Sarcoidosis: Causes, Diagnosis, Clinical Features, and Treatments
Abstract
1. Introduction
2. Epidemiology
3. Causes
3.1. Genetic Factors
3.2. Environmental Risk Factors
3.3. Infection
3.4. Autoimmunity
4. Immunopathogenesis
5. Clinical Features
| Radiographic Type | Radiographic Characteristics |
| 0 | No visible findings |
| I | Bilateral hilar lymphadenopathy |
| II | Bilateral hilar lymphadenopathy and parenchymal infiltration |
| III | Parenchymal infiltration without hilar adenopathy in regular chest radiography |
| IV | Advanced fibrosis with severe distortion of the normal lung architecture predominately in the middle and upper lobes with evidence of bronchiectasis, hilar retraction, bulla, cysts and more rarely “honeycombing” |
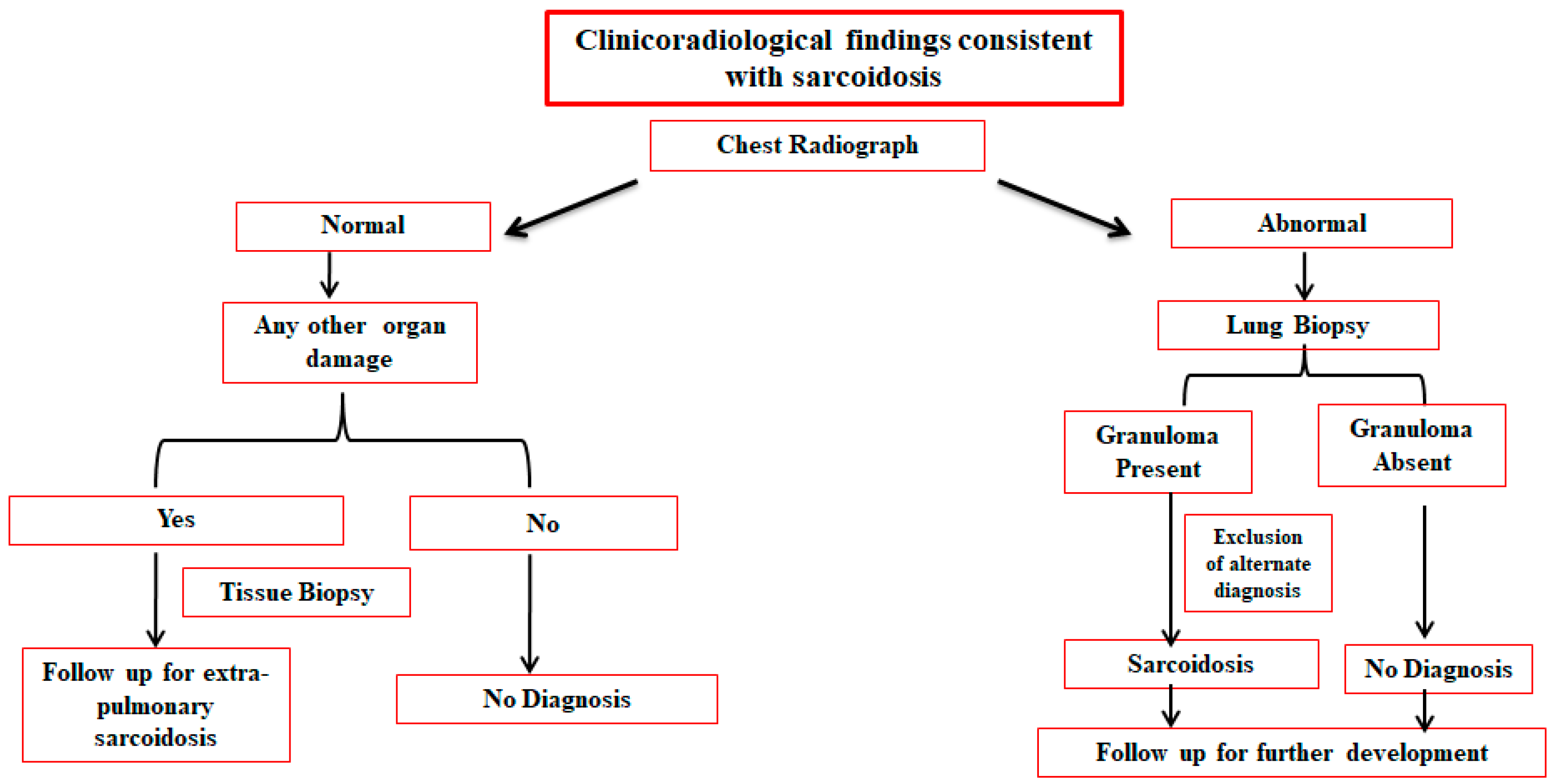
6. Screening and Diagnosis
7. Biomarkers for Sarcoidosis
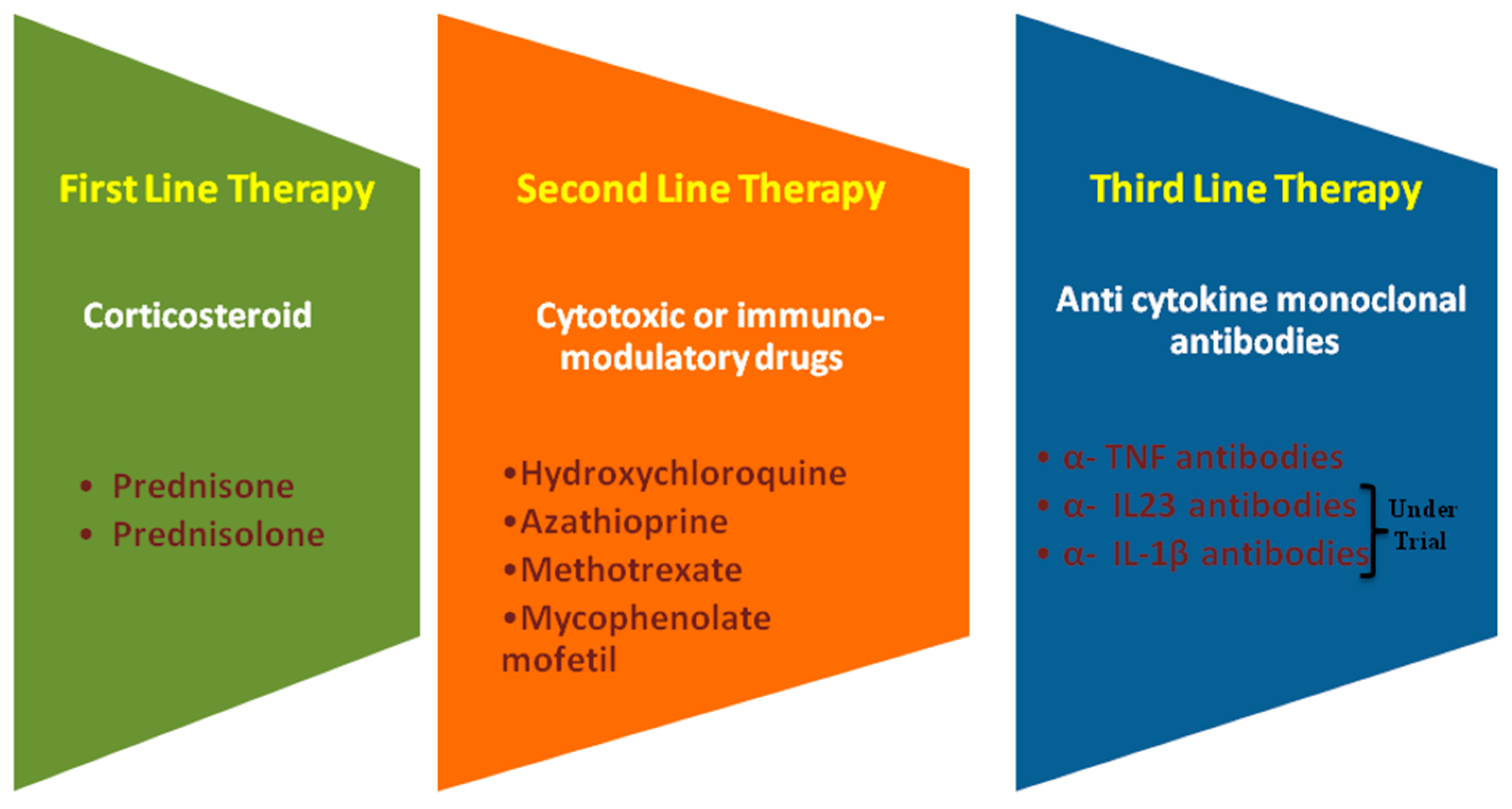
8. Treatment
9. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Hutchinson, J. Anomalous disease of the skin of the fingers: Case of livid papillary psoriasis. Illus. Clin. Surg. 1877, 1, 42–43. [Google Scholar]
- Gupta, S.K. Sarcoidosis: A journey through 50 years. Indian J. Chest Dis. Allied Sci. 2002, 44, 247–254. [Google Scholar]
- Hunninghake, G. Statement on sarcoidosis. Am. J. Respir. Crit. Care Med. 1999, 160, 736–755. [Google Scholar]
- Baughman, R.P.; Teirstein, A.S.; Judson, M.A.; Rossman, M.D.; Yeager, H., Jr.; Bresnitz, E.A.; DePalo, L.; Hunninghake, G.; Iannuzzi, M.C.; Johns, C.J.; et al. Clinical characteristics of patients in a case control study of sarcoidosis. Am. J. Respir. Crit. Care Med. 2001, 164, 1885–1889. [Google Scholar] [CrossRef] [PubMed]
- Li, C.-W.; Tao, R.-J.; Zou, D.-F.; Li, M.-H.; Xu, X.; Cao, W.-J. Pulmonary sarcoidosis with and without extrapulmonary involvement: A cross-sectional and observational study in china. BMJ Open 2018, 8, e018865. [Google Scholar] [CrossRef] [PubMed]
- Siltzbach, L.E.; James, D.G.; Neville, E.; Turiaf, J.; Battesti, J.P.; Sharma, O.P.; Hosoda, Y.; Mikami, R.; Odaka, M. Course and prognosis of sarcoidosis around the world. Am. J. Med. 1974, 57, 847–852. [Google Scholar] [CrossRef]
- Miyara, M.; Amoura, Z.; Parizot, C.; Badoual, C.; Dorgham, K.; Trad, S.; Kambouchner, M.; Valeyre, D.; Chapelon-Abric, C.; Debré, P.; et al. The immune paradox of sarcoidosis and regulatory t cells. J. Exp. Med. 2006, 203, 359–370. [Google Scholar] [CrossRef]
- Zissel, G. Cellular activation in the immune response of sarcoidosis. Semin. Respir. Crit. Care Med. 2014, 35, 307–315. [Google Scholar] [CrossRef]
- Iannuzzi, M.C.; Rybicki, B.A.; Teirstein, A.S. Sarcoidosis. N. Engl. J. Med. 2007, 357, 2153–2165. [Google Scholar] [CrossRef]
- Prior, C.; Knight, R.A.; Herold, M.; Ott, G.; Spiteri, M.A. Pulmonary sarcoidosis: Patterns of cytokine release in vitro. Eur. Respir. J. 1996, 9, 47–53. [Google Scholar] [CrossRef]
- Peros-Golubicic, T.; Ljubic, S. Cigarette smoking and sarcoidosis. Acta Med. Croat. 1995, 49, 187–193. [Google Scholar]
- Siltzbach, L.E. Current thoughts on the epidemiology and etiology of sarcoidosis. Am. J. Med. 1965, 39, 361–368. [Google Scholar] [CrossRef]
- Arkema, E.V.; Cozier, Y.C. Epidemiology of sarcoidosis: Current findings and future directions. Ther. Adv. Chronic Dis. 2018, 9, 227–240. [Google Scholar] [CrossRef] [PubMed]
- Arkema, E.V.; Grunewald, J.; Kullberg, S.; Eklund, A.; Askling, J. Sarcoidosis incidence and prevalence: A nationwide register-based assessment in sweden. Eur. Respir. J. 2016, 48, 1690–1699. [Google Scholar] [CrossRef]
- Bresnitz, E.A.; Strom, B.L. Epidemiology of sarcoidosis. Epidemiol. Rev. 1983, 5, 124–156. [Google Scholar] [CrossRef]
- Gillman, A.; Steinfort, C. Sarcoidosis in australia. Intern. Med. J. 2007, 37, 356–359. [Google Scholar] [CrossRef]
- Hosoda, Y.; Yamaguchi, M.; Hiraga, Y. Global epidemiology of sarcoidosis. What story do prevalence and incidence tell us? Clin. Chest Med. 1997, 18, 681–694. [Google Scholar] [CrossRef]
- James, D.G. Epidemiology of sarcoidosis. Sarcoidosis 1992, 9, 79–87. [Google Scholar]
- Reich, J.; Johnson, R. Incidence of clinically identified sarcoidosis in a northwest United States population. Sarcoidosis Vasc. Diffus. Lung Dis. Off. J. WASOG 1996, 13, 173–177. [Google Scholar]
- Karakatsani, A.; Papakosta, D.; Rapti, A.; Antoniou, K.M.; Dimadi, M.; Markopoulou, A.; Latsi, P.; Polychronopoulos, V.; Birba, G.; Ch, L.; et al. Epidemiology of interstitial lung diseases in greece. Respir. Med. 2009, 103, 1122–1129. [Google Scholar] [CrossRef]
- Sharma, S.; Mohan, A. Sarcoidosis in India: Not so rare. J. Indian Acad. Clin. Med. 2004, 5, 12–21. [Google Scholar]
- Gupta, S.; Gupta, S. Sarcoidosis in India: A review of 125 biopsy-proven cases from eastern India. Sarcoidosis 1990, 7, 43–49. [Google Scholar] [PubMed]
- Martusewicz-Boros, M.M.; Boros, P.W.; Wiatr, E.; Roszkowski-Śliż, K. What comorbidities accompany sarcoidosis? A large cohort (n = 1779) patients analysis. Sarcoidosis Vasc. Diffus. Lung Dis. 2015, 32, 115–120. [Google Scholar]
- Nowinski, A.; Puscinska, E.; Goljan-Geremek, A.; Bednarek, M.; Kaminski, D.; Gorecka, D. Comorbidities associated with sarcoidosis—Results from long-term observational study. Eur. Respir. J. 2014, 44, 461. [Google Scholar]
- Wu, C.H.; Chung, P.I.; Wu, C.Y.; Chen, Y.T.; Chiu, Y.W.; Chang, Y.T.; Liu, H.N. Comorbid autoimmune diseases in patients with sarcoidosis: A nationwide case-control study in taiwan. J. Dermatol. 2017, 44, 423–430. [Google Scholar] [CrossRef]
- Carmi, O.; Berla, M.; Edelstein, E.; Levy, Y. Coexisting systemic sclerosis-polymyositis and sarcoidosis: Case report and review of the literature. J. Clin. Rheumatol. Pract. Rep. Rheum. Musculoskelet. Dis. 2018, 24, 238–240. [Google Scholar] [CrossRef]
- Grunewald, J.; Spagnolo, P.; Wahlstrom, J.; Eklund, A. Immunogenetics of disease-causing inflammation in sarcoidosis. Clin. Rev. Allergy Immunol. 2015, 49, 19–35. [Google Scholar] [CrossRef]
- Fischer, A.; Ellinghaus, D.; Nutsua, M.; Hofmann, S.; Montgomery, C.G.; Iannuzzi, M.C.; Rybicki, B.A.; Petrek, M.; Mrazek, F.; Pabst, S.; et al. Identification of immune-relevant factors conferring sarcoidosis genetic risk. Am. J. Respir. Crit. Care Med. 2015, 192, 727–736. [Google Scholar] [CrossRef]
- Rybicki, B.A.; Iannuzzi, M.C. Epidemiology of sarcoidosis: Recent advances and future prospects. Semin. Respir. Crit. Care Med. 2007, 28, 22–35. [Google Scholar] [CrossRef]
- Fabrellas, E.F. Epidemiología de la sarcoidosis. Arch. Bronconeumol. 2007, 43, 92–100. [Google Scholar] [CrossRef]
- Rybicki, B.A.; Iannuzzi, M.C.; Frederick, M.M.; Thompson, B.W.; Rossman, M.D.; Bresnitz, E.A.; Terrin, M.L.; Moller, D.R.; Barnard, J.; Baughman, R.P.; et al. Familial aggregation of sarcoidosis. A case-control etiologic study of sarcoidosis (access). Am. J. Respir. Crit. Care Med. 2001, 164, 2085–2091. [Google Scholar] [CrossRef]
- Sverrild, A.; Backer, V.; Kyvik, K.O.; Kaprio, J.; Milman, N.; Svendsen, C.B.; Thomsen, S.F. Heredity in sarcoidosis: A registry-based twin study. Thorax 2008, 63, 894–896. [Google Scholar] [CrossRef]
- Schurmann, M.; REICHEL, P.; Muller-Myhsok, B.; Schlaak, M.; Muller-Quernheim, J.; Schwinger, E. Results from a genome-wide search for predisposing genes in sarcoidosis. Am. J. Respir. Crit. Care Med. 2001, 164, 840–846. [Google Scholar] [CrossRef] [PubMed]
- Ishihara, M.; Ohno, S.; Ishida, T.; Ando, H.; Naruse, T.; Nose, Y.; Inoko, H. Molecular genetic studies of hla class ii alleles in sarcoidosis. Tissue Antigens 1994, 43, 238–241. [Google Scholar] [CrossRef]
- Pabst, S.; Fränken, T.; Schönau, J.; Stier, S.; Nickenig, G.; Meyer, R.; Skowasch, D.; Grohé, C. Transforming growth factor-β gene polymorphisms in different phenotypes of sarcoidosis. Eur. Respir. J. 2011, 38, 169–175. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Ghosh, B.; Sharma, S. Association of tnf polymorphisms with sarcoidosis, its prognosis and tumour necrosis factor (tnf)-α levels in Asian Indians. Clin. Exp. Immunol. 2008, 151, 251–259. [Google Scholar] [CrossRef] [PubMed]
- Pabst, S.; Baumgarten, G.; Stremmel, A.; Lennarz, M.; Knüfermann, P.; Gillissen, A.; Vetter, H.; Grohe, C. Toll-like receptor (tlr) 4 polymorphisms are associated with a chronic course of sarcoidosis. Clin. Exp. Immunol. 2006, 143, 420–426. [Google Scholar] [CrossRef] [PubMed]
- Grunewald, J. Role of genetics in susceptibility and outcome of sarcoidosis. Semin. Respir. Crit. Care Med. 2010, 31, 380–389. [Google Scholar] [CrossRef]
- Iannuzzi, M.C. Genetics of sarcoidosis. Semin. Respir. Crit. Care Med. 2007, 28, 15–21. [Google Scholar] [CrossRef]
- Kucera, G.P.; Rybicki, B.A.; Kirkey, K.L.; Coon, S.W.; Major, M.L.; Maliarik, M.J.; Iannuzzi, M.C. Occupational risk factors for sarcoidosis in african-american siblings. Chest 2003, 123, 1527–1535. [Google Scholar] [CrossRef]
- Newman, L.S.; Rose, C.S.; Bresnitz, E.A.; Rossman, M.D.; Barnard, J.; Frederick, M.; Terrin, M.L.; Weinberger, S.E.; Moller, D.R.; McLennan, G.; et al. A case control etiologic study of sarcoidosis: Environmental and occupational risk factors. Am. J. Respir. Crit. Care Med. 2004, 170, 1324–1330. [Google Scholar] [CrossRef] [PubMed]
- Newman, K.L.; Newman, L.S. Occupational causes of sarcoidosis. Curr. Opin. Allergy Clin. Immunol. 2012, 12, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Vihlborg, P.; Bryngelsson, L.; Andersson, L.; Graff, P. Risk of sarcoidosis and seropositive rheumatoid arthritis from occupational silica exposure in swedish iron foundries: A retrospective cohort study. BMJ Open 2017, 7, e016839. [Google Scholar] [CrossRef]
- Izbicki, G.; Chavko, R.; Banauch, G.I.; Weiden, M.D.; Berger, K.I.; Aldrich, T.K.; Hall, C.; Kelly, K.J.; Prezant, D.J. World trade center “sarcoid-like” granulomatous pulmonary disease in new york city fire department rescue workers. Chest 2007, 131, 1414–1423. [Google Scholar] [CrossRef] [PubMed]
- Newman, L. Aetiologies of sarcoidosis. Eur. Respir. Monogr. 2005, 32, 23–48. [Google Scholar]
- Vidal, S.; De la Horra, C.; Martin, J.; Montes-Cano, M.; Rodríguez, E.; Respaldiza, N.; Rodriguez, F.; Varela, J.; Medrano, F.; Calderón, E. Pneumocystis jirovecii colonisation in patients with interstitial lung disease. Clin. Microbiol. Infect. 2006, 12, 231–235. [Google Scholar] [CrossRef]
- Drake, W.P.; Newman, L.S. Mycobacterial antigens may be important in sarcoidosis pathogenesis. Curr. Opin. Pulm. Med. 2006, 12, 359–363. [Google Scholar] [CrossRef]
- Ishige, I.; Eishi, Y.; Takemura, T.; Kobayashi, I.; Nakata, K.; Tanaka, I.; Nagaoka, S.; Iwai, K.; Watanabe, K.; Takizawa, T. Propionibacterium acnes is the most common bacterium commensal in peripheral lung tissue and mediastinal lymph nodes from subjects without sarcoidosis. Sarcoidosis Vasc. Diffuse Lung Dis. 2005, 22, 33–42. [Google Scholar]
- Allen, S.S.; Evans, W.; Carlisle, J.; Hajizadeh, R.; Nadaf, M.; Shepherd, B.E.; Pride, D.T.; Johnson, J.E.; Drake, W.P. Superoxide dismutase a antigens derived from molecular analysis of sarcoidosis granulomas elicit systemic th-1 immune responses. Respir. Res. 2008, 9, 36. [Google Scholar] [CrossRef]
- Song, Z.; Marzilli, L.; Greenlee, B.M.; Chen, E.S.; Silver, R.F.; Askin, F.B.; Teirstein, A.S.; Zhang, Y.; Cotter, R.J.; Moller, D.R. Mycobacterial catalase-peroxidase is a tissue antigen and target of the adaptive immune response in systemic sarcoidosis. J. Exp. Med. 2005, 201, 755–767. [Google Scholar] [CrossRef]
- Drake, W.P.; Dhason, M.S.; Nadaf, M.; Shepherd, B.E.; Vadivelu, S.; Hajizadeh, R.; Newman, L.S.; Kalams, S.A. Cellular recognition of mycobacterium tuberculosis esat-6 and katg peptides in systemic sarcoidosis. Infect. Immun. 2007, 75, 527–530. [Google Scholar] [CrossRef] [PubMed]
- Hirano, A.; Kataoka, M.; Nakata, Y.; Takeda, K.; Kamao, T.; Hiramatsu, J.; Kimura, G.; Tanimoto, Y.; Kanehiro, A.; Tanimoto, M. Sarcoidosis occurring after interferon-alpha therapy for chronic hepatitis c: Report of two cases. Respirology 2005, 10, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Trien, R.; Cooper, C.J.; Paez, D.; Colon, E.; Ajmal, S.; Salameh, H. Interferon-alpha-induced sarcoidosis in a patient being treated for hepatitis c. Am. J. Case Rep. 2014, 15, 235–238. [Google Scholar]
- Brjalin, V.; Salupere, R.; Tefanova, V.; Prikk, K.; Lapidus, N.; Jõeste, E. Sarcoidosis and chronic hepatitis c: A case report. World J. Gastroenterol. 2012, 18, 5816–5820. [Google Scholar] [CrossRef] [PubMed]
- Ramos-Casals, M.; Mana, J.; Nardi, N.; Brito-Zeron, P.; Xaubet, A.; Sanchez-Tapias, J.M.; Cervera, R.; Font, J. Sarcoidosis in patients with chronic hepatitis c virus infection: Analysis of 68 cases. Medicine 2005, 84, 69–80. [Google Scholar] [CrossRef] [PubMed]
- Grunewald, J.; Kaiser, Y.; Ostadkarampour, M.; Rivera, N.V.; Vezzi, F.; Lötstedt, B.; Olsen, R.-A.; Sylwan, L.; Lundin, S.; Käller, M. T-cell receptor—Hla-drb1 associations suggest specific antigens in pulmonary sarcoidosis. Eur. Respir. J. 2016, 47, 898–909. [Google Scholar] [CrossRef] [PubMed]
- Wahlström, J.; Dengjel, J.; Winqvist, O.; Targoff, I.; Persson, B.; Duyar, H.; Rammensee, H.-G.; Eklund, A.; Weissert, R.; Grunewald, J. Autoimmune t cell responses to antigenic peptides presented by bronchoalveolar lavage cell hla-dr molecules in sarcoidosis. Clin. Immunol. 2009, 133, 353–363. [Google Scholar] [CrossRef]
- Zissel, G.; Müller-Quernheim, J. Specific antigen(s) in sarcoidosis: A link to autoimmunity? Eur. Respir. Soc. 2016, 47, 707–709. [Google Scholar] [CrossRef]
- Kaiser, Y.; Eklund, A.; Grunewald, J. Moving target: Shifting the focus to pulmonary sarcoidosis as an autoimmune spectrum disorder. Eur. Respir. J. 2019, 54, 1802153. [Google Scholar] [CrossRef]
- Starshinova, A.A.; Malkova, A.M.; Basantsova, N.Y.; Zinchenko, Y.S.; Kudryavtsev, I.V.; Ershov, G.A.; Soprun, L.A.; Mayevskaya, V.A.; Churilov, L.P.; Yablonskiy, P.K. Sarcoidosis as an autoimmune disease. Front. Immunol. 2019, 10, 2933. [Google Scholar] [CrossRef]
- Haggmark, A.; Hamsten, C.; Wiklundh, E.; Lindskog, C.; Mattsson, C.; Andersson, E.; Lundberg, I.E.; Gronlund, H.; Schwenk, J.M.; Eklund, A.; et al. Proteomic profiling reveals autoimmune targets in sarcoidosis. Am. J. Respir. Crit. Care Med. 2015, 191, 574–583. [Google Scholar] [CrossRef] [PubMed]
- Gianchecchi, E.; Fierabracci, A. Recent advances on microbiota involvement in the pathogenesis of autoimmunity. Int. J. Mol. Sci. 2019, 20, 283. [Google Scholar] [CrossRef] [PubMed]
- Korsten, P.; Tampe, B.; Konig, M.F.; Nikiphorou, E. Sarcoidosis and autoimmune diseases: Differences, similarities and overlaps. Curr. Opin. Pulm. Med. 2018, 24, 504–512. [Google Scholar] [CrossRef] [PubMed]
- Chu, F.; Shi, M.; Lang, Y.; Shen, D.; Jin, T.; Zhu, J.; Cui, L. Gut microbiota in multiple sclerosis and experimental autoimmune encephalomyelitis: Current applications and future perspectives. Mediat. Inflamm. 2018. [Google Scholar] [CrossRef] [PubMed]
- Becker, A.; Vella, G.; Galata, V.; Rentz, K.; Beisswenger, C.; Herr, C.; Walter, J.; Tierling, S.; Slevogt, H.; Keller, A.; et al. The composition of the pulmonary microbiota in sarcoidosis—An observational study. Respir. Res. 2019, 20, 46. [Google Scholar] [CrossRef] [PubMed]
- Inaoka, P.T.; Shono, M.; Kamada, M.; Espinoza, J.L. Host-microbe interactions in the pathogenesis and clinical course of sarcoidosis. J. Biomed. Sci. 2019, 26, 45. [Google Scholar] [CrossRef]
- Agostini, C.; Adami, F.; Semenzato, G. New pathogenetic insights into the sarcoid granuloma. Curr. Opin. Rheumatol. 2000, 12, 71–76. [Google Scholar] [CrossRef]
- Wynn, T.A.; Barron, L. Macrophages: Master regulators of inflammation and fibrosis. Semin. Liver Dis. 2010, 30, 245–257. [Google Scholar] [CrossRef]
- Branton, M.H.; Kopp, J.B. Tgf-beta and fibrosis. Microbes. Infect. 1999, 1, 1349–1365. [Google Scholar] [CrossRef]
- Miedema, J.R.; Kaiser, Y.; Broos, C.E.; Wijsenbeek, M.S.; Grunewald, J.; Kool, M. Th17-lineage cells in pulmonary sarcoidosis and löfgren’s syndrome: Friend or foe? J. Autoimmun. 2018, 87, 82–96. [Google Scholar] [CrossRef]
- Huang, H.; Lu, Z.; Jiang, C.; Liu, J.; Wang, Y.; Xu, Z. Imbalance between th17 and regulatory t-cells in sarcoidosis. Int. J. Mol. Sci. 2013, 14, 21463–21473. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Qiu, L.; Wang, Y.; Aimurola, H.; Zhao, Y.; Li, S.; Xu, Z. The circulating treg/th17 cell ratio is correlated with relapse and treatment response in pulmonary sarcoidosis patients after corticosteroid withdrawal. PLoS ONE 2016, 11, e0148207. [Google Scholar] [CrossRef]
- Kelly, A.; Trowsdale, J. Genetics of antigen processing and presentation. Immunogenetics 2019, 71, 161–170. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.A.; Sinkovits, R.S.; Mock, D.; Rab, E.L.; Cai, J.; Yang, P.; Saunders, B.; Hsueh, R.C.; Choi, S.; Subramaniam, S.; et al. Components of the antigen processing and presentation pathway revealed by gene expression microarray analysis following b cell antigen receptor (bcr) stimulation. BMC Bioinformatics 2006, 7, 237. [Google Scholar]
- Bennett, D.; Bargagli, E.; Refini, R.M.; Rottoli, P. New concepts in the pathogenesis of sarcoidosis. Expert Rev. Respir. Med. 2019, 13, 981–991. [Google Scholar] [CrossRef]
- Pierce, T.B.; Margolis, M.; Razzuk, M.A. Sarcoidosis: Still a mystery? Bayl. Univ. Med Cent. Proc. 2001, 14, 8–12. [Google Scholar] [CrossRef]
- Hu, X.; Carmona, E.M.; Yi, E.S.; Pellikka, P.A.; Ryu, J. Causes of death in patients with chronic sarcoidosis. Sarcoidosis Vasc. Diffuse Lung Dis. 2016, 33, 275–280. [Google Scholar]
- Wirnsberger, R.M.; de Vries, J.; Wouters, E.F.; Drent, M. Clinical presentation of sarcoidosis in the netherlands an epidemiological study. Neth. J. Med. 1998, 53, 53–60. [Google Scholar] [CrossRef]
- Papiris, S.A.; Georgakopoulos, A.; Papaioannou, A.I.; Pianou, N.; Kallergi, M.; Kelekis, N.L.; Gialafos, H.; Manali, E.D.; Chatziioannou, S. Emerging phenotypes of sarcoidosis based on 18f-fdg pet/ct: A hierarchical cluster analysis. Expert Rev. Respir. Med. 2020, 14, 229–238. [Google Scholar] [CrossRef]
- Tavana, S.; Alizadeh, M.; Mohajerani, S.; Hashemian, S. Pulmonary and extra-pulmonary manifestations of sarcoidosis. Niger. Med. J. 2015, 56, 258–262. [Google Scholar]
- Nunes, H.; Uzunhan, Y.; Gille, T.; Lamberto, C.; Valeyre, D.; Brillet, P.Y. Imaging of sarcoidosis of the airways and lung parenchyma and correlation with lung function. Eur. Respir. J. 2012, 40, 750–765. [Google Scholar] [CrossRef] [PubMed]
- Spagnolo, P.; Rossi, G.; Trisolini, R.; Sverzellati, N.; Baughman, R.P.; Wells, A.U. Pulmonary sarcoidosis. Lancet Respir. Med. 2018, 6, 389–402. [Google Scholar] [CrossRef]
- Ozgul, M.; Cetinkaya, E.; Kirkil, G.; Ozgul, G.; Abul, Y.; Acat, M.; Onaran, H.; Urer, H.; Tutar, N.; Dincer, H. Lymph node characteristics of sarcoidosis with endobronchial ultrasound. Endosc. Ultrasound 2014, 3, 232–237. [Google Scholar] [PubMed]
- Koo, H.J.; Kim, M.Y.; Shin, S.Y.; Shin, S.; Kim, S.-S.; Lee, S.W.; Choi, C.-M. Evaluation of mediastinal lymph nodes in sarcoidosis, sarcoid reaction, and malignant lymph nodes using ct and fdg-pet/ct. Medicine 2015, 94, e1095. [Google Scholar] [CrossRef] [PubMed]
- Robinson, L.A.; Smith, P.; Sengupta, D.J.; Prentice, J.L.; Sandin, R.L. Molecular analysis of sarcoidosis lymph nodes for microorganisms: A case-control study with clinical correlates. BMJ Open 2013, 3, e004065. [Google Scholar] [CrossRef]
- Porter, N.; Beynon, H.L.; Randeva, H.S. Endocrine and reproductive manifestations of sarcoidosis. QJM 2003, 96, 553–561. [Google Scholar] [CrossRef] [PubMed]
- Bell, N.H. Endocrine complications of sarcoidosis. Endocrinol. Metab. Clin. N. Am. 1991, 20, 645–654. [Google Scholar] [CrossRef]
- Yanardag, H.; Pamuk, O.N.; Karayel, T. Cutaneous involvement in sarcoidosis: Analysis of the features in 170 patients. Respir. Med. 2003, 97, 978–982. [Google Scholar] [CrossRef]
- Yanardag, H.; Tetikkurt, C.; Bilir, M.; Demirci, S.; Iscimen, A. Diagnosis of cutaneous sarcoidosis; clinical and the prognostic significance of skin lesions. Multidiscip. Respir. Med. 2013, 8, 26. [Google Scholar] [CrossRef]
- Pasadhika, S.; Rosenbaum, J.T. Ocular sarcoidosis. Clin. Chest Med. 2015, 36, 669–683. [Google Scholar] [CrossRef]
- Raevis, J.J.; Antonova, N.; Agemy, S. Ocular involvement in sarcoidosis. J. Rheumatol. 2018, 45, 580. [Google Scholar] [CrossRef]
- Kansal, V.; Dollin, M. Ocular involvement in sarcoidosis. CMAJ 2017, 189, E609. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Nessrine, A.; Zahra, A.F.; Taoufik, H. Musculoskeletal involvement in sarcoidosis. J. Brasileiro Pneumol. 2014, 40, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Zhou, Y.; Lower, E.E.; Li, H.; Farhey, Y.; Baughman, R.P. Clinical characteristics of patients with bone sarcoidosis. Semin. Arthritis Rheum. 2017, 47, 143–148. [Google Scholar] [CrossRef] [PubMed]
- Conte, G.; Zugni, F.; Colleoni, M.; Renne, G.; Bellomi, M.; Petralia, G. Sarcoidosis with bone involvement mimicking metastatic disease at (18)f-fdg pet/ct: Problem solving by diffusion whole-body mri. Ecancermedicalscience 2015, 9, 537. [Google Scholar] [CrossRef] [PubMed]
- Rottoli, P.; Bargagli, E.; Chidichimo, C.; Nuti, D.; Cintorino, M.; Ginanneschi, C.; Caruso, G. Sarcoidosis with upper respiratory tract involvement. Respir. Med. 2006, 100, 253–257. [Google Scholar] [CrossRef]
- Soares, M.T.; Sousa, C.; Garanito, L.; Freire, F. Extensive upper respiratory tract sarcoidosis. BMJ Case Rep. 2016. [Google Scholar] [CrossRef]
- Wilson, R.; Lund, V.; Sweatman, M.; Mackay, I.; Mitchell, D. Upper respiratory tract involvement in sarcoidosis and its management. Eur. Respir. J. 1988, 1, 269–272. [Google Scholar]
- Hilderson, I.; Van Laecke, S.; Wauters, A.; Donck, J. Treatment of renal sarcoidosis: Is there a guideline? Overview of the different treatment options. Nephrol. Dial. Transplant. 2013, 29, 1841–1847. [Google Scholar] [CrossRef]
- Kala, D.; Naik, N.; Agarwal, A. Our experience in the management of vaginal agenesis: Its psychosocial impact and role of contrast magnetic resonance imaging scan with vaginal mold in the interpretation of high transverse vaginal septum. Saudi J. Kidney Dis. Transpl. 2008, 19, 67–71. [Google Scholar]
- Birnie, D.H.; Kandolin, R.; Nery, P.B.; Kupari, M. Cardiac manifestations of sarcoidosis: Diagnosis and management. Eur. Heart J. 2017, 38, 2663–2670. [Google Scholar] [CrossRef] [PubMed]
- Lynch, J.P., III; Hwang, J.; Bradfield, J.; Fishbein, M.; Shivkumar, K.; Tung, R. Cardiac involvement in sarcoidosis: Evolving concepts in diagnosis and treatment. Semin. Respir. Crit. Care Med. 2014, 35, 372–390. [Google Scholar]
- Ibitoye, R.T.; Wilkins, A.; Scolding, N.J. Neurosarcoidosis: A clinical approach to diagnosis and management. J. Neurol. 2017, 264, 1023–1028. [Google Scholar] [CrossRef] [PubMed]
- Lacomis, D. Neurosarcoidosis. Curr. Neuropharmacol. 2011, 9, 429–436. [Google Scholar] [CrossRef] [PubMed]
- Warshauer, D.M.; Molina, P.L.; Hamman, S.M.; Koehler, R.E.; Paulson, E.K.; Bechtold, R.E.; Perlmutter, M.L.; Hiken, J.N.; Francis, I.R.; Cooper, C.J.; et al. Nodular sarcoidosis of the liver and spleen: Analysis of 32 cases. Radiology 1995, 195, 757–762. [Google Scholar] [CrossRef] [PubMed]
- Patel, I.; Ismajli, M.; Steuer, A. Sarcoidosis presenting as massive splenic infarction. Case Rep. Rheumatol. 2012. [Google Scholar] [CrossRef] [PubMed]
- Raber, E.L.; Haba, J.; Beck, P. Splenic sarcoidosis: A case report and review of the imaging findings of multiple incidental splenic lesions as the initial presentation of sarcoidosis. Can. J. Gastroenterol. 2011, 25, 477–478. [Google Scholar] [CrossRef]
- Valeyre, D.; Prasse, A.; Nunes, H.; Uzunhan, Y.; Brillet, P.-Y.; Müller-Quernheim, J. Sarcoidosis. Lancet 2014, 383, 1155–1167. [Google Scholar] [CrossRef]
- Prasse, A. The diagnosis, differential diagnosis, and treatment of sarcoidosis. Deutsches Ärzteblatt Int. 2016, 113, 565–574. [Google Scholar] [CrossRef]
- Sweiss, N.J.; Salloum, R.; Ghandi, S.; Alegre, M.-L.; Sawaqed, R.; Badaracco, M.; Pursell, K.; Pitrak, D.; Baughman, R.P.; Moller, D.R. Significant cd4, cd8, and cd19 lymphopenia in peripheral blood of sarcoidosis patients correlates with severe disease manifestations. PLoS ONE 2010, 5, e9088. [Google Scholar] [CrossRef]
- Chopra, A.; Kalkanis, A.; Judson, M.A. Biomarkers in sarcoidosis. Expert Rev. Clin. Immunol. 2016, 12, 1191–1208. [Google Scholar] [CrossRef] [PubMed]
- Kikuchi, H.; Mori, T.; Rai, T.; Uchida, S. Acute kidney injury caused by sarcoid granulomatous interstitial nephritis without extrarenal manifestations. CEN Case Rep. 2015, 4, 212–217. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tanizawa, K.; Handa, T.; Nagai, S.; Niimi, A.; Oguma, T.; Kubo, T.; Ito, Y.; Aihara, K.; Ikezoe, K.; Matsumoto, H.; et al. Comprehensive evaluation of airway involvement in pulmonary sarcoidosis. ERJ Open Res. 2017, 3. [Google Scholar] [CrossRef]
- Mitchell, D.N.; Scadding, J.G.; Heard, B.E.; Hinson, K.F. Sarcoidosis: Histopathological definition and clinical diagnosis. J. Clin. Pathol. 1977, 30, 395–408. [Google Scholar] [CrossRef] [PubMed]
- Akten, H.S.; Kilic, H.; Celik, B.; Erbas, G.; Isikdogan, Z.; Turktas, H.; Kokturk, N. Diagnostic yield of transbronchial biopsy in comparison to high resolution computerized tomography in sarcoidosis cases. Asian Pac. J. Cancer Prev. 2018, 19, 1029. [Google Scholar]
- Navasakulpong, A.; Auger, M.; Gonzalez, A.V. Yield of ebus-tbna for the diagnosis of sarcoidosis: Impact of operator and cytopathologist experience. BMJ Open Respir. Res. 2016, 3, e000144. [Google Scholar] [CrossRef]
- Smith-Rohrberg, D.; Sharma, S.K. Tuberculin skin test among pulmonary sarcoidosis patients with and without tuberculosis: Its utility for the screening of the two conditions in tuberculosis-endemic regions. Sarcoidosis Vasc. Diffuse Lung Dis. 2006, 23, 130–134. [Google Scholar] [PubMed]
- Mambretti, J. Chest x-ray stages of sarcoidosis. J. Insur. Med. 2004, 36, 91–92. [Google Scholar]
- Avital, M.; Hadas-Halpern, I.; Deeb, M.; Izbicki, G. Radiological findings in sarcoidosis. Isr. Med. Assoc. J. 2008, 10, 572–574. [Google Scholar]
- Lynch, J.P., III. Computed tomographic scanning in sarcoidosis. Semin. Respir. Crit. Care Med. 2003, 24, 393–418. [Google Scholar] [CrossRef]
- Keijsers, R.G.M.; van den Heuvel, D.A.F.; Grutters, J.C. Imaging the inflammatory activity of sarcoidosis. Eur. Respir. J. 2013, 41, 743–751. [Google Scholar] [CrossRef] [PubMed]
- Piotrowski, W.J. Radiological examinations in the diagnosis and monitoring of pulmonary sarcoidosis. Polski Merkuriusz Lekarski Organ Polskiego Towarzystwa Lekarskiego 2018, 44, 118–123. [Google Scholar] [PubMed]
- Thunell, M.; Bjerle, P.; Stjernberg, N. Ecg abnormalities in patients with sarcoidosis. Acta Med. Scand. 1983, 213, 115–118. [Google Scholar] [CrossRef] [PubMed]
- Błaut-Jurkowska, J.; Kaźnica-Wiatr, M.; Żygadło, A.; Tomkiewicz-Pająk, L.; Podolec, P.; Olszowska, M. Electrocardiographic abnormalities in patients with pulmonary sarcoidosis (Rcd Code: Iii). J. Rare Cardiovasc. Dis. 2017, 3, 81–85. [Google Scholar] [CrossRef][Green Version]
- Komada, T.; Suzuki, K.; Ishiguchi, H.; Kawai, H.; Okumura, T.; Hirashiki, A.; Naganawa, S. Magnetic resonance imaging of cardiac sarcoidosis: An evaluation of the cardiac segments and layers that exhibit late gadolinium enhancement. Nagoya J. Med. Sci. 2016, 78, 437–446. [Google Scholar]
- Craig, D.A.; Colletti, P.M.; Ratto, D.; Gordonson, J.S.; Raval, J.K.; Sharma, O.P. Mri findings in pulmonary sarcoidosis. Magn. Reson. Imaging 1988, 6, 567–573. [Google Scholar] [CrossRef]
- Strimbu, K.; Tavel, J.A. What are biomarkers? Curr. Opin. HIV AIDS 2010, 5, 463. [Google Scholar] [CrossRef]
- Ramos-Casals, M.; Retamozo, S.; Siso-Almirall, A.; Perez-Alvarez, R.; Pallares, L.; Brito-Zeron, P. Clinically-useful serum biomarkers for diagnosis and prognosis of sarcoidosis. Expert Rev. Clin. Immunol. 2019, 15, 391–405. [Google Scholar] [CrossRef] [PubMed]
- Bunting, P.S.; Szalai, J.P.; Katic, M. Diagnostic aspects of angiotensin converting enzyme in pulmonary sarcoidosis. Clin. Biochem. 1987, 20, 213–219. [Google Scholar] [CrossRef]
- Ungprasert, P.; Carmona, E.M.; Crowson, C.S.; Matteson, E.L. Diagnostic utility of angiotensin-converting enzyme in sarcoidosis: A population-based study. Lung 2016, 194, 91–95. [Google Scholar] [CrossRef]
- Kahkouee, S.; Samadi, K.; Alai, A.; Abedini, A.; Rezaiian, L. Serum ace level in sarcoidosis patients with typical and atypical hrct manifestation. Pol. J. Radiol. 2016, 81, 458–461. [Google Scholar] [CrossRef] [PubMed]
- Bargagli, E.; Bennett, D.; Maggiorelli, C.; Di Sipio, P.; Margollicci, M.; Bianchi, N.; Rottoli, P. Human chitotriosidase: A sensitive biomarker of sarcoidosis. J. Clin. Immunol. 2013, 33, 264–270. [Google Scholar] [CrossRef] [PubMed]
- Popević, S.; Šumarac, Z.; Jovanović, D.; Babić, D.; Stjepanović, M.; Jovičić, S.; Šobić-Šaranović, D.; Filipović, S.; Gvozdenović, B.; Omčikus, M.; et al. Verifying sarcoidosis activity: Chitotriosidase versus ace in sarcoidosis—A case-control study. J. Med Biochem. 2016, 35, 390–400. [Google Scholar] [CrossRef]
- Bennett, D.; Cameli, P.; Lanzarone, N.; Carobene, L.; Bianchi, N.; Fui, A.; Rizzi, L.; Bergantini, L.; Cillis, G.; d’Alessandro, M.; et al. Chitotriosidase: A biomarker of activity and severity in patients with sarcoidosis. Respir. Res. 2020, 21, 6. [Google Scholar] [CrossRef] [PubMed]
- Sahin, O.; Ziaei, A.; Karaismailoglu, E.; Taheri, N. The serum angiotensin converting enzyme and lysozyme levels in patients with ocular involvement of autoimmune and infectious diseases. BMC Ophthalmol. 2016, 16, 19. [Google Scholar] [CrossRef] [PubMed]
- Tomita, H.; Sato, S.; Matsuda, R.; Sugiura, Y.; Kawaguchi, H.; Niimi, T.; Yoshida, S.; Morishita, M. Serum lysozyme levels and clinical features of sarcoidosis. Lung 1999, 177, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Prior, C.; Frank, A.; Fuchs, D.; Hausen, A.; Judmaier, G.; Reibnegger, G.; Werner, E.R.; Wachter, H. Urinary neopterin excretion in pulmonary sarcoidosis: Correlation to clinical course of the disease. Clin. Chim. Acta 1988, 177, 211–220. [Google Scholar] [CrossRef]
- Eklund, A.; Blaschke, E. Elevated serum neopterin levels in sarcoidosis. Lung 1986, 164, 325–332. [Google Scholar] [CrossRef]
- Lacronique, J.; Auzeby, A.; Valeyre, D.; Traore, B.M.; Barbosa, M.L.; Soler, P.; Choudat, D.; Battesti, J.P.; Touitou, Y.; Marsac, J. Urinary neopterin in pulmonary sarcoidosis. Relationship to clinical and biologic assessment of the disease. Am. Rev. Respir. Dis. 1989, 139, 1474–1478. [Google Scholar] [CrossRef]
- Sharma, O.P. Hypercalcemia in granulomatous disorders: A clinical review. Curr. Opin. Pulm. Med. 2000, 6, 442–447. [Google Scholar] [CrossRef]
- Ibrik, O.; Samon, R.; Roda, A.; Roca, R.; Gonzalez, J.C.; Viladoms, J.; Vilaseca, J.; Serrano, M. Sarcoidosis: Diagnosis from the renal function and hypercalcaemia study. Nefrologia 2011, 31, 371–372. [Google Scholar] [PubMed]
- Demetriou, E.T.; Pietras, S.M.; Holick, M.F. Hypercalcemia and soft tissue calcification owing to sarcoidosis: The sunlight-cola connection. J. Bone Miner. Res. 2010, 25, 1695–1699. [Google Scholar] [CrossRef] [PubMed]
- Grutters, J.C.; Fellrath, J.M.; Mulder, L.; Janssen, R.; van den Bosch, J.M.; van Velzen-Blad, H. Serum soluble interleukin-2 receptor measurement in patients with sarcoidosis: A clinical evaluation. Chest 2003, 124, 186–195. [Google Scholar] [CrossRef] [PubMed]
- Thi Hong Nguyen, C.; Kambe, N.; Kishimoto, I.; Ueda-Hayakawa, I.; Okamoto, H. Serum soluble interleukin-2 receptor level is more sensitive than angiotensin-converting enzyme or lysozyme for diagnosis of sarcoidosis and may be a marker of multiple organ involvement. J. Dermatol. 2017, 44, 789–797. [Google Scholar] [CrossRef] [PubMed]
- Ina, Y.; Takada, K.; Sato, T.; Yamamoto, M.; Noda, M.; Morishita, M. Soluble interleukin 2 receptors in patients with sarcoidosis. Possible origin. Chest 1992, 102, 1128–1133. [Google Scholar] [CrossRef] [PubMed]
- Bargagli, E.; Olivieri, C.; Landi, C.; Magi, B.; Bennett, D.; Bianchi, N.; Perrone, A.; Fossi, A.; Rottoli, P. Serum amyloid a as a potential biomarker of sarcoidosis. Eur. Respir. J. 2011, 38, 3807. [Google Scholar]
- Chen, E.S.; Song, Z.; Willett, M.H.; Heine, S.; Yung, R.C.; Liu, M.C.; Groshong, S.D.; Zhang, Y.; Tuder, R.M.; Moller, D.R. Serum amyloid a regulates granulomatous inflammation in sarcoidosis through toll-like receptor-2. Am. J. Respir. Crit. Care Med. 2010, 181, 360–373. [Google Scholar] [CrossRef]
- Huho, A.; Foulke, L.; Jennings, T.; Koutroumpakis, E.; Dalvi, S.; Chaudhry, H.; Chopra, A.; Modi, A.; Rane, N.; Prezant, D.J.; et al. The role of serum amyloid a staining of granulomatous tissues for the diagnosis of sarcoidosis. Respir. Med. 2017, 126, 1–8. [Google Scholar] [CrossRef]
- Boot, R.G.; Hollak, C.E.; Verhoek, M.; Alberts, C.; Jonkers, R.E.; Aerts, J.M. Plasma chitotriosidase and ccl18 as surrogate markers for granulomatous macrophages in sarcoidosis. Clin. Chim. Acta 2010, 411, 31–36. [Google Scholar] [CrossRef]
- Cai, M.; Bonella, F.; He, X.; Sixt, S.U.; Sarria, R.; Guzman, J.; Costabel, U. Ccl18 in serum, bal fluid and alveolar macrophage culture supernatant in interstitial lung diseases. Respir. Med. 2013, 107, 1444–1452. [Google Scholar] [CrossRef]
- Su, R.; Nguyen, M.-L.T.; Agarwal, M.R.; Kirby, C.; Nguyen, C.P.; Ramstein, J.; Darnell, E.P.; Gomez, A.D.; Ho, M.; Woodruff, P.G. Interferon-inducible chemokines reflect severity and progression in sarcoidosis. Respir. Res. 2013, 14, 121. [Google Scholar] [CrossRef] [PubMed]
- Miyoshi, S.; Hamada, H.; Kadowaki, T.; Hamaguchi, N.; Ito, R.; Irifune, K.; Higaki, J. Comparative evaluation of serum markers in pulmonary sarcoidosis. Chest 2010, 137, 1391–1397. [Google Scholar] [CrossRef] [PubMed]
- Ramstein, J.; Broos, C.E.; Simpson, L.J.; Ansel, K.M.; Sun, S.A.; Ho, M.E.; Woodruff, P.G.; Bhakta, N.R.; Christian, L.; Nguyen, C.P.; et al. Ifn-gamma-producing t-helper 17.1 cells are increased in sarcoidosis and are more prevalent than t-helper type 1 cells. Am. J. Respir. Crit. Care Med. 2016, 193, 1281–1291. [Google Scholar] [CrossRef] [PubMed]
- Prior, C.; Haslam, P.L. Increased levels of serum interferon-gamma in pulmonary sarcoidosis and relationship with response to corticosteroid therapy. Am. Rev. Respir. Dis. 1991, 143, 53–60. [Google Scholar] [CrossRef]
- Salez, F.; Gosset, P.; Copin, M.C.; Lamblin Degros, C.; Tonnel, A.B.; Wallaert, B. Transforming growth factor-beta1 in sarcoidosis. Eur. Respir. J. 1998, 12, 913–919. [Google Scholar] [CrossRef]
- Piotrowski, W.J.; Kiszalkiewicz, J.; Pastuszak-Lewandoska, D.; Antczak, A.; Gorski, P.; Migdalska-Sek, M.; Gorski, W.; Czarnecka, K.; Nawrot, E.; Domanska, D.; et al. Tgf-beta and smads mrna expression in pulmonary sarcoidosis. Adv. Exp. Med. Biol. 2015, 852, 59–69. [Google Scholar]
- Drent, M. Sarcoidosis: Is there a role for anti-tnf-α? Rev. Port. Pneumol. 2007, 13, S51–S57. [Google Scholar] [CrossRef]
- Amber, K.T.; Bloom, R.; Mrowietz, U.; Hertl, M. Tnf-alpha: A treatment target or cause of sarcoidosis? J. Eur. Acad. Dermatol. Venereol. 2015, 29, 2104–2111. [Google Scholar] [CrossRef]
- James, W.E. Leaving history behind: Cd4/cd8 ratio as a diagnostic tool in sarcoidosis. EBioMedicine 2016, 8, 20. [Google Scholar] [CrossRef]
- Shen, Y.; Pang, C.; Wu, Y.; Li, D.; Wan, C.; Liao, Z.; Yang, T.; Chen, L.; Wen, F. Diagnostic performance of bronchoalveolar lavage fluid cd4/cd8 ratio for sarcoidosis: A meta-analysis. EBioMedicine 2016, 8, 302–308. [Google Scholar] [CrossRef]
- Winterbauer, R.H.; Lammert, J.; Selland, M.; Wu, R.; Corley, D.; Springmeyer, S.C. Bronchoalveolar lavage cell populations in the diagnosis of sarcoidosis. Chest 1993, 104, 352–361. [Google Scholar] [CrossRef] [PubMed]
- Drent, M.; Mansour, K.; Linssen, C. Bronchoalveolar lavage in sarcoidosis. Semin. Respir. Crit. Care Med. 2007, 28, 486–495. [Google Scholar] [CrossRef] [PubMed]
- Psathakis, K.; Papatheodorou, G.; Plataki, M.; Panagou, P.; Loukides, S.; Siafakas, N.M.; Bouros, D. 8-isoprostane, a marker of oxidative stress, is increased in the expired breath condensate of patients with pulmonary sarcoidosis. Chest 2004, 125, 1005–1011. [Google Scholar] [CrossRef] [PubMed]
- Piotrowski, W.J.; Antczak, A.; Marczak, J.; Nawrocka, A.; Kurmanowska, Z.; Górski, P. Eicosanoids in exhaled breath condensate and bal fluid of patients with sarcoidosis. Chest 2007, 132, 589–596. [Google Scholar] [CrossRef] [PubMed]
- Ciarleglio, G.; Refini, R.; Pieroni, M. Exhaled carbon monoxide in sarcoidosis. Sarcoidosis Vasc. Diffus. Lung Dis. 2008, 25, 46–50. [Google Scholar]
- Moodley, Y.; Chetty, R.; Lalloo, U. Nitric oxide levels in exhaled air and inducible nitric oxide synthase immunolocalization in pulmonary sarcoidosis. Eur. Respir. J. 1999, 14, 822–827. [Google Scholar] [CrossRef]
- Wilsher, M.L.; Fergusson, W.; Milne, D.; Wells, A.U. Exhaled nitric oxide in sarcoidosis. Thorax 2005, 60, 967–970. [Google Scholar] [CrossRef]
- Carleo, A.; Bennett, D.; Rottoli, P. Biomarkers in sarcoidosis: The contribution of system biology. Curr. Opin. Pulm. Med. 2016, 22, 509–514. [Google Scholar] [CrossRef]
- Su, R.; Li, M.M.; Bhakta, N.R.; Solberg, O.D.; Darnell, E.P.; Ramstein, J.; Garudadri, S.; Ho, M.; Woodruff, P.G.; Koth, L.L. Longitudinal analysis of sarcoidosis blood transcriptomic signatures and disease outcomes. Eur. Respir. J. 2014, 44, 985–993. [Google Scholar] [CrossRef]
- Schupp, J.C.; Vukmirovic, M.; Kaminski, N.; Prasse, A. Transcriptome profiles in sarcoidosis and their potential role in disease prediction. Curr. Opin. Pulm. Med. 2017, 23, 487–492. [Google Scholar] [CrossRef]
- Ascoli, C.; Huang, Y.; Schott, C.; Turturice, B.A.; Metwally, A.; Perkins, D.L.; Finn, P.W. A circulating microrna signature serves as a diagnostic and prognostic indicator in sarcoidosis. Am. J. Respir. Cell Mol. Biol. 2018, 58, 40–54. [Google Scholar] [CrossRef] [PubMed]
- Kiszałkiewicz, J.; Piotrowski, W.J.; Pastuszak-Lewandoska, D.; Górski, P.; Antczak, A.; Górski, W.; Domańska-Senderowska, D.; Migdalska-Sęk, M.; Czarnecka, K.H.; Nawrot, E. Altered mirna expression in pulmonary sarcoidosis. BMC Med. Genet. 2016, 17, 2. [Google Scholar] [CrossRef] [PubMed]
- Geamanu, A.; Gupta, S.V.; Bauerfeld, C.; Samavati, L. Metabolomics connects aberrant bioenergetic, transmethylation, and gut microbiota in sarcoidosis. Metab. Off. J. Metab. Soc. 2016, 12, 35. [Google Scholar] [CrossRef] [PubMed]
- Banoei, M.M.; Iupe, I.; Bazaz, R.D.; Campos, M.; Vogel, H.J.; Winston, B.W.; Mirsaeidi, M. Metabolomic and metallomic profile differences between veterans and civilians with pulmonary sarcoidosis. Sci. Rep. 2019, 9, 19584. [Google Scholar] [CrossRef] [PubMed]
- Judson, M.A.; Baughman, R.P.; Costabel, U.; Mack, M.; Barnathan, E.S. The potential additional benefit of infliximab in patients with chronic pulmonary sarcoidosis already receiving corticosteroids: A retrospective analysis from a randomized clinical trial. Respir. Med. 2014, 108, 189–194. [Google Scholar] [CrossRef] [PubMed]
- Pande, A.; Culver, D.A. Knowing when to use steroids, immunosuppressants or biologics for the treatment of sarcoidosis. Expert Rev. Respir. Med. 2020, 14, 285–298. [Google Scholar] [CrossRef]
- James, W.E.; Judson, M.A. Therapeutic strategies for pulmonary sarcoidosis. Expert Rev. Respir. Med. 2020, 14, 391–403. [Google Scholar] [CrossRef]
- Gibson, G.; Prescott, R.; Muers, M.; Middleton, W.; Mitchell, D.; Connolly, C.; Harrison, B. British thoracic society sarcoidosis study: Effects of long term corticosteroid treatment. Thorax 1996, 51, 238–247. [Google Scholar] [CrossRef]
- Grunewald, J.; Grutters, J.C.; Arkema, E.V.; Saketkoo, L.A.; Moller, D.R.; Müller-Quernheim, J. Sarcoidosis. Nat. Rev. Dis. Primers 2019, 5, 45. [Google Scholar] [CrossRef] [PubMed]
- Muller-Quernheim, J.; Kienast, K.; Held, M.; Pfeifer, S.; Costabel, U. Treatment of chronic sarcoidosis with an azathioprine/prednisolone regimen. Eur. Respir. J. 1999, 14, 1117–1122. [Google Scholar] [CrossRef] [PubMed]
- Baughman, R.; Winget, D.; Lower, E. Methotrexate is steroid sparing in acute sarcoidosis: Results of a double blind, randomized trial. Sarcoidosis Vasc. Diffus. Lung Dis. Off. J. WASOG 2000, 17, 60–66. [Google Scholar]
- Brill, A.-K.; Ott, S.R.; Geiser, T. Effect and safety of mycophenolate mofetil in chronic pulmonary sarcoidosis: A retrospective study. Respiration 2013, 86, 376–383. [Google Scholar] [CrossRef] [PubMed]
- Papiris, S.; Stagaki, E.; Papadaki, G.; Kolilekas, L.; Korbila, I.; Apollonatou, V.; Kallieri, M.; Gialafos, H.; Chatziioannou, S.; Papaioannou, A.I.; et al. Mycophenolate mofetil as an alternative treatment in sarcoidosis. Pulm. Pharmacol. Ther. 2019, 58, 101840. [Google Scholar] [CrossRef] [PubMed]
- Wyser, C.P.; van Schalkwyk, E.M.; Alheit, B.; Bardin, P.G.; Joubert, J.R. Treatment of progressive pulmonary sarcoidosis with cyclosporin a: A randomized controlled trial. Am. J. Respir. Crit. Care Med. 1997, 156, 1371–1376. [Google Scholar] [CrossRef] [PubMed]
- Korsten, P.; Mirsaeidi, M.; Sweiss, N.J. Nonsteroidal therapy of sarcoidosis. Curr. Opin. Pulm. Med. 2013, 19, 516. [Google Scholar] [CrossRef] [PubMed]
- Baughman, R.; Lower, E. Leflunomide for chronic sarcoidosis. Sarcoidosis Vasc. Diffus. Lung Dis. Off. J. WASOG 2004, 21, 43–48. [Google Scholar]
- Sharma, O.P. Effectiveness of chloroquine and hydroxychloroquine in treating selected patients with sarcoidosis with neurological involvement. Arch. Neurol. 1998, 55, 1248–1254. [Google Scholar] [CrossRef]
- Saketkoo, L.A.; Baughman, R.P. Biologic therapies in the treatment of sarcoidosis. Expert Rev. Clin. Immunol. 2016, 12, 817–825. [Google Scholar] [CrossRef]
- Muller-Quernheim, J. Sarcoidosis: Immunopathogenetic concepts and their clinical application. Eur. Respir. J. 1998, 12, 716–738. [Google Scholar] [CrossRef]
- Hostettler, K.E.; Studler, U.; Tamm, M.; Brutsche, M.H. Long-term treatment with infliximab in patients with sarcoidosis. Respiration 2012, 83, 218–224. [Google Scholar] [CrossRef]
- Baughman, R.P.; Drent, M.; Kavuru, M.; Judson, M.A.; Costabel, U.; du Bois, R.; Albera, C.; Brutsche, M.; Davis, G.; Donohue, J.F. Infliximab therapy in patients with chronic sarcoidosis and pulmonary involvement. Am. J. Respir. Crit. Care Med. 2006, 174, 795–802. [Google Scholar] [CrossRef] [PubMed]
- Loza, M.J.; Brodmerkel, C.; Du Bois, R.M.; Judson, M.A.; Costabel, U.; Drent, M.; Kavuru, M.; Flavin, S.; Lo, K.H.; Barnathan, E.S. Inflammatory profile and response to anti-tumor necrosis factor therapy in patients with chronic pulmonary sarcoidosis. Clin. Vaccine Immunol. 2011, 18, 931–939. [Google Scholar] [CrossRef] [PubMed]
- Judson, M.A.; Baughman, R.P.; Costabel, U.; Drent, M.; Gibson, K.F.; Raghu, G.; Shigemitsu, H.; Barney, J.B.; Culver, D.A.; Hamzeh, N.Y. Safety and efficacy of ustekinumab or golimumab in patients with chronic sarcoidosis. Eur. Respir. J. 2014, 44, 1296–1307. [Google Scholar] [CrossRef] [PubMed]
- Carmona, E.M.; Kalra, S.; Ryu, J.H. Pulmonary sarcoidosis: Diagnosis and treatment. Mayo Clin. Proc. 2016, 91, 946–954. [Google Scholar] [CrossRef] [PubMed]
- Sauer, W.H.; Stern, B.J.; Baughman, R.P.; Culver, D.A.; Royal, W. High-risk sarcoidosis. Current concepts and research imperatives. Ann. Am. Thorac. Soc. 2017, 14, S437–S444. [Google Scholar] [CrossRef] [PubMed]
- Ahmadzai, H.; Huang, S.; Steinfort, C.; Markos, J.; Allen, R.K.; Wakefield, D.; Wilsher, M.; Thomas, P.S. Sarcoidosis: A state of the art review from the thoracic society of australia and new zealand. Med. J. Aust. 2018, 208, 499–504. [Google Scholar] [CrossRef]
- Baughman, R.P.; Grutters, J.C. New treatment strategies for pulmonary sarcoidosis: Antimetabolites, biological drugs, and other treatment approaches. Lancet Respir. Med. 2015, 3, 813–822. [Google Scholar] [CrossRef]
- Dastoori, M.; Fedele, S.; Leao, J.C.; Porter, S.R. Sarcoidosis—A clinically orientated review. J. Oral Pathol. Med. 2013, 42, 281–289. [Google Scholar] [CrossRef]
- Landi, C.; Carleo, A.; Cillis, G.; Rottoli, P. Sarcoidosis: Proteomics and new perspectives for improving personalized medicine. Expert Rev. Proteom. 2018, 15, 829–835. [Google Scholar] [CrossRef]
- Gligorijevic, V.; Malod-Dognin, N.; Przulj, N. Integrative methods for analyzing big data in precision medicine. Proteomics 2016, 16, 741–758. [Google Scholar] [CrossRef]
- Hočevar, K.; Maver, A.; Kunej, T.; Peterlin, B. Sarcoidosis related novel candidate genes identified by multi-omics integrative analyses. Omics J. Integr. Biol. 2018, 22, 322–331. [Google Scholar] [CrossRef] [PubMed]
| Organ Involvement | Prevalence of Organ Involvement | Manifestations | References |
|---|---|---|---|
| Lung involvement | more than 90% (With hilar and mediastinal lymph node) | Dry cough, wheezing, dysponea, fatigue Acute: Pleural effusion, pericardial effusion, pneumothorax, and lymph-node Chronic: lung fibrosis and respiratory failure | [80,81,82] |
| Lymph node involvement | 20% of patients | Peripheral lymphadenopathy, affected lymph nodes are moderately swollen, and are usually not painful. | [83,84,85] |
| Endocrine and exocrine involvement | Thyroid glands and parotid glands are usually affected in 20%–50% of cases | Thyroid dysfunction (5%), Parotid enlargement (5%–10%), hypothalamic-pituitary effects (for example, diabetes insipidus), | [86,87] |
| Skin involvement | 20%–30% of patients | Erythema nodosum (most common), profuse sweating, nodules, papules and plaques. | [88,89] |
| Eye involvement | more than 40% of patients | pain, photophobia, and hyperaemia, sometimes associated with the Löfgren syndrome | [90,91,92] |
| Bone involvement | 1%–13% of patients | Osteoporosis and osteopenia are common, Nodular lesions, cystic lesions involving the joints, arthritis and arthralgia | [93,94,95] |
| Upper respiratory tract | In most patients with systemic sarcoidosis | Larynx, nasopharynx and nose are affected | [96,97,98] |
| Renal involvement | 5% | Renal calculi, nephrocalcinosis, interstitial nephritis, and kidney failure | [99,100] |
| Cardiac involvement | 20%–27% of sarcoidosis | Heart failure, arrhythmias, syncope | [101,102] |
| Neurological involvement or neurosarcoidosis | less than 10% of patients | Facial palsy, Meningeal inflammation, encephalopathy, vasculopathy, seizures, hydrocephalus, and mass lesions | [103,104] |
| Liver and spleen involvement | 18% | Hepatosplenomegaly, intrahepatic cholestasis, and portal hypertension and altered liver function | [105,106,107] |
| Test | Indication for Sarcoidosis | References |
|---|---|---|
| Physical examination | fever, fatigue, malaise, weight loss, and erythema nodosum | [108] |
| Routine ophthalmologic examination | orbital and eyelid granulomas | [109] |
| Peripheral blood count | Lymphopenia | [110] |
| Renal function tests | High level of calcium, urea, and creatinine | [111] |
| Urine analysis | Hypercalciurea | [112] |
| Pulmonary function Tests | Assess pulmonary involvement and disease severity | [113] |
| Tissue biopsy | For the presence of granuloma (Lungs, lymph node, skin, salivary gland, conjunctiva) | [114] |
| Bronchial Biopsy | Detect pulmonary involvement, (Endobronchial ultrasound-guided transbronchial needle aspirate [EBUS-TBNA], Trans and endobronchial Biopsy) | [115,116] |
| Tuberculin skin test (Mantoux) | Negative in the most sarcoidosis patients | [117] |
| Chest X-ray | Bilateral hilar lymphadenopathy, Disseminated nodules in the lungs | [118,119] |
| HRCT | Differentiation of sarcoidosis from other pulmonary conditions | [120,121] |
| FDG-PET | Highly sensitive to detect cardiac and pulmonary involvement | [122] |
| Electrocardiogram (ECG) | Repolarization disturbances, Ectopic beats, Rhythm abnormalities | [123,124] |
| MRI | Detect neurological involvement, spinal cord, meninges, skull vault, and pituitary lesions. | [125,126] |
| Biomarkers | Indication for Sarcoidosis | Diagnostic Value | Prognostic Value | Disease Severity Assessment | References |
|---|---|---|---|---|---|
| Serological Biomarkers | |||||
| SACE |
| + | − | ++ | [129,130,131] |
| Chitotriosidase |
| − | − | ++ | [132,133,134] |
| Lysozyme |
| − | − | + | [135,136] |
| Neopterin |
| − | − | + | [137,138,139] |
| Hypercalcemia |
| − | − | + | [140,141,142] |
| Soluble IL2 receptor |
| − | + | ++ | [143,144,145] |
| SAA |
| + | − | + | [146,147,148] |
| Chemokines |
| − | + | + | [149,150,151] |
| KL 6 |
| − | + | + | [152] |
| IFN-gamma |
| − | − | − | [153,154] |
| TGF-β |
| − | + | + | [155,156] |
| TNF-α |
| − | − | − | [157,158] |
| Biomarkers in BAL | |||||
| CD4/CD8 ratio in BAL |
| + | − | + | [159,160] |
| Percentage of White Blood cells in BAL |
| - | − | + | [161,162] |
| Exhaled Breath Biomarkers | |||||
| 8-isoprostane |
| + | − | − | [163,164] |
| Carbon monoxide |
| − | − | − | [165] |
| Nitric oxide |
| − | − | − | [166,167] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jain, R.; Yadav, D.; Puranik, N.; Guleria, R.; Jin, J.-O. Sarcoidosis: Causes, Diagnosis, Clinical Features, and Treatments. J. Clin. Med. 2020, 9, 1081. https://doi.org/10.3390/jcm9041081
Jain R, Yadav D, Puranik N, Guleria R, Jin J-O. Sarcoidosis: Causes, Diagnosis, Clinical Features, and Treatments. Journal of Clinical Medicine. 2020; 9(4):1081. https://doi.org/10.3390/jcm9041081
Chicago/Turabian StyleJain, Rashi, Dhananjay Yadav, Nidhi Puranik, Randeep Guleria, and Jun-O Jin. 2020. "Sarcoidosis: Causes, Diagnosis, Clinical Features, and Treatments" Journal of Clinical Medicine 9, no. 4: 1081. https://doi.org/10.3390/jcm9041081
APA StyleJain, R., Yadav, D., Puranik, N., Guleria, R., & Jin, J.-O. (2020). Sarcoidosis: Causes, Diagnosis, Clinical Features, and Treatments. Journal of Clinical Medicine, 9(4), 1081. https://doi.org/10.3390/jcm9041081







