Impact of Aging on the Accuracy of 3D-Printed Dental Models: An In Vitro Investigation
Abstract
1. Introduction
2. Experimental Section
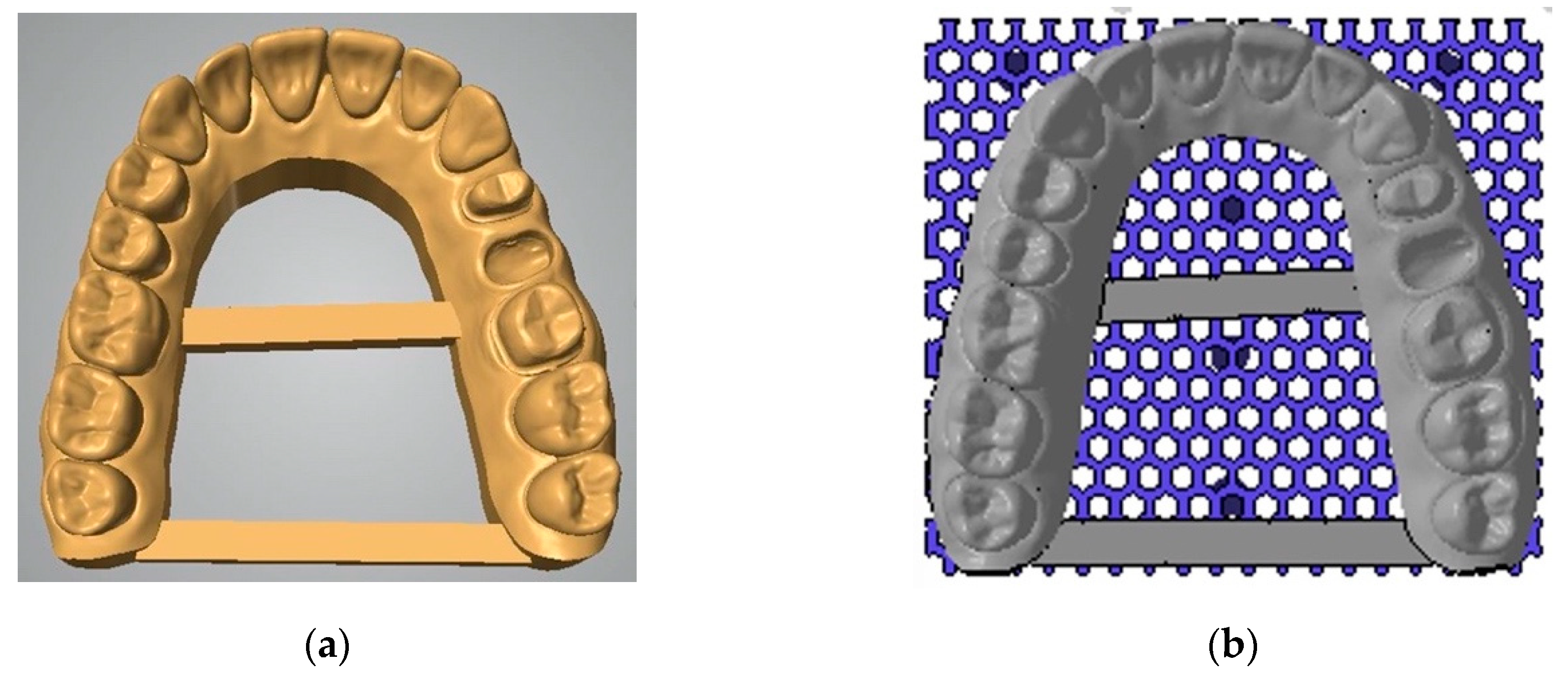
2.1. Study Setup
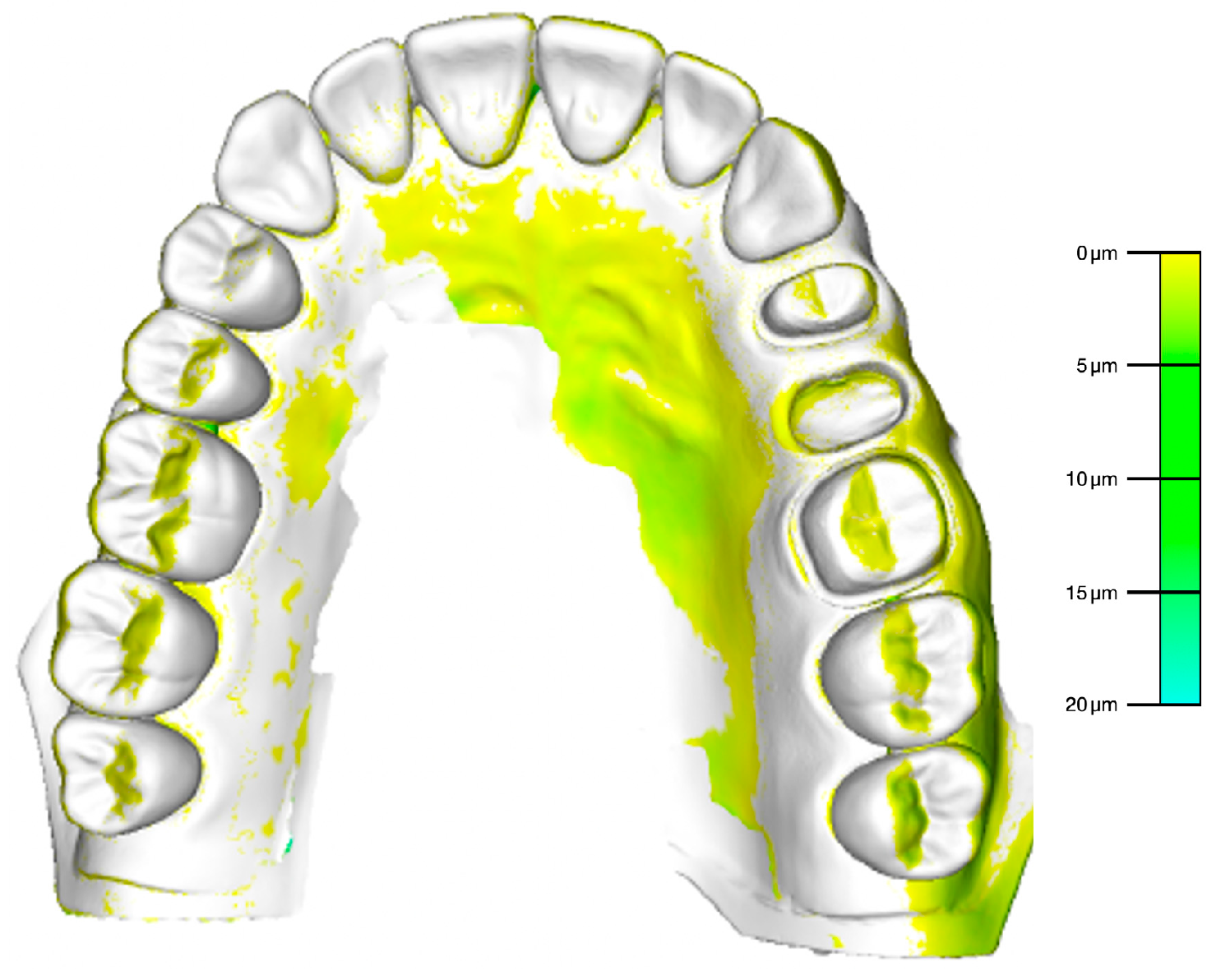
2.2. Accuracy Analysis
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Chiu, A.; Chen, Y.W.; Hayashi, J.; Sadr, A. Accuracy of CAD/CAM Digital Impressions with Different Intraoral Scanner Parameters. Sensors 2020, 20, 1157. [Google Scholar] [CrossRef] [PubMed]
- Joda, T.; Bornstein, M.M.; Jung, R.E.; Ferrari, M.; Waltimo, T.; Zitzmann, N.U. Recent Trends and Future Direction of Dental Research in the Digital Era. Int. J. Environ. Res. Public Health 2020, 17, 1987. [Google Scholar] [CrossRef] [PubMed]
- Blatz, M.B.; Conejo, J. The Current State of Chairside Digital Dentistry and Materials. Dent. Clin. N. Am. 2019, 63, 175–197. [Google Scholar] [CrossRef] [PubMed]
- Joda, T.; Bragger, U. Patient-centered outcomes comparing digital and conventional implant impression procedures: A randomized crossover trial. Clin. Oral Implant. Res. 2016, 27, e185–e189. [Google Scholar] [CrossRef]
- Guo, D.N.; Liu, Y.S.; Pan, S.X.; Wang, P.F.; Wang, B.; Liu, J.Z.; Gao, W.H.; Zhou, Y.S. Clinical Efficiency and Patient Preference of Immediate Digital Impression after Implant Placement for Single Implant-Supported Crown. Chin. J. Dent. Res. 2019, 22, 21–28. [Google Scholar]
- Joda, T.; Zarone, F.; Ferrari, M. The complete digital workflow in fixed prosthodontics: A systematic review. BMC Oral Health 2017, 17, 124. [Google Scholar] [CrossRef]
- Joda, T.; Bragger, U. Time-efficiency analysis of the treatment with monolithic implant crowns in a digital workflow: A randomized controlled trial. Clin. Oral Implant. Res. 2016, 27, 1401–1406. [Google Scholar] [CrossRef]
- Joda, T.; Ferrari, M.; Bragger, U. Monolithic implant-supported lithium disilicate (LS2) crowns in a complete digital workflow: A prospective clinical trial with a 2-year follow-up. Clin. Implant Dent. Relat. Res. 2017, 19, 505–511. [Google Scholar] [CrossRef]
- Joda, T.; Bragger, U. Time-Efficiency Analysis Comparing Digital and Conventional Workflows for Implant Crowns: A Prospective Clinical Crossover Trial. Int. J. Oral Maxillofac. Implant. 2015, 30, 1047–1053. [Google Scholar] [CrossRef]
- Joda, T.; Bragger, U. Digital vs. conventional implant prosthetic workflows: A cost/time analysis. Clin. Oral Implant. Res. 2015, 26, 1430–1435. [Google Scholar] [CrossRef]
- Almufleh, B.; Emami, E.; Alageel, O.; de Melo, F.; Seng, F.; Caron, E.; Nader, S.A.; Al-Hashedi, A.; Albuquerque, R.; Feine, J.; et al. Patient satisfaction with laser-sintered removable partial dentures: A crossover pilot clinical trial. J. Prosthet. Dent. 2018, 119, 560–567. [Google Scholar] [CrossRef] [PubMed]
- Gintaute, A.; Straface, A.; Zitzmann, N.U.; Joda, T. Removable Dental Prosthesis 2.0: Digital from A to Z? Swiss Dent. J. 2020, 130, 229–235. [Google Scholar] [PubMed]
- Joda, T.; Ferrari, M.; Gallucci, G.O.; Wittneben, J.G.; Bragger, U. Digital technology in fixed implant prosthodontics. Periodontology 2000 2017, 73, 178–192. [Google Scholar] [CrossRef] [PubMed]
- Alharbi, N.; Wismeijer, D.; Osman, R.B. Additive Manufacturing Techniques in Prosthodontics: Where Do We Currently Stand? A Critical Review. Int. J. Prosthodont. 2017, 30, 474–484. [Google Scholar] [CrossRef]
- Quan, H.; Zhang, T.; Xu, H.; Luo, S.; Nie, J.; Zhu, X. Photo-curing 3D printing technique and its challenges. Bioact. Mater. 2020, 5, 110–115. [Google Scholar] [CrossRef]
- Hazeveld, A.; Huddleston Slater, J.J.; Ren, Y. Accuracy and reproducibility of dental replica models reconstructed by different rapid prototyping techniques. Am. J. Orthod. Dentofac. Orthop. 2014, 145, 108–115. [Google Scholar] [CrossRef]
- Jeong, Y.G.; Lee, W.S.; Lee, K.B. Accuracy evaluation of dental models manufactured by CAD/CAM milling method and 3D printing method. J. Adv. Prosthodont. 2018, 10, 245–251. [Google Scholar] [CrossRef]
- Zhang, Z.C.; Li, P.L.; Chu, F.T.; Shen, G. Influence of the three-dimensional printing technique and printing layer thickness on model accuracy. J. Orofac. Orthop. 2019, 80, 194–204. [Google Scholar] [CrossRef]
- Nestler, N.; Wesemann, C.; Spies, B.C.; Beuer, F.; Bumann, A. Dimensional accuracy of extrusion- and photopolymerization-based 3D printers: In vitro study comparing printed casts. J. Prosthet. Dent. 2020. [Google Scholar] [CrossRef]
- Rungrojwittayakul, O.; Kan, J.Y.; Shiozaki, K.; Swamidass, R.S.; Goodacre, B.J.; Goodacre, C.J.; Lozada, J.L. Accuracy of 3D Printed Models Created by Two Technologies of Printers with Different Designs of Model Base. J. Prosthodont. 2020, 29, 124–128. [Google Scholar] [CrossRef]
- Sim, J.Y.; Jang, Y.; Kim, W.C.; Kim, H.Y.; Lee, D.H.; Kim, J.H. Comparing the accuracy (trueness and precision) of models of fixed dental prostheses fabricated by digital and conventional workflows. J. Prosthodont. Res. 2019, 63, 25–30. [Google Scholar] [CrossRef] [PubMed]
- Dietrich, C.A.; Ender, A.; Baumgartner, S.; Mehl, A. A validation study of reconstructed rapid prototyping models produced by two technologies. Angle Orthod. 2017, 87, 782–787. [Google Scholar] [CrossRef] [PubMed]
- Muhlemann, S.; Benic, G.I.; Fehmer, V.; Hammerle, C.H.F.; Sailer, I. Randomized controlled clinical trial of digital and conventional workflows for the fabrication of zirconia-ceramic posterior fixed partial dentures. Part II: Time efficiency of CAD-CAM versus conventional laboratory procedures. J. Prosthet. Dent. 2019, 121, 252–257. [Google Scholar] [CrossRef] [PubMed]
- Valente Vda, S.; Zanetti, A.L.; Feltrin, P.P.; Inoue, R.T.; de Moura, C.D.; Padua, L.E. Dimensional accuracy of stone casts obtained with multiple pours into the same mold. ISRN Dent. 2012, 2012, 730674. [Google Scholar] [CrossRef][Green Version]
- Vitti, R.P.; da Silva, M.A.; Consani, R.L.; Sinhoreti, M.A. Dimensional accuracy of stone casts made from silicone-based impression materials and three impression techniques. Braz. Dent. J. 2013, 24, 498–502. [Google Scholar] [CrossRef][Green Version]
- Barazanchi, A.; Li, K.C.; Al-Amleh, B.; Lyons, K.; Waddell, J.N. Additive Technology: Update on Current Materials and Applications in Dentistry. J. Prosthodont. 2017, 26, 156–163. [Google Scholar] [CrossRef]
- Kim, S.Y.; Shin, Y.S.; Jung, H.D.; Hwang, C.J.; Baik, H.S.; Cha, J.Y. Precision and trueness of dental models manufactured with different 3-dimensional printing techniques. Am. J. Orthod. Dentofac. Orthop. 2018, 153, 144–153. [Google Scholar] [CrossRef]
- Jockusch, J.; Ozcan, M. Additive manufacturing of dental polymers: An overview on processes, materials and applications. Dent. Mater. J. 2020. [Google Scholar] [CrossRef]

| 1 Day | 1 Week | 2 Weeks | 3 Weeks | 4 Weeks | |
|---|---|---|---|---|---|
| #01 | 2 | 2 | 3 | 5 | 6 |
| #02 | 1 | 2 | 2 | 3 | 5 |
| #03 | 2 | 3 | 2 | 7 | 8 |
| #04 | 2 | 2 | 3 | 4 | 9 |
| #05 | 4 | 3 | 6 | 6 | 9 |
| #06 | 4 | 6 | 5 | 7 | 10 |
| #07 | 5 | 7 | 6 | 8 | 12 |
| #08 | 5 | 5 | 7 | 7 | 9 |
| #09 | 3 | 4 | 7 | 8 | 9 |
| #10 | 5 | 6 | 8 | 9 | 12 |
| Mean | 3.3 | 4.0 | 4.9 | 6.4 | 8.9 |
| SD | 1.3 | 1.9 | 2.2 | 1.9 | 2.2 |
| Min | 1 | 2 | 2 | 3 | 5 |
| Max | 5 | 7 | 8 | 9 | 12 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Joda, T.; Matthisson, L.; Zitzmann, N.U. Impact of Aging on the Accuracy of 3D-Printed Dental Models: An In Vitro Investigation. J. Clin. Med. 2020, 9, 1436. https://doi.org/10.3390/jcm9051436
Joda T, Matthisson L, Zitzmann NU. Impact of Aging on the Accuracy of 3D-Printed Dental Models: An In Vitro Investigation. Journal of Clinical Medicine. 2020; 9(5):1436. https://doi.org/10.3390/jcm9051436
Chicago/Turabian StyleJoda, Tim, Lea Matthisson, and Nicola U. Zitzmann. 2020. "Impact of Aging on the Accuracy of 3D-Printed Dental Models: An In Vitro Investigation" Journal of Clinical Medicine 9, no. 5: 1436. https://doi.org/10.3390/jcm9051436
APA StyleJoda, T., Matthisson, L., & Zitzmann, N. U. (2020). Impact of Aging on the Accuracy of 3D-Printed Dental Models: An In Vitro Investigation. Journal of Clinical Medicine, 9(5), 1436. https://doi.org/10.3390/jcm9051436






