Short-Term Effects of Comprehensive Pulmonary Rehabilitation and its Maintenance in Patients with Idiopathic Pulmonary Fibrosis: A Randomized Controlled Trial
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
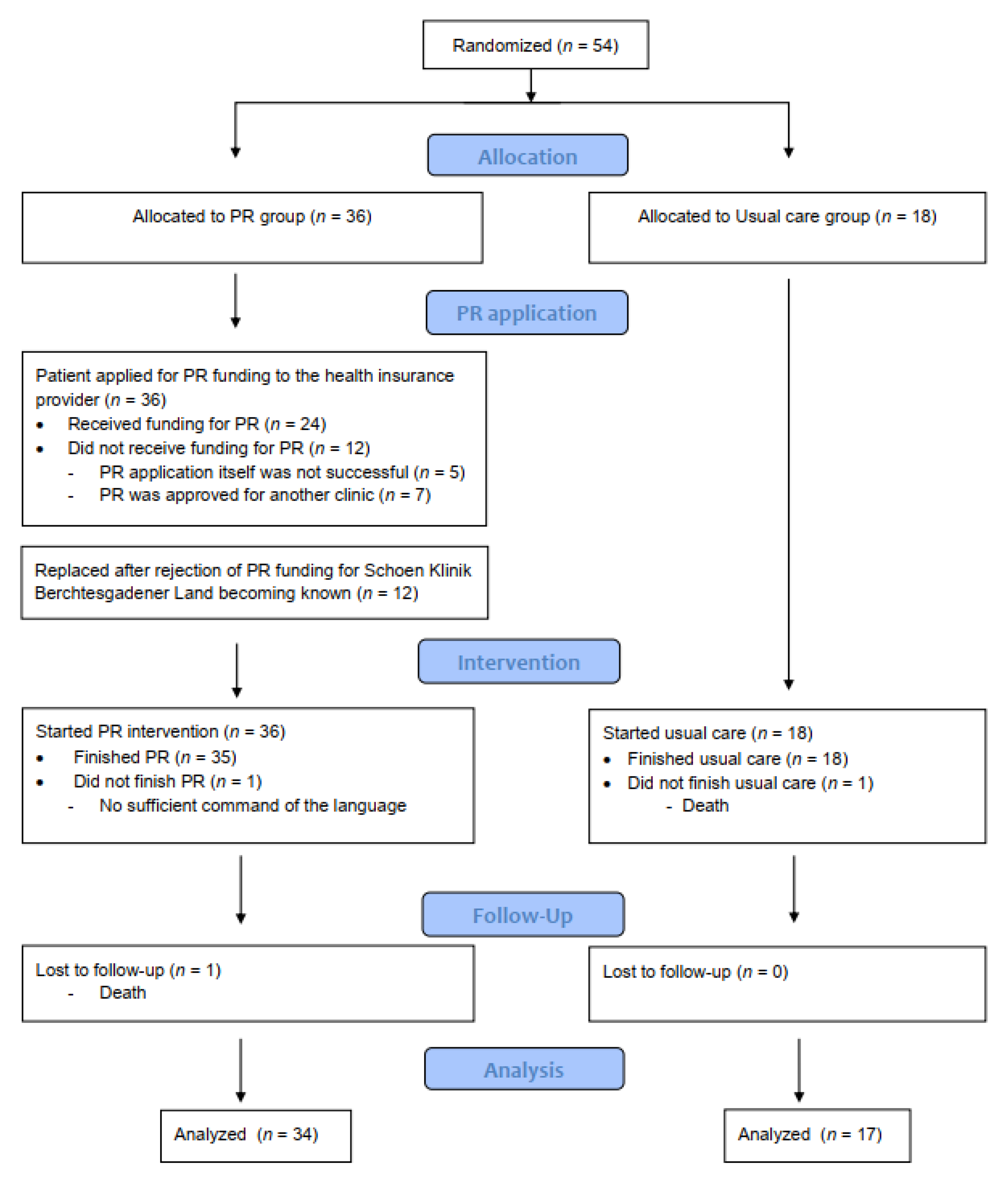
2.2. Study Design
2.3. Assessment
2.4. Statistical Methods
3. Results
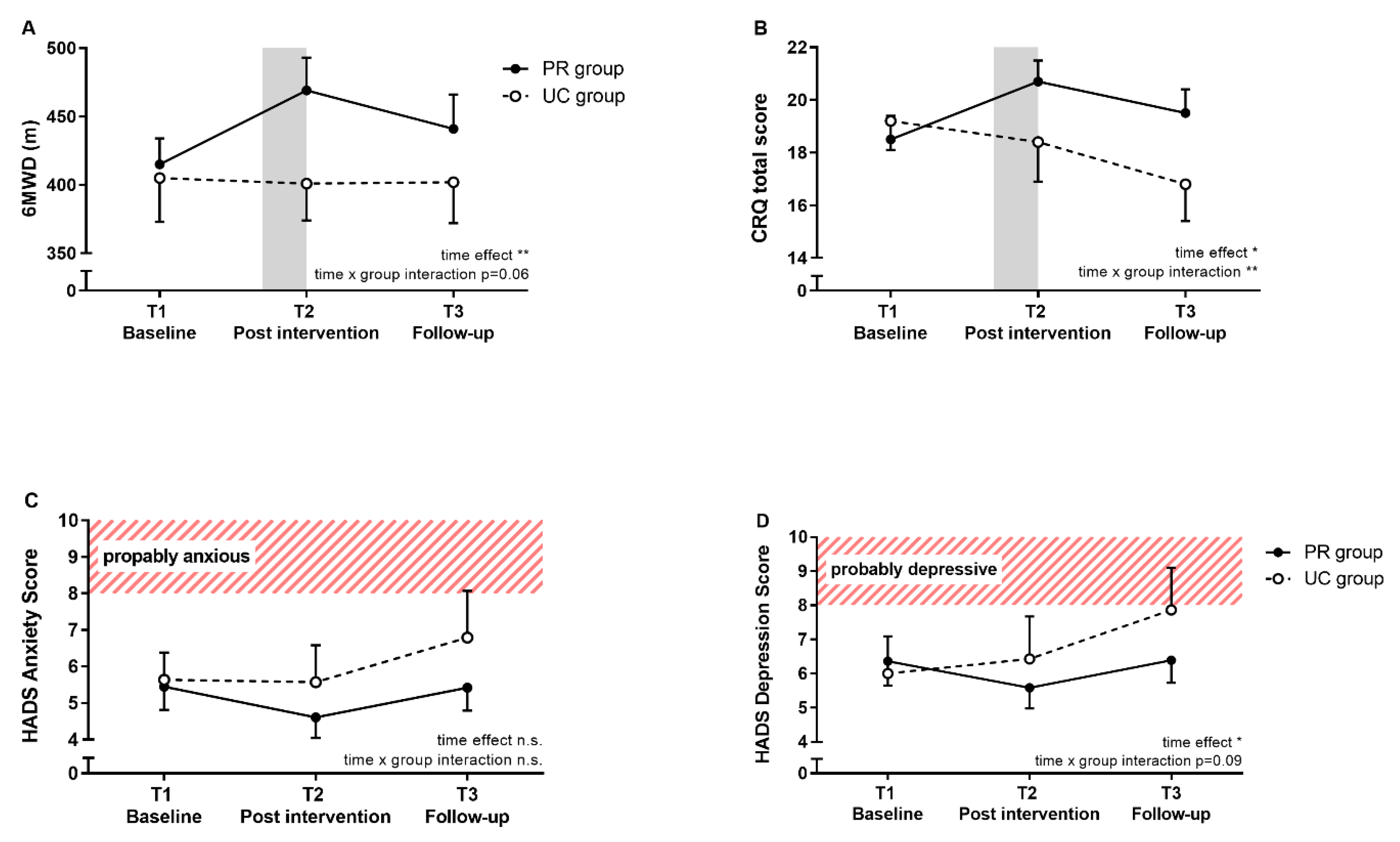
3.1. Primary Outcome
3.2. Secondary Outcomes
4. Discussion
4.1. Short-Term PR Effects
4.2. Maintenance of PR Effects
4.3. Determinants of Short-Term PR Success
4.4. Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| 6MWD | 6-min walk distance |
| 6MWT | 6-min walk test |
| ATS | American Thoracic Society |
| BMI | Body mass index |
| CRQ | Chronic Respiratory disease Questionnaire |
| DLCO | Diffusion capacity of the lung for carbon monoxide |
| ERS | European Respiratory Society |
| FEV1 | Forced expiratory volume in 1 s |
| FVC | Forced vital capacity |
| GAP index | Gender, age and physiologic variables index |
| HADS | Hospital Anxiety and Depression Scale |
| HRCT | High-resolution computed tomography |
| HRQL | Health-related quality of life |
| ILD | Interstitial lung disease |
| IPF | Idiopathic pulmonary fibrosis |
| LTOT | Long term oxygen therapy |
| PaO2 | Partial pressure of oxygen by breathing room air |
| PaCO2 | Partial pressure of carbon dioxide by breathing room air |
| PR | Pulmonary Rehabilitation |
| SF36 | Short-form 36 |
| T1 | Baseline |
| T2 | Post pulmonary rehabilitation (Pulmonary rehabilitation group) or after 9 weeks from baseline (Usual care group) |
| T3 | at 3 months follow-up |
| TLC | Total lung capacity |
| UC | Usual care. |
References
- Lederer, D.J.; Martinez, F.J. Idiopathic Pulmonary Fibrosis. N. Engl. J. Med. 2018, 378, 1811–1823. [Google Scholar] [CrossRef]
- Raghu, G.; Collard, H.R.; Egan, J.J.; Martinez, F.J.; Behr, J.; Brown, K.K.; Lynch, D.A. An official ATS/ERS/JRS/ALAT statement: Idiopathic pulmonary fibrosis: Evidence-based guidelines for diagnosis and management. Am. J. Respir. Crit. Care Med. 2011, 183, 788–824. [Google Scholar] [CrossRef]
- Kreuter, M.; Swigris, J.; Pittrow, D.; Geier, S.; Klotsche, J.; Prasse, A.; Grohé, C. The clinical course of idiopathic pulmonary fibrosis and its association to quality of life over time: Longitudinal data from the INSIGHTS-IPF registry. Respir. Res. 2019, 20, 59. [Google Scholar] [CrossRef] [PubMed]
- Bahmer, T.; Kirsten, A.M.; Waschki, B.; Rabe, K.F.; Magnussen, H.; Kirsten, D.; Watz, H. Prognosis and longitudinal changes of physical activity in idiopathic pulmonary fibrosis. BMC Pulm. Med. 2017, 17, 104. [Google Scholar] [CrossRef] [PubMed]
- Spruit, M.A.; Singh, S.J.; Garvey, C.; ZuWallack, R.; Nici, L.; Rochester, C.; Pitta, F. An official American Thoracic Society/European Respiratory Society statement: Key concepts and advances in pulmonary rehabilitation. Am. J. Respir. Crit. Care Med. 2013, 188, e13–e64. [Google Scholar] [CrossRef] [PubMed]
- Dowman, L.; Hill, C.J.; Holland, A.E. Pulmonary rehabilitation for interstitial lung disease. Cochrane Database Syst. Rev. 2014, 10, CD006322. [Google Scholar] [CrossRef]
- Huppmann, P.; Sczepanski, B.; Boensch, M.; Winterkamp, S.; Schönheit-Kenn, U.; Neurohr, C.; Kenn, K. Effects of inpatient pulmonary rehabilitation in patients with interstitial lung disease. Eur. Respir. J. 2013, 42, 444–453. [Google Scholar] [CrossRef]
- Holland, A.E.; Hill, C.J.; Conron, M.; Munro, P.; McDonald, C.F. Short term improvement in exercise capacity and symptoms following exercise training in interstitial lung disease. Thorax 2008, 63, 549–554. [Google Scholar] [CrossRef]
- Dowman, L.M.; McDonald, C.F.; Hill, C.J.; Lee, A.L.; Barker, K.; Boote, C.; Gillies, R. The evidence of benefits of exercise training in interstitial lung disease: A randomised controlled trial. Thorax 2017, 72, 610–619. [Google Scholar] [CrossRef]
- Perez-Bogerd, S.; Wuyts, W.; Barbier, V.; Demeyer, H.; Van Muylem, A.; Janssens, W.; Troosters, T. Short and long-term effects of pulmonary rehabilitation in interstitial lung diseases: A randomised controlled trial. Respir Res 2018, 19, 182. [Google Scholar] [CrossRef]
- Sharp, C.; McCabe, M.; Hussain, M.J.; Dodd, J.W.; Lamb, H.; Adamali, H.; Smith, D. Duration of benefit following completion of pulmonary rehabilitation in interstitial lung disease-an observational study. QJM Mon. J. Assoc. Phys. 2017, 110, 17–22. [Google Scholar] [CrossRef] [PubMed]
- Holland, A.E.; Hill , C.J.; Glaspole , I.; Goh , N.; McDonald , C.F. Predictors of benefit following pulmonary rehabilitation for interstitial lung disease. Respir. Med. 2012, 106, 429–435. [Google Scholar] [CrossRef] [PubMed]
- Gloeckl, R.; Heinzelmann, I.; Baeuerle, S.; Damm, E.; Schwedhelm, A.L.; Diril, M.; Kenn, K. Effects of whole body vibration in patients with chronic obstructive pulmonary disease—A randomized controlled trial. Respir. Med. 2012, 106, 75–83. [Google Scholar] [CrossRef]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef] [PubMed]
- Kim, E.S.; Choi, S.M.; Lee, J.; Park, Y.S.; Lee, C.H.; Yim, J.J.; Lee, S.M. Validation of the GAP score in Korean patients with idiopathic pulmonary fibrosis. Chest 2015, 147, 430–437. [Google Scholar] [CrossRef] [PubMed]
- Ley, B.; Ryerson, C.J.; Vittinghoff, E.; Ryu, J.H.; Tomassetti, S.; Lee, J.S.; King, T.E. A multidimensional index and staging system for idiopathic pulmonary fibrosis. Ann. Intern. Med. 2012, 156, 684–691. [Google Scholar] [CrossRef]
- Singh, S.J.; Puhan, M.A.; Andrianopoulos, V.; Hernandes, N.A.; Mitchell, K.E.; Hill, C.J.; Carlin, B.W. An official systematic review of the European Respiratory Society/American Thoracic Society: Measurement properties of field walking tests in chronic respiratory disease. Eur. Respir. J. 2014, 44, 1447–1478. [Google Scholar] [CrossRef]
- Puhan, M.A.; Frey, M.; Büchi, S.; Schünemann, H.J. The minimal important difference of the hospital anxiety and depression scale in patients with chronic obstructive pulmonary disease. Health Qual. Life Outcomes 2008, 6, 46. [Google Scholar] [CrossRef]
- Arizono, S.; Taniguchi, H.; Sakamoto, K.; Kondoh, Y.; Kimura, T.; Kataoka, K.; Kozu, R. Endurance time is the most responsive exercise measurement in idiopathic pulmonary fibrosis. Respir. Care 2014, 59, 1108–1115. [Google Scholar] [CrossRef]
- Vainshelboim, B.; Oliveira, J.; Fox, B.D.; Soreck, Y.; Fruchter, O.; Kramer, M.R. Long-term effects of a 12-week exercise training program on clinical outcomes in idiopathic pulmonary fibrosis. Lung 2015, 193, 345–354. [Google Scholar] [CrossRef]
- Ryerson, C.J.; Cayou, C.; Topp, F.; Hilling, L.; Camp, P.G.; Wilcox, P.G.; Garvey, C. Pulmonary rehabilitation improves long-term outcomes in interstitial lung disease: A prospective cohort study. Respir. Med. 2014, 108, 203–210. [Google Scholar] [CrossRef] [PubMed]
- Holland, A.E.; Spruit, M.A.; Troosters, T.; Puhan, M.A.; Pepin, V.; Saey, D.; Wanger, J. An official European Respiratory Society/American Thoracic Society technical standard: Field walking tests in chronic respiratory disease. Eur. Respir. J. 2014, 44, 1428–1446. [Google Scholar] [CrossRef] [PubMed]
- Mesquita, R.; Vanfleteren, L.E.; Franssen, F.M.; Sarv, J.; Taib, Z.; Groenen, M.T.; Spruit, M.A. Objectively identified comorbidities in COPD: Impact on pulmonary rehabilitation outcomes. Eur. Respir. J. 2015, 46, 545–548. [Google Scholar] [CrossRef] [PubMed]
- Janssens, T.; De Peuter, S.; Stans, L.; Verleden, G.; Troosters, T.; Decramer, M.; Van den Bergh, O. Dyspnea perception in COPD: Association between anxiety, dyspnea-related fear, and dyspnea in a pulmonary rehabilitation program. Chest 2011, 140, 618–625. [Google Scholar] [CrossRef]
- Maurer, J.; Rebbapragada, V.; Borson, S.; Goldstein, R.; Kunik, M.E.; Yohannes, A.M.; Hanania, N.A. Anxiety and depression in COPD: Current understanding, unanswered questions, and research needs. Chest 2008, 134 (Suppl. 4), 43S–56S. [Google Scholar] [CrossRef]
- Zhou, Y.H.; Mak, Y.W. Psycho-Physiological Associates of Dyspnea in Hospitalized Patients with Interstitial Lung Diseases: A Cross-Sectional Study. Int. J. Environ. Res. Public Health 2017, 14, 1277. [Google Scholar] [CrossRef]
| UC Group (n = 17) | PR Group (n = 34) | |
|---|---|---|
| Gender, m (%) | 13 (81) | 25 (76) |
| Age, y | 65 (10) | 68 (9) |
| BMI, kg/m2 | 27.8 (5.1) | 27.2 (4.4) |
| FVC, % pred. | 72 (20) | 74 (19) |
| TLC, % pred. | 70 (17) | 71 (14) |
| DLCO, % pred. | 36.6 (18.8) | 44.1 (15.4) |
| PaO2, mmHg | 61.1 (15.0) | 72.8 (13.3) |
| PaCO2, mmHg | 37.5 (4.6) | 38.8 (4.1) |
| Time between T1 and T2 (days) | 65 (26) | 77 (37) |
| 6MWD, m | 405 (109) | 415 (101) |
| GAP index | ||
| Stage I, n (%) | 6 (35) | 18 (53) |
| Stage II, n (%) | 8 (47) | 11 (32) |
| Stage III, n (%) | 3 (18) | 5 (15) |
| CRQ scores | ||
| dyspnea | 4.5 (1.4) | 4.7 (1.7) |
| fatigue | 4.4 (1.1) | 4.4 (1.2) |
| emotional function | 4.7 (0.9) | 4.7 (1.2) |
| mastery | 5.0 (1.2) | 4.8 (1.5) |
| total | 18.7 (3.8) | 18.6 (5.0) |
| SF36 summary scores | ||
| physical component | 39.9 (10.0) | 41.4 (9.9) |
| mental component | 45.3 (13.3) | 44.6 (12.9) |
| HADS scores | ||
| anxiety | 5.4 (2.8) | 5.5 (3.7) |
| depression | 5.9 (3.9) | 6.4 (4.1) |
| LTOT, n | 6 (38) | 7 (22) |
| Between-Group Difference (Mean Difference (95% CI)) | p-Value | |
|---|---|---|
| CRQ total | ||
| T1 to T2 | 3.0 (0.7–5.3) | 0.011 |
| T1 to T3 | 3.5 (1.5–5.4) | 0.001 |
| CRQ dyspnea | ||
| T1 to T2 | 0.9 (0.2–1.6) | 0.013 |
| T1 to T3 | 1.3 (0.5–2.1) | 0.002 |
| CRQ fatigue | ||
| T1 to T2 | 0.7 (0.0–1.4) | 0.059 |
| T1 to T3 | 0.7 (0.2–1.1) | 0.003 |
| CRQ emotional function | ||
| T1 to T2 | 0.8 (0.2–1.4) | 0.008 |
| T1 to T3 | 0.7 (0.2–1.2) | 0.009 |
| CRQ mastery | ||
| T1 to T2 | 0.6 (0.1–1.1) | 0.019 |
| T1 to T3 | 0.8 (0.1–1.4) | 0.018 |
| SF-36 physical component summary score | ||
| T1 to T2 | 2.8 (1.6–7.2) | 0.213 |
| T1 to T3 | 2.1 (4.3–8.6) | 0.504 |
| SF-36 mental component summary score | ||
| T1 to T2 | 7.1 (1.9–12.3) | 0.008 |
| T1 to T3 | 6.1 (–3.9–16) | 0.222 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jarosch, I.; Schneeberger, T.; Gloeckl, R.; Kreuter, M.; Frankenberger, M.; Neurohr, C.; Prasse, A.; Freise, J.; Behr, J.; Hitzl, W.; et al. Short-Term Effects of Comprehensive Pulmonary Rehabilitation and its Maintenance in Patients with Idiopathic Pulmonary Fibrosis: A Randomized Controlled Trial. J. Clin. Med. 2020, 9, 1567. https://doi.org/10.3390/jcm9051567
Jarosch I, Schneeberger T, Gloeckl R, Kreuter M, Frankenberger M, Neurohr C, Prasse A, Freise J, Behr J, Hitzl W, et al. Short-Term Effects of Comprehensive Pulmonary Rehabilitation and its Maintenance in Patients with Idiopathic Pulmonary Fibrosis: A Randomized Controlled Trial. Journal of Clinical Medicine. 2020; 9(5):1567. https://doi.org/10.3390/jcm9051567
Chicago/Turabian StyleJarosch, Inga, Tessa Schneeberger, Rainer Gloeckl, Michael Kreuter, Marion Frankenberger, Claus Neurohr, Antje Prasse, Julia Freise, Juergen Behr, Wolfgang Hitzl, and et al. 2020. "Short-Term Effects of Comprehensive Pulmonary Rehabilitation and its Maintenance in Patients with Idiopathic Pulmonary Fibrosis: A Randomized Controlled Trial" Journal of Clinical Medicine 9, no. 5: 1567. https://doi.org/10.3390/jcm9051567
APA StyleJarosch, I., Schneeberger, T., Gloeckl, R., Kreuter, M., Frankenberger, M., Neurohr, C., Prasse, A., Freise, J., Behr, J., Hitzl, W., Koczulla, A. R., & Kenn, K. (2020). Short-Term Effects of Comprehensive Pulmonary Rehabilitation and its Maintenance in Patients with Idiopathic Pulmonary Fibrosis: A Randomized Controlled Trial. Journal of Clinical Medicine, 9(5), 1567. https://doi.org/10.3390/jcm9051567






