Comparison of Renal Effects of Ezetimibe–Statin Combination versus Statin Monotherapy: A Propensity-Score-Matched Analysis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design and Population
2.2. Study Outcomes
2.3. Statistical Analysis
3. Results
3.1. Study-Population Characteristics
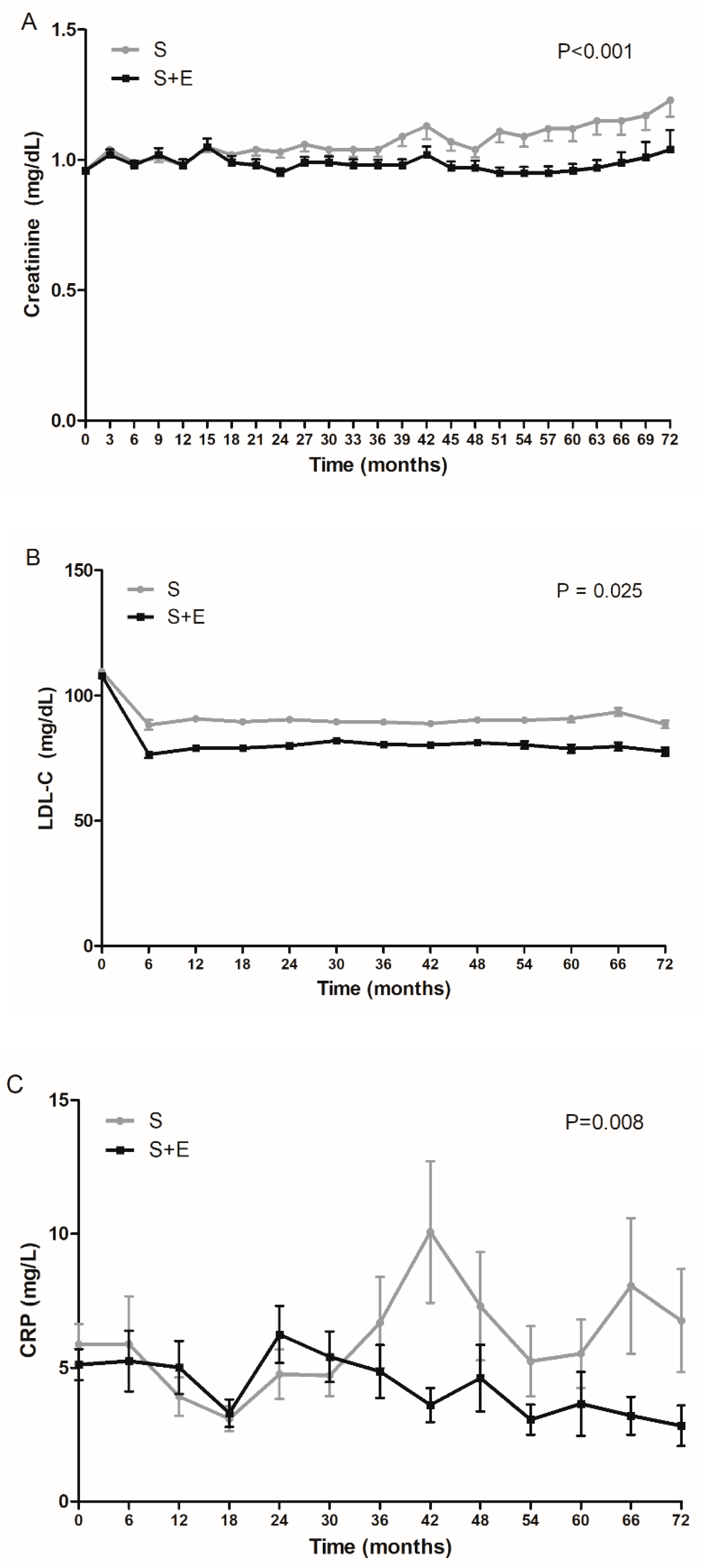
3.2. Effects of S + E or S on Changes of Serum Creatinine, LDL-Cholesterol, and CRP
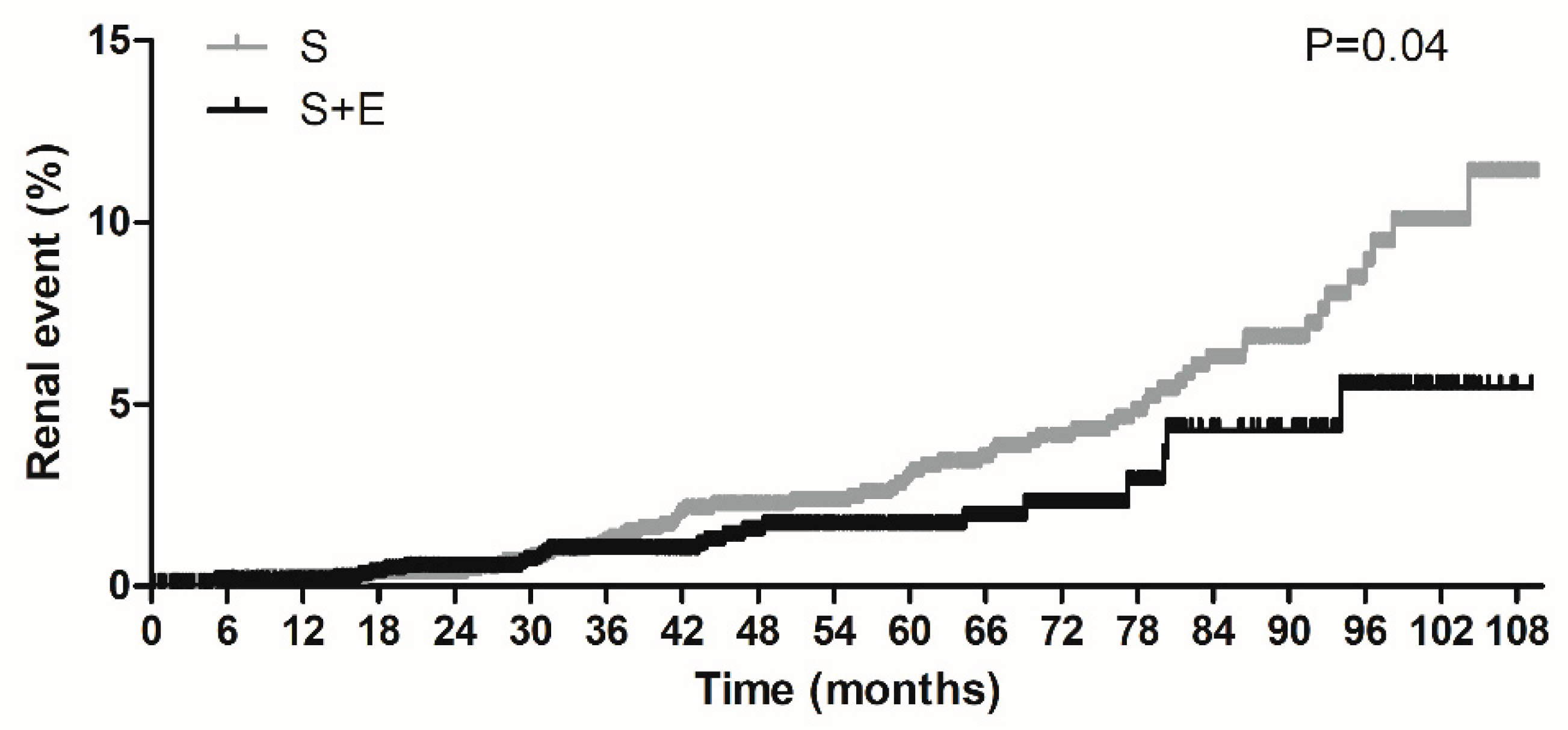
3.3. Effects of S + E or S on Occurrence of Renal Events
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- GBD 2015 DALYs and HALE Collaborator. Global, regional, and national disability-adjusted life-years (dalys) for 315 diseases and injuries and healthy life expectancy (hale), 1990-2015: A systematic analysis for the global burden of disease study 2015. Lancet 2016, 388, 1603–1658. [Google Scholar] [CrossRef] [Green Version]
- Inker, L.A.; Astor, B.C.; Fox, C.H.; Isakova, T.; Lash, J.P.; Peralta, C.A.; Tamura, M.K.; Feldman, H. KDOQI US Commentary on the 2012 KDIGO Clinical Practice Guideline for the Evaluation and Management of CKD. Am. J. Kidney Dis. 2014, 63, 713–735. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Thomas, B.; Matsushita, K.; Abate, K.H.; Al-Aly, Z.; Ärnlöv, J.; Asayama, K.; Atkins, R.; Badawi, A.; Ballew, S.; Banerjee, A.; et al. Global Cardiovascular and Renal Outcomes of Reduced GFR. J. Am. Soc. Nephrol. 2017, 28, 2167–2179. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lewis, E.J.; Hunsicker, L.G.; Rohde, R.D.; Bain, R.P. The Effect of Angiotensin-Converting-Enzyme Inhibition on Diabetic Nephropathy. N. Engl. J. Med. 1993, 329, 1456–1462. [Google Scholar] [CrossRef] [PubMed]
- Lewis, E.J.; Hunsicker, L.G.; Clarke, W.R.; Berl, T.; Pohl, M.A.; Lewis, J.B.; Ritz, E.; Atkins, R.C.; Rohde, R.; Raz, I. Renoprotective Effect of the Angiotensin-Receptor Antagonist Irbesartan in Patients with Nephropathy Due to Type 2 Diabetes. N. Engl. J. Med. 2001, 345, 851–860. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- American Diabetes Association. 11. Microvascular complications and foot care: Standards of medical care in diabetes—2019. Diabetes Care 2019, 42, S124–S138. [Google Scholar] [CrossRef] [Green Version]
- Wanner, C.; Inzucchi, S.E.; Lachin, J.M.; Fitchett, D.; Von Eynatten, M.; Mattheus, M.; Johansen, O.E.; Woerle, H.J.; Broedl, U.C.; Zinman, B. Empagliflozin and Progression of Kidney Disease in Type 2 Diabetes. N. Engl. J. Med. 2016, 375, 323–334. [Google Scholar] [CrossRef]
- Perkovic, V.; Jardine, M.J.; Neal, B.; Bompoint, S.; Heerspink, H.J.; Charytan, D.M.; Edwards, R.; Agarwal, R.; Bakris, G.; Bull, S.; et al. Canagliflozin and Renal Outcomes in Type 2 Diabetes and Nephropathy. N. Engl. J. Med. 2019, 380, 2295–2306. [Google Scholar] [CrossRef] [Green Version]
- Stone, N.J.; Robinson, J.G.; Lichtenstein, A.H.; Merz, C.N.B.; Blum, C.B.; Eckel, R.H.; Goldberg, A.C.; Gordon, D.; Levy, D.; Lloyd-Jones, D.M.; et al. 2013 ACC/AHA Guideline on the Treatment of Blood Cholesterol to Reduce Atherosclerotic Cardiovascular Risk in Adults: A report of the american college of cardiology/american heart association task force on practice guidelines. J. Am. Coll. Cardiol. 2014, 63, 2889–2934. [Google Scholar] [CrossRef] [Green Version]
- Schaeffner, E.S.; Kurth, T.; Curhan, G.C.; Glynn, R.J.; Rexrode, K.M.; Baigent, C.; Buring, J.E.; Gaziano, J. Cholesterol and the risk of renal dysfunction in apparently healthy men. J. Am. Soc. Nephrol. 2003, 14, 2084–2091. [Google Scholar]
- Mänttäri, M.; Tiula, E.; Alikoski, T.; Manninen, V. Effects of Hypertension and Dyslipidemia on the Decline in Renal Function. Hypertension 1995, 26, 670–675. [Google Scholar] [CrossRef] [PubMed]
- Sandhu, S.; Wiebe, N.; Fried, L.F.; Tonelli, M. Statins for Improving Renal Outcomes: A Meta-Analysis. J. Am. Soc. Nephrol. 2006, 17, 2006–2016. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- He, Y.; Li, X.; Gasevic, D.; Brunt, E.; McLachlan, F.; Millenson, M.; Timofeeva, M.; Ioannidis, J.P.; Campbell, H.; Theodoratou, E. Statins and Multiple Noncardiovascular Outcomes. Ann. Intern. Med. 2018, 169, 543. [Google Scholar] [CrossRef] [PubMed]
- Kimura, G.; Kasahara, M.; Ueshima, K.; Tanaka, S.; Yasuno, S.; Fujimoto, A.; Sato, T.; Imamoto, M.; Kosugi, S.; Nakao, K. Effects of atorvastatin on renal function in patients with dyslipidemia and chronic kidney disease: Assessment of clinical usefulness in CKD patients with atorvastatin (ASUCA) trial. Clin. Exp. Nephrol. 2016, 21, 417–424. [Google Scholar] [CrossRef] [Green Version]
- Jellinger, P.S.; Handelsman, Y.; Rosenblit, P.D.; Bloomgarden, Z.T.; Fonseca, V.; Garber, A.J.; Grunberger, G.; Guerin, C.K.; Bell, D.S.; Mechanick, J.I.; et al. American association of clinical endocrinologists and american college of endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr. Pract. 2017, 23, 1–87. [Google Scholar] [CrossRef]
- Lloyd-Jones, D.M.; Morris, P.B.; Ballantyne, C.M.; Birtcher, K.K.; Daly, D.D.; DePalma, S.; Minissian, M.B.; Orringer, C.E.; Smith, S.C. 2017 Focused Update of the 2016 ACC Expert Consensus Decision Pathway on the Role of Non-Statin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk. J. Am. Coll. Cardiol. 2017, 70, 1785–1822. [Google Scholar] [CrossRef]
- Nutescu, E.A.; Shapiro, N.L. Ezetimibe: A selective cholesterol absorption inhibitor. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2003, 23, 1463–1474. [Google Scholar] [CrossRef]
- Ai, C.; Zhang, S.; He, Q.; Shi, J. Comparing the combination therapy of ezetimibe and atorvastatin with atorvastatin monotherapy for regulating blood lipids: A systematic review and meta-analyse. Lipids Health Dis. 2018, 17, 239. [Google Scholar] [CrossRef] [Green Version]
- Ahmed, O.; Littmann, K.; Gustafsson, U.; Pramfalk, C.; Öörni, K.; Larsson, L.; Minniti, M.E.; Sahlin, S.; Camejo, G.; Parini, P.; et al. Ezetimibe in Combination With Simvastatin Reduces Remnant Cholesterol Without Affecting Biliary Lipid Concentrations in Gallstone Patients. J. Am. Heart Assoc. 2018, 7, 009876. [Google Scholar] [CrossRef] [Green Version]
- Hwang, Y.; Jun, J.E.; Jeong, I.-K.; Ahn, K.J.; Chung, H.Y. Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus. Diabetes Metab. J. 2019, 43, 582. [Google Scholar] [CrossRef]
- Lee, Y.-H.; Hong, N.; Lee, C.J.; Park, S.; Lee, B.-W.; Cha, B.-S.; Kang, E.S. Differential association of ezetimibe-simvastatin combination with major adverse cardiovascular events in patients with or without diabetes: A retrospective propensity score-matched cohort study. Sci. Rep. 2018, 8, 11925. [Google Scholar] [CrossRef] [PubMed]
- Hong, N.; Lee, Y.-H.; Tsujita, K.; Gonzalez, J.A.; Kramer, C.M.; Kovárník, T.; Kouvelos, G.N.; Suzuki, H.; Han, K.; Lee, C.J.; et al. Comparison of the Effects of Ezetimibe-Statin Combination Therapy on Major Adverse Cardiovascular Events in Patients with and without Diabetes: A Meta-Analysis. Endocrinol. Metab. 2018, 33, 219–227. [Google Scholar] [CrossRef]
- Kim, S.H.; Kim, G.; Han, D.H.; Lee, M.; Kim, I.; Kim, B.; Kim, K.H.; Song, Y.-M.; Yoo, J.E.; Wang, H.J.; et al. Ezetimibe ameliorates steatohepatitis via AMP activated protein kinase-TFEB-mediated activation of autophagy and NLRP3 inflammasome inhibition. Autophagy 2017, 13, 1767–1781. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.; Li, X.; Matei, N.; McBride, D.W.; Tang, J.; Yan, M.; Zhang, F. Ezetimibe, a NPC1L1 inhibitor, attenuates neuronal apoptosis through AMPK dependent autophagy activation after MCAO in rats. Exp. Neurol. 2018, 307, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Kimura, T.; Isaka, Y.; Yoshimori, T. Autophagy and kidney inflammation. Autophagy 2017, 13, 997–1003. [Google Scholar] [CrossRef]
- Kinouchi, K.; Ichihara, A.; Bokuda, K.; Morimoto, S.; Itoh, H. Effects of adding ezetimibe to fluvastatin on kidney function in patients with hypercholesterolemia: A randomized control trial. J. Atheroscler. Thromb. 2012, 20, 245–256. [Google Scholar] [CrossRef] [Green Version]
- Nakamura, T.; Sato, E.; Fujiwara, N.; Kawagoe, Y.; Ueda, Y.; Suzuki, T.; Ueda, S.; Fukami, K.; Okuda, S.; Hirano, T. Co-administration of ezetimibe enhances proteinuria-lowering effects of pitavastatin in chronic kidney disease patients partly via a cholesterol-independent manner. Pharmacol. Res. 2010, 61, 58–61. [Google Scholar] [CrossRef]
- Kouvelos, G.; Arnaoutoglou, E.M.; Milionis, H.J.; Raikou, V.; Papa, N.; Matsagkas, M.I. The Effect of Adding Ezetimibe to Rosuvastatin on Renal Function in Patients Undergoing Elective Vascular Surgery. Angiology 2014, 66, 128–135. [Google Scholar] [CrossRef]
- Suzuki, H.; Watanabe, Y.; Kumagai, H.; Shuto, H. Comparative efficacy and adverse effects of the addition of ezetimibe to statin versus statin titration in chronic kidney disease patients. Ther. Adv. Cardiovasc. Dis. 2013, 7, 306–315. [Google Scholar] [CrossRef]
- Kazancıoğlu, R. Risk factors for chronic kidney disease: An update. Kidney Int. Suppl. 2013, 3, 368–371. [Google Scholar] [CrossRef] [Green Version]
- Suleymanlar, G.; Utaş, C.; Arinsoy, T.; Ateş, K.; Altun, B.; Altiparmak, M.R.; Ecder, T.; Yilmaz, M.E.; Çamsari, T.; Başçi, A.; et al. A population-based survey of Chronic REnal Disease In Turkey—The CREDIT study. Nephrol. Dial. Transplant. 2010, 26, 1862–1871. [Google Scholar] [CrossRef] [PubMed]
- Lea, J.P.; Nicholas, S.B. Diabetes mellitus and hypertension: Key risk factors for kidney disease. J. Natl. Med Assoc. 2002, 94, 7S–15S. [Google Scholar] [PubMed]
- Klag, M.J.; Whelton, P.K.; Randall, B.L.; Neaton, J.D.; Brancati, F.L.; Ford, C.E.; Shulman, N.B.; Stamler, J. Blood Pressure and End-Stage Renal Disease in Men. N. Engl. J. Med. 1996, 334, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Pugliese, G. Updating the natural history of diabetic nephropathy. Acta Diabetol. 2014, 51, 905–915. [Google Scholar] [CrossRef]
- Kim, K.-S.; Park, S.W.; Cho, Y.-W.; Kim, S.-K. Higher Prevalence and Progression Rate of Chronic Kidney Disease in Elderly Patients with Type 2 Diabetes Mellitus. Diabetes Metab. J. 2018, 42, 224–232. [Google Scholar] [CrossRef]
- McClellan, W.M. Risk Factors for Progressive Chronic Kidney Disease. J. Am. Soc. Nephrol. 2003, 14, 65–70. [Google Scholar] [CrossRef] [Green Version]
- French, S.W.; Yamanaka, W.; Ostwald, R. Dietary induced glomerulosclerosis in the guinea pig. Arch. Pathol. 1967, 83, 204–210. [Google Scholar]
- Wellmann, K.F.; Volk, B.W. Renal changes in experimental hypercholesterolemia in normal and in subdiabetic rabbits. II. Long term studies. Lab. Investig. 1971, 24, 144–155. [Google Scholar]
- Kasiske, B.L.; Phillips, W.T.T.A.O.F.; O’Donnell, M.E.; Schmitz, P.G.; Kim, Y.; Keane, W.F.; Daniels, F.; Holden, G. Renal injury of diet-induced hypercholesterolemia in rats. Kidney Int. 1990, 37, 880–891. [Google Scholar] [CrossRef] [Green Version]
- Hunsicker, L.G.; Modification of Diet in Renal Disease Study Group; Adler, S.; Caggiula, A.; England, B.K.; Greene, T.; Kusek, J.W.; Rogers, N.L.; Teschan, P.E.; Beck, G. Predictors of the progression of renal disease in the Modification of Diet in Renal Disease Study. Kidney Int. 1997, 51, 1908–1919. [Google Scholar] [CrossRef] [Green Version]
- Fried, L.F.; Orchard, T.; Kasiske, B.L. Effect of lipid reduction on the progression of renal disease: A meta-analysis. Kidney Int. 2001, 59, 260–269. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Haynes, R.; Lewis, D.; Emberson, J.; Reith, C.; Agodoa, L.; Cass, A.; Craig, J.; De Zeeuw, D.; Feldt-Rasmussen, B.; Fellström, B.; et al. Effects of Lowering LDL Cholesterol on Progression of Kidney Disease. J. Am. Soc. Nephrol. 2014, 25, 1825–1833. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Laufs, U.; Gertz, K.; Huang, P.; Nickenig, G.; Dirnagl, U.; Endres, M.; Böhm, M.; Vaughan, C.J. Atorvastatin Upregulates Type III Nitric Oxide Synthase in Thrombocytes, Decreases Platelet Activation, and Protects From Cerebral Ischemia in Normocholesterolemic Mice. Stroke 2000, 31, 2442–2449. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Antoniades, C.; Bakogiannis, C.; Leeson, P.; Guzik, T.J.; Zhang, M.-H.; Tousoulis, D.; Antonopoulos, A.S.; Demosthenous, M.; Marinou, K.; Hale, A.; et al. Rapid, direct effects of statin treatment on arterial redox state and nitric oxide bioavailability in human atherosclerosis via tetrahydrobiopterin-mediated endothelial nitric oxide synthase coupling. Circulation 2011, 124, 335–345. [Google Scholar] [CrossRef]
- Cohn, J.N.; Wilson, D.J.; Neutel, J.; Houston, M.; Weinberger, M.H.; Grimm, R.; Smith, D.H.; Sun, W. Coadministered Amlodipine and Atorvastatin Produces Early Improvements in Arterial Wall Compliance in Hypertensive Patients With Dyslipidemia. Am. J. Hypertens. 2009, 22, 137–144. [Google Scholar] [CrossRef] [Green Version]
- Tonelli, M.; Isles, C.; Craven, T.; Tonkin, A.; Pfeffer, M.A.; Shepherd, J.; Sacks, F.M.; Furberg, C.; Cobbe, S.M.; Simes, J.; et al. Effect of Pravastatin on Rate of Kidney Function Loss in People With or at Risk for Coronary Disease. Circulation 2005, 112, 171–178. [Google Scholar] [CrossRef] [Green Version]
- Athyros, V.G.; Mikhailidis, D.P.; Papageorgiou, A.A.; Symeonidis, A.N.; Pehlivanidis, A.N.; Bouloukos, V.I.; Elisaf, M. The effect of statins versus untreated dyslipidaemia on renal function in patients with coronary heart disease. A subgroup analysis of the Greek atorvastatin and coronary heart disease evaluation (GREACE) study. J. Clin. Pathol. 2004, 57, 728–734. [Google Scholar] [CrossRef] [Green Version]
- Shepherd, J.; Kastelein, J.J.; Bittner, V.A.; Deedwania, P.; Breazna, A.; Dobson, S.; Wilson, D.J.; Zuckerman, A.; Wenger, N.K.; For the Treating to New Targets Investigators. Effect of Intensive Lipid Lowering with Atorvastatin on Renal Function in Patients with Coronary Heart Disease: The Treating to New Targets (TNT) Study. Clin. J. Am. Soc. Nephrol. 2007, 2, 1131–1139. [Google Scholar] [CrossRef]
- Grundy, S.M.; Stone, N.J.; Bailey, A.L.; Beam, C.; Birtcher, K.K.; Blumenthal, R.S.; Braun, L.T.; de Ferranti, S.; Faiella-Tommasino, J.; Forman, D.E.; et al. 2018 aha/acc/aacvpr/aapa/abc/acpm/ada/ags/apha/aspc/nla/pcna guideline on the management of blood cholesterol: A report of the american college of cardiology/american heart association task force on clinical practice guidelines. J. Am. Coll. Cardiol. 2018. [Google Scholar] [CrossRef]
- Qin, L.; Yang, Y.B.; Yang, Y.X.; Zhu, N.; Li, S.X.; Liao, D.F.; Zheng, X.L. Anti-inflammatory activity of ezetimibe by regulating nf-kappab/mapk pathway in thp-1 macrophages. Pharmacology 2014, 93, 69–75. [Google Scholar] [CrossRef]
- Tie, C.; Gao, K.; Zhang, N.; Zhang, S.; Shen, J.; Xie, X.; Wang, J.-A. Ezetimibe Attenuates Atherosclerosis Associated with Lipid Reduction and Inflammation Inhibition. PLoS ONE 2015, 10, e0142430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, X.-X.; Zhao, L.; Chang, Y.; Liu, B.-S.; Xu, F.; Zhang, C.; Ji, X.-P.; Chen, Y.; Li, C.-B. Ezetimibe prevents myocardial remodeling in an obese rat model by inhibiting inflammation. Acta Biochim. Pol. 2018, 65, 465–470. [Google Scholar] [CrossRef] [PubMed]
- Chang, E.; Kim, L.; Park, S.E.; Rhee, E.-J.; Lee, W.-Y.; Oh, K.-W.; Park, S.-W.; Park, C.-Y. Ezetimibe improves hepatic steatosis in relation to autophagy in obese and diabetic rats. World J. Gastroenterol. 2015, 21, 7754–7763. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.H.; Han, D.H.; Nam, K.T.; Park, J.S.; Kim, S.H.; Lee, M.; Kim, G.; Min, B.S.; Cha, B.-S.; Lee, Y.S.; et al. Ezetimibe, an NPC1L1 inhibitor, is a potent Nrf2 activator that protects mice from diet-induced nonalcoholic steatohepatitis. Free Radic. Biol. Med. 2016, 99, 520–532. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Sato, E.; Fujiwara, N.; Kawagoe, Y.; Ueda, Y.; Suzuki, T.; Ueda, S.; Adachi, H.; Okuda, S.; Hirano, T. Ezetimibe decreases serum levels of asymmetric dimethylarginine (ADMA) and ameliorates renal injury in non-diabetic chronic kidney disease patients in a cholesterol-independent manner. Pharmacol. Res. 2009, 60, 525–528. [Google Scholar] [CrossRef] [PubMed]
- Sureshbabu, A.; Ryter, S.W.; Choi, M.E. Oxidative stress and autophagy: Crucial modulators of kidney injury. Redox Biol. 2015, 4, 208–214. [Google Scholar] [CrossRef] [Green Version]
- Liu, S.; Hartleben, B.; Kretz, O.; Wiech, T.; Igarashi, P.; Mizushima, N.; Walz, G.; Huber, T.B. Autophagy plays a critical role in kidney tubule maintenance, aging and ischemia-reperfusion injury. Autophagy 2012, 8, 826–837. [Google Scholar] [CrossRef] [Green Version]
- Mihai, S.; Codrici, E.; Popescu, I.D.; Enciu, A.-M.; Albulescu, L.; Necula, L.G.; Mambet, C.; Anton, G.; Tanase, C. Inflammation-Related Mechanisms in Chronic Kidney Disease Prediction, Progression, and Outcome. J. Immunol. Res. 2018, 2018, 2180373. [Google Scholar] [CrossRef]
- Vilaysane, A.; Chun, J.; Seamone, M.E.; Wang, W.; Chin, R.; Hirota, S.; Li, Y.; Clark, S.A.; Tschopp, J.; Trpkov, K.; et al. The NLRP3 inflammasome promotes renal inflammation and contributes to CKD. J. Am. Soc. Nephrol. 2010, 21, 1732–1744. [Google Scholar] [CrossRef] [Green Version]
- Knauf, F.; Asplin, J.R.; Granja, I.; Schmidt, I.M.; Moeckel, G.W.; David, R.J.; Flavell, R.A.; Aronson, P.S. NALP3-mediated inflammation is a principal cause of progressive renal failure in oxalate nephropathy. Kidney Int. 2013, 84, 895–901. [Google Scholar] [CrossRef] [Green Version]
- Iyer, S.S.; Pulskens, W.P.; Sadler, J.J.; Butter, L.M.; Teske, G.J.; Ulland, T.; Eisenbarth, S.C.; Florquin, S.; Flavell, R.A.; Leemans, J.C.; et al. Necrotic cells trigger a sterile inflammatory response through the Nlrp3 inflammasome. Proc. Natl. Acad. Sci. USA 2009, 106, 20388–20393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Levey, A.S.; Cattran, D.; Friedman, A.; Miller, W.G.; Sedor, J.; Tuttle, K.; Kasiske, B.; Hostetter, T. Proteinuria as a Surrogate Outcome in CKD: Report of a Scientific Workshop Sponsored by the National Kidney Foundation and the US Food and Drug Administration. Am. J. Kidney Dis. 2009, 54, 205–226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Messerli, F.H.; Staessen, J.A.; Zannad, F. Of fads, fashion, surrogate endpoints and dual RAS blockade. Eur. Heart J. 2010, 31, 2205–2208. [Google Scholar] [CrossRef] [PubMed]
- Cannon, C.P.; Blazing, M.A.; Giugliano, R.P.; McCagg, A.; White, J.A.; Théroux, P.; Darius, H.; Lewis, B.S.; Ophuis, T.O.; Jukema, J.W.; et al. Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes. N. Engl. J. Med. 2015, 372, 2387–2397. [Google Scholar] [CrossRef] [Green Version]
| S + E (N = 1552) | S (N = 1552) | P-Value | |
|---|---|---|---|
| Age, years | 68.3 ± 10.1 | 68.8 ± 11.0 | 0.185 |
| Men, n (%) | 766 (49.4) | 797 (51.4) | 0.266 |
| BMI, kg/m2 | 24.5 ± 3.0 | 24.5 ± 3.2 | 0.654 |
| Current smoker, n (%) | 240 (15.5) | 217 (14.0) | 0.244 |
| Obesity, n (%) 1 | 605 (39.0) | 617 (39.8) | 0.659 |
| HTN, n (%) | 758 (48.8) | 755 (48.6) | 0.914 |
| DM, n (%) | 388 (25.0) | 357 (23.0) | 0.193 |
| CKD stage 1, n (%) 2 | 497 (32.0) | 526 (33.9) | 0.268 |
| CKD stage 2, n (%) 3 | 469 (30.2) | 439 (28.3) | 0.237 |
| CKD stage 3, n (%) 4 | 547 (35.2) | 548 (35.3) | 0.970 |
| CKD stage 4, n (%) 5 | 39 (2.5) | 39 (2.5) | >0.999 |
| History of UA, n (%) | 94 (6.1) | 81 (5.2) | 0.312 |
| History of MI, n (%) | 53 (3.4) | 54 (3.5) | 0.922 |
| History of Stroke, n (%) | 133 (8.6) | 119 (7.7) | 0.358 |
| Medication of aspirin, n (%) | 994 (64.0) | 970 (62.5) | 0.372 |
| Medication of β-blocker, n (%) | 641 (41.3) | 640 (41.2) | 0.971 |
| Medication of CCB, n (%) | 670 (43.2) | 683 (44.0) | 0.638 |
| Medication of ACEi/ARB, n (%) | 724 (46.6) | 737 (47.5) | 0.640 |
| Proteinuria, n (%) 6,7 | 44 (7.1) | 59 (8.4) | 0.355 |
| Albumin to creatinine ratio (mg/g) | 159.9 ± 493.1 | 238.7 ± 754.2 | 0.315 |
| Total cholesterol, mg/dL | 187.4 ± 50.1 | 188.9 ± 50.8 | 0.406 |
| LDL-C, mg/dL | 107.9 ± 43.2 | 109.5 ± 41.6 | 0.288 |
| HDL-C, mg/dL | 49.0 ± 12.8 | 49.4 ± 12.2 | 0.341 |
| Triglyceride, mg/dL | 145.5 ± 101.0 | 143.8 ± 86.4 | 0.620 |
| Uric acid, mg/dL 8 | 5.2 ± 1.4 | 5.1 ± 1.4 | 0.103 |
| CRP, mg/L 9 | 5.1 ± 16.9 | 5.9 ± 17.6 | 0.418 |
| Fasting glucose, mg/dL | 108.9 ± 30.7 | 107.8 ± 30.6 | 0.300 |
| HbA1c, % 10 | 7.1 ± 1.6 | 7.0 ± 1.4 | 0.437 |
| Creatinine, mg/dL | 1.0 ± 0.3 | 1.0 ± 0.3 | 0.661 |
| eGFR, mL/min per 1.73 m2 11 | 76.6 ± 31.5 | 76.7 ± 30.9 | 0.953 |
| Renal Events | |||||
|---|---|---|---|---|---|
| Events/Total, n | HR | 95% CI | P-Value | ||
| S + E | S | ||||
| Overall | 22/1552 | 62/1552 | 0.58 | 0.35–0.95 | 0.032 |
| Age, years | * 0.310 | ||||
| <60 | 5/293 | 8/297 | 1.14 | 0.23–5.79 | 0.868 |
| ≥60 | 17/1259 | 54/1255 | 0.52 | 0.30–0.91 | 0.021 |
| Sex | * 0.603 | ||||
| Male | 13/766 | 36/797 | 0.60 | 0.31–1.15 | 0.125 |
| Female | 9/786 | 26/755 | 0.53 | 0.24–1.13 | 0.100 |
| BMI | * 0.326 | ||||
| <25 | 12/947 | 40/935 | 0.46 | 0.24–0.89 | 0.021 |
| ≥25 | 10/605 | 22/617 | 0.69 | 0.32–1.51 | 0.356 |
| CKD | * 0.073 | ||||
| Stage 1/2 | 5/966 | 29/965 | 0.27 | 0.10–0.70 | 0.007 |
| Stage 3/4 | 17/586 | 33/587 | 0.89 | 0.48–1.66 | 0.713 |
| HTN | * 0.374 | ||||
| No | 6/794 | 25/797 | 0.40 | 0.16–0.99 | 0.048 |
| Yes | 16/758 | 37/755 | 0.71 | 0.39–1.29 | 0.254 |
| DM | * 0.175 | ||||
| No | 9/1164 | 36/1195 | 0.44 | 0.21–0.92 | 0.029 |
| Yes | 13/388 | 26/357 | 0.73 | 0.37–1.46 | 0.372 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bae, J.; Hong, N.; Lee, B.-W.; Kang, E.S.; Cha, B.-S.; Lee, Y.-h. Comparison of Renal Effects of Ezetimibe–Statin Combination versus Statin Monotherapy: A Propensity-Score-Matched Analysis. J. Clin. Med. 2020, 9, 798. https://doi.org/10.3390/jcm9030798
Bae J, Hong N, Lee B-W, Kang ES, Cha B-S, Lee Y-h. Comparison of Renal Effects of Ezetimibe–Statin Combination versus Statin Monotherapy: A Propensity-Score-Matched Analysis. Journal of Clinical Medicine. 2020; 9(3):798. https://doi.org/10.3390/jcm9030798
Chicago/Turabian StyleBae, Jaehyun, Namki Hong, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, and Yong-ho Lee. 2020. "Comparison of Renal Effects of Ezetimibe–Statin Combination versus Statin Monotherapy: A Propensity-Score-Matched Analysis" Journal of Clinical Medicine 9, no. 3: 798. https://doi.org/10.3390/jcm9030798
APA StyleBae, J., Hong, N., Lee, B.-W., Kang, E. S., Cha, B.-S., & Lee, Y.-h. (2020). Comparison of Renal Effects of Ezetimibe–Statin Combination versus Statin Monotherapy: A Propensity-Score-Matched Analysis. Journal of Clinical Medicine, 9(3), 798. https://doi.org/10.3390/jcm9030798





