Galectin-3 is Associated with Cardiovascular Events in Post-Acute Coronary Syndrome Patients with Type-2 Diabetes
Abstract
1. Introduction
2. Experimental Section
2.1. Patients
2.2. Ethics Statement
2.3. Study Design
2.4. Biomarker and Analytical Studies
2.5. Statistics
3. Results
3.1. Baseline Characteristics
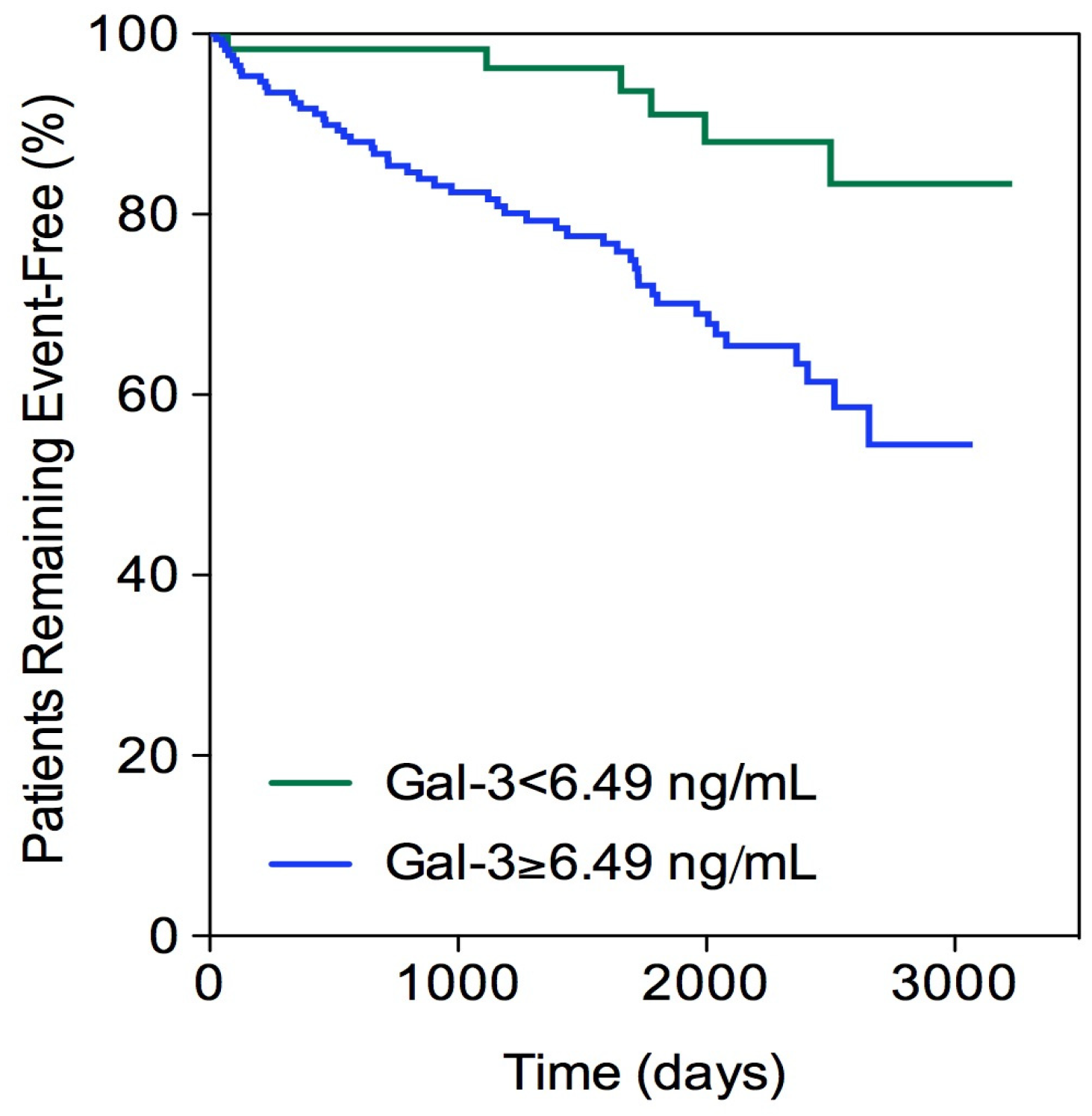
3.2. Primary Outcome
3.3. Acute Ischemic Events
3.4. Heart Failure or Death
4. Discussion
Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Mitchell, S.; Malanda, B.; Damasceno, A.; Eckel, R.H.; Gaita, D.; Kotseva, K.; Januzzi, J.L.; Mensah, G.; Plutzky, J.; Prystupiuk, M.; et al. A Roadmap on the Prevention of Cardiovascular Disease among People Living With Diabetes. Glob. Heart 2019, 14, 215–240. [Google Scholar] [CrossRef] [PubMed]
- Rao Kondapally Seshasai, S.; Kaptoge, S.; Thompson, A.; Di Angelantonio, E.; Gao, P.; Sarwar, N.; Whincup, P.H.; Mukamal, K.J.; Gillum, R.F.; Holme, I.; et al. Emerging Risk Factors Collaboration. Diabetes mellitus, fasting glucose, and risk of cause-specific death. NEJM 2011, 364, 829–841. [Google Scholar] [PubMed]
- Sörensen, B.M.; Houben, A.J.; Berendschot, T.T.; Schouten, J.S.; Kroon, A.A.; van der Kallen, C.J.; Henry, R.M.; Koster, A.; Sep, S.J.; Dagnelie, P.C.; et al. Prediabetes and type 2 diabetes are associated with generalized microvascular dysfunction: The maastricht study. Circulation 2016, 134, 1339–1352. [Google Scholar] [CrossRef] [PubMed]
- Alberto Zamora, J.M. Prognosis of diabetic patients with coronary heart disease. Rev. Esp. Card. 2002, 55, 751–762. [Google Scholar]
- Moreno, P.R.; Murcia, A.M.; Palacios, I.F.; Leon, M.N.; Bernardi, V.H.; Fuster, V.; Fallon, J.T. Coronary composition and macrophage infiltra-tion in atherectomy specimens from patients with diabetes me-llitus. Circulation 2000, 102, 2180–2184. [Google Scholar] [CrossRef]
- Winocour, P.D. Platelet abnormalities in diabetes mellitus. Diabetes 1992, 41 (Suppl. 2), 26–31. [Google Scholar] [CrossRef]
- Fuster, V. Remodelado del trombo: Punto clave en la progresion dela aterosclerosis coronaria. Rev. Esp. Cardiol. 2000, 53 (Suppl. 1), 2–7. [Google Scholar]
- Tuñón, J.; Fernández-Fernández, B.; Carda, R.; Pello, A.M.; Cristóbal, C.; Tarín, N.; Aceña, Á.; González-Casaus, M.L.; Huelmos, A.; Alonso, J.; et al. Circulating fibroblast growth factor-23 plasma levels predict adverse cardiovascular outcomes in patients with diabetes mellitus with coronary artery disease. Diabetes Metab. Res. Rev. 2016, 32, 685–693. [Google Scholar] [CrossRef]
- Li, P.; Liu, S.; Lu, M.; Bandyopadhyay, G.; Oh, D.; Imamura, T.; Johnson, A.M.F.; Sears, D.; Shen, Z.; Cui, B.; et al. Hematopoietic-derived galectin-3 causes cellular and systemic insulin resistance. Cell 2016, 167, 973–984. [Google Scholar] [CrossRef]
- Morigny, P.; Houssier, M.; Mouisel, E.; Langin, D. Adipocyte lipolysis and insulin resistance. Biochimie 2016, 125, 259–266. [Google Scholar] [CrossRef]
- Vora, A.; de Lemos, J.A.; Ayers, C.; Grodin, J.L.; Lingvay, I. Association of galectin-3 with diabetes mellitus in the dallas heart study. J. Clin. Endocrinol. Metab. 2019, 104, 4449–4458. [Google Scholar] [CrossRef] [PubMed]
- Tuñón, J.; Blanco-Colio, L.; Cristóbal, C.; Tarín, N.; Higueras, J.; Huelmos, A.; Alonso, J.; Egido, J.; Asensio, D.; Lorenzo, Ó.; et al. Usefulness of a combination of monocyte chemoattractant protein-1, galectin-3, and N-terminal probrain natriuretic peptide to predict cardiovascular events in patients with coronary artery disease. Am. J. Cardiol. 2014, 113, 434. [Google Scholar] [CrossRef] [PubMed]
- Maack, C.; Lehrke, M.; Backs, J.; Heinzel, F.R.; Hulot, J.-S.; Marx, N.; Paulus, W.J.; Rossignol, P.; Taegtmeyer, H.; Bauersachs, J.; et al. Heart failure and diabetes: Metabolic alterations and therapeutic interventions: A state-of-the-art review from the Translational Research Committee of the Heart Failure Association European Society of Cardiology. Eur. Heart J. 2018, 39, 4243–4254. [Google Scholar] [CrossRef] [PubMed]
- Sharma, U.C.; Pokharel, S.; van Brakel, T.J.; van Berlo, J.H.; Cleutjens, J.P.; Schroen, B.; André, S.; Crijns, H.J.; Gabius, H.J.; Maessen, J.P.Y.M. Galectin-3 marks activated macrophages in failure-prone hypertrophied hearts and contributes to cardiac dysfunction. Circulation 2004, 110, 3121–3128. [Google Scholar] [CrossRef]
- Meijers, W.C.; van der Velde, A.R.; Pascual-Figal, D.A.d.B.R. Galectin-3 and post-myocardial infarction cardiac remodeling. Eur. J. Pharmacol. 2015, 763, 115–121. [Google Scholar] [CrossRef]
- González, G.E.; Cassaglia, P.; Noli Truant, S.; Fernández, M.M.; Wilensky, L.; Volberg, V.; Malchiodi, E.L.; Morales, C.G.R. Galectin-3 is essential for early wound healing and ventricular remodeling after myocardial infarction in mice. Int. J. Cardiol. 2014, 176, 1423–1425. [Google Scholar] [CrossRef]
- Aksan, G.; Gedikli, Ö.; Keskin, K.; Nar, G.; İnci, S.; Yıldız, S.S.; Kaplan, Ö.; Soylu, K.; Kılıçkesmez, K.O.Ş.M. Is galectin-3 a biomarker, a player-or both-in the presence of coronary atherosclerosis? J. Investig. Med. 2016, 64, 764. [Google Scholar] [CrossRef]
- Sano, H.; Hsu, D.K.; Yu, L.; Apgar, J.R.; Kuwabara, I.; Yamanaka, T.; Hirashima, M.L.F.T. Human galectin-3 is a novel chemoattractant for monocytes and macrophages. J. Immunol. 2000, 165, 215. [Google Scholar] [CrossRef]
- Hansson, G.K.; Libby, P.T.I. Inflammation and plaque vulnerability. J. Intern. Med. 2015, 278, 483. [Google Scholar] [CrossRef]
- Novak, R.; Dabelic, S.D.J. Galectin-1 and galectin-3 expression profiles in classically and alternatively activated human macrophages. Biochim. Biophys. Acta 2012, 1820, 13. [Google Scholar] [CrossRef]
- Papaspyridonos, M.; McNeill, E.; de Bono, J.P.; Smith, A.; Burnand, K.G.; Channon, K.M.; Greaves, D.R. Galectin-3 is an amplifier of inflammation in atherosclerotic plaque progression through macrophage activation and monocyte chemoattraction. Arterioscler. Thromb. Vasc. Biol. 2008, 28, 433–440. [Google Scholar] [CrossRef] [PubMed]
- Nachtigal, M.; Al-Assaad, Z.; Mayer, E.P.; Kim, K.; Monsigny, M. Galectin-3 expression in human atherosclerotic lesions. Am. J. Pathol. 1998, 152, 1199–1208. [Google Scholar] [PubMed]
- Tian, L.; Chen, K.; Cao, J.; Han, Z.; Gao, L.; Wang, Y.; Fan, Y.; Wang, C. Galectin-3-induced oxidized low-density lipoprotein promotes the phenotypic transformation of vascular smooth muscle cells. Mol. Med. Rep. 2015, 12, 4995–5002. [Google Scholar] [CrossRef]
- Kingwell, K. Diabetes: Turning down galectin 3 to combat insulin resistance. Nat. Rev. Drug Discov. 2016, 16, 18. [Google Scholar] [CrossRef] [PubMed]
- Motiwala, S.R.; Szymonifka, J.; Belcher, A.; Weiner, R.B.; Baggish, A.L.; Sluss, P.; Gaggin, H.K.; Bhardwaj, A.; Januzzi, J.L. Serial measurement of galectin-3 in patients with chronic heart failure: Results from the ProBNP Outpatient Tailored Chronic Heart Failure Therapy (PROTECT) study. Eur. J. Heart Fail. 2013, 15, 1157–1163. [Google Scholar] [CrossRef] [PubMed]
- Falcone, C.; Lucibello, S.; Mazzucchelli, I.; Bozzini, S.; D’Angelo, A.; Schirinzi, S.; Totaro, R.; Falcone, R.; Bondesan, M.; Pelissero, G. Galectin-3 plasma levels and coronary artery disease: A new possible biomarker of acute coronary syndrome. Int. J. Immunopathol. Pharmacol. 2011, 24, 905–913. [Google Scholar] [CrossRef]
- Maiolino, G.; Rossitto, G.; Pedon, L.; Cesari, M.; Frigo, A.C.; Azzolini, M.; Plebani, M.R.G. Galectin-3 predicts long-term cardiovascular death in high-risk patients with coronary artery disease. Arterioscler. Thromb. Vasc. Biol. 2015, 35, 725. [Google Scholar] [CrossRef]
- De Boer, R.A.; Lok, D.J.; Jaarsma, T.; van der Meer, P.; Voors, A.A.; van Hillege, H.L.V.D. Predictive value of plasma galectin-3 levels in heart failure with reduced and preserved ejection fraction. Ann. Med. 2011, 43, 60. [Google Scholar] [CrossRef]
- Yilmaz, H.; Cakmak, M.; Inan, O.; Darcin, T.A.A. Increased levels of galectin-3 were associated with prediabetes and diabetes: New risk factor? J. Endocrinol. Investig. 2015, 38, 527. [Google Scholar] [CrossRef]
- Pugliese, G.; Iacobini, C.; Ricci, C.; Blasetti Fantauzzi, C.M.S. Galectin-3 in diabetic patients. Clin. Chem. Lab. Med. 2014, 52, 1413–1423. [Google Scholar] [CrossRef]
- Canning, P.; Glenn, J.V.; Hsu, D.K.; Liu, F.T.; Gardiner, T.A.; Stitt, A.W. Inhibition of advanced glycation and absence of galectin-3 prevent blood-retinal barrier dysfunction during short-term diabetes. Exp. Diabetes Res. 2007, 2007, 51837. [Google Scholar] [CrossRef] [PubMed]
- Iacobini, C.; Menini, S.; Oddi, G.; Ricci, C.; Amadio, L.; Pricci, F.; Olivieri, A.; Sorcini, M.; Di Mario, U.; Pesce, C.; et al. Galectin-3/AGE-receptor 3 knockout mice show accelerated AGE-induced glomerular injury: Evidence for a protective role of galectin-3 as an AGE receptor. FASEB J. 2004, 18, 1773–1775. [Google Scholar] [CrossRef] [PubMed]
- Ozturk, D.; Celik, O.; Satilmis, S.; Aslan, S.; Erturk, M.; Cakmak, H.A.; Kalkan, A.K.; Ozyilmaz, S.; Diker, V.G.M. Association between serum galectin-3 levels and coronary atherosclerosis and plaque burden/structure in patients with type 2 diabetes mellitus. Coron. Artery Dis. 2015, 26, 396. [Google Scholar] [CrossRef] [PubMed]
- Tan, K.C.B.; Cheung, C.L.; Lee, A.C.H.; Lam, J.K.Y.; Wong, Y.S.S. Galectin-3 and risk of cardiovascular events and all-cause mortality in type 2 diabetes. Diabetes Metab. Res. Rev. 2019, 35, e309. [Google Scholar] [CrossRef]
- Drechsler, C.; Delgado, G.; Wanner, C.; Blouin, K.; Pilz, S.; Tomaschitz, A.; Kleber, M.E.; Dressel, A.; Willmes, C.; Krane, V.; et al. Galectin-3, renal function, and clinical outcomes: Results from the LURIC and 4D studies. J. Am. Soc. Nephrol. 2015, 26, 2213. [Google Scholar] [CrossRef] [PubMed]
- Seferovic, J.P.; Lalic, N.M.; Floridi, F.; Tesic, M.; Seferovic, P.M.; Giga, V.; Lalic, K.; Jotic, A.; Jovicic, S.; Colak, E.; et al. Structural myocardial alterations in diabetes and hypertension: The role of galectin-3. Clin. Chem. Lab. Med. 2014, 52, 1499–1505. [Google Scholar] [CrossRef] [PubMed]
- De Lemos, J.A.; Morrow, D.A.; Blazing, M.A.; Jarolim, P.; Wiviott, S.D.; Sabatine, M.S.; Califf, R.M.B.E. Serial measurement of monocyte chemoattractant protein-1 after acute coronary syndromes: Results from the A to Z trial. J. Am. Coll. Cardiol. 2007, 50, 211. [Google Scholar] [CrossRef]
- Alonso, N.; Lupón, J.; Barallat, J.; De Antonio, M.; Domingo, M.; Zamora, E.; Moliner, P.; Galán, A.; Santesmases, J.; Pastor, C.; et al. Impact of diabetes on the predictive value of heart failure biomarkers. Cardiovasc. Diabetol. 2016, 15, 151. [Google Scholar] [CrossRef]
| Characteristic | Patients without Diabetes (N = 732) | Patients with Diabetes (N = 232) | p-Value |
|---|---|---|---|
| Age (yr) | 60.0 (51–71) | 61 (54–72) | 0.092 |
| Male sex (%) | 76.6 | 75.0 | 0.609 |
| Body mass index (Kg/m2) | 27.7 (25.3–30.3) | 29.0 (26.9–32.1) | <0.001 |
| Present Smoker (%) | 14.1 | 13.4 | 0.786 |
| Hypertension (%) | 58.6 | 81.9 | <0.001 |
| Previous heart failure (%) | 9.0 | 19.8 | <0.001 |
| Cerebrovascular events (%) | 2.3 | 4.3 | 0.110 |
| Present or past atrial fibrillation (%) | 6.7 | 5.2 | 0.407 |
| Total cholesterol (mg(dL) | 145 (126–165) | 140 (121–157) | 0.010 |
| LDL cholesterol (mg/dL) | 79 (65–93) | 73 (62–88) | 0.005 |
| HDL cholesterol (mg/dL) | 42 (35–48) | 38 (33–45) | <0.001 |
| Triglycerides (mg/dL) | 97 (75–135) | 113 (82–161) | <0.001 |
| Glucose (mg/dL) | 97 (90–106) | 130 (109–159) | <0.001 |
| GFR (CKD-EPI) (mL/min/1.73 m2) | 81 (67–93) | 77 (63–91) | 0.078 |
| High-sensitivity C-reactive protein (mg/L) | 1.1 (0.3–2.9) | 1.5 (0.6–4.5) | 0.002 |
| NT-ProBNP (pg/mL) | 168 (89–381) | 193 (101–473) | 0.103 |
| MCP-1 (pg/mL) | 133 (105–173) | 144 (113–195) | 0.006 |
| Galectin-3 (ng/mL) | 7.8 (5.9–9.8) | 8.3 (6.5–10.5) | 0.049 |
| High-sensitivity troponin I (ng/mL) | 0.003 (0.000–0.010) | 0.004 (0.000-0.011) | 0.174 |
| Medical Therapy | |||
| Acetylsalicylic acid (%) | 92.5 | 97.0 | 0.015 |
| AntiP2Y12 (%) | 74.9 | 77.2 | 0.480 |
| Acenocumarol (%) | 5.3 | 6.0 | 0.681 |
| Statins (%) | 95.1 | 94.0 | 0.504 |
| Oral antidiabetic drugs (%) | 0 | 71.1 | <0.001 |
| Insulin (%) | 0 | 27.6 | <0.001 |
| ACE inhibitors (%) | 62.3 | 63.4 | 0.770 |
| Angiotensin receptor blockers (%) | 13.9 | 19.8 | 0.030 |
| Aldosterone receptor blockers (%) | 6.1 | 8.6 | 0.191 |
| Betablockers (%) | 79.1 | 78.9 | 0.943 |
| Diuretics (%) | 15.4 | 29.3 | <0.001 |
| Nitrates (%) | 11.2 | 18.5 | 0.004 |
| Data at Last Acute Coronary Event | |||
| STEMI/Non-STEACS (%) | 48.7/51.3 | 55.6/44.4 | 0.070 |
| Number of vessels diseased | 1.0 (1.0, 2.0) | 1.0 (1.0, 2.0) | <0.001 |
| Drug-eluting stent (%) | 49.0 | 62.9 | <0.001 |
| Coronary artery bypass graft (%) | 4.5 | 9.0 | 0.009 |
| Complete revascularization (%) | 73.2 | 60.8 | <0.001 |
| No Diabetic Patients | Diabetic Patients | |||
|---|---|---|---|---|
| Variable | Model 1 | Model 2 | Model 1 | Model 2 |
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Age, years | 1.04 (1.02–1.07) | 1.04 (1.02–1.06) | 1.02 (0.99–1.06) | 1.03 (0.99–1.06) |
| Sex, male | 1.83 (1.05–3.16) | 2.03 (1.15–3.61) | 0.38 (0.17–0.86) | 0.44 (0.18-1.04) |
| Smoker, yes | 1.33 (0.70–2.56) | 0.78 (0.47–1.28) | 1.82 (0.73–4.57) | 2.29 (0.84–6.25) |
| Hypertension, yes | 1.42 (0.88–2.30) | 1.36 (0.83–3.69) | 1.46 (0.53–4.00) | 1.79 (0.64–4.95) |
| Body mass index, kg/m2 | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 0.99 (0.97–1.01) | 0.99 (0.97–1.01) |
| History of CVE, yes | 0.84 (0.24–2.91) | 1.06 (0.31–3.71) | 9.62 (2.47–37.6) | 9.01 (2.10–38.7) |
| Ejection fraction <40%, yes | 2.11 (1.21–3.69) | 1.66 (0.89–3.07) | 0.62 (0.26–1.50) | 0.68 (0.27–1.67) |
| Atrial Fibrillation, yes | 0.79 (0.32–1.89) | 0.70 (0.27–1.81) | 3.33 (0.99–11.14) | 3.27 (0.91–11.83) |
| Acute myocardial infarction, yes | 0.84 (0.24–2.91) | 0.67 (0.43–1.03) | 1.19 (0.57–2.46) | 1.10 (0.53–2.29) |
| Complete Revascularization | 0.89 (0.58–1.35) | 0.87 (0.57–1.34) | 0.75 (0.38–1.48) | 0.85 (0.43–1.67) |
| LDL-c, mg/dL | 1.00 (0.99–1.01) | 1.00 (1.00–1.01) | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) |
| HDL-c, mg/dL | 1.00 (0.98–1.02) | 1.00 (0.98–1.02) | 1.01 (0.97–1.05) | 1.01 (0.97–1.05) |
| Triglycerides, mg/dL | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.00 (1.00–1.01) |
| CKD-EPI <60 mL/min/1.73 m2 | 0.96 (0.59–1.57) | 0.75 (0.44–1.27) | 0.86 (0.40–1.84) | 0.77 (0.34–1.71) |
| Acetylsalicylic acid, yes | 1.20 (0.59–2.42) | 1.11 (0.54–2.25) | 0.66 (0.14–3.08) | 0.84 (0.18–3.93) |
| AntiP2Y12, yes | 0.96 (0.63–1.45) | 0.98 (0.64–1.51) | 0.42 (0.20–0.87) | 0.44 (0.21–0.95) |
| Anticoagulants, yes | 1.19 (0.50–2.82) | 1.00 (0.39–2.53) | 2.65 (0.65–10.7) | 2.81 (0.64–12.2) |
| Statins, yes | 0.45 (0.25–0.82) | 0.44 (0.24–0.82) | 0.32 (0.11–0.98) | 0.37 (0.98–3.89) |
| ACE inhibitors, yes | 0.89 (0.56–1.43) | 0.92 (0.56–1.49) | 0.49 (0.23–10.4) | 0.49 (0.22–1.08) |
| ARB, yes | 1.12 (0.63–2.00) | 1.16 (0.63–2.11) | 0.95 (0.40–2.26) | 0.82 (0.32–2.07) |
| Anti-aldosterone, yes | 0.79 (0.36–1.77) | 0.76 (0.33–1.75) | 2.62 (0.95–7.20) | 2.12 (0.75–6.04) |
| β-Blockers, yes | 0.86 (0.55–1.36) | 0.84 (0.52–1.34) | 0.98 (0.48–2.01) | 0.92 (0.45–1.86) |
| Nitrates, yes | 1.53 (0.93–2.53) | 1.34 (0.79–2.26) | 1.98 (0.93–4.20) | 1.83 (0.86–3.90) |
| Diuretics, yes | 1.19 (0.74–1.92) | 1.14 (0.70–1.88) | 1.04 (0.50–2.14) | 0.89 (0.40–1.95) |
| Insulin, yes | - | - | 1.89 (1.00–3.60) | 1.95 (0.98–3.89) |
| Oral antidiabetic drugs, yes | - | - | 0.98 (0.49–1.97) | 1.01 (0.48–2.11) |
| Hs-CRP, mg/L | 0.98 (0.95–1.01) | 0.98 (0.95–1.02) | 0.97 (0.93–1.01) | 0.96 (0.92–1.01) |
| NT-proBNP, 1-SD | - | 1.21 (1.04–1.42) | - | 1.08 (0.81–1.44) |
| MCP-1, 1-SD | - | 1.23 (1.05–1.44) | - | 0.93 (0.61–1.41) |
| Gal-3, 1-SD | - | 1.07 (0.89–1.28) | - | 1.57 (1.07–2.30) |
| Hs-cTnT, 1-SD | - | 1.42 (0.49–4.09) | - | 0.95 (0.81–1.12) |
| Nondiabetic Patients | Diabetic Patients | |||
|---|---|---|---|---|
| Variable | Model 1 | Model 2 | Model 1 | Model 2 |
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Age, years | 1.01 (0.99–1.04) | 1.01 (0.98–1.04) | 0.99 (0.94–1.03) | 0.98 (0.94–1.03) |
| Sex, male | 2.28 (1.14–4.56) | 2.45 (1.19.5.01) | 0.30 (0.11–0.82) | 0.32 (0.11–0.91) |
| Smoker, yes | 1.90 (1.08–3.35) | 1.97 (1.10–3.51) | 1.30 (0.41–4.19) | 1.71 (0.47–6.15) |
| Hypertension, yes | 1.46 (0.81–2.63) | 1.42 (0.78–2.56) | 3.08 (0.77–12.3) | 3.45 (0.87–13.7) |
| Body mass index, kg/m2 | 1.00 (0.94–1.06) | 0.99 (0.93–1.06) | 0.99 (0.96–1.02) | 0.99 (0.95–1.02) |
| History of CVE, yes | 0.00 (0.00–1.5 × 1026) | 0.00 (0.00–1.8 × 1019) | 13.4 (2.60–69.4) | 12.4 (2.16–71.1) |
| Ejection fraction <40%, yes | 2.03 (0.95–4.36) | 1.75 (0.79–3.87) | 0.56 (0.18–1.77) | 0.63 (0.19–2.03) |
| Atrial Fibrillation, yes | 0.46 (0.11–1.96) | 0.48 (0.12–2.03) | 2.01 (0.39–10.3) | 2.11 (0.34–13.0) |
| Acute myocardial infarction, yes | 0.60 (0.35–1.03) | 0.62 (0.36–1.06) | 0.61 (0.24–1.55) | 0.57 (0.22–1.47) |
| Complete Revascularization | 0.73 (0.44–1.21) | 0.70 (0.42–1.16) | 0.61 (0.26–1.45) | 0.69 (0.28–1.70) |
| LDL-C, mg/dL | 1.01 (1.00–1.02) | 1.01 (1.00–1.02) | 1.00 (0.99–1.02) | 1.00 (0.99–1.02) |
| HDL-C, mg/dL | 0.99 (0.96–1.02) | 0.99 (0.96–1.02) | 1.01 (0.97–1.06) | 1.01 (0.97–1.06) |
| Triglycerides, mg/dL | 1.00 (1.00.1.01) | 1.00 (1.00–1.01) | 1.00 (1.00–1.01) | 1.00 (1.00–1.01) |
| CKD-EPI <60 mL/min/1.73 m2 | 1.07 (0.55–2.08) | 0.93 (0.47–1.84) | 0.86 (0.31–2.37) | 0.93 (0.32–2.71) |
| Acetylsalicylic acid, yes | 1.48 (0.53–4.11) | 1.43 (0.52–3.93) | 1.29 (0.12–13.4) | 1.57 (0.15–16.5) |
| AntiP2Y12, yes | 1.06 (0.62–1.81) | 1.14 (0.66–1.96) | 0.49 (0.20–1.23) | 0.60 (0.22–1.62) |
| Anticoagulants, yes | 1.43 (0.39–5.26) | 1.31 (0.34–5.08) | 1.01 (0.20–5.22) | 0.87 (0.16–4.84) |
| Statins, yes | 0.67 (0.30–1.50) | 0.68 (0.30–1.54) | 0.49 (0.14–1.73) | 0.61 (0.15–2.53) |
| ACE inhibitors, yes | 0.80 (0.45–1.41) | 0.75 (0.42–1.33) | 0.34 (0.14–0.83) | 0.35 (0.14–0.87) |
| ARB, yes | 1.38 (0.71–2.71) | 1.26 (0.63–2.51) | 0.77 (0.26–2.26) | 0.57 (0.17–1.82) |
| Anti-aldosterone, yes | 1.06 (0.38–2.93) | 0.88 (0.30–2.58) | 1.31 (0.33–5.23) | 1.03 (0.24–4.40) |
| β-Blockers, yes | 1.10 (0.59–2.06) | 1.16 (0.61–2.20) | 0.99 (0.42–2.33) | 0.87 (0.36–2.06) |
| Nitrates, yes | 1.42 (0.75–2.67) | 1.27 (0.66–2.44) | 1.33 (0.53–3.34) | 1.10 (0.42–2.87) |
| Diuretics, yes | 0.93 (0.49–1.75) | 0.99 (0.52–1.88) | 0.77 (0.31–1.94) | 0.66 (0.23–1.89) |
| Insulin, yes | - | - | 2.37 (1.05–5.34) | 2.29 (0.95–5.53) |
| Oral antidiabetic drugs, yes | - | - | 0.70 (0.30–1.60) | 0.73 (0.30–1.80) |
| Hs-CRP, mg/L | 0.97 (0.92–1.03) | 0.96 (0.91–1.02) | 0.97 (0.93–1.02) | 0.97 (0.93–1.03) |
| NT-proBNP, 1-SD | - | 1.15 (0.89–1.47) | - | 0.95 (0.68–1.33) |
| MCP-1, 1-SD | - | 1.23 (1.01–1.49) | - | 0.78 (0.44–1.38) |
| Gal-3, 1-SD | - | 1.07 (0.87–1.31) | - | 1.83 (1.13–2.98) |
| Hs-cTnT, 1-SD | - | 1.18 (0.35–3.96) | - | 1.02 (0.84–1.23) |
| Nondiabetic Patients | Diabetic Patients | |||
|---|---|---|---|---|
| Variable | Model 1 | Model 2 | Model 1 | Model 2 |
| HR (95% CI) | HR (95% CI) | HR (95% CI) | HR (95% CI) | |
| Age, years | 1.12 (1.08–1.15) | 1.11 (1.07–1.15) | 1.10 (1.05–1.16) | 1.10 (1.04–1.15) |
| Sex, male | 1.27 (0.53–3.05) | 1.50 (0.60–3.78) | 0.57 (0.16–1.97) | 0.87 (0.22–3.40) |
| Smoker, yes | 0.49 (0.22–1.10) | 0.57 (0.24–1.33) | 2.58 (0.70–9.55) | 3.55 (0.79–15.9) |
| Hypertension, yes | 1.31 (0.60–2.85) | 1.19 (0.53–2.68) | 1.50 (0.28–8.08) | 2.02 (0.38–10.8) |
| Body mass index, kg/m2 | 1.00 (1.00–1.00) | 1.00 (1.00–1.00) | 1.01 (0.98–1.03) | 1.00 (0.97–1.03) |
| History of CVE, yes | 2.30 (0.57–9.18) | 2.70 (0.68–10.8) | 10.2 (1.31–80.2) | 10.0 (0.98–102.8) |
| Ejection fraction <40%, yes | 3.31 (1.54–7.11) | 2.14 (0.89–5.12) | 0.34 (0.08–1.45) | 0.48 (0.12–1.96) |
| Atrial Fibrillation, yes | 1.00 (0.33–3.05) | 0.70 (0.21–2.36) | 6.49 (1.04–40.4) | 8.84 (1.07–73.7) |
| Acute myocardial infarction, yes | 1.00 (0.52–1.93) | 0.86 (0.43–1.69) | 2.38 (0.78–7.19) | 2.02 (0.66–6.15) |
| Complete Revascularization | 0.71 (0.37–1.38) | 0.65 (0.33–1.30) | 1.43 (0.50–4.05) | 1.31 (0.47–3.66) |
| LDL-C, mg/dL | 0.99 (0.98–1.01) | 0.99 (0.98–1.01) | 0.97 (0.95–0.99) | 0.97 (0.95–0.99) |
| HDL-C, mg/dL | 1.04 (0.98–1.07) | 1.03 (0.98–1.05) | 1.00 (0.95–1.05) | 0.99 (0.94–1.04) |
| Triglycerides, mg/dL | 1.00 (0.99–1.00) | 1.00 (0.99–1.00) | 1.00 (0.99–1.01) | 1.00 (0.99–1.01) |
| CKD-EPI <60 mL/min/1.73 m2 | 0.85 (0.44–1.65) | 0.99 (0.98–1.01) | 1.33 (0.50–3.54) | 0.86 (0.29–2.50) |
| Acetylsalicylic acid, yes | 0.95 (0.40–2.27) | 0.73 (0.29–1.82) | 0.31 (0.04–2.48) | 0.44 (0.05–3.83) |
| AntiP2Y12, yes | 0.93 (0.49–1.76) | 0.94 (0.49–1.82) | 0.43 (0.13–1.35) | 0.36 (0.10–1.22) |
| Anticoagulants, yes | 1.36 (0.47–4.00) | 1.12 (0.33–3.79) | 15.9 (1.62–157.0) | 33.32 (2.46-450.5) |
| Statins, yes | 0.35 (0.14–0.84) | 0.29 (0.11–0.76) | 0.90 (0.14–5.55) | 0.84 (0.10–7.21) |
| ACE inhibitors, yes | 1.05 (0.48–2.27) | 1.30 (0.54–3.12) | 0.98 (0.29–3.25) | 0.72 (0.20–2.59) |
| ARB, yes | 0.40 (0.14–1.14) | 0.51 (0.17–1.55) | 1.13 (0.29–4.47) | 0.74 (0.16–3.52) |
| Anti-aldosterone, yes | 0.47 (0.15–1.44) | 0.60 (0.18–1.99) | 10.2 (2.82–39.9) | 7.59 (1.66–34.7) |
| β-Blockers, yes | 0.64 (0.34–1.23) | 0.60 (0.30–1.18) | 0.88 (0.32–2.46) | 0.90 (0.32–2.57) |
| Nitrates, yes | 1.02 (0.44–1.65) | 0.83 (0.36–1.91) | 3.86 (1.16–12.8) | 4.05 (1.20–13.6) |
| Diuretics, yes | 2.02 (1.05–3.87) | 1.59 (0.78–3.24) | 1.84 (0.56–6.02) | 1.32 (0.37–4.72) |
| Insulin, yes | - | - | 2.82 (1.03–7.72) | 2.59 (0.81–8.31) |
| Oral antidiabetic drugs, yes | - | - | 2.25 (0.71–7.14) | 1.88 (0.53–6.75) |
| Hs-CRP, mg/L | 0.99 (0.95–1.03) | 1.00 (0.96–1.03) | 0.97 (0.92–1.02) | 0.96 (0.90–1.02) |
| NT-proBNP, 1-SD | - | 1.29 (1.07–1.56) | - | 1.29 (0.91–1.83) |
| MCP-1, 1-SD | - | 1.14 (0.90–1.45) | - | 0.89 (0.47–1.67) |
| Gal-3, 1-SD | - | 1.22 (0.96–1.56) | - | 2.14 (1.17–3.91) |
| Hs-cTnT, 1-SD | - | 2.45 (0.73–8.21) | - | 0.96 (0.78–1.17) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lorenzo-Almorós, A.; Pello, A.; Aceña, Á.; Martínez-Milla, J.; González-Lorenzo, Ó.; Tarín, N.; Cristóbal, C.; Blanco-Colio, L.M.; Martín-Ventura, J.L.; Huelmos, A.; et al. Galectin-3 is Associated with Cardiovascular Events in Post-Acute Coronary Syndrome Patients with Type-2 Diabetes. J. Clin. Med. 2020, 9, 1105. https://doi.org/10.3390/jcm9041105
Lorenzo-Almorós A, Pello A, Aceña Á, Martínez-Milla J, González-Lorenzo Ó, Tarín N, Cristóbal C, Blanco-Colio LM, Martín-Ventura JL, Huelmos A, et al. Galectin-3 is Associated with Cardiovascular Events in Post-Acute Coronary Syndrome Patients with Type-2 Diabetes. Journal of Clinical Medicine. 2020; 9(4):1105. https://doi.org/10.3390/jcm9041105
Chicago/Turabian StyleLorenzo-Almorós, Ana, Ana Pello, Álvaro Aceña, Juan Martínez-Milla, Óscar González-Lorenzo, Nieves Tarín, Carmen Cristóbal, Luis M Blanco-Colio, José Luis Martín-Ventura, Ana Huelmos, and et al. 2020. "Galectin-3 is Associated with Cardiovascular Events in Post-Acute Coronary Syndrome Patients with Type-2 Diabetes" Journal of Clinical Medicine 9, no. 4: 1105. https://doi.org/10.3390/jcm9041105
APA StyleLorenzo-Almorós, A., Pello, A., Aceña, Á., Martínez-Milla, J., González-Lorenzo, Ó., Tarín, N., Cristóbal, C., Blanco-Colio, L. M., Martín-Ventura, J. L., Huelmos, A., Gutiérrez-Landaluce, C., López-Castillo, M., Kallmeyer, A., Cánovas, E., Alonso, J., López Bescós, L., Egido, J., Lorenzo, Ó., & Tuñón, J. (2020). Galectin-3 is Associated with Cardiovascular Events in Post-Acute Coronary Syndrome Patients with Type-2 Diabetes. Journal of Clinical Medicine, 9(4), 1105. https://doi.org/10.3390/jcm9041105









