Impact of the Geriatric Nutritional Risk Index on In-Hospital Mortality and Length of Hospitalization in Patients with Acute Decompensated Heart Failure with Preserved or Reduced Ejection Fraction
Abstract
1. Introduction
2. Materials and Methods
2.1. Subjects
2.2. Data Collection
2.3. Statistical Analyses
3. Results
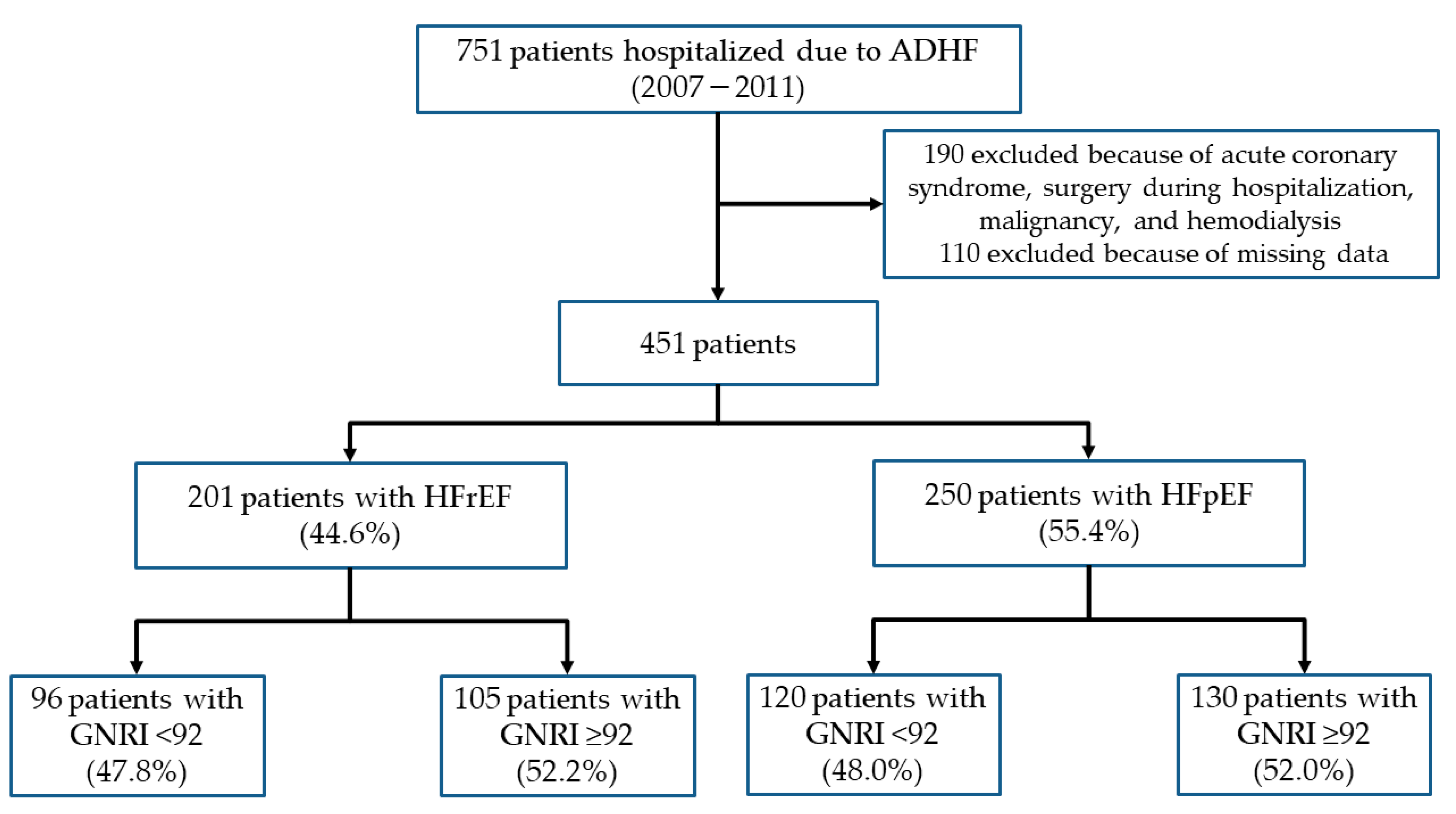
3.1. Study Population
3.2. Heart Failure with Reduced Ejection Fraction
3.2.1. Baseline Characteristics
3.2.2. In-Hospital Mortality
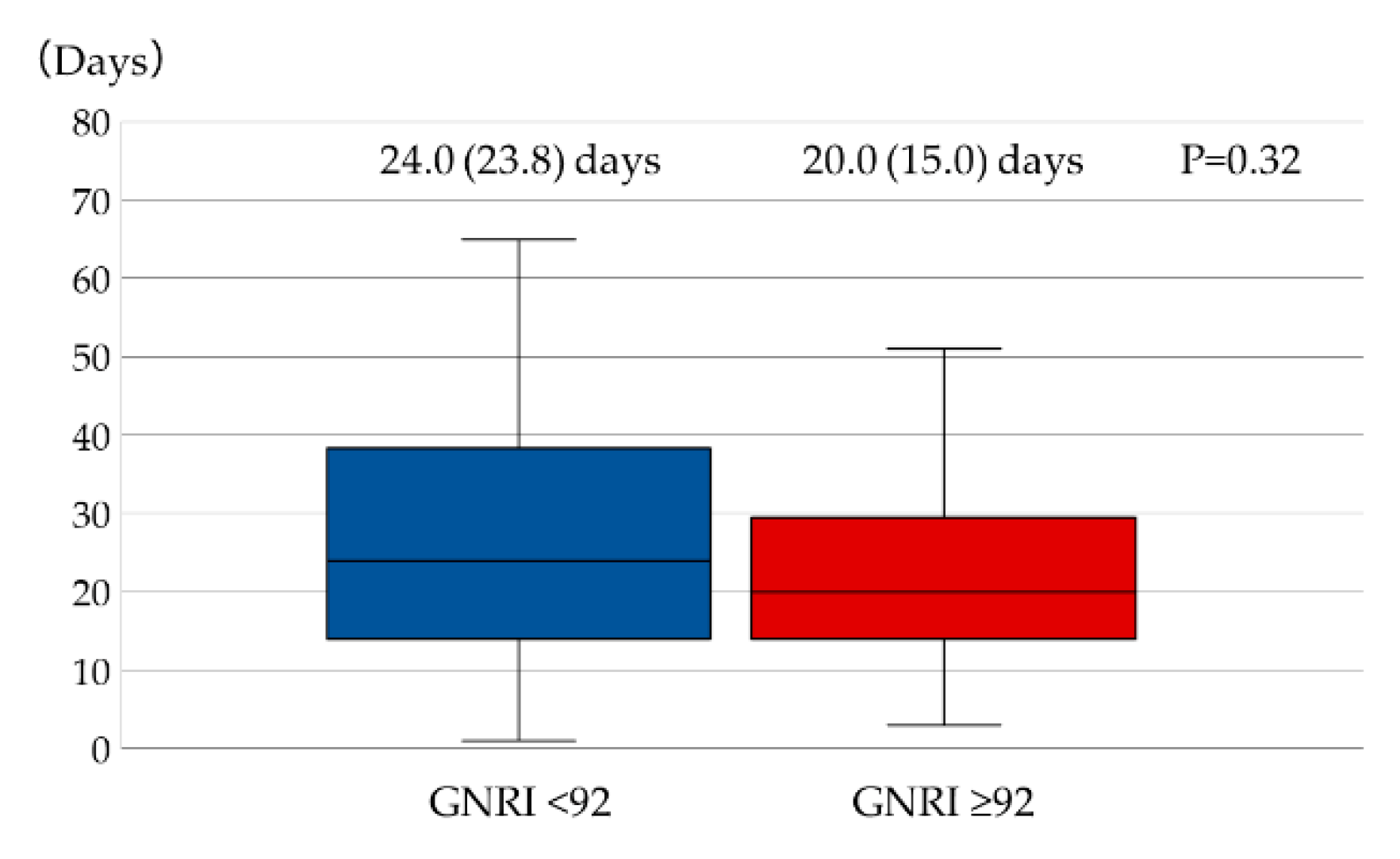
3.2.3. Length of Hospital Stay
3.3. Heart Failure with Preserved Ejection Fraction
3.3.1. Baseline Characteristics
3.3.2. In-Hospital Mortality
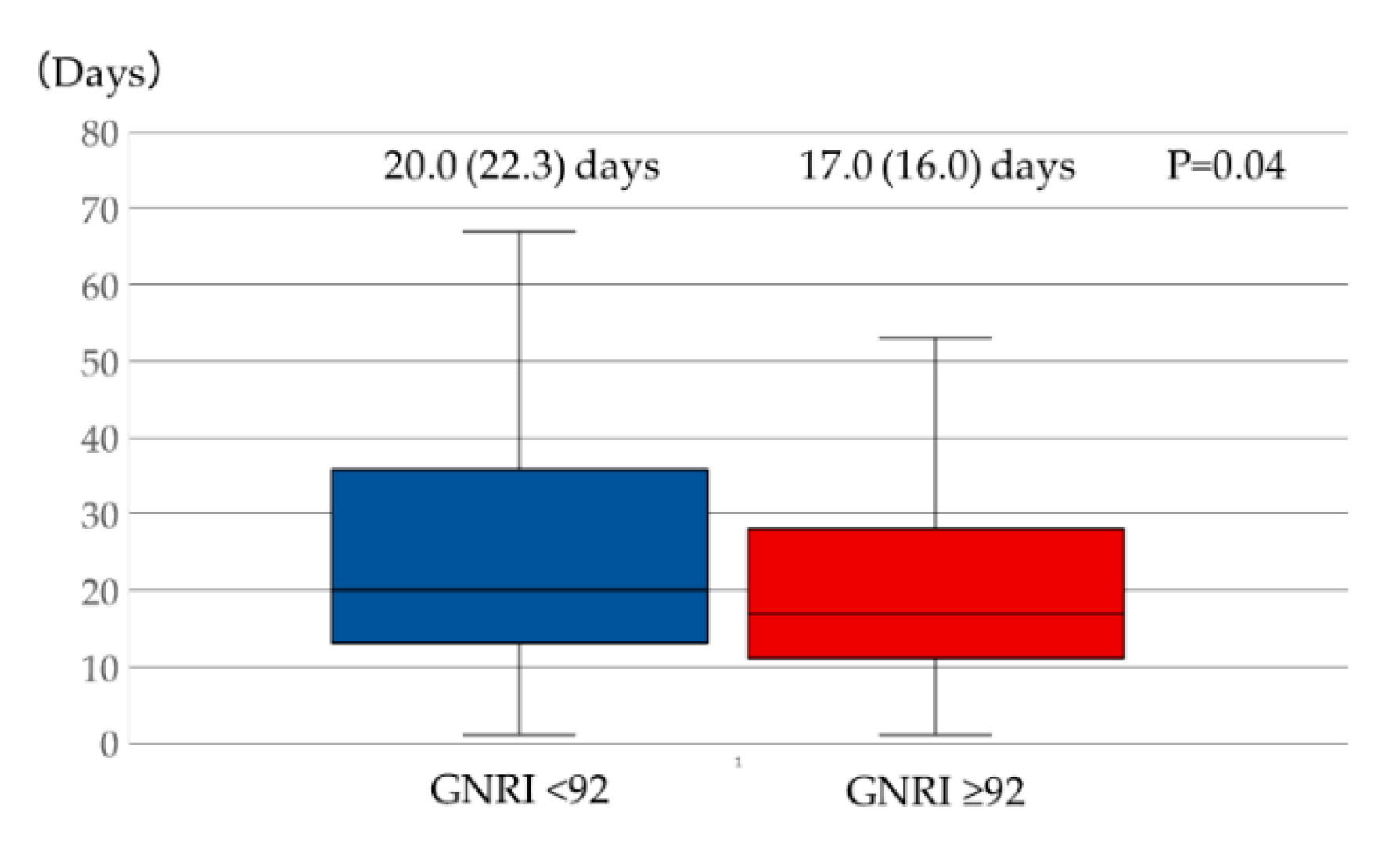
3.3.3. Length of Hospital Stay
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hunt, S.A.; Abraham, W.T.; Chin, M.H.; Feldman, A.M.; Francis, G.S.; Ganiats, T.G.; Jessup, M.; Konstam, M.A.; Mancini, D.M.; Michl, K.; et al. 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: A report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines: Developed in collaboration with the International Society for Heart and Lung Transplantation. J. Am. Coll. Cardiol. 2009, 53, 1–90. [Google Scholar]
- Okura, Y.; Ramadan, M.M.; Ohno, Y.; Mitsuma, W.; Tanaka, K.; Ito, M.; Suzuki, K.; Tanabe, N.; Kodama, M.; Aizawa, Y. Impending epidemic: Future projection of heart failure in Japan to the year 2055. Circ. J. 2008, 72, 489–491. [Google Scholar] [CrossRef] [PubMed]
- Arai, H.; Ouchi, Y.; Toba, K.; Endo, T.; Shimokado, K.; Tsubota, K.; Matsuo, S.; Mori, H.; Yumura, W.; Yokode, M.; et al. Japan as the front-runner of super-aged societies: Perspectives from medicine and medical care in Japan. Geriatr. Gerontol. Int. 2015, 15, 673–687. [Google Scholar] [CrossRef] [PubMed]
- Nojiri, S.; Itoh, H.; Kasai, T.; Fujibayashi, K.; Saito, T.; Hiratsuka, Y.; Okuzawa, A.; Naito, T.; Yokoyama, K.; Daida, H. Comorbidity status in hospitalized elderly in Japan: Analysis from National Database of Health Insurance Claims and Specific Health Checkups. Sci. Rep. 2019, 9, 20237. [Google Scholar] [CrossRef] [PubMed]
- Shiraishi, Y.; Kohsaka, S.; Sato, N.; Takano, T.; Kitai, T.; Yoshikawa, T.; Matsue, Y. 9-year trend in the management of acute heart failure in Japan: A report from the National Consortium of Acute Heart Failure Registries. J. Am. Heart Assoc. 2018, 7, e008687. [Google Scholar] [CrossRef] [PubMed]
- Yatsu, S.; Kasai, T.; Suda, S.; Matsumoto, H.; Shiroshita, N.; Kato, M.; Kawana, F.; Murata, A.; Kato, T.; Hiki, M.; et al. Impact on clinical outcomes of periodic leg movements during sleep in hospitalized patients following acute decompensated heart failure. Circ. J. 2017, 81, 495–500. [Google Scholar] [CrossRef]
- Suda, S.; Kasai, T.; Matsumoto, H.; Shiroshita, N.; Kato, M.; Kawana, F.; Yatsu, S.; Murata, A.; Kato, T.; Hiki, M.; et al. Prevalence and clinical correlates of sleep-disordered breathing in patients hospitalized with acute decompensated heart failure. Can. J. Cardiol. 2018, 34, 784–790. [Google Scholar] [CrossRef]
- Ambrosy, A.P.; Fonarow, G.C.; Butler, J.; Chioncel, O.; Greene, S.J.; Vaduganathan, M.; Nodari, S.; Lam, C.S.P.; Sato, N.; Shah, A.N.; et al. The global health and economic burden of hospitalizations for heart failure: Lessons learned from hospitalized heart failure registries. J. Am. Coll. Cardiol. 2014, 63, 1123–1133. [Google Scholar] [CrossRef]
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; González-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar]
- Lin, H.; Zhang, H.; Lin, Z.; Li, X.; Kong, X.; Sun, G. Review of nutritional screening and assessment tools and clinical outcomes in heart failure. Heart Fail Rev. 2016, 21, 549–565. [Google Scholar] [CrossRef]
- Honda, Y.; Nagai, T.; Iwakami, N.; Sugano, Y.; Honda, S.; Okada, A.; Asaumi, Y.; Aiba, T.; Noguchi, T.; Kusano, K.; et al. Usefulness of Geriatric Nutritional Risk Index for assessing nutritional status and its prognostic impact in patients aged ≥65 years with acute heart failure. Am. J. Cardiol. 2016, 118, 550–555. [Google Scholar] [CrossRef] [PubMed]
- Bouillanne, O.; Morineau, G.; Dupont, C.; Coulombel, I.; Vincent, J.P.; Nicolis, I.; Benazeth, S.; Cynober, L.; Aussel, C. Geriatric Nutritional Risk Index: A new index for evaluating at-risk elderly medical patients. Am. J. Clin. Nutr. 2005, 82, 777–783. [Google Scholar] [CrossRef] [PubMed]
- McKee, P.A.; Castelli, W.P.; McNamara, P.M.; Kannel, W.B. The natural history of congestive heart failure: The Framingham study. N. Engl. J. Med. 1971, 285, 1441–1446. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, S.; Pfeffer, M.A.; Swedberg, K.; Granger, C.B.; Held, P.; McMurray, J.J.; Michelson, E.L.; Olofsson, B.; Ostergren, J.; CHARM Investigators and Committees. Effects of candesartan in patients with chronic heart failure and preserved left-ventricular ejection fraction: The CHARM-Preserved Trial. Lancet 2003, 362, 777–781. [Google Scholar] [CrossRef]
- Matsuo, S.; Imai, E.; Horio, M.; Yasuda, Y.; Tomita, K.; Nitta, K.; Yamagata, K.; Tomino, Y.; Yokoyama, H.; Hishida, A.; et al. Revised equations for estimated GFR from serum creatinine in Japan. Am. J. Kidney Dis. 2009, 53, 982–992. [Google Scholar] [CrossRef]
- Mac Giollabhui, N.; Ellman, L.M.; Coe, C.L.; Byrne, M.L.; Abramson, L.Y.; Alloy, L.B. To exclude or not to exclude: Considerations and recommendations for C-reactive protein values higher than 10 mg/L. Brain Behav. Immun. 2020, in press. [Google Scholar] [CrossRef]
- Horwich, T.B.; Kalantar-Zadeh, K.; MacLellan, R.W.; Fonarow, G.C. Albumin levels predict survival in patients with systolic heart failure. Am. Heart J. 2008, 155, 883–889. [Google Scholar] [CrossRef]
- Liu, M.; Chan, C.P.; Yan, B.P.; Zhang, Q.; Lam, Y.Y.; Li, R.J.; Sanderson, J.E.; Coats, A.J.; Sun, J.P.; Yip, G.W.; et al. Albumin levels predict survival in patients with heart failure and preserved ejection fraction. Eur. J. Heart Fail. 2012, 14, 39–44. [Google Scholar] [CrossRef]
- Shah, R.; Gayat, E.; Januzzi, J.L., Jr.; Sato, N.; Cohen-Solal, A.; diSomma, S.; Fairman, E.; Harjola, V.P.; Ishihara, S.; Lassus, J.; et al. Body mass index and mortality in acutely decompensated heart failure worldwide: A global obesity paradox. J. Am. Coll. Cardiol. 2014, 63, 778–785. [Google Scholar] [CrossRef]
- Cheng, Y.L.; Sung, S.H.; Cheng, H.M.; Hsu, P.F.; Guo, C.Y.; Yu, W.C.; Chen, C.H. Prognostic nutritional index and the risk of mortality in patients with acute heart failure. J. Am. Heart Assoc. 2017, 6, e004876. [Google Scholar] [CrossRef]
- Iwakami, N.; Nagai, T.; Furukawa, T.A.; Sugano, Y.; Honda, S.; Okada, A.; Asaumi, Y.; Aiba, T.; Noguchi, T.; Kusano, K.; et al. Prognostic value of malnutrition assessed by Controlling Nutritional Status score for long-term mortality in patients with acute heart failure. Int. J. Cardiol. 2017, 230, 529–536. [Google Scholar] [CrossRef] [PubMed]
- Shirakabe, A.; Hata, N.; Kobayashi, N.; Okazaki, H.; Matsushita, M.; Shibata, Y.; Nishigoori, S.; Uchiyama, S.; Asai, K.; Shimizu, W. The prognostic impact of malnutrition in patients with severely decompensated acute heart failure, as assessed using the Prognostic Nutritional Index (PNI) and Controlling Nutritional Status (CONUT) score. Heart Vessel. 2018, 33, 134–144. [Google Scholar] [CrossRef] [PubMed]
- Sze, S.; Pellicori, P.; Kazmi, S.; Rigby, A.; Cleland, J.G.F.; Wong, K.; Clark, A.L. Prevalence and prognostic significance of malnutrition using 3 scoring systems among outpatients with heart failure: A comparison with body mass index. JACC Heart Fail. 2018, 6, 476–486. [Google Scholar] [CrossRef]
- Kinugasa, Y.; Kato, M.; Sugihara, S.; Hirai, M.; Yamada, K.; Yanagihara, K.; Yamamoto, K. Geriatric nutritional risk index predicts functional dependency and mortality in patients with heart failure with preserved ejection fraction. Circ. J. 2013, 77, 705–711. [Google Scholar] [CrossRef] [PubMed]
- Yoshihisa, A.; Kanno, Y.; Watanabe, S.; Yokokawa, T.; Abe, S.; Miyata, M.; Sato, T.; Suzuki, S.; Oikawa, M.; Kobayashi, A.; et al. Impact of nutritional indices on mortality in patients with heart failure. Open Heart 2018, 5, e000730. [Google Scholar] [CrossRef] [PubMed]
- Aziz, E.F.; Javed, F.; Pratap, B.; Musat, D.; Nader, A.; Pulimi, S.; Alivar, C.L.; Herzog, E.; Kukin, M.L. Malnutrition as assessed by nutritional risk index is associated with worse outcome in patients admitted with acute decompensated heart failure: An ACAP-HF data analysis. Heart Int. 2011, 6, e2. [Google Scholar] [CrossRef]
- Nishino, M.; Matsuhiro, Y.; Nakamura, H.; Yasumoto, K.; Yasumura, K.; Tanaka, A.; Matsunaga-Lee, Y.; Nakamura, D.; Yano, M.; Yamato, M.; et al. Which factors are associated with length of stay in older patients with acute decompensated heart failure with preserved ejection fraction?: AURORA study. Geriatr. Gerontol. Int. 2019, 19, 1084–1087. [Google Scholar] [CrossRef]
- Goyal, P.; Almarzooq, Z.I.; Horn, E.M.; Karas, M.G.; Sobol, I.; Swaminathan, R.V.; Feldman, D.N.; Minutello, R.M.; Singh, H.S.; Bergman, G.W.; et al. Characteristics of hospitalizations for heart failure with preserved ejection fraction. Am. J. Med. 2016, 129, 635.e15–635.e26. [Google Scholar] [CrossRef]
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E., Jr.; Colvin, M.M.; Drazner, M.H.; Filippatos, G.S.; Fonarow, G.C.; Givertz, M.M.; et al. 2017 ACC/AHA/HFSA focused update of the 2013 ACCF/AHA guideline for the management of heart failure: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation 2017, 136, e137–e161. [Google Scholar]
| Total (n = 201) | GNRI < 92 (n = 96) | GNRI ≥ 92 (n = 105) | p | |
|---|---|---|---|---|
| Age, years | 67.1 ± 14.3 | 71.0 ± 12.0 | 63.6 ± 15.3 | <0.01 |
| Male sex | 142 (70.7) | 66 (68.8) | 76 (72.4) | 0.64 |
| Body mass index, kg/m2 | 23.0 ± 5.2 | 20.5 ± 3.4 | 25.2 ± 5.6 | <0.01 |
| Current smoker | 104 (51.7) | 54 (56.2) | 50 (47.6) | 0.26 |
| Hypertension | 141 (70.2) | 65 (67.7) | 76 (72.4) | 0.54 |
| Diabetes mellitus | 76 (37.8) | 40 (41.7) | 36 (34.3) | 0.31 |
| Ischemic etiology | 88 (43.8) | 46 (47.9) | 42 (40.0) | 0.32 |
| Atrial fibrillation | 65 (32.3) | 30 (31.2) | 35 (33.3) | 0.77 |
| Prior HF hospitalization | 111 (55.2) | 51 (53.1) | 60 (57.1) | 0.57 |
| LVEF, % | 27.1 ± 6.9 | 27.1 ± 7.1 | 27.0 ± 6.8 | 0.87 |
| NYHA class ≥ III | 175 (87.6) | 85 (88.5) | 90 (85.7) | 0.68 |
| Serum albumin, mg/dL | 3.3 ± 0.6 | 2.9 ± 0.5 | 3.7 ± 0.4 | <0.01 |
| Serum sodium, mmol/L | 138.6 ± 4.2 | 138.2 ± 4.3 | 138.9 ± 4.1 | 0.27 |
| Serum potassium, mmol/L | 4.2 ± 0.6 | 4.3 ± 0.8 | 4.2 ± 0.5 | 0.33 |
| Hemoglobin, g/dL | 13.0 ± 2.6 | 12.4 ± 2.6 | 13.5 ± 2.4 | <0.01 |
| eGFR, mL/min/1.73 m2 | 54.5 ± 26.2 | 52.0 ± 27.2 | 56.7 ± 25.1 | 0.20 |
| BNP, pg/dL | 1106.3 (770.0) | 1269.4 (893.6) | 950.0 (683.6) | <0.01 |
| CRP, mg/dL | 3.5 (0.9) | 4.1 (1.0) | 3.0 (0.9) | 0.21 |
| Elevated CRP | 91 (45.3) | 45 (46.9) | 46 (43.8) | 0.88 |
| GNRI | 93.1 ± 13.6 | 82.2 ± 6.7 | 103.1 ± 10.3 | <0.01 |
| Medications | ||||
| ACE-Is/ARBs | 70 (34.8) | 28 (29.2) | 42 (40.0) | 0.14 |
| Aldosterone blockers | 36 (17.9) | 19 (19.8) | 17 (16.2) | 0.58 |
| β-blockers | 69 (34.3) | 31 (32.3) | 38 (36.2) | 0.66 |
| Diuretics | 86 (42.8) | 47 (49.0) | 39 (37.1) | 0.12 |
| Variables | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| GNRI < 92 (yes) | 2.94 | 0.89–9.70 | 0.08 | - | - | - |
| Diuretics (yes) | 2.57 | 0.83–7.97 | 0.10 | - | - | - |
| Serum sodium (1 mmol/L increase) | 0.79 | 0.70–0.89 | <0.01 | 0.81 | 0.71–0.91 | <0.01 |
| Hemoglobin (1 g/dL increase) | 0.74 | 0.59–0.93 | <0.01 | 0.78 | 0.61–1.00 | 0.04 |
| Variables | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| GNRI < 92 (yes) | 1.62 | 0.91–2.88 | 0.11 | - | - | - |
| NYHA class ≥ III (yes) | 5.32 | 1.74–16.2 | <0.01 | 4.83 | 1.57–14.9 | <0.01 |
| Serum potassium (1 mmol/L increase) | 1.76 | 1.03–2.99 | 0.04 | - | - | - |
| Serum sodium (1 mmol/L increase) | 0.89 | 0.82–0.97 | <0.01 | 0.90 | 0.83–0.98 | 0.01 |
| Hemoglobin (1 g/dL increase) | 0.84 | 0.74–0.94 | <0.01 | - | - | - |
| eGFR (1 mL/min/1.73 m2 increase) | 0.99 | 0.98–1.00 | 0.10 | - | - | - |
| Total (n = 250) | GNRI < 92 (n = 120) | GNRI ≥ 92 (n = 130) | p | |
|---|---|---|---|---|
| Age, years | 71.5 ± 13.1 | 74.1 ± 12.6 | 69.0 ± 13.3 | <0.01 |
| Male sex | 154 (61.6) | 71 (59.2) | 83 (63.8) | 0.51 |
| Body mass index, kg/m2 | 22.8 ± 4.4 | 20.2 ± 3.1 | 25.2 ± 4.2 | <0.01 |
| Current smoker | 108 (43.2) | 53 (44.2) | 55 (42.3) | 0.80 |
| Hypertension | 195 (78.0) | 90 (75.0) | 105 (80.8) | 0.29 |
| Diabetes mellitus | 102 (40.8) | 45 (37.5) | 57 (43.8) | 0.37 |
| Ischemic etiology | 92 (36.8) | 41 (34.2) | 51 (39.2) | 0.43 |
| Atrial fibrillation | 96 (38.4) | 45 (37.5) | 51 (39.2) | 0.80 |
| Prior HF hospitalization | 134 (53.6) | 66 (55.0) | 68 (52.3) | 0.70 |
| LVEF, % | 56.0 (38.4) | 55.6 (11.6) | 56.3 (11.1) | 0.67 |
| NYHA class ≥ III | 202 (80.8) | 97 (80.8) | 105 (80.8) | 1.00 |
| Serum creatinine, mg/dL | 1.3 ± 1.0 | 1.4 ± 1.2 | 1.2 ± 0.8 | 0.11 |
| Serum albumin, mg/dL | 3.3 ± 0.6 | 2.9 ± 0.5 | 3.6 ± 0.5 | <0.01 |
| Serum potassium, mmol/L | 4.2 ± 0.7 | 4.2 ± 0.7 | 4.2 ± 0.7 | 0.92 |
| Serum sodium, mmol/L | 138.8 ± 4.2 | 138.4 ± 4.3 | 139.1 ± 4.2 | 0.22 |
| Hemoglobin, g/dL | 11.9 ± 2.5 | 11.7 ± 2.4 | 12.1 ± 2.5 | 0.20 |
| eGFR, mL/min/1.73 m2 | 53.7 ± 27.4 | 53.3 ± 30.9 | 54.1 ± 23.8 | 0.80 |
| BNP, pg/dL | 757.9 (517.6) | 820.0 (553.6) | 706.0 (462.5) | 0.10 |
| CRP, mg/dL | 3.3 (0.9) | 3.8 (0.9) | 2.9 (0.7) | 0.15 |
| Elevated CRP | 109 (43.6) | 55 (45.8) | 54 (41.5) | 0.21 |
| GNRI | 92.3 ± 12.5 | 82.0 ± 7.1 | 101.8±8.2 | <0.01 |
| Medications | ||||
| ACE-Is/ARBs | 103 (41.2) | 45 (37.5) | 58 (44.6) | 0.30 |
| Aldosterone blockers | 28 (11.2) | 13 (10.8) | 15 (11.5) | 1.00 |
| β-blockers | 72 (28.8) | 30 (25.0) | 42 (32.3) | 0.21 |
| Diuretics | 93 (37.2) | 46 (38.3) | 47 (36.2) | 0.79 |
| Variables | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Age (1-year increase) | 1.04 | 1.00–1.08 | 0.03 | - | - | - |
| Diabetes mellitus (yes) | 2.32 | 1.03–5.23 | 0.04 | - | - | - |
| Atrial fibrillation (yes) | 0.42 | 0.16–1.09 | 0.07 | - | - | - |
| Prior HF hospitalization (yes) | 3.41 | 1.32–8.77 | 0.01 | 3.10 | 1.19–8.10 | 0.02 |
| Serum sodium (1 mmol/L increase) | 0.91 | 0.84–1.00 | 0.04 | - | - | - |
| Hemoglobin (1 g/dL increase) | 0.78 | 0.65–0.93 | <0.01 | - | - | - |
| eGFR (1 mL/min/1.73 m2 increase) | 0.97 | 0.96–0.99 | <0.01 | 0.97 | 0.96–0.99 | <0.01 |
| Variables | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p | OR | 95% CI | p | |
| Male sex | 0.66 | 0.38–1.14 | 0.14 | |||
| GNRI < 92 (yes) | 1.71 | 1.01–2.92 | <0.05 | 1.91 | 1.00–3.65 | <0.05 |
| Hypertension (yes) | 0.50 | 0.27–0.95 | 0.04 | |||
| Ischemic etiology (yes) | 0.55 | 0.31–0.97 | 0.04 | |||
| Diuretics (yes) | 1.56 | 0.09–2.70 | 0.11 | |||
| Serum potassium (1 mmol/L increase) | 0.72 | 0.48–1.08 | 0.12 | |||
| Hemoglobin (1 g/dL increase) | 0.84 | 0.74–0.94 | <0.01 | 0.83 | 0.72–0.95 | <0.01 |
| Log-transformed BNP (1 pg/dL increase) | 2.57 | 1.36–4.85 | <0.01 | 2.06 | 1.03–4.12 | 0.04 |
| Elevated CRP (yes) | 2.85 | 1.62–5.01 | <0.01 | 3.03 | 1.59–5.78 | <0.01 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hirose, S.; Miyazaki, S.; Yatsu, S.; Sato, A.; Ishiwata, S.; Matsumoto, H.; Shitara, J.; Murata, A.; Kato, T.; Suda, S.; et al. Impact of the Geriatric Nutritional Risk Index on In-Hospital Mortality and Length of Hospitalization in Patients with Acute Decompensated Heart Failure with Preserved or Reduced Ejection Fraction. J. Clin. Med. 2020, 9, 1169. https://doi.org/10.3390/jcm9041169
Hirose S, Miyazaki S, Yatsu S, Sato A, Ishiwata S, Matsumoto H, Shitara J, Murata A, Kato T, Suda S, et al. Impact of the Geriatric Nutritional Risk Index on In-Hospital Mortality and Length of Hospitalization in Patients with Acute Decompensated Heart Failure with Preserved or Reduced Ejection Fraction. Journal of Clinical Medicine. 2020; 9(4):1169. https://doi.org/10.3390/jcm9041169
Chicago/Turabian StyleHirose, Susumu, Sakiko Miyazaki, Shoichiro Yatsu, Akihiro Sato, Sayaki Ishiwata, Hiroki Matsumoto, Jun Shitara, Azusa Murata, Takao Kato, Shoko Suda, and et al. 2020. "Impact of the Geriatric Nutritional Risk Index on In-Hospital Mortality and Length of Hospitalization in Patients with Acute Decompensated Heart Failure with Preserved or Reduced Ejection Fraction" Journal of Clinical Medicine 9, no. 4: 1169. https://doi.org/10.3390/jcm9041169
APA StyleHirose, S., Miyazaki, S., Yatsu, S., Sato, A., Ishiwata, S., Matsumoto, H., Shitara, J., Murata, A., Kato, T., Suda, S., Matsue, Y., Hiki, M., Takagi, A., Daida, H., & Kasai, T. (2020). Impact of the Geriatric Nutritional Risk Index on In-Hospital Mortality and Length of Hospitalization in Patients with Acute Decompensated Heart Failure with Preserved or Reduced Ejection Fraction. Journal of Clinical Medicine, 9(4), 1169. https://doi.org/10.3390/jcm9041169






