The Outcome of Distal Radius Fractures with Concomitant Injuries Is Similar to those of Isolated Distal Radius Fractures Provided that an Arthroscopically Supported Treatment Is Performed
Abstract
1. Introduction
2. Methods
2.1. Ethical Approval
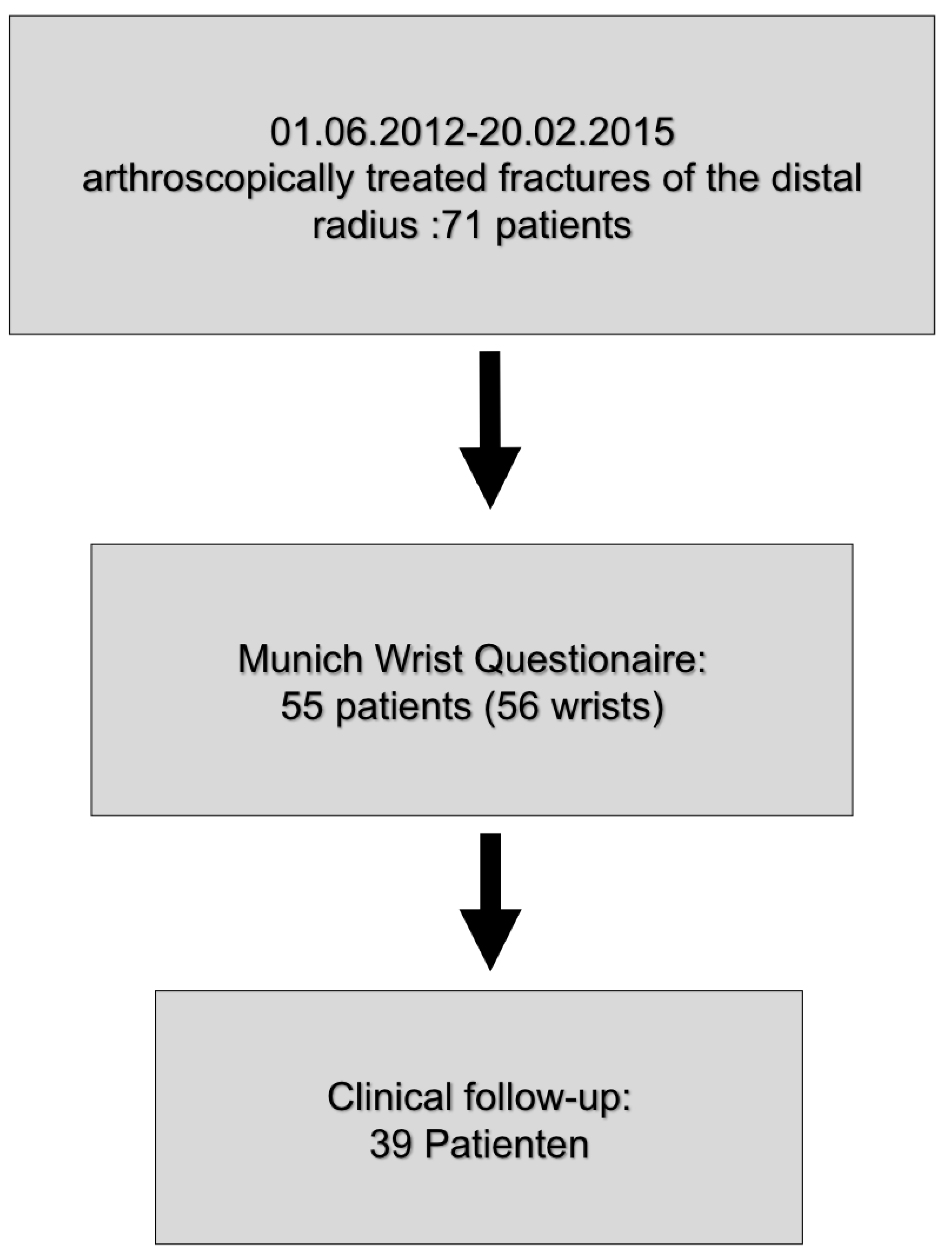
2.2. Study Population
2.3. Control Population
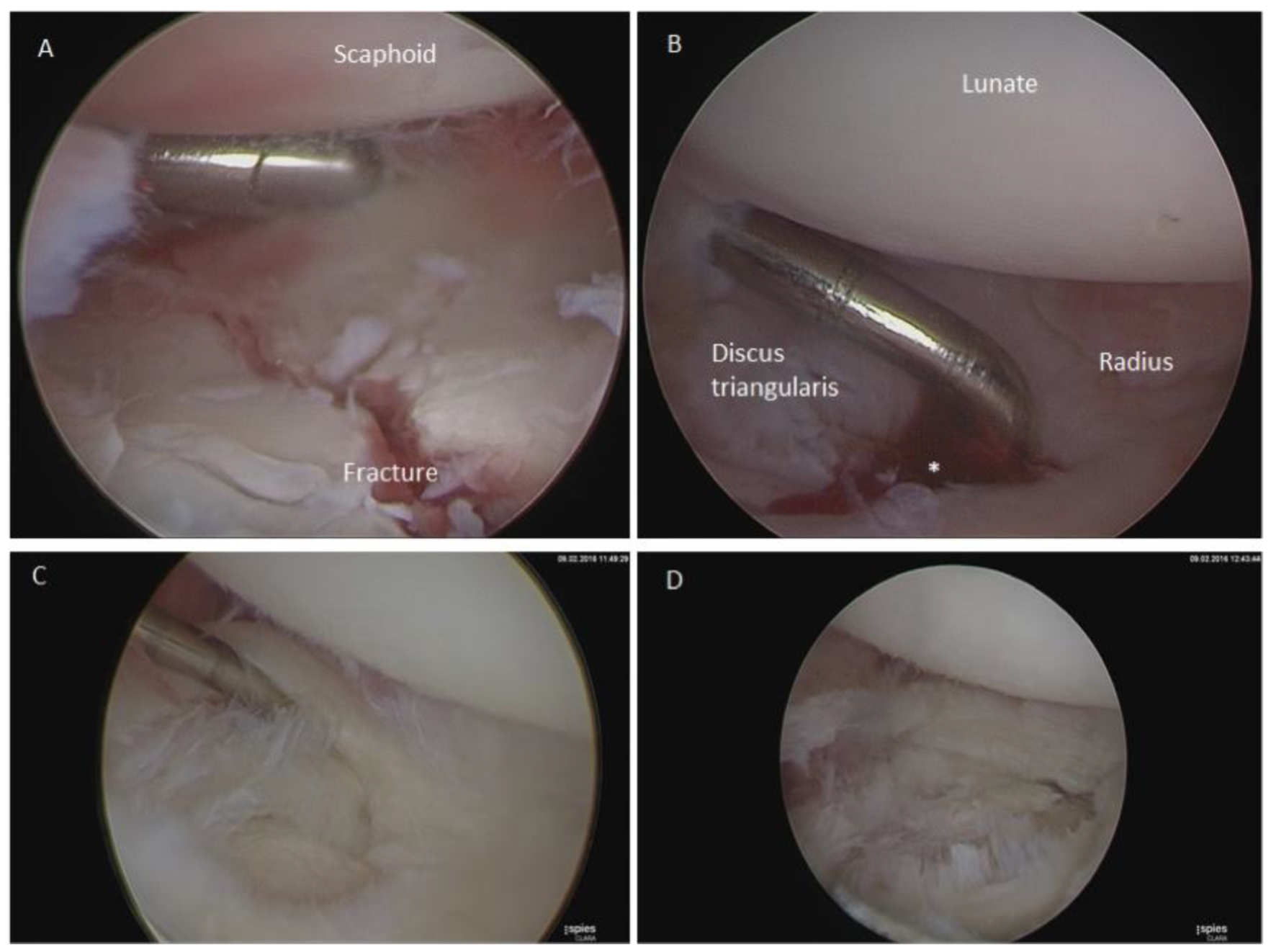
2.4. Surgery
2.5. Primary Outcome Measures
2.6. Demographic Target Parameters
2.7. Subjective Function Parameters
2.8. Objective Target Parameters
2.9. Statistical Analysis
3. Results
3.1. Study Population
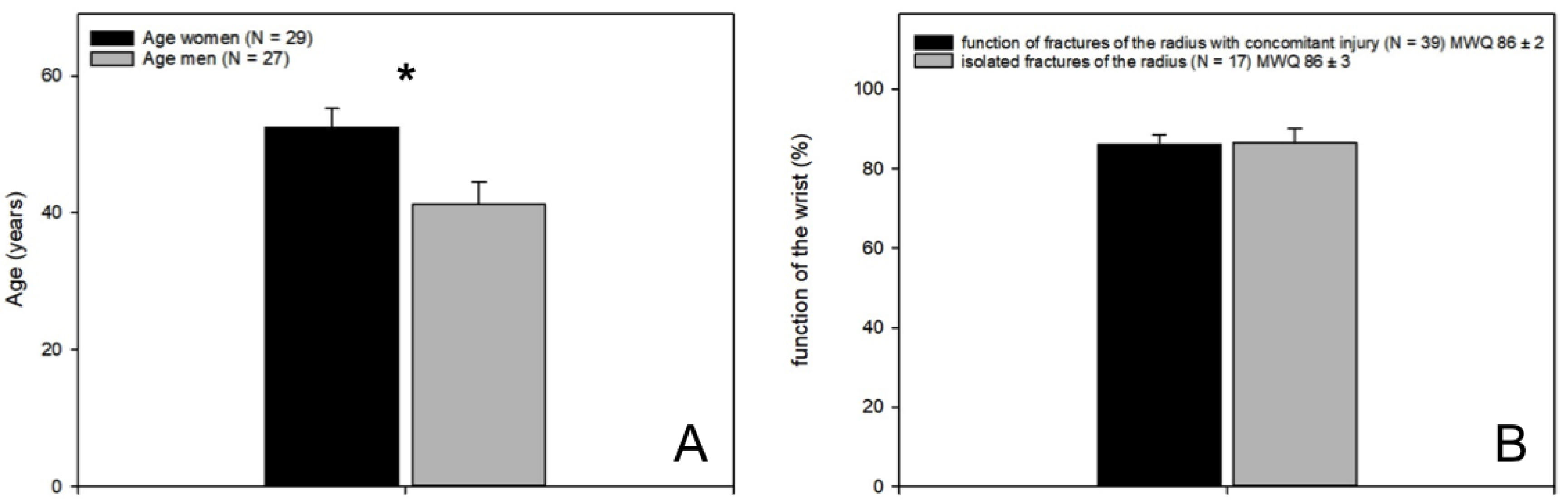
3.2. Demographic Target Parameters
3.3. Follow-Up by Self-Assessment Score (MWQ)
3.4. Clinical Follow-Up
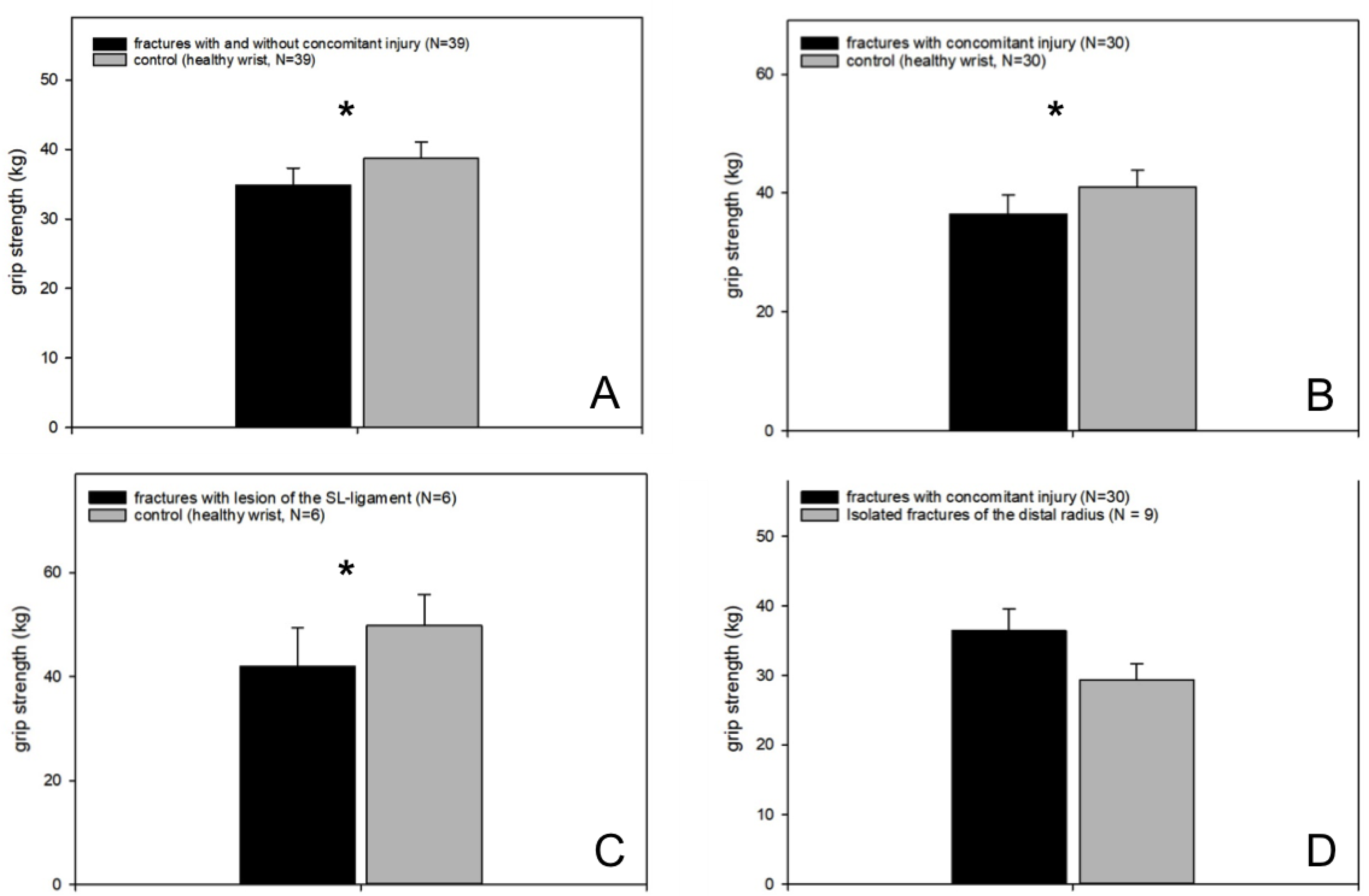
3.4.1. Grip Strength
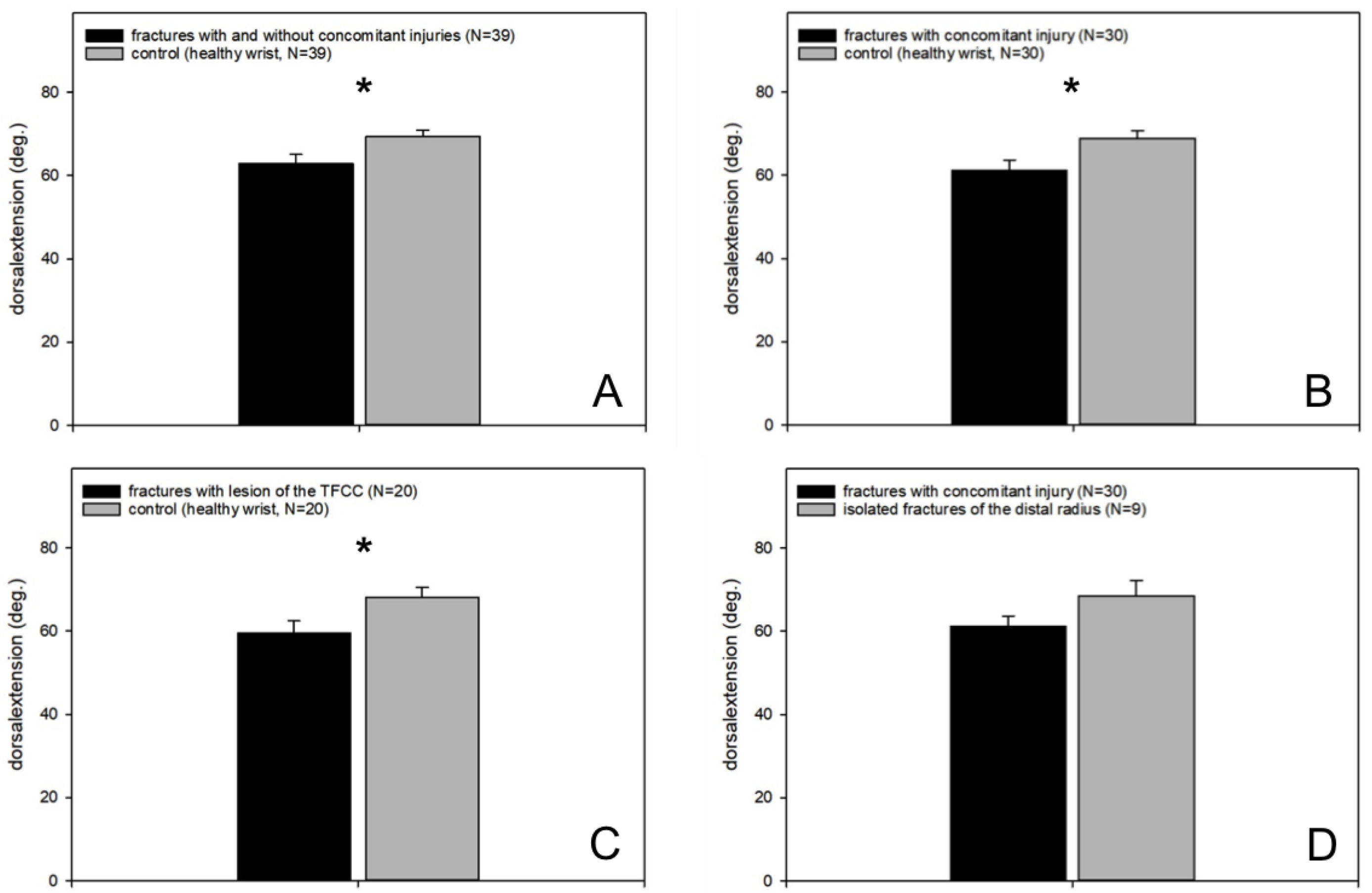
3.4.2. Range of Motion
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Deiler, S.; Haberle, S.; Quentmeier, P.; Biberthaler, P.; Ahrens, P. Arthroscopy-assisted management of wrist fractures. Der Unfallchirurg 2013, 116, 305–310. [Google Scholar] [CrossRef] [PubMed]
- Rueger, J.M.; Hartel, M.J.; Ruecker, A.H.; Hoffmann, M. Fractures of the distal radius. Der Unfallchirurg 2014, 117, 1025–1034. [Google Scholar] [CrossRef] [PubMed]
- Huber-Wagner, S.; Beirer, M.; Neu, J. Conservative treatment of distal radius fracture. Consequences of an uncritical follow-up. Der Unfallchirurg 2014, 117, 1050–1053. [Google Scholar] [CrossRef] [PubMed]
- Rikli, D.A.; Babst, R.; Jupiter, J.B. Distal radius fractures: New concepts as basis for surgical treatment. Handchir. Mikrochir. Plast. Chir. 2007, 39, 2–8. [Google Scholar] [CrossRef] [PubMed]
- Testa, G.; Vescio, A.; Di Masi, P.; Bruno, G.; Sessa, G.; Pavone, V. Comparison between Surgical and Conservative Treatment for Distal Radius Fractures in Patients over 65 Years. J. Funct. Morphol. Kinesiol. 2019, 4, 26. [Google Scholar] [CrossRef]
- Swart, E.; Tang, P. The Effect of Ligament Injuries on Outcomes of Operatively Treated Distal Radius Fractures. Am. J. Orthop. 2017, 46, E41–E46. [Google Scholar] [PubMed]
- Rappold, G.; Leixnering, M.; Pezzei, C. Carpal injuries associated with distal radius fractures. Diagnosis and therapy. Handchir. Mikrochir. Plast. Chir. 2001, 33, 221–228. [Google Scholar] [CrossRef] [PubMed]
- Prommersberger, K.J.; Muhldorfer-Fodor, M.; Kalb, K.; Schmitt, R.; van Schoonhoven, J. Scapholunate lesions. Der Unfallchirurg 2014, 117, 723–737. [Google Scholar] [CrossRef] [PubMed]
- Geissler, W.B. Intra-articular distal radius fractures: The role of arthroscopy? Hand Clin. 2005, 21, 407–416. [Google Scholar] [CrossRef] [PubMed]
- Geissler, W.B. Arthroscopically assisted reduction of intra-articular fractures of the distal radius. Hand Clin. 1995, 11, 19–29. [Google Scholar] [PubMed]
- Weiss, A.P.; Akelman, E.; Lambiase, R. Comparison of the findings of triple-injection cinearthrography of the wrist with those of arthroscopy. J. Bone Jt. Surg. 1996, 78, 348–356. [Google Scholar] [CrossRef] [PubMed]
- Volkmer, E.; Hagen, C.S.; Holzbach, T.; Leitsch, S.; Giunta, R.E. Results after Arthroscopically Assisted Management of Intra-Articular Distal Radius Fractures. Handchir. Mikrochir. Plast. Chir. 2015, 47, 155–163. [Google Scholar] [CrossRef] [PubMed]
- Wolf, J.M.; Dukas, A.; Pensak, M. Advances in wrist arthroscopy. J. Am. Acad. Orthop. Surg. 2012, 20, 725–734. [Google Scholar] [CrossRef] [PubMed]
- Beirer, M.; Serly, J.; Vester, H.; Pforringer, D.; Cronlein, M.; Deiler, S.; Biberthaler, P.; Kirchhoff, C. The Munich Wrist Questionnaire (MWQ)—Development and validation of a new patient-reported outcome measurement tool for wrist disorders. BMC Musculoskelet. Disord. 2016, 17, 167. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Lindau, T.; Adlercreutz, C.; Aspenberg, P. Peripheral tears of the triangular fibrocartilage complex cause distal radioulnar joint instability after distal radial fractures. J. Hand Surg. 2000, 25, 464–468. [Google Scholar] [CrossRef] [PubMed]
- Gradl, G.; Pillukat, T.; Fuchsberger, T.; Knobe, M.; Ring, D.; Prommersberger, K.J. The functional outcome of acute scapholunate ligament repair in patients with intraarticular distal radius fractures treated by internal fixation. Arch. Orthop. Trauma Surg. 2013, 133, 1281–1287. [Google Scholar] [CrossRef] [PubMed]
- Kasapinova, K.; Kamiloski, V. The correlation of initial radiographic characteristics of distal radius fractures and injuries of the triangular fibrocartilage complex. J. Hand Surg. 2016, 41, 516–520. [Google Scholar] [CrossRef] [PubMed]
- Pechlaner, S.; Gabl, M.; Lutz, M.; Krappinger, D.; Leixnering, M.; Krulis, B.; Ulmer, H.; Rudisch, A.; Arbeitsgruppe, A. Distal radius fractures--aetiology, treatment and outcome. Handchir. Mikrochir. Plast. Chir. 2007, 39, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Smeraglia, F.; Del Buono, A.; Maffulli, N. Wrist arthroscopy in the management of articular distal radius fractures. Br. Med Bull. 2016, 119, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Kasapinova, K.; Kamiloski, V. Outcomes of surgically treated distal radial fractures with associated triangular fibrocartilage complex injury. J. Hand Ther. Off. J. Am. Soc. Hand Ther. 2017. [Google Scholar] [CrossRef] [PubMed]

| Characteristics of the Evaluated Patients | |
|---|---|
| AO fracture type A | 5 (9%) |
| AO fracture type B | 9 (16%) |
| AO fracture type C | 42 (75%) |
| Distal radius fracture + isolated TFCC lesion | 24 (43%) |
| Distal radius fracture + isolated SL ligament tear | 8 (14%) |
| Distal radius fracture + TFCC lesion + SL ligament tear | 7 (12.5%) |
| Distal Radius Fracture + Concomitant Lesion | Distal Radius Fracture + Concomitant Lesion | Comparison of Function with Munich Wrist Questionnaire (MWQ) |
|---|---|---|
| Distal Radius Fracture + TFCC lesion (n = 24) | distal radius fracture + SL ligament tear (n = 8) | t-test (p-value = 1.0) |
| Distal Radius Fracture + TFCC lesion (n = 24) | distal radius fracture + TFCC lesion + SL ligament tear (n = 7) | t-test (p-value = 0.636) |
| Distal Radius Fracture + TFCC lesion (n = 24) | distal radius fracture without concomitant lesions (n = 17) | t-test (p-value = 0.979) |
| Distal Radius Fracture + SL Ligament tear (n = 8) | distal radius fracture + TFCC lesion + SL ligament tear (n = 7) | t-test (p-value = 0.779) |
| Distal Radius Fracture + SL Ligament tear (n = 8) | distal radius fracture without concomitant lesions (n = 17) | t-test (p-value = 0.954) |
| Distal Radius Fracture + TFCC lesion + SL Ligament tear (n = 7) | distal radius fracture without concomitant lesions (n = 17) | t-test (p-value = 0.775) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
von Matthey, F.; Schmid, K.; Zyskowski, M.; Deiler, S.; Biberthaler, P.; Vester, H. The Outcome of Distal Radius Fractures with Concomitant Injuries Is Similar to those of Isolated Distal Radius Fractures Provided that an Arthroscopically Supported Treatment Is Performed. J. Clin. Med. 2020, 9, 974. https://doi.org/10.3390/jcm9040974
von Matthey F, Schmid K, Zyskowski M, Deiler S, Biberthaler P, Vester H. The Outcome of Distal Radius Fractures with Concomitant Injuries Is Similar to those of Isolated Distal Radius Fractures Provided that an Arthroscopically Supported Treatment Is Performed. Journal of Clinical Medicine. 2020; 9(4):974. https://doi.org/10.3390/jcm9040974
Chicago/Turabian Stylevon Matthey, Francesca, Karola Schmid, Michael Zyskowski, Stephan Deiler, Peter Biberthaler, and Helen Vester. 2020. "The Outcome of Distal Radius Fractures with Concomitant Injuries Is Similar to those of Isolated Distal Radius Fractures Provided that an Arthroscopically Supported Treatment Is Performed" Journal of Clinical Medicine 9, no. 4: 974. https://doi.org/10.3390/jcm9040974
APA Stylevon Matthey, F., Schmid, K., Zyskowski, M., Deiler, S., Biberthaler, P., & Vester, H. (2020). The Outcome of Distal Radius Fractures with Concomitant Injuries Is Similar to those of Isolated Distal Radius Fractures Provided that an Arthroscopically Supported Treatment Is Performed. Journal of Clinical Medicine, 9(4), 974. https://doi.org/10.3390/jcm9040974





