Quantitative Susceptibility Mapping and Vessel Wall Imaging as Screening Tools to Detect Microbleed in Sentinel Headache
Abstract
:1. Introduction
2. Methods
2.1. Ethical Approval
2.2. Patients and Study Design
2.3. MR Acquisition
2.4. Image Analysis and Detection of the MBs and AWE
2.5. Statistical Analyses
3. Results
3.1. Patient Demographics and Characteristics of IA
3.2. Performance of QSM in Detecting SH
3.3. Performance of VWI Against SH
4. Discussion
Limitations
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Pereira, J.L.; de Albuquerque, L.A.; Dellaretti, M.; de Carvalho, G.T.; Vieira, G., Jr.; Rocha, M.I.; Loures, L.L.; Christo, P.P.; de Sousa, A.A. Importance of recognizing sentinel headache. Surg. Neurol. Int. 2012, 3, 162. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Polmear, A. Sentinel headaches in aneurysmal subarachnoid haemorrhage: What is the true incidence? A systematic review. Cephalalgia 2003, 23, 935–941. [Google Scholar] [CrossRef] [PubMed]
- Leblanc, R. The minor leak preceding subarachnoid hemorrhage. J. Neurosurg. 1987, 66, 35–39. [Google Scholar] [CrossRef] [PubMed]
- Jakobsson, K.E.; Saveland, H.; Hillman, J.; Edner, G.; Zygmunt, S.; Brandt, L.; Pellettieri, L. Warning leak and management outcome in aneurysmal subarachnoid hemorrhage. J. Neurosurg. 1996, 85, 995–999. [Google Scholar] [CrossRef] [PubMed]
- Ostergaard, J.R. Warning leak in subarachnoid haemorrhage. BMJ 1990, 301, 190–191. [Google Scholar] [CrossRef] [Green Version]
- Connolly, E.S., Jr.; Rabinstein, A.A.; Carhuapoma, J.R.; Derdeyn, C.P.; Dion, J.; Higashida, R.T.; Hoh, B.L.; Kirkness, C.J.; Naidech, A.M.; Ogilvy, C.S.; et al. Guidelines for the management of aneurysmal subarachnoid hemorrhage: A guideline for healthcare professionals from the American Heart Association/american Stroke Association. Stroke 2012, 43, 1711–1737. [Google Scholar] [CrossRef] [Green Version]
- Shah, K.H.; Richard, K.M.; Nicholas, S.; Edlow, J.A. Incidence of traumatic lumbar puncture. Acad. Emerg. Med. 2003, 10, 151–154. [Google Scholar] [CrossRef]
- Eskey, C.J.; Ogilvy, C.S. Fluoroscopy-guided lumbar puncture: Decreased frequency of traumatic tap and implications for the assessment of CT-negative acute subarachnoid hemorrhage. Am. J. Neuroradiol. 2001, 22, 571–576. [Google Scholar]
- Polanczyk, A.; Wozniak, T.; Strzelecki, M.; Szubert, W.; Strzelecki, M. Evaluating an algorithm for 3D reconstruction of blood vessels for further simulations of hemodynamic in human artery branches. In Proceedings of the 2016 Signal Processing: Algorithms, Architectures, Arrangements, and Applications (SPA), Poznan, Poland, 21–23 September 2016. [Google Scholar]
- Polanczyk, A.; Strzelecki, M.; Wozniak, T.; Szubert, W.; Stefanczyk, L. 3D Blood Vessels Reconstruction Based on Segmented CT Data for Further Simulations of Hemodynamic in Human Artery Branches. Found. Comput. Decis. Sci. 2017, 42, 13. [Google Scholar] [CrossRef] [Green Version]
- Liu, T.; Surapaneni, K.; Lou, M.; Cheng, L.; Spincemaille, P.; Wang, Y. Cerebral microbleeds: Burden assessment by using quantitative susceptibility mapping. Radiology 2012, 262, 269–278. [Google Scholar] [CrossRef] [Green Version]
- Zhang, S.; Chiang, G.C.; Knapp, J.M.; Zecca, C.M.; He, D.; Ramakrishna, R.; Magge, R.S.; Pisapia, D.J.; Fine, H.A.; Tsiouris, A.J.; et al. Grading meningiomas utilizing multiparametric MRI with inclusion of susceptibility weighted imaging and quantitative susceptibility mapping. J. Neuroradiol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Schneider, T.M.; Nagel, A.M.; Zorn, M.; Wetscherek, A.; Bendszus, M.; Ladd, M.E.; Straub, S. Quantitative susceptibility mapping and (23) Na imaging-based in vitro characterization of blood clotting kinetics. NMR Biomed. 2018, 31, e3926. [Google Scholar] [CrossRef] [PubMed]
- Girard, R.; Fam, M.D.; Zeineddine, H.A.; Tan, H.; Mikati, A.G.; Shi, C.; Jesselson, M.; Shenkar, R.; Wu, M.; Cao, Y.; et al. Vascular permeability and iron deposition biomarkers in longitudinal follow-up of cerebral cavernous malformations. J. Neurosurg. 2017, 127, 102–110. [Google Scholar] [CrossRef] [PubMed]
- Ikebe, Y.; Ishimaru, H.; Imai, H.; Abe, K.; Izumo, T.; Morofuji, Y.; Ideguchi, R.; Morikawa, M.; Uetani, M. Quantitative Susceptibility Mapping for Carotid Atherosclerotic Plaques: A Pilot Study. Magn. Reson. Med. Sci. 2019. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nakagawa, D.; Cushing, C.; Nagahama, Y.; Allan, L.; Hasan, D. Quantitative Susceptibility Mapping as a Possible Tool to Radiographically Diagnose Sentinel Headache Associated with Intracranial Aneurysm: Case Report. World Neurosurg. 2017, 103, 954.e1–954.e4. [Google Scholar] [CrossRef] [PubMed]
- Nakagawa, D.; Kudo, K.; Awe, O.; Zanaty, M.; Nagahama, Y.; Cushing, C.; Magnotta, V.; Hayakawa, M.; Allan, L.; Greenlee, J.; et al. Detection of microbleeds associated with sentinel headache using MRI quantitative susceptibility mapping: Pilot study. J. Neurosurg. 2018, 130, 1391–1397. [Google Scholar] [CrossRef] [Green Version]
- Hu, P.; Yang, Q.; Wang, D.D.; Guan, S.C.; Zhang, H.Q. Wall enhancement on high-resolution magnetic resonance imaging may predict an unsteady state of an intracranial saccular aneurysm. Neuroradiology 2016, 58, 979–985. [Google Scholar] [CrossRef]
- Edjlali, M.; Gentric, J.C.; Regent-Rodriguez, C.; Trystram, D.; Hassen, W.B.; Lion, S.; Nataf, F.; Raymond, J.; Wieben, O.; Turski, P.; et al. Does aneurysmal wall enhancement on vessel wall MRI help to distinguish stable from unstable intracranial aneurysms? Stroke 2014, 45, 3704–3706. [Google Scholar] [CrossRef] [Green Version]
- Thompson, B.G.; Brown, R.D., Jr.; Amin-Hanjani, S.; Broderick, J.P.; Cockroft, K.M.; Connolly, E.S., Jr.; Duckwiler, G.R.; Harris, C.C.; Howard, V.J.; Johnston, S.C.; et al. Guidelines for the Management of Patients With Unruptured Intracranial Aneurysms: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke 2015, 46, 2368–2400. [Google Scholar] [CrossRef] [Green Version]
- Fedorov, A.; Beichel, R.; Kalpathy-Cramer, J.; Finet, J.; Fillion-Robin, J.C.; Pujol, S.; Bauer, C.; Jennings, D.; Fennessy, F.; Sonka, M.; et al. 3D Slicer as an image computing platform for the Quantitative Imaging Network. Magn. Reson. Imaging 2012, 30, 1323–1341. [Google Scholar] [CrossRef] [Green Version]
- Tan, H.; Zhang, L.; Mikati, A.G.; Girard, R.; Khanna, O.; Fam, M.D.; Liu, T.; Wang, Y.; Edelman, R.R.; Christoforidis, G.; et al. Quantitative Susceptibility Mapping in Cerebral Cavernous Malformations: Clinical Correlations. Am. J. Neuroradiol. 2016, 37, 1209–1215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Omodaka, S.; Endo, H.; Niizuma, K.; Fujimura, M.; Endo, T.; Sato, K.; Sugiyama, S.I.; Inoue, T.; Tominaga, T. Circumferential Wall Enhancement on Magnetic Resonance Imaging is Useful to Identify Rupture Site in Patients with Multiple Cerebral Aneurysms. Neurosurgery 2018, 82, 638–644. [Google Scholar] [CrossRef] [PubMed]
- Omodaka, S.; Endo, H.; Niizuma, K.; Fujimura, M.; Inoue, T.; Endo, T.; Sato, K.; Sugiyama, S.I.; Tominaga, T. Circumferential wall enhancement in evolving intracranial aneurysms on magnetic resonance vessel wall imaging. J. Neurosurg. 2018, 131, 1262–1268. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gill, H.S.; Marcolini, E.G.; Barber, D.; Wira, C.R. The Utility of Lumbar Puncture After a Negative Head CT in the Emergency Department Evaluation of Subarachnoid Hemorrhage. Yale J. Biol. Med. 2018, 91, 3–11. [Google Scholar] [PubMed]
- Zeineddine, H.A.; Girard, R.; Cao, Y.; Hobson, N.; Fam, M.D.; Stadnik, A.; Tan, H.; Shen, J.; Chaudagar, K.; Shenkar, R.; et al. Quantitative susceptibility mapping as a monitoring biomarker in cerebral cavernous malformations with recent hemorrhage. J. Magn. Reson. Imaging 2018, 47, 1133–1138. [Google Scholar] [CrossRef]
- Ishii, D.; Matsushige, T.; Sakamoto, S.; Shimonaga, K.; Akiyama, Y.; Okazaki, T.; Oshita, J.; Kurisu, K. Decreased Antiatherogenic Protein Levels are Associated with Aneurysm Structure Alterations in MR Vessel Wall Imaging. J Stroke Cereb. Dis. 2019, 28, 2221–2227. [Google Scholar] [CrossRef]
- Edjlali, M.; Guedon, A.; Ben Hassen, W.; Boulouis, G.; Benzakoun, J.; Rodriguez-Regent, C.; Trystram, D.; Nataf, F.; Meder, J.F.; Turski, P.; et al. Circumferential Thick Enhancement at Vessel Wall MRI Has High Specificity for Intracranial Aneurysm Instability. Radiology 2018, 289, 181–187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Greving, J.P.; Wermer, M.J.; Brown, R.D., Jr.; Morita, A.; Juvela, S.; Yonekura, M.; Ishibashi, T.; Torner, J.C.; Nakayama, T.; Rinkel, G.J.; et al. Development of the PHASES score for prediction of risk of rupture of intracranial aneurysms: A pooled analysis of six prospective cohort studies. Lancet Neurol. 2014, 13, 59–66. [Google Scholar] [CrossRef]
- Signorelli, F.; Pailler-Mattei, C.; Gory, B.; Larquet, P.; Robinson, P.; Vargiolu, R.; Zahouani, H.; Labeyrie, P.E.; Guyotat, J.; Pelissou-Guyotat, I.; et al. Biomechanical Characterization of Intracranial Aneurysm Wall: A Multiscale Study. World Neurosurg. 2018, 119, e882–e889. [Google Scholar] [CrossRef]
- Matsushige, T.; Shimonaga, K.; Ishii, D.; Sakamoto, S.; Hosogai, M.; Hashimoto, Y.; Kaneko, M.; Ono, C.; Mizoue, T.; Kurisu, K. Vessel Wall Imaging of Evolving Unruptured Intracranial Aneurysms. Stroke J. Cereb. Circ. 2019, 50, 1891–1894. [Google Scholar] [CrossRef]
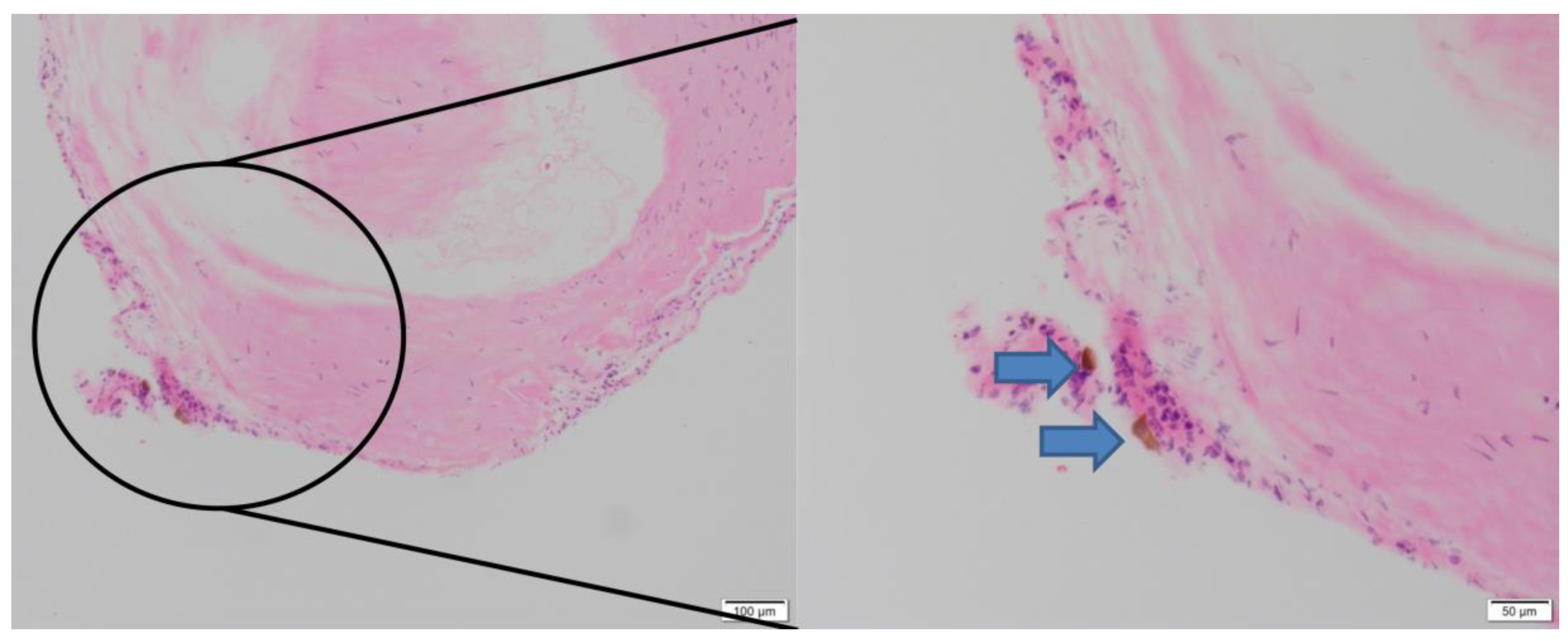
- Shimonaga, K.; Matsushige, T.; Ishii, D.; Sakamoto, S.; Hosogai, M.; Kawasumi, T.; Kaneko, M.; Ono, C.; Kurisu, K. Clinicopathological Insights From Vessel Wall Imaging of Unruptured Intracranial Aneurysms. Stroke J. Cereb. Circ. 2018, 49, 2516–2519. [Google Scholar] [CrossRef] [PubMed]
- Hudson, J.S.; Zanaty, M.; Nakagawa, D.; Kung, D.K.; Jabbour, P.; Samaniego, E.A.; Hasan, D. Magnetic Resonance Vessel Wall Imaging in Human Intracranial Aneurysms. Stroke J. Cereb. Circ. 2019, 50, e1. [Google Scholar] [CrossRef] [PubMed]
- Nagahata, S.; Nagahata, M.; Obara, M.; Kondo, R.; Minagawa, N.; Sato, S.; Sato, S.; Mouri, W.; Saito, S.; Kayama, T. Wall Enhancement of the Intracranial Aneurysms Revealed by Magnetic Resonance Vessel Wall Imaging Using Three-Dimensional Turbo Spin-Echo Sequence with Motion-Sensitized Driven-Equilibrium: A Sign of Ruptured Aneurysm? Clin. Neuroradiol. 2016, 26, 277–283. [Google Scholar] [CrossRef] [PubMed]
- Texakalidis, P.; Hilditch, C.A.; Lehman, V.; Lanzino, G.; Pereira, V.M.; Brinjikji, W. Vessel Wall Imaging of Intracranial Aneurysms: Systematic Review and Meta-analysis. World Neurosurg. 2018, 117, 453–458. [Google Scholar] [CrossRef]
- Tan, H.; Liu, T.; Wu, Y.; Thacker, J.; Shenkar, R.; Mikati, A.G.; Shi, C.; Dykstra, C.; Wang, Y.; Prasad, P.V.; et al. Evaluation of iron content in human cerebral cavernous malformation using quantitative susceptibility mapping. Investig. Radiol. 2014, 49, 498–504. [Google Scholar] [CrossRef] [PubMed]


| Characteristics | Value |
|---|---|
| Patients Age ± SD (range), years Female Sex, n (%) SH, n (%) Aneurysms ICA, n (%) | 62.4 ± 11.8 (43–85) 44 (86.3%) 11 (27.5%) 10 (19.6%) |
| ACA, n (%) MCA, n (%) Posterior circulation, n (%) Maximum diameter, mean ± SD (range) (mm) Saccular, n (%) Microbleeds, n (%) AWE, n (%) Treatments Microsurgical clipping, n (%) Endovascular procedure, n (%) Observation, n (%) | 9 (17.6%) 16 (31.4%) 16 (31.4%) 7.3 ± 5.0 (3.0–24.8) 45 (88.2%) 12 (23.5%) 22 (43.1%) 7 (13.7%) 27 (52.9%) 17 (33.3%) |
| Subjects with Presentation of Severe Headache Suggestive of SH | |||
|---|---|---|---|
| Positive | Negative | ||
| Subjects with | Positive QSM | 11 | 0 |
| Negative QSM | 0 | 29 | |
| Microbleeds Detected by QSM | |||
|---|---|---|---|
| Positive | Negative | ||
| AWE | Positive | 11 | 11 |
| Negative | 1 | 28 | |
| QSM | ||||
|---|---|---|---|---|
| Available | Unavailable | |||
| Positive | Negative | |||
| AWE | Positive | Strongly recommended | Might be considered | Might be considered |
| Negative | Strongly recommended | Conservative | Conservative | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ishii, D.; Nakagawa, D.; Zanaty, M.; Roa, J.A.; Al Kasab, S.; Shaban, A.; Hudson, J.S.; Osorno-Cruz, C.; Byer, S.; Allan, L.; et al. Quantitative Susceptibility Mapping and Vessel Wall Imaging as Screening Tools to Detect Microbleed in Sentinel Headache. J. Clin. Med. 2020, 9, 979. https://doi.org/10.3390/jcm9040979
Ishii D, Nakagawa D, Zanaty M, Roa JA, Al Kasab S, Shaban A, Hudson JS, Osorno-Cruz C, Byer S, Allan L, et al. Quantitative Susceptibility Mapping and Vessel Wall Imaging as Screening Tools to Detect Microbleed in Sentinel Headache. Journal of Clinical Medicine. 2020; 9(4):979. https://doi.org/10.3390/jcm9040979
Chicago/Turabian StyleIshii, Daizo, Daichi Nakagawa, Mario Zanaty, Jorge A. Roa, Sami Al Kasab, Amir Shaban, Joseph S. Hudson, Carlos Osorno-Cruz, Stefano Byer, Lauren Allan, and et al. 2020. "Quantitative Susceptibility Mapping and Vessel Wall Imaging as Screening Tools to Detect Microbleed in Sentinel Headache" Journal of Clinical Medicine 9, no. 4: 979. https://doi.org/10.3390/jcm9040979
APA StyleIshii, D., Nakagawa, D., Zanaty, M., Roa, J. A., Al Kasab, S., Shaban, A., Hudson, J. S., Osorno-Cruz, C., Byer, S., Allan, L., Torner, J. C., Awad, I. A., Carroll, T. J., Samaniego, E. A., & Hasan, D. M. (2020). Quantitative Susceptibility Mapping and Vessel Wall Imaging as Screening Tools to Detect Microbleed in Sentinel Headache. Journal of Clinical Medicine, 9(4), 979. https://doi.org/10.3390/jcm9040979





