Yoga and Mindfulness as a Tool for Influencing Affectivity, Anxiety, Mental Health, and Stress among Healthcare Workers: Results of a Single-Arm Clinical Trial
Abstract
1. Introduction
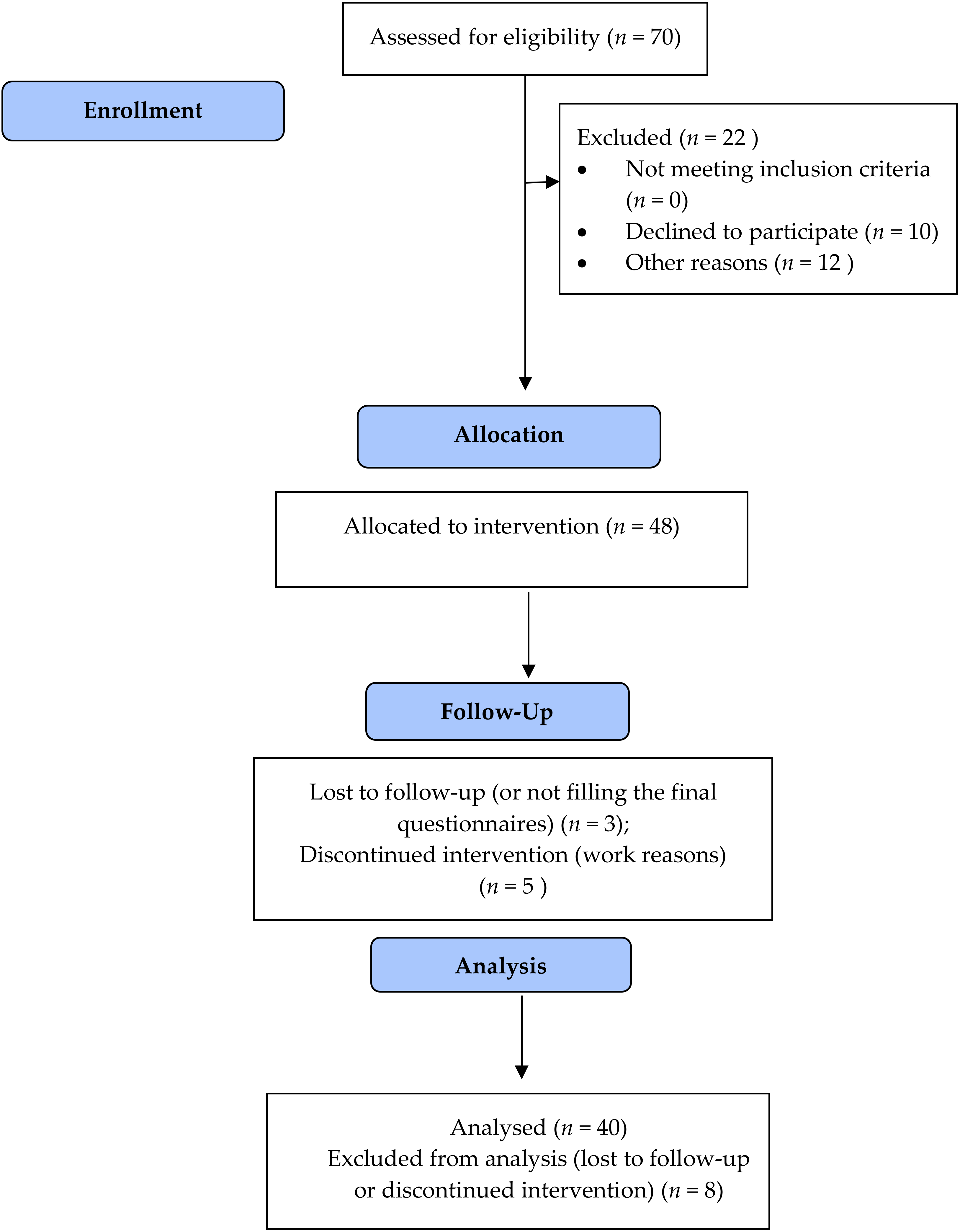
2. Materials and Methods
2.1. Settings and Participants
2.2. Intervention
- 5–10 min of starting session with motivational purposes
- 30 min of breathing, posture, and sound exercises meant to achieve benefits for work-related stress and burnout (shoulders, neck, hips, and leg muscles were the most treated body district)
- 20 min of pranayama, aiming at slowing and controlling breathing with diaphragmatic respiration exercises to reduce perceived anxiety. The most used pranayamas were “bastrika” breathing, Nadi Shodana, alternate nostrils breathing, and breath of fire. Participants were asked to do home practice by performing the yoga programs as often as possible, at least twice a week.
- 20 min of specific meditation exercises with movements and postures for releasing tension, relieving fatigue, and achieving mental well-being.
- 5 min of mantra (formula repeated many times with meditative purposes)
- 10 min of relaxation
2.3. Instruments
- before the beginning of the course: SF-12, the 15-item form of Karasek, and STAI Y2
- before starting each 4 h session: STAI Y1 and PANAS
- at the end of each 4 h session: STAI Y1 and PANAS
- 21 days after the courses: SF-12, a short form of Karasek, and STAI Y2.
2.3.1. SF-12
2.3.2. Job Content Questionnaire
- decision latitude;
- psychological demands;
- social support;
- physical demands;
- job insecurity.
2.3.3. STAI
2.3.4. PANAS
2.4. Statistical Analysis
3. Results
3.1. Univariate Analysis: Comparison Pre- and Postintervention
3.1.1. SF-12
3.1.2. JCQ
3.1.3. PANAS
3.1.4. STAI
3.2. Multivariate Analysis: Linear Regression on Delta Scores
4. Discussion
4.1. Limitations
4.2. Directions for Future Research
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Baer, R.A. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clin. Psychol. Sci. Pract. 2003, 10, 125–143. [Google Scholar] [CrossRef]
- Didonna, F. Introduction: Where new and old paths to dealing with suffering meet. In Clinical Handbook of Mindfulness; Didonna, F., Ed.; Springer: New York, NY, USA, 2009; pp. 1–17. [Google Scholar]
- Chiesa, A.; Serretti, A. Mindfulness based cognitive therapy for psychiatric disorders: A systematic review and meta-analysis. Psychiatry Res. 2011, 187, 441–453. [Google Scholar] [CrossRef] [PubMed]
- Malinowski, P. Neural mechanisms of attentional control in mindfulness meditation. Front. Neurosci. 2013, 7, 8. [Google Scholar] [CrossRef]
- Alberts, H.; Hülsheger, U. Applying mindfulness in the context of work: Mindfulness-based interventions. In Mindfulness in Organizations. Foundations, Research and Applications; Reb, J., Atkins, P.W.B., Eds.; Cambridge University Press: Cambridge, UK, 2015; pp. 100–132. [Google Scholar]
- Lazar, S.W.; Kerr, C.E.; Wasserman, R.H.; Gray, J.R.; Greve, D.N.; Treadway, M.T.; McGarvey, M.; Quinn, B.T.; Dusek, J.A.; Benson, H.; et al. Meditation experience is associated with increased cortical thickness. Neuroreport 2005, 16, 1893–1897. [Google Scholar] [CrossRef]
- Tang, Y.Y.; Lu, Q.; Fan, M.; Yang, Y.; Posner, M.I. Mechanisms of white matter changes induced by meditation. Proc. Natl. Acad. Sci. USA 2012, 109, 10570–10574. [Google Scholar] [CrossRef]
- Zeidan, F.; Johnson, S.K.; Diamond, B.J.; David, Z.; Goolkasian, P. Mindfulness meditation improves cognition: Evidence of brief mental training. Conscious. Cogn. 2010, 19, 597–605. [Google Scholar] [CrossRef]
- Slagter, H.A.; Davidson, R.J.; Lutz, A. Mental training as a tool in the scientific study of brain and cognitive plasticity. Front. Hum. Neurosci. 2011, 5, 17. [Google Scholar] [CrossRef] [PubMed]
- Davis, D.M.; Hayes, J.A. What are the benefits of mindfulness? A practice review of psychotherapy-related research. Psychotherapy 2011, 48, 198–208. [Google Scholar] [CrossRef]
- Lomas, T.; Medina, J.C.; Ivtzan, I.; Rupprecht, S.; Hart, R.; Eiroa-Orosa, F.J. The impact of mindfulness on well-being and performance in the workplace: An inclusive systematic review of the empirical literature. Eur. J. Work Organ. Psychol. 2017, 26, 492–513. [Google Scholar] [CrossRef]
- Gard, T.; Holzel, B.K.; Lazar, S.W. The potential effects of meditation on age-related cognitive decline: A systematic review. Ann. N. Y. Acad. Sci. 2014, 1307, 89–103. [Google Scholar] [CrossRef]
- Luders, E. Exploring age-related brain degeneration in meditation practitioners. Ann. N. Y. Acad. Sci. 2014, 1307, 82–88. [Google Scholar] [CrossRef] [PubMed]
- Bischoff, L.L.; Otto, A.K.; Hold, C.; Wollesen, B. The effect of physical activity interventions on occupational stress for health personnel: A systematic review. Int. J. Nurs. Stud. 2019, 97, 94–104. [Google Scholar] [CrossRef]
- Cocchiara, R.A.; Peruzzo, M.; Mannocci, A.; Ottolenghi, L.; Villari, P.; Polimeni, A.; Guerra, F.; La Torre, G. The use of yoga to manage stress and burnout in healthcare workers: A systematic review. J. Clin. Med. 2019, 8, 284. [Google Scholar] [CrossRef] [PubMed]
- García-Sesnich, J.N.; Flores, M.G.; Ríos, M.H.; Aravena, J.G. Longitudinal and immediate effect of Kundalini Yoga on salivary levels of cortisol and activity of alpha-amylase and its effect on perceived stress. Int. J. Yoga 2017, 10, 73–80. [Google Scholar] [CrossRef] [PubMed]
- Gabriel, M.G.; Curtiss, J.; Hofmann, S.G.; Khalsa, S.B.S. Kundalini Yoga for generalized anxiety disorder: An exploration of treatment efficacy and possible mechanisms. Int. J. Yoga Therap. 2018, 28, 97–105. [Google Scholar] [CrossRef]
- Wolff, M. Yoga as a Treatment for Hypertension in Primary Care. A Quantitative and Qualitative Analysis Conducted in Sweden. Ph.D. Thesis, Lund University, Lund, Sweden, 2016. [Google Scholar]
- Tang, Y.Y.; Posner, M.I. Training brain networks and states. Trends Cogn. Sci. 2014, 18, 345–350. [Google Scholar] [CrossRef]
- Raffone, A.; Srinivasan, N. Mindfulness and cognitive functions: Toward a unifying neurocognitive framework. Mindfulness 2017, 8, 1–9. [Google Scholar] [CrossRef]
- Raffone, A.; Marzetti, L.; Del Gratta, C.; Perrucci, M.G.; Romani, G.L.; Pizzella, V. Toward a brain theory of meditation. Prog. Brain Res. 2019, 244, 207–232. [Google Scholar]
- Kabat-Zinn, J. Mindfulness-based interventions in context: Past, present and future. Clin. Psychol. Sci. Pract. 2003, 10, 144–156. [Google Scholar] [CrossRef]
- Ruiz-Fernández, M.D.; Ortíz-Amo, R.; Ortega-Galán, Á.M.; Ibáñez-Masero, O.; Rodríguez-Salvador, M.D.M.; Ramos-Pichardo, J.D. Mindfulness therapies on health professionals. Int. J. Ment. Health Nurs. 2020, 29, 127–140. [Google Scholar] [CrossRef]
- Mackenzie, C.S.; Poulin, P.A.; Seidman-Carlson, R. A brief mindfulness-based stress reduction intervention for nurses and nurse aides. Appl. Nurs. Res. 2006, 19, 105–109. [Google Scholar] [CrossRef]
- Bergen-Cico, D.; Possemato, K.; Pigeon, W. Reductions in cortisol associated with primary care brief mindfulness program for veterans with PTSD. Med. Care 2014, 52, S25–S31. [Google Scholar] [CrossRef] [PubMed]
- Kabat-Zinn, J.; Kabat-Zinn, J. Bringing mindfulness to medicine. Interview by Karolyn, A. Gazella. Altern. Ther. Health Med. 2005, 11, 56–64. [Google Scholar]
- Lutz, A.; Slagter, H.A.; Dunne, J.D.; Davidson, R.J. Attention regulation and monitoring in meditation. Trends Cogn. Sci. 2008, 12, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Edwards, M.K.; Rosenbaum, S.; Loprinzi, P.D. Differential experimental effects of a short bout of walking, meditation, or combination of walking and meditation on state anxiety among young adults. Am. J. Health Promot. 2018, 32, 949–958. [Google Scholar] [CrossRef] [PubMed]
- Tang, Y.; Ma, Y.; Wang, J.; Fan, Y.; Feng, S.; Lu, Q.; Sui, D.; Rothbart, M.K.; Posner, M.I. Short-term meditation training improves attention and self-regulation. Proc. Natl. Acad. Sci. USA 2007, 104, 17152–17156. [Google Scholar] [CrossRef]
- Tang, Y.Y.; Hölzel, B.K.; Posner, M.I. The neuroscience of mindfulness meditation. Nat. Rev. Neurosci. 2015, 16, 213–225. [Google Scholar] [CrossRef]
- Ware, J.E.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36) I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Jenkinson, C.; Layte, R.; Jenkinson, D.; Lawrence, K.; Petersen, S.; Paice, C.; Stradling, J. A shorter form health survey: Can the SF-12 replicate results from the SF-36 in longitudinal studies? J. Public Health Med. 1997, 19, 179–186. [Google Scholar] [CrossRef]
- Karasek, R.; Brisson, C.; Kawakami, N.; Houtman, I.; Bongers, P.; Amick, B. The Job Content Questionnaire (JCQ): An instrument for internationally comparative assessments of psychosocial job characteristics. J. Occup. Health Psychol. 1998, 3, 322–355. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.; Vagg, P.R.; Jacobs, G.A. Manual for the State-Trait Anxiety Inventory; Consulting Psychologists Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Watson, D.; Clark, L.A.; Tellegen, A. Development and validation of brief measures of positive and negative affect: The PANAS scales. J. Pers. Soc. Psychol. 1988, 54, 1063–1070. [Google Scholar] [CrossRef] [PubMed]
- Crawford, J.R.; Henry, J.D. The positive and negative affect schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. Br. J. Clin. Psychol. 2004, 43, 245–265. [Google Scholar] [CrossRef] [PubMed]
- Mannocci, A.; Sestili, C.; Carnevale, F.; Minotti, C.; De Giusti, M.; Villari, P.; Foà, R.; Cartoni, C.; La Torre, G. Assessment of burnout in health care personnel in hematological unit of a teaching hospital. G. Ital. Med. Lav. Ergon. 2019, 41, 45–51. [Google Scholar] [PubMed]
- Fang, R.; Li, X. A regular yoga intervention for staff nurse sleep quality and work stress: A randomised controlled trial. J. Clin. Nurs. 2015, 24, 3374–3379. [Google Scholar] [CrossRef] [PubMed]
- Riley, K.E.; Park, C.L.; Wilson, A.; Sabo, A.N.; Antoni, M.H.; Braun, T.D.; Harrington, J.; Reiss, J.; Pasalis, E.; Harris, A.D.; et al. Improving physical and mental health in frontline mental health care providers: Yoga-based stress management versus cognitive behavioral stress management. J. Workplace Behav. Health 2017, 32, 26–48. [Google Scholar] [CrossRef]
- Klatt, M.; Steinberg, B.; Duchemin, A.M. Mindfulness in Motion (MIM): An Onsite Mindfulness Based Intervention (MBI) for chronically high stress work environments to increase resiliency and work engagement. J. Vis. Exp. 2015, 101, e52359. [Google Scholar] [CrossRef]
- Lamothe, M.; Rondeau, É.; Malboeuf-Hurtubise, C.; Duval, M.; Sultan, S. Outcomes of MBSR or MBSR-based interventions in health care providers: A systematic review with a focus on empathy and emotional competencies. Complement Ther. Med. 2016, 24, 19–28. [Google Scholar] [CrossRef]
- Spinelli, C.; Wisener, M.; Khoury, B. Mindfulness training for healthcare professionals and trainees: A meta-analysis of randomized controlled trials. J. Psychosom. Res. 2019, 120, 29–38. [Google Scholar] [CrossRef]
- Smith, S.A. Mindfulness-based stress reduction: An intervention to enhance the effectiveness of nurses’ coping with work-related stress. Int. J. Nurs. Knowl. 2014, 25, 119–130. [Google Scholar] [CrossRef]
- Stillwell, S.B.; Vermeesch, A.L.; Scott, J.G. Interventions to reduce perceived stress among graduate students: A systematic review with implications for evidence-based practice. Worldviews Evid. Based Nurs. 2017, 14, 507–513. [Google Scholar] [CrossRef]
- O’Driscoll, M.; Byrne, S.; Mc Gillicuddy, A.; Lambert, S.; Sahm, L.J. The effects of mindfulness-based interventions for health and social care undergraduate students - a systematic review of the literature. Psychol. Health Med. 2017, 22, 851–865. [Google Scholar] [CrossRef] [PubMed]
- Van den Heuvel, S.G.; Roozeboom, B.; Eekhout, I.; Venema, A. Management of Psychosocial Risks in European Workplaces: Evidence from the Second European Survey of Enterprises on New and Merging Risks (ESENER-2). 2019. Available online: https://osha.europa.eu/en/publications/management-psychosocial-risks-european-workplaces-evidence-second-european-survey (accessed on 6 April 2020).
| Variable | n (%) or Mean (SD) |
|---|---|
| Gender | |
| Females | 34 (85) |
| Males | 6 (15) |
| Age | 47.3 (10.9) |
| Health Professions | |
| Physicians | 13 (32.5) |
| Nurses | 15 (37.5) |
| Other HCW | 12 (30) |
| Hospital | |
| Teaching hospital | 28 (70) |
| Pediatric hospital | 12 (30) |
| Variables | Pre-Course Median (Min–Max) | Post-Course Median (Min–Max) | p-Value |
|---|---|---|---|
| SF-12: | |||
| MCS-12 | 43.5 (21.5–59.4) | 48.1 (20.4–56.7) | 0.041 |
| PCS-12 | 49.4 (36.2–65.5) | 54.8 (36.6–60.5) | 0.09 |
| JCQ: | |||
| Decision latitude | 54 (42–66) | 54 (4– 68) | 0.419 |
| Job demand | 27 (11–41) | 26 (12–38) | 0.373 |
| Job strain | 0.76 (0.28–1.18) | 0.72 (0.36–1.08) | 0.100 |
| PANAS: | |||
| Positive | 37 (21–49) | 36.5 (18–50) | 0.762 |
| Negative | 16 (10–34) | 10 (8–26) | <0.001 |
| STAI Y2 (trait) | 46.0 (38–56) | 43.5 (32–55) | 0.009 |
| STAI Y1 (state) | 62 (55–72) | 45.5 (34–52) | <0.001 |
| Variables | Gender | Age | Physicians | Teaching Hospital | R2 |
|---|---|---|---|---|---|
| SF-12 | |||||
| MCS-12 | −0.005 (0.979) | 0.056 (0.772) | 0.089 (0.606) | −0.075 (0.702) | 0.014 |
| PCS-12 | −0.05 (0.765) | −0.205 (0.268) | 0.123 (0.457) | 0.373 (0.052) | 0.111 |
| Karasek | |||||
| Decision latitude | −0.074 (0.646) | 0.092 (0.604) | 0.050 (0-753) | −0.422 (0.024) | 0.171 |
| Job demand | −0.058 (0.728) | −0.138 (0.458) | −0.176 (0.296) | 0.243 (0.204) | 0.086 |
| Job strain | −0.032 (0.838) | −0.204 (0.248) | −0.141 (0.372) | 0.455 (0.015) | 0.189 |
| PANAS | |||||
| Positive | 0.0 (0.999) | 0.284 (0.127) | 0.227 (0.173) | −0.075 (0.689) | 0.111 |
| Negative | −0.185 (0.276) | 0.010 (0.959) | 0.098 (0.559) | −0.171 (0.370) | 0.082 |
| STAI Y2 trait | 0.115 (0.483) | −0.128 (0.481) | −0.326 (0.05) | −0.122 (0.510) | 0.130 |
| STAI Y1 state | 0.089 (0.601) | 0.197 (0.298) | 0.053 (0.755) | 0.082 (0.671) | 0.061 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
La Torre, G.; Raffone, A.; Peruzzo, M.; Calabrese, L.; Cocchiara, R.A.; D’Egidio, V.; Leggieri, P.F.; Dorelli, B.; Zaffina, S.; Mannocci, A.; et al. Yoga and Mindfulness as a Tool for Influencing Affectivity, Anxiety, Mental Health, and Stress among Healthcare Workers: Results of a Single-Arm Clinical Trial. J. Clin. Med. 2020, 9, 1037. https://doi.org/10.3390/jcm9041037
La Torre G, Raffone A, Peruzzo M, Calabrese L, Cocchiara RA, D’Egidio V, Leggieri PF, Dorelli B, Zaffina S, Mannocci A, et al. Yoga and Mindfulness as a Tool for Influencing Affectivity, Anxiety, Mental Health, and Stress among Healthcare Workers: Results of a Single-Arm Clinical Trial. Journal of Clinical Medicine. 2020; 9(4):1037. https://doi.org/10.3390/jcm9041037
Chicago/Turabian StyleLa Torre, Giuseppe, Antonino Raffone, Margherita Peruzzo, Lucia Calabrese, Rosario Andrea Cocchiara, Valeria D’Egidio, Pasquale Fabio Leggieri, Barbara Dorelli, Salvatore Zaffina, Alice Mannocci, and et al. 2020. "Yoga and Mindfulness as a Tool for Influencing Affectivity, Anxiety, Mental Health, and Stress among Healthcare Workers: Results of a Single-Arm Clinical Trial" Journal of Clinical Medicine 9, no. 4: 1037. https://doi.org/10.3390/jcm9041037
APA StyleLa Torre, G., Raffone, A., Peruzzo, M., Calabrese, L., Cocchiara, R. A., D’Egidio, V., Leggieri, P. F., Dorelli, B., Zaffina, S., Mannocci, A., & YOMIN Collaborative Group. (2020). Yoga and Mindfulness as a Tool for Influencing Affectivity, Anxiety, Mental Health, and Stress among Healthcare Workers: Results of a Single-Arm Clinical Trial. Journal of Clinical Medicine, 9(4), 1037. https://doi.org/10.3390/jcm9041037







