Disorders of Puberty: Endocrinology of the Pre-Pubertal Testis
Abstract
Author Contributions
Funding
Conflicts of Interest
References
- Cannarella, R.; Arato, I.; Condorelli, R.A.; Luca, G.; Barbagallo, F.; Alamo, A.; Bellucci, C.; Lilli, C.; La Vignera, S.; Calafiore, R.; et al. The IGF1 Receptor Is Involved in Follicle-Stimulating Hormone Signaling in Porcine Neonatal Sertoli Cells. J. Clin. Med. 2019, 8, 577. [Google Scholar] [CrossRef] [PubMed]
- Cannarella, R.; Mancuso, F.; Condorelli, R.A.; Arato, I.; Mongioì, L.M.; Giacone, F.; Lilli, C.; Bellucci, C.; La Vignera, S.; Calafiore, R.; et al. Effects of GH and IGF1 on Basal and FSH-Modulated Porcine Sertoli Cells In Vitro. J. Clin. Med. 2019, 8, 811. [Google Scholar] [CrossRef] [PubMed]
- Cannarella, R.; Arato, I.; Condorelli, R.A.; Mongioì, L.M.; Lilli, C.; Bellucci, C.; La Vignera, S.; Luca, G.; Mancuso, F.; Calogero, A.E. Effects of Insulin on Porcine Neonatal Sertoli Cell Responsiveness to FSH In Vitro. J. Clin. Med. 2019, 8, 809. [Google Scholar] [CrossRef] [PubMed]
- Duca, Y.; Di Cataldo, A.; Russo, G.; Cannata, E.; Burgio, G.; Compagnone, M.; Alamo, A.; Condorelli, R.A.; La Vignera, S.; Calogero, A.E. Testicular Function of Childhood Cancer Survivors: Who Is Worse? J. Clin. Med. 2019, 8, 2204. [Google Scholar] [CrossRef] [PubMed]
- Cannarella, R.; Calogero, A.E.; Condorelli, R.A.; Giacone, F.; Aversa, A.; La Vignera, S. Management and Treatment of Varicocele in Children and Adolescents: An Endocrinologic Perspective. J. Clin. Med. 2019, 8, 1410. [Google Scholar] [CrossRef] [PubMed]
- Perri, A.; Lofaro, D.; Izzo, G.; Aquino, B.; Bitonti, M.; Ciambrone, G.; La Vignera, S.; Pozza, C.; Gianfrilli, D.; Aversa, A. The Risky Health Behaviours of Male Adolescents in the Southern Italian Region: Implications for Sexual and Reproductive Disease. J. Clin. Med. 2019, 8, 1414. [Google Scholar] [CrossRef] [PubMed]
- Duca, Y.; Aversa, A.; Condorelli, R.A.; Calogero, A.E.; La Vignera, S. Substance Abuse and Male Hypogonadism. J. Clin. Med. 2019, 8, 732. [Google Scholar] [CrossRef] [PubMed]
- Condorelli, R.A.; Calogero, A.E.; Cannarella, R.; Giacone, F.; Mongioi’, L.M.; Cimino, L.; Aversa, A.; La Vignera, S. Poor Efficacy of L-Acetylcarnitine in the Treatment of Asthenozoospermia in Patients with Type 1 Diabetes. J. Clin. Med. 2019, 8, 585. [Google Scholar] [CrossRef] [PubMed]
- Condorelli, R.A.; La Vignera, S.; Mongioì, L.M.; Alamo, A.; Giacone, F.; Cannarella, R.; Calogero, A.E. Thyroid Hormones and Spermatozoa: In VitroEffects on Sperm Mitochondria, Viability and DNA Integrity. J. Clin. Med. 2019, 8, 756. [Google Scholar] [CrossRef] [PubMed]
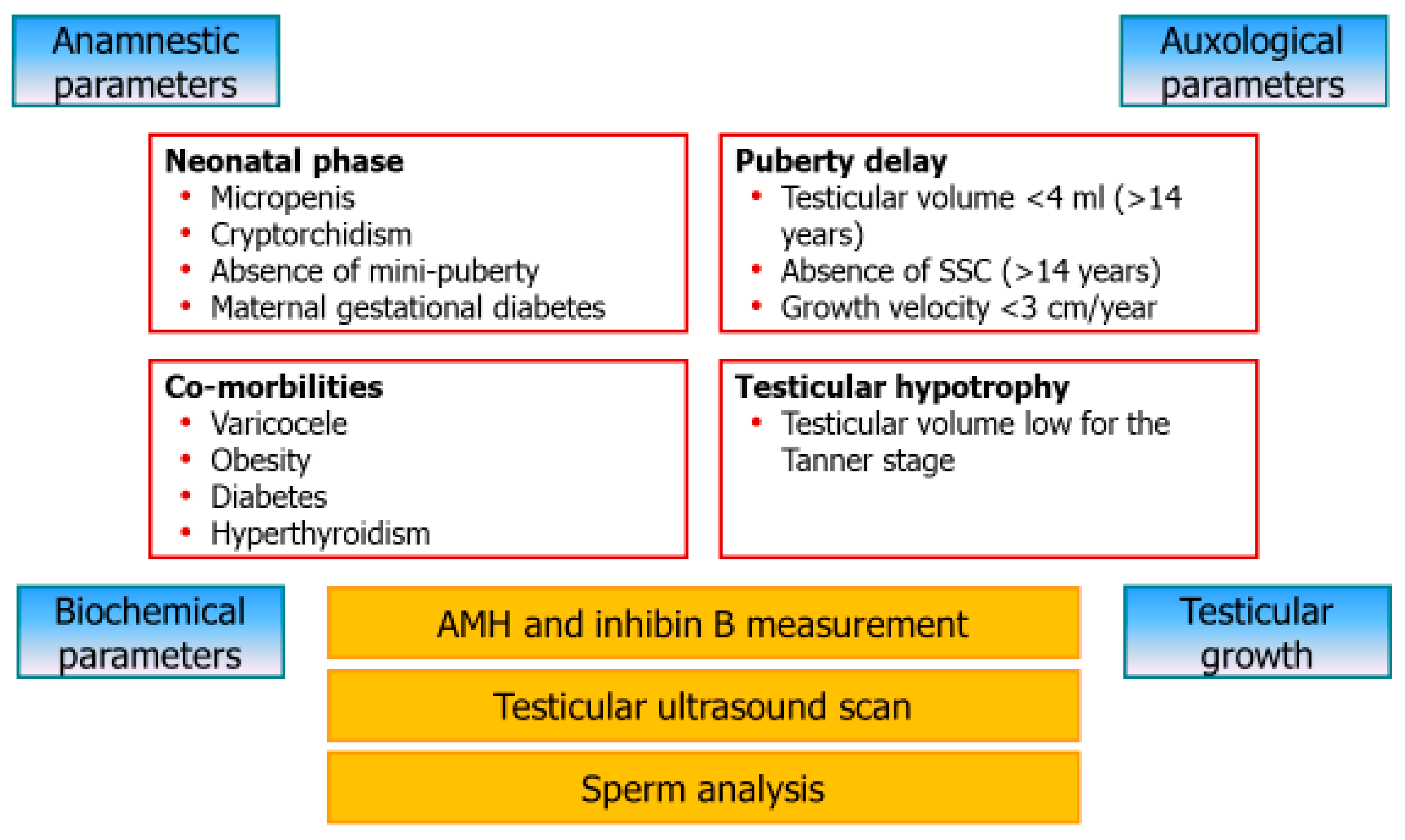
- La Vignera, S.; Condorelli, R.A.; Cimino, L.; Cannarella, R.; Giacone, F.; Calogero, A.E. Early Identification of Isolated Sertoli Cell Dysfunction in Prepubertal and Transition Age: Is It Time? J. Clin. Med. 2019, 8, 636. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
La Vignera, S.; Cannarella, R.; Condorelli, R.A.; Calogero, A.E. Disorders of Puberty: Endocrinology of the Pre-Pubertal Testis. J. Clin. Med. 2020, 9, 780. https://doi.org/10.3390/jcm9030780
La Vignera S, Cannarella R, Condorelli RA, Calogero AE. Disorders of Puberty: Endocrinology of the Pre-Pubertal Testis. Journal of Clinical Medicine. 2020; 9(3):780. https://doi.org/10.3390/jcm9030780
Chicago/Turabian StyleLa Vignera, Sandro, Rossella Cannarella, Rosita A. Condorelli, and Aldo E. Calogero. 2020. "Disorders of Puberty: Endocrinology of the Pre-Pubertal Testis" Journal of Clinical Medicine 9, no. 3: 780. https://doi.org/10.3390/jcm9030780
APA StyleLa Vignera, S., Cannarella, R., Condorelli, R. A., & Calogero, A. E. (2020). Disorders of Puberty: Endocrinology of the Pre-Pubertal Testis. Journal of Clinical Medicine, 9(3), 780. https://doi.org/10.3390/jcm9030780







