Upstroke Time Per Cardiac Cycle as A Novel Parameter for Mortality Prediction in Patients with Acute Myocardial Infarction
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population and Design
2.2. Ethics Statement
2.3. Assessment of ABI, UTCC, and Four Limb Blood Pressures by ABI-form Device
2.4. Collection of Demographic and Medical Data
2.5. Statistical Analysis
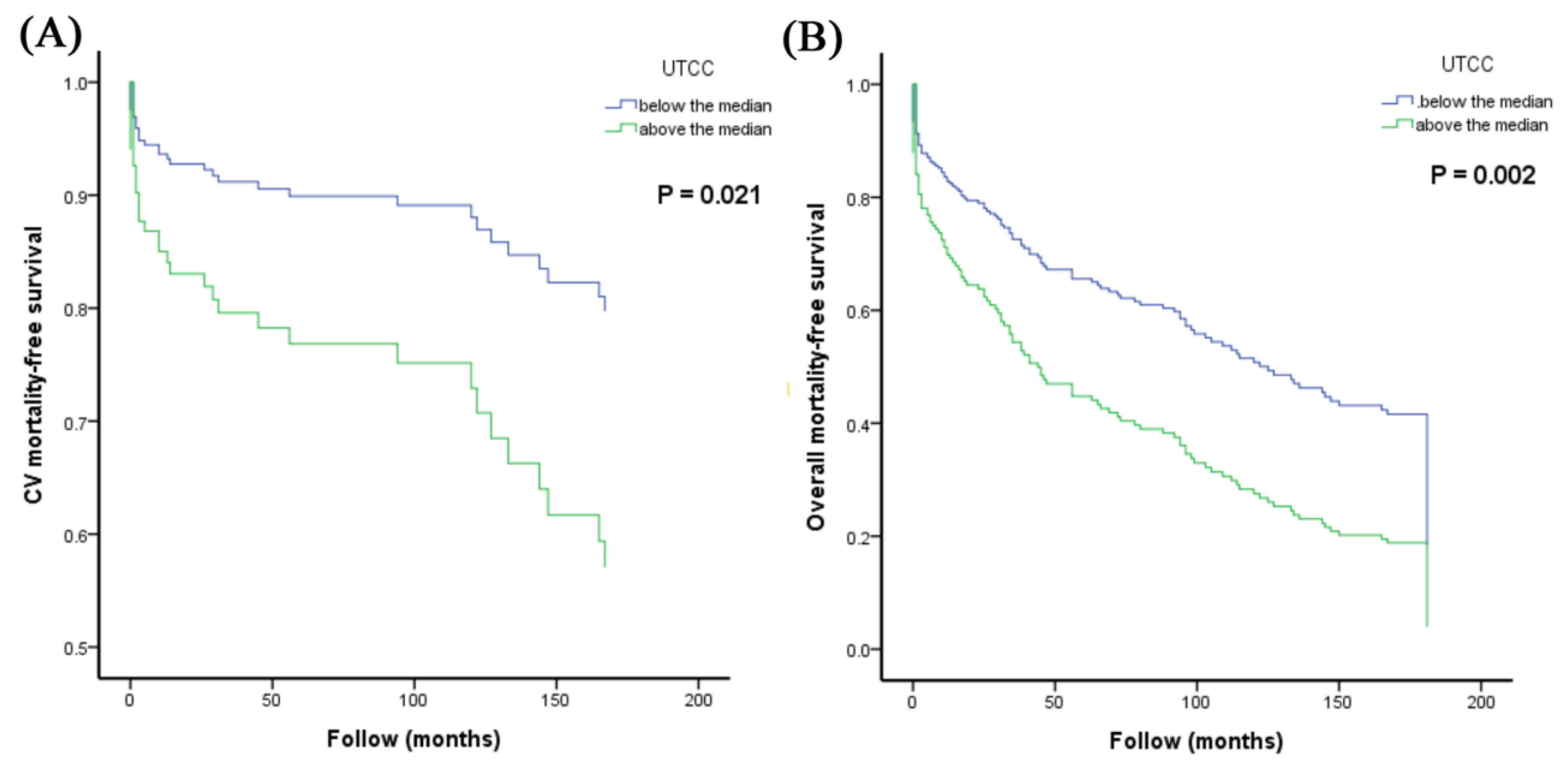
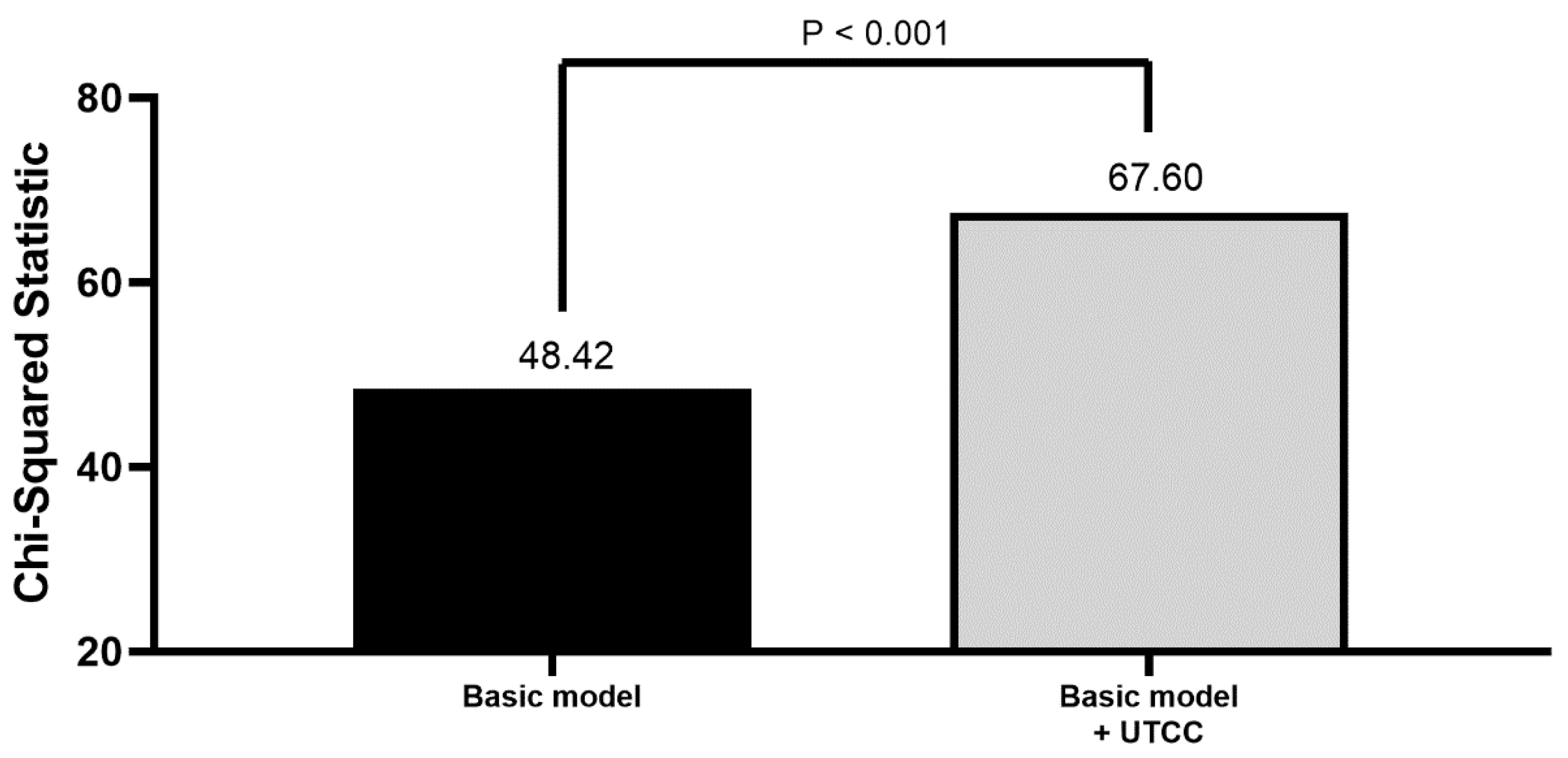
3. Results
4. Discussion
Study Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Anderson, J.L.; Morrow, D.A. Acute Myocardial Infarction. N. Engl. J. Med. 2017, 376, 2053–2064. [Google Scholar] [CrossRef] [PubMed]
- Murray, C.J.; Vos, T.; Lozano, R.; Naghavi, M.; Flaxman, A.D.; Michaud, C.; Ezzati, M.; Shibuya, K.; Salomon, J.A.; Abdalla, S.; et al. Disability-adjusted life years (DALYs) for 291 diseases and injuries in 21 regions, 1990–2010: A systematic analysis for the Global Burden of Disease Study 2010. Lancet 2012, 380, 2197–2223. [Google Scholar] [CrossRef]
- Li, Y.H.; Wang, Y.C.; Wang, Y.C.; Liu, J.C.; Lee, C.H.; Chen, C.C.; Hsieh, I.C.; Kuo, F.Y.; Huang, W.C.; Sung, S.H.; et al. 2018 Guidelines of the Taiwan Society of Cardiology, Taiwan Society of Emergency Medicine and Taiwan Society of Cardiovascular Interventions for the management of non ST-segment elevation acute coronary syndrome. J. Formos. Med. Assoc. 2018, 117, 766–790. [Google Scholar] [CrossRef] [PubMed]
- Carter, S.A. Indirect systolic pressures and pulse waves in arterial occlusive diseases of the lower extremities. Circulation 1968, 37, 624–637. [Google Scholar] [CrossRef] [PubMed]
- Allen, J.; Overbeck, K.; Nath, A.F.; Murray, A.; Stansby, G. A prospective comparison of bilateral photoplethysmography versus the ankle-brachial pressure index for detecting and quantifying lower limb peripheral arterial disease. J. Vasc. Surg. 2008, 47, 794–802. [Google Scholar] [CrossRef]
- Cachovan, M.; Linhart, J.; Prerovsky, I. Morphology of pulse wave curve from various segments of the lower limb in man. Angiology 1968, 19, 381–392. [Google Scholar] [CrossRef]
- Sheng, C.S.; Li, Y.; Huang, Q.F.; Kang, Y.Y.; Li, F.K.; Wang, J.G. Pulse Waves in the Lower Extremities as a Diagnostic Tool of Peripheral Arterial Disease and Predictor of Mortality in Elderly Chinese. Hypertension 2016, 67, 527–534. [Google Scholar] [CrossRef]
- Yamashina, A.; Tomiyama, H.; Takeda, K.; Tsuda, H.; Arai, T.; Hirose, K.; Koji, Y.; Hori, S.; Yamamoto, Y. Validity, reproducibility, and clinical significance of noninvasive brachial-ankle pulse wave velocity measurement. Hypertens. Res. 2002, 25, 359–364. [Google Scholar] [CrossRef] [PubMed]
- Tomiyama, H.; Yamashina, A.; Arai, T.; Hirose, K.; Koji, Y.; Chikamori, T.; Hori, S.; Yamamoto, Y.; Doba, N.; Hinohara, S. Influences of age and gender on results of noninvasive brachial-ankle pulse wave velocity measurement—A survey of 12517 subjects. Atherosclerosis 2003, 166, 303–309. [Google Scholar] [CrossRef]
- Yu, S.; Lu, Y.; Xiong, J.; Teliewubai, J.; Chi, C.; Ji, H.; Zhou, Y.; Fan, X.; Zhang, J.; Blacher, J.; et al. Comparison of ankle-brachial index and upstroke time in association with target organ damage: The Northern Shanghai Study. J. Am. Soc. Hypertens. 2018, 12, 703–713. [Google Scholar] [CrossRef] [PubMed]
- Rac-Albu, M.; Iliuta, L.; Guberna, S.M.; Sinescu, C. The role of ankle-brachial index for predicting peripheral arterial disease. Maedica 2014, 9, 295–302. [Google Scholar] [PubMed]
- Leng, G.C.; Fowkes, F.G.; Lee, A.J.; Dunbar, J.; Housley, E.; Ruckley, C.V. Use of ankle brachial pressure index to predict cardiovascular events and death: A cohort study. BMJ 1996, 313, 1440–1444. [Google Scholar] [CrossRef] [PubMed]
- Diehm, C.; Lange, S.; Darius, H.; Pittrow, D.; von Stritzky, B.; Tepohl, G.; Haberl, R.L.; Allenberg, J.R.; Dasch, B.; Trampisch, H.J. Association of low ankle brachial index with high mortality in primary care. Eur. Heart J. 2006, 27, 1743–1749. [Google Scholar] [CrossRef] [PubMed]
- McDermott, M.M.; Feinglass, J.; Slavensky, R.; Pearce, W.H. The ankle-brachial index as a predictor of survival in patients with peripheral vascular disease. J. Gen. Intern. Med. 1994, 9, 445–449. [Google Scholar] [CrossRef] [PubMed]
- Feringa, H.H.; Bax, J.J.; van Waning, V.H.; Boersma, E.; Elhendy, A.; Schouten, O.; Tangelder, M.J.; van Sambeek, M.H.; van den Meiracker, A.H.; Poldermans, D. The long-term prognostic value of the resting and postexercise ankle-brachial index. Arch Intern. Med. 2006, 166, 529–535. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Caro, J.; Migliaccio-Walle, K.; Ishak, K.J.; Proskorovsky, I. The morbidity and mortality following a diagnosis of peripheral arterial disease: Long-term follow-up of a large database. BMC Cardiovasc. Disord. 2005, 5, 14. [Google Scholar] [CrossRef] [PubMed]
- Sartipy, F.; Sigvant, B.; Lundin, F.; Wahlberg, E. Ten Year Mortality in Different Peripheral Arterial Disease Stages: A Population Based Observational Study on Outcome. Eur. J. Vasc. Endovasc. Surg. 2018, 55, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Manfredini, F.; Lamberti, N.; Guerzoni, F.; Napoli, N.; Gasbarro, V.; Zamboni, P.; Mascoli, F.; Manfredini, R.; Basaglia, N.; Rodriguez-Borrego, M.A.; et al. Rehabilitative Exercise Reduced the Impact of Peripheral Artery Disease on Vascular Outcomes in Elderly Patients with Claudication: A Three-Year Single Center Retrospective Study. J. Clin. Med. 2019, 8, 210. [Google Scholar] [CrossRef] [PubMed]
| Baseline Characteristics | UTCC below the Median | UTCC above the Median | P value |
|---|---|---|---|
| Number | 92 | 92 | |
| Age (years) | 60 ± 13 | 71 ± 12 | <0.001 |
| Male gender (%) | 82.6% | 62.0% | 0.003 |
| Dyslipidemia (%) | 26.1% | 37.0% | 0.153 |
| Diabetes mellitus (%) | 23.9% | 30.4% | 0.407 |
| Hypertension (%) | 31.5% | 54.3% | 0.003 |
| STEMI (%) | 19.6% | 20.7% | 1.000 |
| NSTEMI (%) | 80.4% | 79.3% | 1.000 |
| PAD (%) | 6.5% | 45.7% | <0.001 |
| Heart rate (beat/min) | 70.3 ± 12.3 | 87.4 ± 17.3 | <0.001 |
| LVEF | 60.9 ± 15.2 | 55.8 ± 15.6 | 0.066 |
| CCI | 2.38 ± 1.64 | 3.95 ± 1.79 | <0.001 |
| Body mass index (kg/m2) | 24.7 ± 3.6 | 24.0 ± 4.0 | 0.231 |
| Ankle brachial index | 1.04 ± 0.11 | 0.86 ± 0.22 | <0.001 |
| UTCC (%) | 16.1 ± 2.07 | 25.9 ± 7.93 | <0.001 |
| Parameter | Univariable Analysis | Multivariable Analysis | ||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| Age (Per 1 year) | 1.049(1.020–1.079) | < 0.001 | - | 0.801 |
| Gender (Male vs. Female) | 0.481(0.245–0.944) | 0.033 | - | 0.406 |
| Diabetes mellitus (Yes vs. No) | 1.154(0.556–2.295) | 0.700 | - | - |
| Hypertension (Yes vs. No) | 2.464(1.258–4.828) | 0.009 | 3.363(1.163-9.731) | 0.025 |
| Dyslipidemia (Yes vs. No) | 0.972(0.478–1.975) | 0.937 | - | - |
| STEMI (Yes vs. No) | 0.947(0.415–2.164) | 0.898 | - | - |
| Heart rate (Per beat/min) | 1.020(1.001–1.038) | 0.036 | - | 0.707 |
| Body mass index (Per 1kg/m2) | 0.950(0.864–1.043) | 0.282 | - | - |
| LVEF (Per 1%) | 0.973(0.947–1.000) | 0.048 | - | 0.355 |
| CCI | 1.400(1.198–1.637) | < 0.001 | - | 0.943 |
| Ankle brachial index (Per 1SD) | 0.656(0.489–0.881) | 0.005 | - | 0.407 |
| UTCC (Per 1SD) | 1.627(1.231–2.151) | 0.001 | 1.844(1.018–3.342) | 0.043 |
| Parameter | Univariable Analysis | Multivariable Analysis | ||
|---|---|---|---|---|
| HR (95% CI) | P | HR (95% CI) | P | |
| Age (Per 1 year) | 1.070(1.053–1.087) | <0.001 | 1.050(1.028–1.073) | <0.001 |
| Gender (Male vs. Female) | 0.606(0.416–0.883) | 0.009 | - | 0.339 |
| Diabetes mellitus (Yes vs. No) | 1.173(0.793–1.736) | 0.424 | - | - |
| Hypertension (Yes vs. No) | 1.570(1.103–2.235) | 0.012 | - | 0.703 |
| Dyslipidemia (Yes vs. No) | 1.072(0.735–1.564) | 0.717 | - | - |
| STEMI (Yes vs. No) | 0.922(0.590–1.440) | 0.721 | - | - |
| Heart rate (Per 1beat/min) | 1.019(1.009–1.029) | <0.001 | - | 0.956 |
| Body mass index (Per 1kg/m2) | 0.902(0.856–0.950) | <0.001 | - | 0.149 |
| LVEF (Per 1%) | 0.983(0.970–0.997) | 0.014 | - | 0.150 |
| CCI | 1.438(1.322–1.564) | < 0.001 | - | 0.506 |
| Ankle brachial index (Per 1SD) | 0.790(0.727–0.858) | < 0.001 | - | 0.493 |
| UTCC (Per 1SD) | 1.084(1.063–1.105) | < 0.001 | 1.849(1.367–2.501) | <0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hsu, P.-C.; Lee, W.-H.; Tsai, W.-C.; Chen, Y.-C.; Chi, N.-Y.; Chang, C.-T.; Chu, C.-Y.; Lin, T.-H.; Lee, C.-S.; Lai, W.-T.; et al. Upstroke Time Per Cardiac Cycle as A Novel Parameter for Mortality Prediction in Patients with Acute Myocardial Infarction. J. Clin. Med. 2020, 9, 904. https://doi.org/10.3390/jcm9040904
Hsu P-C, Lee W-H, Tsai W-C, Chen Y-C, Chi N-Y, Chang C-T, Chu C-Y, Lin T-H, Lee C-S, Lai W-T, et al. Upstroke Time Per Cardiac Cycle as A Novel Parameter for Mortality Prediction in Patients with Acute Myocardial Infarction. Journal of Clinical Medicine. 2020; 9(4):904. https://doi.org/10.3390/jcm9040904
Chicago/Turabian StyleHsu, Po-Chao, Wen-Hsien Lee, Wei-Chung Tsai, Ying-Chih Chen, Nai-Yu Chi, Ching-Tang Chang, Chun-Yuan Chu, Tsung-Hsien Lin, Chee-Siong Lee, Wen-Ter Lai, and et al. 2020. "Upstroke Time Per Cardiac Cycle as A Novel Parameter for Mortality Prediction in Patients with Acute Myocardial Infarction" Journal of Clinical Medicine 9, no. 4: 904. https://doi.org/10.3390/jcm9040904
APA StyleHsu, P.-C., Lee, W.-H., Tsai, W.-C., Chen, Y.-C., Chi, N.-Y., Chang, C.-T., Chu, C.-Y., Lin, T.-H., Lee, C.-S., Lai, W.-T., Sheu, S.-H., & Su, H.-M. (2020). Upstroke Time Per Cardiac Cycle as A Novel Parameter for Mortality Prediction in Patients with Acute Myocardial Infarction. Journal of Clinical Medicine, 9(4), 904. https://doi.org/10.3390/jcm9040904





