Sympatho–Vagal Dysfunction in Patients with End-Stage Lung Disease Awaiting Lung Transplantation
Abstract
1. Introduction
2. Materials and Methods
2.1. Sample
2.2. Experimental Design
2.3. Lung Disease Severity and Autonomic Modulation
2.4. Heart Rate Variability Analysis
2.5. Statistical Analysis
3. Results
3.1. Study Populations
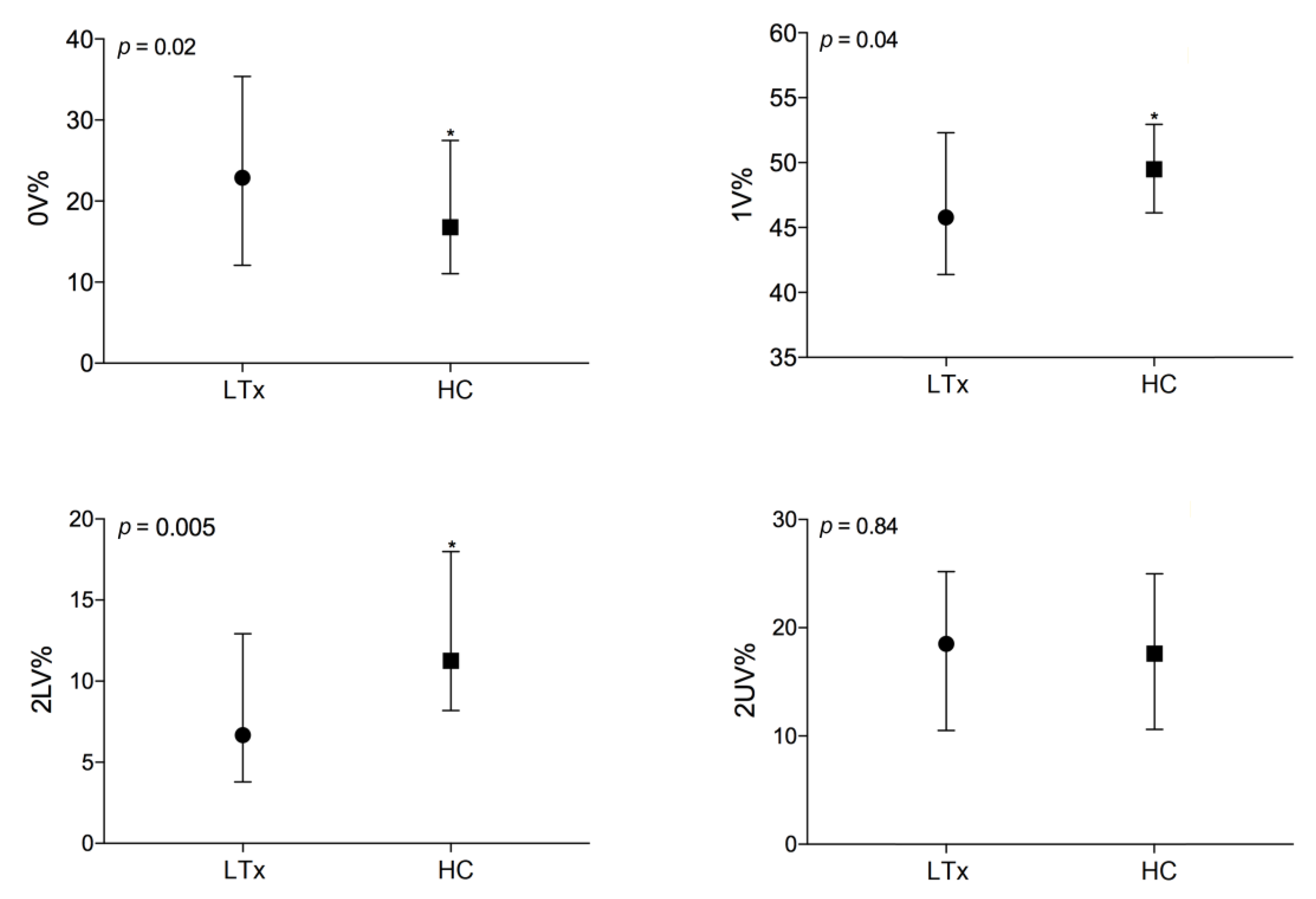
3.2. Autonomic Evaluation of End-Stage Lung Disease Patients vs. Healthy Controls
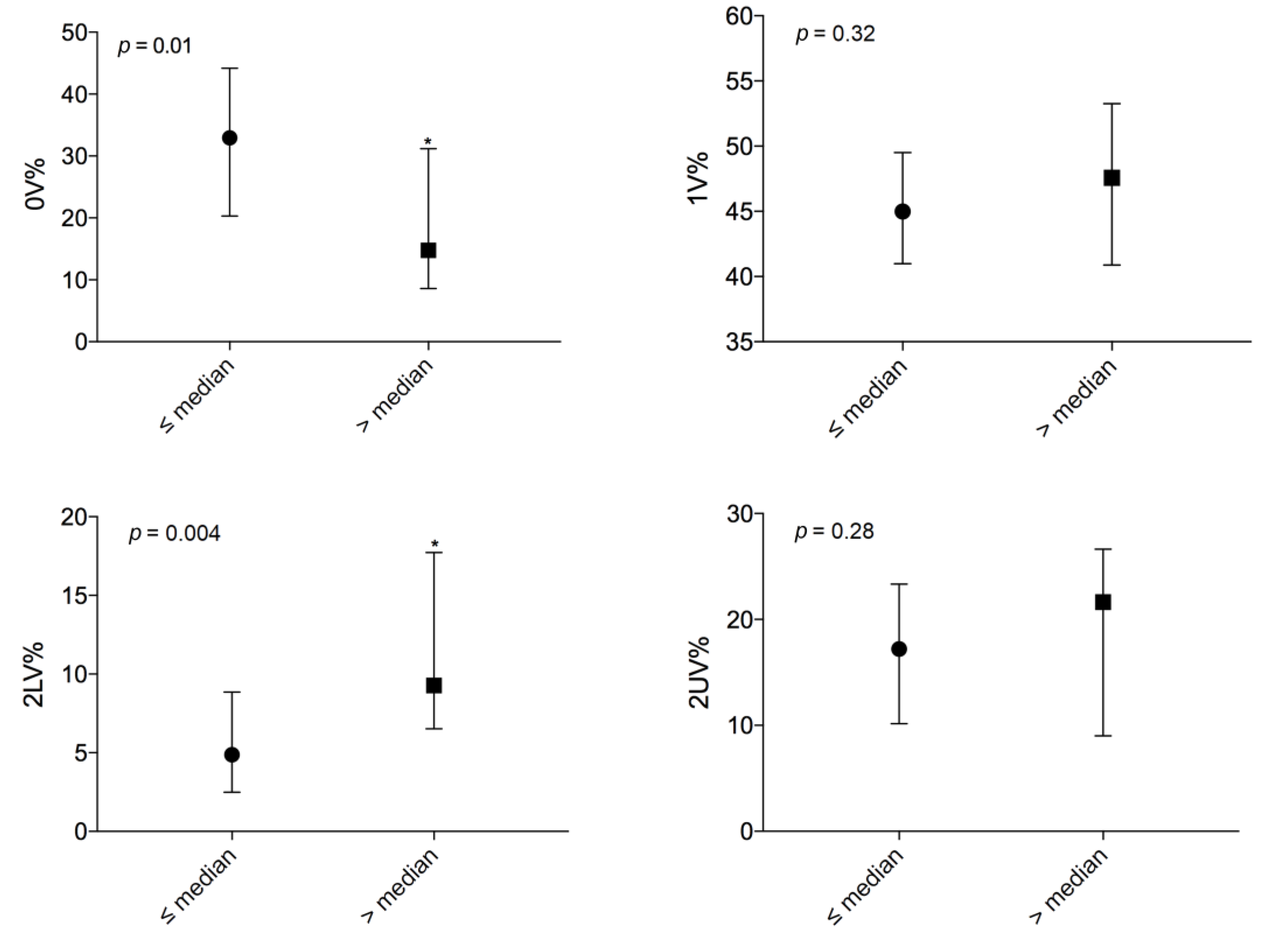
3.3. Autonomic Evaluation Among End-Stage Lung Disease Patients According to Disease Severity
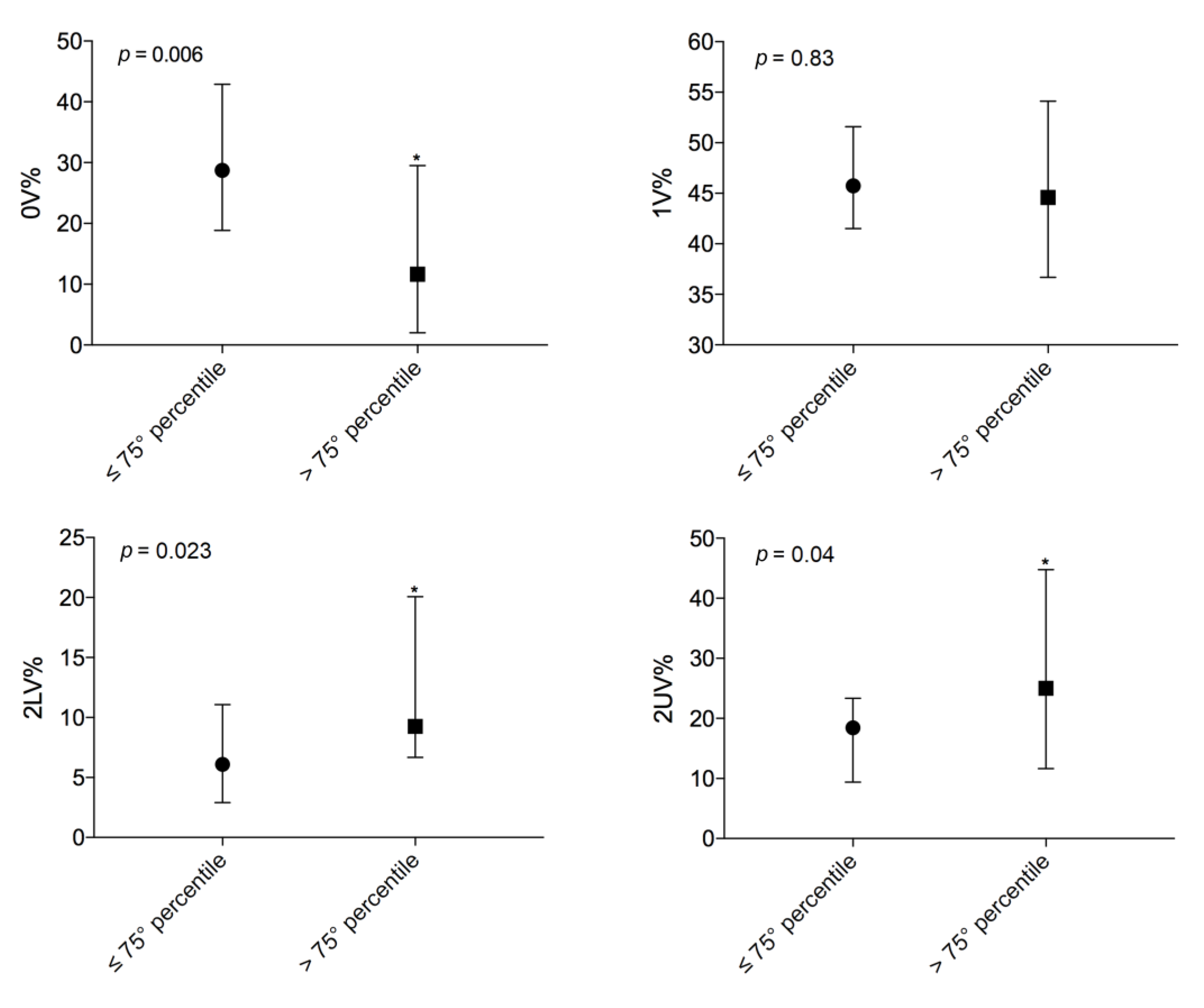
3.4. Comparison Above and Below the 75th Percentile LAS
3.5. Cardiac Autonomic Control during the Active Standing Test
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Selimovic, N.; Andersson, B.; Bergh, C.-H.; Mårtensson, G.; Nilsson, F.; Bech-Hanssen, O.; Rundqvist, B. Pulmonary Hemodynamics as Predictors of Mortality in Patients Awaiting Lung Transplantation. Transpl. Int. Off. J. Eur. Soc. Organ Transpl. 2008, 21, 314–319. [Google Scholar] [CrossRef] [PubMed]
- He, W.-X.; Yang, Y.-L.; Xia, Y.; Song, N.; Liu, M.; Zhang, P.; Fan, J.; Jiang, G.-N. Outcomes of Chinese Patients with End-Stage Pulmonary Disease While Awaiting Lung Transplantation: A Single-Center Study. Chin. Med. J. 2016, 129, 3–7. [Google Scholar] [CrossRef] [PubMed]
- Montano, N.; Porta, A.; Cogliati, C.; Costantino, G.; Tobaldini, E.; Casali, K.R.; Iellamo, F. Heart Rate Variability Explored in the Frequency Domain: A Tool to Investigate the Link between Heart and Behavior. Neurosci. Biobehav. Rev. 2009, 33, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Berakis, A.; Williams, T.J.; Naughton, M.T.; Martin, J.H.; Muhlmann, M.; Krum, H. Altered Sympathetic and Parasympathetic Activity in Lung Transplantation Patients at Rest and Following Autonomic Perturbation. Chest 2002, 122, 1192–1199. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Aliberti, S.; Tobaldini, E.; Giuliani, F.; Nunziata, V.; Casazza, G.; Suigo, G.; D’Adda, A.; Bonaiti, G.; Roveda, A.; Queiroz, A.; et al. Cardiovascular Autonomic Alterations in Hospitalized Patients with Community-Acquired Pneumonia. Respir. Res. 2016, 17, 98. [Google Scholar] [CrossRef] [PubMed]
- Mazzuco, A.; Medeiros, W.M.; Sperling, M.P.R.; de Souza, A.S.; Alencar, M.C.N.; Arbex, F.F.; Neder, J.A.; Arena, R.; Borghi-Silva, A. Relationship between Linear and Nonlinear Dynamics of Heart Rate and Impairment of Lung Function in COPD Patients. Int. J. Chron. Obs. Pulmon. Dis. 2015, 10, 1651–1661. [Google Scholar] [CrossRef]
- Chen, W.-L.; Chen, G.-Y.; Kuo, C.-D. Hypoxemia and Autonomic Nervous Dysfunction in Patients with Chronic Obstructive Pulmonary Disease. Respir. Med. 2006, 100, 1547–1553. [Google Scholar] [CrossRef]
- Egan, T.M.; Murray, S.; Bustami, R.T.; Shearon, T.H.; McCullough, K.P.; Edwards, L.B.; Coke, M.A.; Garrity, E.R.; Sweet, S.C.; Heiney, D.A.; et al. Development of the New Lung Allocation System in the United States. Am. J. Transpl. Off. J. Am. Soc. Transpl. Am. Soc. Transpl. Surg. 2006, 6 Pt 2, 1212–1227. [Google Scholar] [CrossRef]
- Eurotransplant International Foundation. LAS Calculator. Available online: https://www.eurotransplant.org/cms/index.php?page=las_calculator (accessed on 28 January 2020).
- Miller, M.R.; Hankinson, J.; Brusasco, V.; Burgos, F.; Casaburi, R.; Coates, A.; Crapo, R.; Enright, P.; van der Grinten, C.P.M.; Gustafsson, P.; et al. Standardisation of Spirometry. Eur. Respir. J. 2005, 26, 319–338. [Google Scholar] [CrossRef]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratorie. ATS Statement: Guidelines for the Six-Minute Walk Test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef]
- Badilini, F.; Pagani, M.; Porta, A. HeartScope: A Software Tool Addressing Autonomic Nervous System Regulation. Comput. Cardiol. 2005, 32, 259–262. [Google Scholar]
- Task force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Standard of measurement, physiological interpretation and clinical use. Circulation 1996, 93, 1043–1065. [Google Scholar] [CrossRef]
- Montano, N.; Ruscone, T.G.; Porta, A.; Lombardi, F.; Pagani, M.; Malliani, A. Power Spectrum Analysis of Heart Rate Variability to Assess the Changes in Sympathovagal Balance during Graded Orthostatic Tilt. Circulation 1994, 90, 1826–1831. [Google Scholar] [CrossRef] [PubMed]
- Guzzetti, S.; Borroni, E.; Garbelli, P.E.; Ceriani, E.; Della Bella, P.; Montano, N.; Cogliati, C.; Somers, V.K.; Malliani, A.; Mallani, A.; et al. Symbolic Dynamics of Heart Rate Variability: A Probe to Investigate Cardiac Autonomic Modulation. Circulation 2005, 112, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Porta, A.; Tobaldini, E.; Guzzetti, S.; Furlan, R.; Montano, N.; Gnecchi-Ruscone, T. Assessment of Cardiac Autonomic Modulation During Graded Head-Up Tilt by Symbolic Analysis of Heart Rate Variability. Am. J. Physiol. Heart Circ. Physiol. 2007, 293, H702–H708. [Google Scholar] [CrossRef] [PubMed]
- Wensel, R.; Jilek, C.; Dörr, M.; Francis, D.P.; Stadler, H.; Lange, T.; Blumberg, F.; Opitz, C.; Pfeifer, M.; Ewert, R. Impaired Cardiac Autonomic Control Relates to Disease Severity in Pulmonary Hypertension. Eur. Respir. J. 2009, 34, 895–901. [Google Scholar] [CrossRef]
- Reznikov, L.R. Cystic Fibrosis and the Nervous System. Chest 2017, 151, 1147–1155. [Google Scholar] [CrossRef]
- Wensel, R.; Opitz, C.F.; Anker, S.D.; Winkler, J.; Höffken, G.; Kleber, F.X.; Sharma, R.; Hummel, M.; Hetzer, R.; Ewert, R. Assessment of Survival in Patients with Primary Pulmonary Hypertension: Importance of Cardiopulmonary Exercise Testing. Circulation 2002, 106, 319–324. [Google Scholar] [CrossRef]
- Velez-Roa, S.; Ciarka, A.; Najem, B.; Vachiery, J.-L.; Naeije, R.; van de Borne, P. Increased Sympathetic Nerve Activity in Pulmonary Artery Hypertension. Circulation 2004, 110, 1308–1312. [Google Scholar] [CrossRef]
- Yi, H.-T.; Hsieh, Y.-C.; Wu, T.-J.; Huang, J.-L.; Lin, W.-W.; Liang, K.-W.; Su, C.-S.; Tsai, W.-J.; Wang, K.-Y. Heart Rate Variability Parameters and Ventricular Arrhythmia Correlate with Pulmonary Arterial Pressure in Adult Patients with Idiopathic Pulmonary Arterial Hypertension. Heart Lung J. Crit. Care 2014, 43, 534–540. [Google Scholar] [CrossRef]
- McGowan, C.L.; Swiston, J.S.; Notarius, C.F.; Mak, S.; Morris, B.L.; Picton, P.E.; Granton, J.T.; Floras, J.S. Discordance between Microneurographic and Heart-Rate Spectral Indices of Sympathetic Activity in Pulmonary Arterial Hypertension. Heart Br. Card. Soc. 2009, 95, 754–758. [Google Scholar] [CrossRef] [PubMed]
- van de Borne, P.; Montano, N.; Pagani, M.; Oren, R.; Somers, V.K. Absence of Low-Frequency Variability of Sympathetic Nerve Activity in Severe Heart Failure. Circulation 1997, 95, 1449–1454. [Google Scholar] [CrossRef]
- Ponikowski, P.; Anker, S.D.; Chua, T.P.; Szelemej, R.; Piepoli, M.; Adamopoulos, S.; Webb-Peploe, K.; Harrington, D.; Banasiak, W.; Wrabec, K.; et al. Depressed Heart Rate Variability as an Independent Predictor of Death in Chronic Congestive Heart Failure Secondary to Ischemic or Idiopathic Dilated Cardiomyopathy. Am. J. Cardiol. 1997, 79, 1645–1650. [Google Scholar] [CrossRef]
- Szollosi, I.; King, S.J.; Wilson, J.W.; Naughton, M.T. Tachycardia in Adults with Cystic Fibrosis Is Associated with Normal Autonomic Function. Intern Med. J. 2011, 41, 455–461. [Google Scholar] [CrossRef] [PubMed]
- Florêncio, R.; Fregonezi, G.; Brilhante, S.; Borghi-Silva, A.; Dias, F.; Resqueti, V. Heart Rate Variability at Rest and after the 6-Minute Walk Test (6MWT) in Children with Cystic Fibrosis. Braz. J. Phys. 2013, 17, 419–426. [Google Scholar] [CrossRef][Green Version]
- Rodrigues, G.D.; Tobaldini, E.; Bellocchi, C.; Santaniello, A.; Caronni, M.; Severino, A.; Froldi, M.; Beretta, L.; da Silva Soares, P.P.; Montano, N. Cardiac Autonomic Modulation at Rest and during Orthostatic Stress among Different Systemic Sclerosis Subsets. Eur. J. Intern. Med. 2019, 66, 75–80. [Google Scholar] [CrossRef] [PubMed]
| Study Population n = 49 | |
|---|---|
| Demographics, n (%) | |
| Age, mean (SD) years | 38 (± 15) |
| Female | 30 (61) |
| Body mass index, mean (SD) | 21.8 (± 3.8) |
| Lung Allocation Score, median (IQR) | 33.777 (32.4–37.5) |
| Cystic fibrosis | 32 (65.5) |
| Idiopathic pulmonary fibrosis | 5 (10) |
| Chronic obstructive pulmonary disease | 3 (6) |
| Nonspecific interstitial pneumonia | 2 (4) |
| Systemic scleroderma | 2 (4) |
| Other indications for lung transplant | 5 (10) |
| Cardiovascular risk factors, n (%) | |
| Hypertension | 6 (12) |
| Diabetes | 20 (41) |
| Pulmonary hypertension | 12 (24.5) |
| mPAP, mean (SD) mmHg | 22 (± 5) |
| Respiratory function, median (IQR) | |
| Exacerbations, n (%) | 32 (65.5) |
| P/F, mean (SD) | 305 (± 61) |
| pCO2, mmHg | 42 (38–48) |
| FEV1 % of predicted | 31 (24–49) |
| FVC % of predicted, mean (SD) | 54 (± 16) |
| FEV1/FVC ratio, mean (SD) | 60 (± 21) |
| DLCO, mean (SD) % | 45 (± 22) |
| 6MWT, mean (SD) m | 406 (± 169) |
| Chronic lung infections, n (%) | |
| Burkholderia cepacia | 1 (2) |
| Pseudomonas aeruginosa | 27 (55) |
| MRSA | 9 (18.5) |
| Aspergillus | 8 (16.5) |
| Candida albicans | 3 (6) |
| NTM | 3 (6) |
| Medications, n (%) | |
| Beta-blockers | 7 (14.5) |
| Beta-agonists | 37 (75.5) |
| Anticholinergics | 12 (24.5) |
| Endothelin Receptor Antagonists | 1 (2) |
| Prostanoids | 2 (4) |
| PDE5 inhibitors | 1 (2) |
| Steroids | 40 (81.5) |
| Oxygen | 37 (75.5) |
| Healthy Controls n = 49 | LTx List Patients n = 49 | p | |
|---|---|---|---|
| (a) SUP | |||
| Heart rate, median (IQR) bpm | 62 (58–71) | 88 (79–99) | <0.0001 |
| Spectral analysis, median (IQR) | |||
| Total power, ms 2 | 2037 (1114–3706) | 533 (180–1051) | <0.0001 |
| LFnu | 31 (22–43) | 64 (36–82) | <0.0001 |
| HFnu | 66 (53–74) | 21 (8–36) | <0.0001 |
| LF/HF | 0.46 (0.34–0.81) | 2.81 (1.30–9.00) | <0.0001 |
| RR-RESP HFk 2 | 0.86 (0.77–0.92) | 0.85 (0.50–0.93) | 0.26 |
| RESP HF, Hz | 0.25 (0.22–0.30) | 0.34 (0.26–0.39) | <0.0001 |
| (b) ∆ORT | |||
| Heart rate, median ∆ORT (IQR) % | 22 (9–38) | 12 (9–16) | <0.0001 |
| Spectral analysis, median ∆ORT (IQR) % | |||
| Total power | −31 (−56–22) | −23 (−56–42) | 0.51 |
| LFnu | 105 (49–274) | 5 (−20–33) | <0.0001 |
| HFnu | −57 (−77–−39) | −1 (−55–50) | <0.0001 |
| LF/HF | 438 (204–1546) | 9 (−60–188) | <0.0001 |
| (a) | (b) | |||||
|---|---|---|---|---|---|---|
| LAS ≤ Median n = 25 | LAS > Median n = 24 | p | LAS ≤ 75th p. n = 37 | LAS > 75th p. n = 12 | p | |
| Heart rate, mean (SD) bpm | 87 (± 18) | 87 (± 15) | 0.97 | 86 (± 17) | 88 (± 12) | 0.79 |
| Spectral analysis, median (IQR) | ||||||
| Total power, ms 2 | 597 (232–1091) | 331 (150–928) | 0.43 | 551 (206–1080) | 439 (164–841) | 0.72 |
| LFnu | 75 (50–85) | 55 (28–69) | 0.04 | 68 (52–85) | 41 (22–62) | 0.005 |
| HFnu | 14 (7–34) | 25 (8–37) | 0.36 | 14 (7–36) | 25 (13–46) | 0.37 |
| LF/HF | 5.98 (1.53–10.89) | 2.24 (1.09–4.29) | 0.17 | 4.13 (1.56–10.92) | 1.70 (0.63–3.47) | 0.04 |
| RR-RESP HFk 2 | 0.73 (0.35–0.89) | 0.90 (0.63–0.94) | 0.11 | 0.80 (0.41–0.92) | 0.91 (0.64–0.94) | 0.35 |
| RESP HF, Hz | 0.35 (0.25–0.44) | 0.34 (0.28–0.37) | 0.67 | 0.35 (0.25–0.40) | 0.34 (0.29–0.36) | 0.91 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tobaldini, E.; D. Rodrigues, G.; Mantoan, G.; Monti, A.; Coti Zelati, G.; Cirelli, C.; Tarsia, P.; Morlacchi, L.C.; Rossetti, V.; Righi, I.; et al. Sympatho–Vagal Dysfunction in Patients with End-Stage Lung Disease Awaiting Lung Transplantation. J. Clin. Med. 2020, 9, 1146. https://doi.org/10.3390/jcm9041146
Tobaldini E, D. Rodrigues G, Mantoan G, Monti A, Coti Zelati G, Cirelli C, Tarsia P, Morlacchi LC, Rossetti V, Righi I, et al. Sympatho–Vagal Dysfunction in Patients with End-Stage Lung Disease Awaiting Lung Transplantation. Journal of Clinical Medicine. 2020; 9(4):1146. https://doi.org/10.3390/jcm9041146
Chicago/Turabian StyleTobaldini, Eleonora, Gabriel D. Rodrigues, Giorgio Mantoan, Alice Monti, Giulia Coti Zelati, Camilla Cirelli, Paolo Tarsia, Letizia Corinna Morlacchi, Valeria Rossetti, Ilaria Righi, and et al. 2020. "Sympatho–Vagal Dysfunction in Patients with End-Stage Lung Disease Awaiting Lung Transplantation" Journal of Clinical Medicine 9, no. 4: 1146. https://doi.org/10.3390/jcm9041146
APA StyleTobaldini, E., D. Rodrigues, G., Mantoan, G., Monti, A., Coti Zelati, G., Cirelli, C., Tarsia, P., Morlacchi, L. C., Rossetti, V., Righi, I., Nosotti, M., da S. Soares, P. P., Montano, N., Aliberti, S., & Blasi, F. (2020). Sympatho–Vagal Dysfunction in Patients with End-Stage Lung Disease Awaiting Lung Transplantation. Journal of Clinical Medicine, 9(4), 1146. https://doi.org/10.3390/jcm9041146








