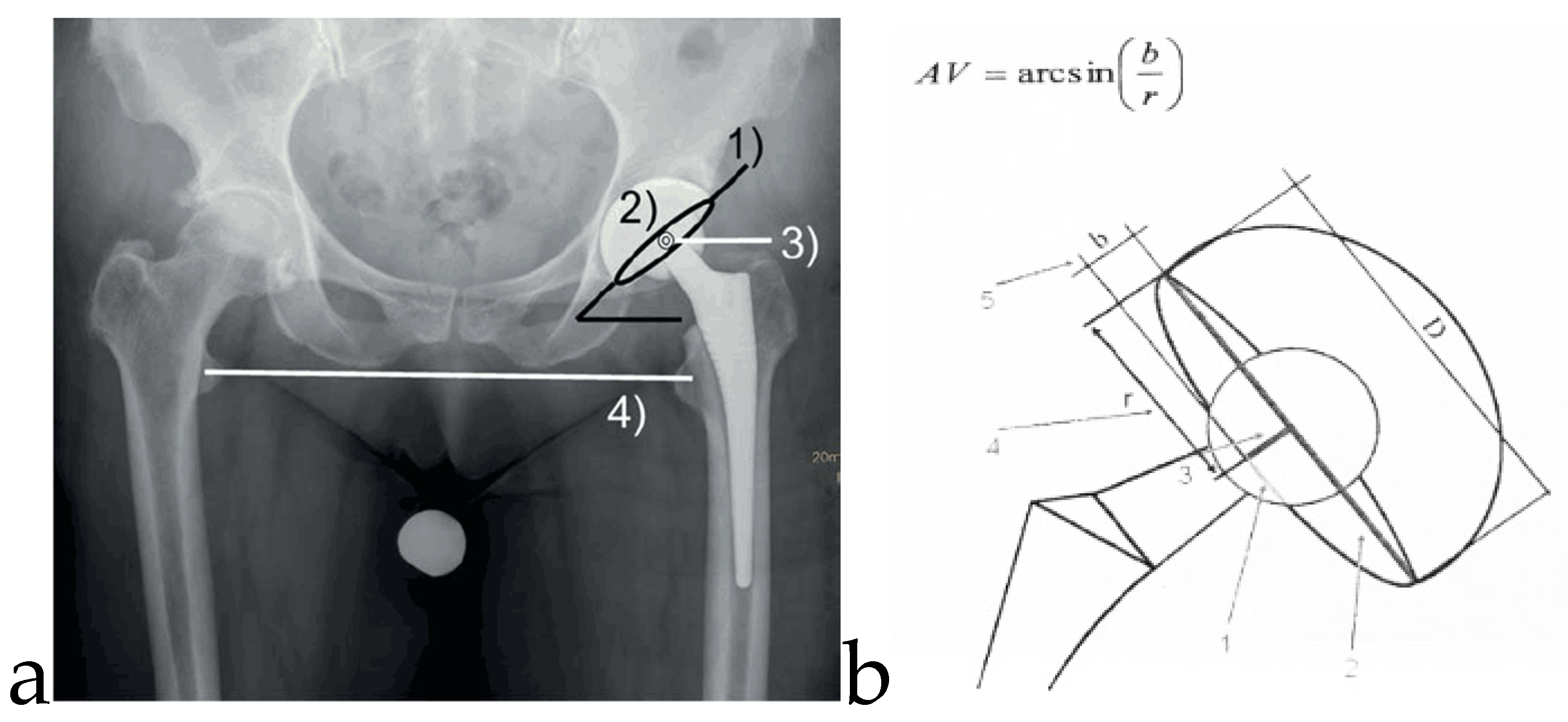
2.2. Study Parameters
2.3. Statistical Analysis
3. Results
3.1. Demographic Data
3.2. Revisions
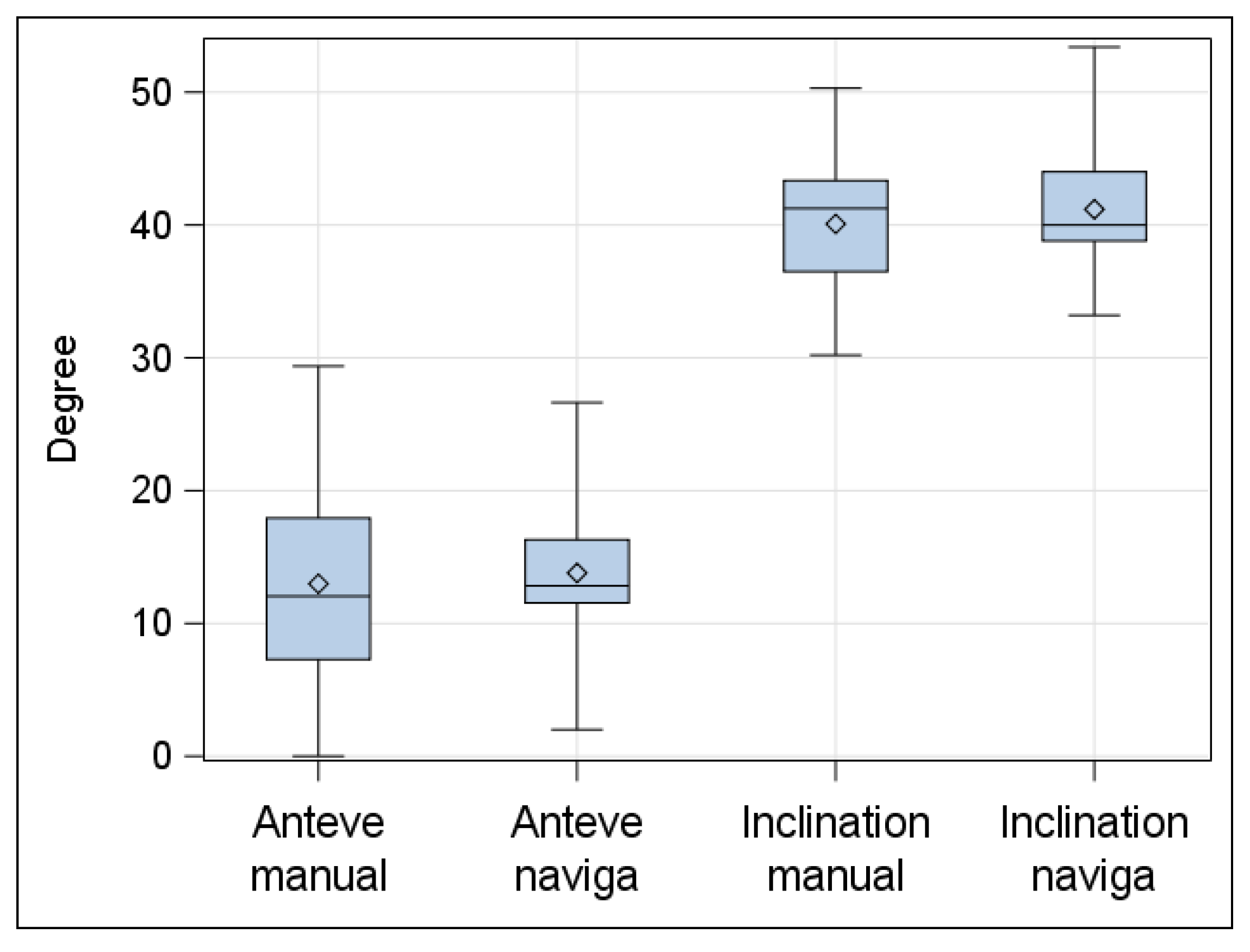
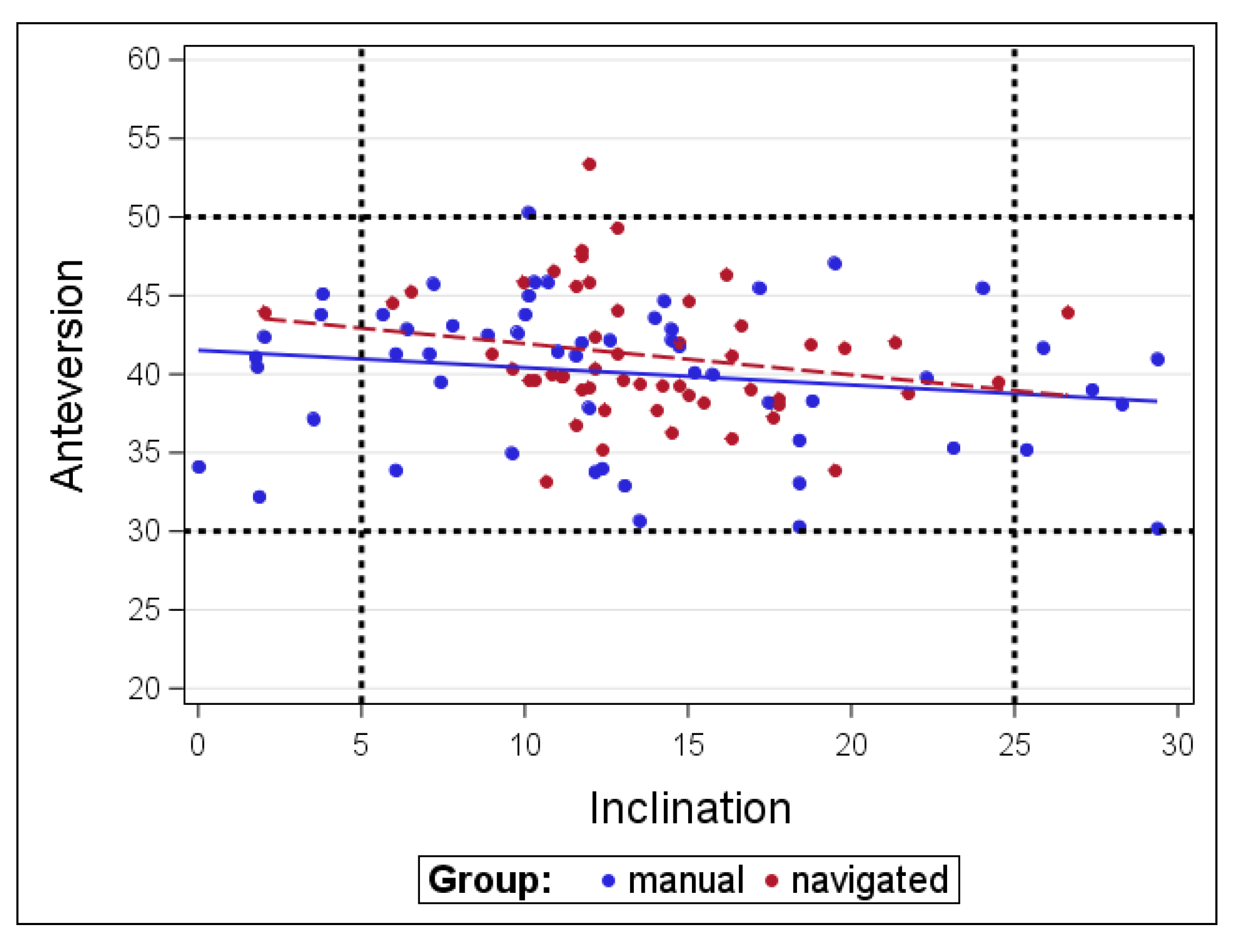
3.3. Radiological Results
3.4. Clinical Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Kennedy, J.G.; Rogers, W.B.; Soffe, K.E.; Sullivan, R.J.; Griffen, D.G.; Sheehan, L.J. Effect of acetabular component orientation on recurrent dislocation, pelvic osteolysis, polyethylene wear and component migration. J. Arthroplast. 1998, 13, 530–534. [Google Scholar] [CrossRef]
- Del Schutte, H., Jr.; Lipman, A.J.; Bannar, S.M.; Livemore, J.T.; Ilstrup, D.; Morrey, B.F. Effects of acetabular abduction on cup wear rates in total hip arthroplasty. J. Arthroplast. 1998, 13, 621–626. [Google Scholar] [CrossRef]
- D’Lima, D.D.; Urquhart, A.G.; Buehler, K.O.; Walker, R.H.; Colwell, C.W.J.R.; La, J.C. The effect of the orientation of acetabular and femoral components on the range of motion of hip at different head-neck ratios. J. Bone Jt. Surg. Am. 2000, 82, 315–321. [Google Scholar] [CrossRef] [PubMed]
- McCollum, D.E.; Gray, W.J. Dislocation after total hip arthroplasty. Causes and preventation. Clin. Orthop. Relat. Res. 1990, 261, 159–170. [Google Scholar]
- Wolf, A.; Digioia, A.M., III; Mor, A.B.; Jaramaz, B. Cup alignment error model for total hip arthroplasty. Clin. Orthop. Relat. Res. 2005, 437, 132–137. [Google Scholar] [CrossRef] [PubMed]
- Abdel, M.P.; von Roth, P.; Jennings, M.T.; Hanssen, A.D.; Pagnano, M.W. What safe zone? The vast majority of dislocated THAs are within the Lewinnek safe zone for acetabular component position. Clin. Orthop. Relat. Res. 2016, 474, 386–391. [Google Scholar] [CrossRef] [PubMed]
- Biedermann, R.; Tonin, A.; Krismer, M.; Rachbauer, F.; Eibl, G.; Stockl, B. Reducing the risk of dislocation after total hip arthroplasty: the effect of orientation on the acetabular component. J. Bone Jt. Surg. Br. 2005, 87, 762–769. [Google Scholar] [CrossRef]
- Banaszkiewicz, P.A. Radiological demarcation of cemented sockets in total hip replacement. In Classic Papers in Orthopaedics; Banaszkiewicz, P., Kader, D., Eds.; Springer: London, UK, 2014; pp. 39–41. [Google Scholar]
- Digioia, A.M., 3rd; Jaramaz, B.; Plakseychuk, A.Y.; Moody, J.E., Jr.; Nikou, C.; Labarca, R.S.; Levison, T.J.; Picard, F. Comparison of a mechanical acetabular alignment guide with computer placement of the socket. J. Arthroplast. 2002, 17, 359–364. [Google Scholar] [CrossRef]
- Lewinnek, G.E.; Lewis, J.L.; Tarr, R.; Compere, C.L.; Zimmermann, J.R. Dislocations after total hip-replacement arthroplasties. J. Bone Jt. Surg. Am. 1978, 60, 217–220. [Google Scholar] [CrossRef]
- Digioia, A.M., III; Plakseychuk, A.Y.; Levison, T.J.; Jaramaz, B. Mini-incision technique for total hip arthroplasty with navigation. J. Arthroplast. 2003, 18, 123–128. [Google Scholar] [CrossRef]
- Massin, P.; Schmidt, L.; Engh, C.A. Evaluation of cementless acetabular component migration. An experimental study. J. Arthroplast. 1989, 4, 245–251. [Google Scholar] [CrossRef]
- Ware, J., Jr.; Kosinski, M.; Keller, S.D. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med. Car. 1996, 43, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Kalteis, T.; Handel, M.; Bathis, H.; Perlick, L.; Tingart, M.; Grifka, J. Imageless navigation for insertion of the acetabular component in total hip arthroplasty: Is it as accurate as CT-based navigation? J. Bone Jt. Surg. Br. 2006, 88, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Hohmann, E.; Bryant, A.; Tetsworth, K. A comparison between imageless navigated and manual freehand technique acetabular cup placement in total hip arthroplasty. J. Arthroplast. 2011, 26, 1078–1082. [Google Scholar] [CrossRef]
- Kumar, M.A.; Shetty, M.S.; Kiran, K.G.; Kini, A.R. Validation of navigation assisted cup placement in total hip arthrosplasty. Int. Orthop. 2012, 36, 17–22. [Google Scholar] [CrossRef][Green Version]
- Moskal, J.T.; Capps, S.G. Acetabular component positioning in total hip arthroplasty: An evidence-based analysis. J. Arthroplast. 2011, 26, 1432–1437. [Google Scholar] [CrossRef]
- Reininga, I.H.; Zijlstra, W.; Wagenmarkers, R.; Boerboom, A.L.; Huijbers, B.P.; Groothoff, J.W.; Bulstra, S.K.; Stevens, M. Minimally invasive and computer-navigated total hip arthroplasty: A qualitative and systematic review of the literature. BMC Musculoskelet. Disord. 2010, 11, 92. [Google Scholar] [CrossRef]
- Bauer, R.; Kerschbaumer, F.; Poisel, S.; Oberthaler, W. The transgluteal approach to the hip joint. Arch. Orthop. Trauma. Surg. 1979, 95, 47–49. [Google Scholar] [CrossRef]
- Lass, R.; Kubista, B.; Olischar, B.; Frantal, S.; Windhager, R.; Giurea, A. Total hip arthroplasty using imageless computer-assisted hip navigation—A prospectiv randomized study. J. Arthroplast. 2014, 29, 786–791. [Google Scholar] [CrossRef]
- Roos, E.M.; Roos, H.P.; Lohmander, L.S.; Ekdahl, C.; Beynnon, B.D. Knee Injury and Osteoarthritis Outcome Score (KOOS)—Development of a self-administered outcome measure. J. Orthop. Sports Phys. Ther. 1998, 28, 88–96. [Google Scholar] [CrossRef]
- Harris, W.H. Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J. Bone Jt. Surg. Am. 1969, 51, 737. [Google Scholar] [CrossRef] [PubMed]
- Widmer, K.H. A simplified method to determine acetabular cup anteversion from plain radiographs. J. Arthroplast. 2004, 19, 387–390. [Google Scholar] [CrossRef] [PubMed]
- Haddad, F.S.; Horriat, S. Robotic and other enhanced technologies: Are we prepared for such innovation? Bone Jt. J. 2019, 101, 1469–1471. [Google Scholar] [CrossRef] [PubMed]
- Nodzo, S.R.; Chang, C.C.; Carroll, K.M.; Barlow, B.T.; Banks, S.A.; Padgett, D.E.; Maymann, D.J.; Jerabek, S.A. Intraoperative placement of total hip arthroplasty components with robotic-arm assisted technology correlates with postoperative implant position: A CT-based study. Bone Jt. J. 2018, 100, 1303–1309. [Google Scholar] [CrossRef] [PubMed]
- Kayani, B.; Konan, S.; Tahmassebi, J.; Pietrzak, J.R.T.; Haddad, F.S. Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: a prospective cohort study. Bone Jt. J. 2018, 100, 930–937. [Google Scholar] [CrossRef] [PubMed]
- Dorr, L.D.; Malik, A.; Wan, Z.; Long, W.T.; Harris, M. Precision and bias of imageless computer navigation and surgeon estimates for acetabular component position. Clin. Orthop. Relat. Res. 2007, 465, 92–99. [Google Scholar] [PubMed]
- Kalteis, T.; Handel, M.; Herold, T.; Perlick, L.; Paetzel, C.; Grifka, J. Position of the acetabular cup—accuracy of radiographic calculation compared to CT-based measurement. Eur. J. Radiol. 2006, 58, 294–300. [Google Scholar] [CrossRef]
- Ghelman, B.; Kepler, C.K.; Lyman, S. CT outperformans radiography for determination of acetabular cup version after THA. Clin. Orthop. Relat. Res. 2009, 467, 2362–2370. [Google Scholar] [CrossRef]
- Xu, K.; Li, Y.; Zhang, H.; Wang, C.G.; Xu, Y.Q.; Li, Z.J. Computer navigation in total hip arthroplasty: A meta-analysis of randomized controlled trials. Int. J. Surg. 2014, 12, 528–533. [Google Scholar] [CrossRef]
- Gurgel, H.M.; Croci, A.T.; Cabrita, H.A.; Vicente, J.R.; Leonhardt, M.C.; Rodrigues, J.C. Acetabular component positioning in total hip arthroplasty with and without a computer-assisted system: A prospective, randomized and controlled study. J. Arthroplast. 2014, 29, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Brown, M.L.; Reed, J.D.; Drinkwater, C.J. Imageless computer-assisted versus conventional total hip arthroplasty: one surgeon’s initial experience. J. Arthroplast. 2014, 29, 1015–1020. [Google Scholar] [CrossRef] [PubMed]
- Parrette, S.; Argenson, J.N. Validation and usefulness of a computer-assisted cup-positioning system in total hip arthroplasty. A prospective, randomized, controlled study. J Bone Jt. Surg. Am. 2007, 89, 494–499. [Google Scholar] [CrossRef]
- Sotereanos, N.G.; Miller, M.C.; Smith, B.; Hube, R.; Sewecke, J.J.; Wohlrab, D. Using intraoperative pelvic landmarks for acetabular component placement in total hip arthroplasty. J. Arthroplast. Sep. 2006, 21, 832–840. [Google Scholar] [CrossRef] [PubMed]
- Parrette, S.; Ollivier, M.; Lunebourg, A.; Flecher, X.; Argenson, J.N. No benefit after THA performed with computer-assisted cup placement: 10-year results of a randomized controlled study. Clin. Orthop. Relat. Res. 2016, 474, 2085–2093. [Google Scholar] [CrossRef]
- Dorr, L.D. Letter to the Editor’s spotlight / Take 5: No benefit after THA performed with computer-assisted cup placement: 10-year results of a randomized controlled study. Clin. Orthop. Relat. Res. 2017, 475, 565–566. [Google Scholar] [CrossRef][Green Version]
- Rittmeister, M.; Callitsis, C. Factors influencing cup orientation in 500 consecutive total hip replacements. Clin. Orthop. Relat. Res. 2006, 445, 192–196. [Google Scholar]
| Type of Operation | Conventional | Navigated | |||||
|---|---|---|---|---|---|---|---|
| n (%) | Mean | Range | n (%) | Mean | Range | Significance (p) | |
| Gender; f/m | 31/25 (55/45) | 38/16 (70/30) | 0.1 | ||||
| Side; r/l | 35/21 (63/37) | 33/21 (61/39) | 0.88 | ||||
| Age (years) | 79.5 | 40–100 | 77.2 | 40–98 | 0.15 | ||
| BMI (kg/m2) | 26.0 | 18–38 | 28.70 | 20–41 | 0.94 | ||
| HHS preoperative | 35.0 | 0–65 | 32.6 | 7–86 | 0.38 | ||
| HHS postop. 6 weeks | 90.2 | 62–100 | 90.9 | 61–100 | 0.72 | ||
| HHS postop. 24 month | 92.2 | 61–100 | 88.8 | 65–100 | 0.3 | ||
| Leg length difference (mm) | 4.4 | 0–20 | 2.7 | 0–15 | 0.09 | ||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lass, R.; Olischar, B.; Kubista, B.; Waldhoer, T.; Giurea, A.; Windhager, R. Total Hip Arthroplasty Using Imageless Computer-Assisted Navigation—2-Year Follow-Up of a Prospective Randomized Study. J. Clin. Med. 2020, 9, 1620. https://doi.org/10.3390/jcm9061620
Lass R, Olischar B, Kubista B, Waldhoer T, Giurea A, Windhager R. Total Hip Arthroplasty Using Imageless Computer-Assisted Navigation—2-Year Follow-Up of a Prospective Randomized Study. Journal of Clinical Medicine. 2020; 9(6):1620. https://doi.org/10.3390/jcm9061620
Chicago/Turabian StyleLass, Richard, Boris Olischar, Bernd Kubista, Thomas Waldhoer, Alexander Giurea, and Reinhard Windhager. 2020. "Total Hip Arthroplasty Using Imageless Computer-Assisted Navigation—2-Year Follow-Up of a Prospective Randomized Study" Journal of Clinical Medicine 9, no. 6: 1620. https://doi.org/10.3390/jcm9061620
APA StyleLass, R., Olischar, B., Kubista, B., Waldhoer, T., Giurea, A., & Windhager, R. (2020). Total Hip Arthroplasty Using Imageless Computer-Assisted Navigation—2-Year Follow-Up of a Prospective Randomized Study. Journal of Clinical Medicine, 9(6), 1620. https://doi.org/10.3390/jcm9061620






