High Levels of Kinesiophobia at Discharge from the Hospital May Negatively Affect the Short-Term Functional Outcome of Patients Who Have Undergone Knee Replacement Surgery
Abstract
1. Introduction
2. Experimental Section
2.1. Subjects
2.2. Experimental Procedure
2.2.1. Data Collection
2.2.2. Patient-Reported Outcome Measures
2.2.3. Performance-Based Measures
2.3. Statistical Analysis
3. Results
3.1. Independent Sample t-Test on PROMs and PBMs
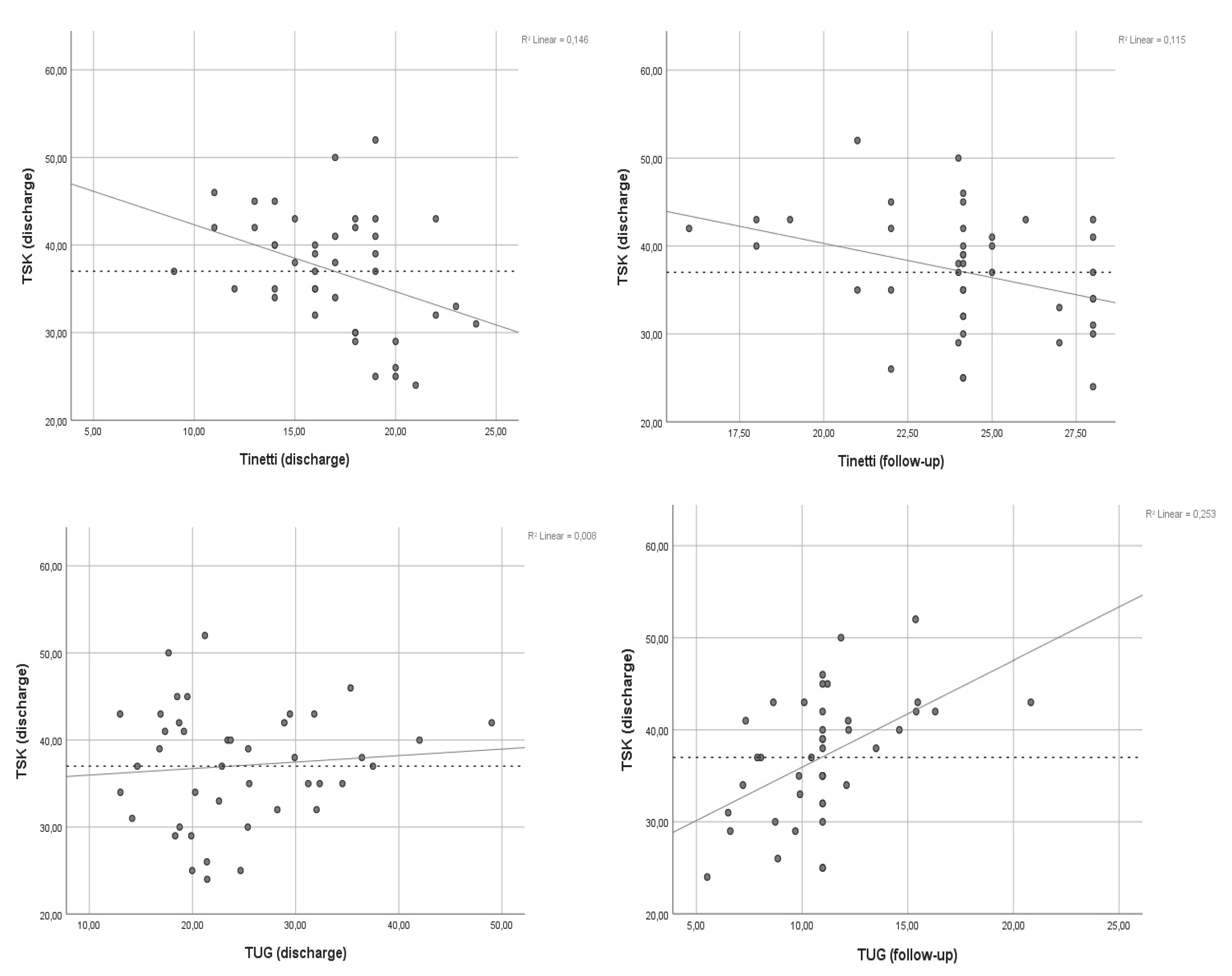
3.2. Bivariate Analyses and Multiple Linear Regressions
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Ethgen, O.; Bruyere, O.; Richy, F.; Dardennes, C.; Reginster, J.Y. Health-related quality of life in total hip and total knee arthroplasty. A qualitative and systematic review of the literature. J. Bone Joint Surg. Am. 2004, 86, 963–974. [Google Scholar] [CrossRef] [PubMed]
- Von Keudell, A.; Sodha, S.; Collins, J.; Minas, T.; Fitz, W.; Gomoll, A.H. Patient satisfaction after primary total and unicompartmental knee arthroplasty: An age-dependent analysis. Knee 2014, 21, 180–184. [Google Scholar] [CrossRef]
- Nüesch, E.; Reichenbach, S.; Iff, S.; Jüni, P.; Dieppe, P.; Williams, S. All cause and disease specific mortality in patients with knee or hip osteoarthritis: Population based cohort study. BMJ 2011, 342, 638. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, W.R.; White, R.P. Unicompartmental arthroplasty of the knee. Postoperative alignment and its influence on overall results. Clin. Orthop. Relat. Res. 1987, 221, 278. [Google Scholar]
- Bourne, R.; Chesworth, B.; Davis, A.; Mahomed, N.; Charron, K. Patient Satisfaction after Total Knee Arthroplasty: Who is Satisfied and Who is Not? Clin. Orthop. Relat. Res. 2010, 468, 57–63. [Google Scholar] [CrossRef] [PubMed]
- Baert, I.A.C.; Meeus, M.; Mahmoudian, A.; Luyten, F.P.; Nijs, J.; Verschueren, S.M.P. Do Psychosocial Factors Predict Muscle Strength, Pain, or Physical Performance in Patients with Knee Osteoarthritis? J. Clin. Rheumatol. 2017, 23, 308–316. [Google Scholar] [CrossRef] [PubMed]
- Lentz, T.A.; Zeppieri, G.; George, S.Z.; Tillman, S.M.; Moser, M.W.; Farmer, K.W.; Chmielewski, T.L. Comparison of Physical Impairment, Functional, and Psychosocial Measures Based on Fear of Reinjury/Lack of Confidence and Return-to-Sport Status After ACL Reconstruction. Am. J. Sports Med. 2015, 43, 345–353. [Google Scholar] [CrossRef]
- Güney-Deniz, H.; Irem Kınıklı, G.; Çağlar, Ö.; Atilla, B.; Yüksel, I. Does kinesiophobia affect the early functional outcomes following total knee arthroplasty? Physiother. Theory Pract. 2017, 33, 448–453. [Google Scholar] [CrossRef]
- Domenech, J.; Sanchis-Alfonso, V.; López, L.; Espejo, B. Influence of kinesiophobia and catastrophizing on pain and disability in anterior knee pain patients. Knee Surg. Sports Traumatol. Arthrosc. 2013, 21, 1562–1568. [Google Scholar] [CrossRef]
- Leeuw, M.; Goossens, M.E.J.B.; Linton, S.J.; Crombez, G.; Boersma, K.; Vlaeyen, J.W.S. The Fear-Avoidance Model of Musculoskeletal Pain: Current State of Scientific Evidence; Springer: Berlin/Heidelberg, Germany, 2007; Volume 30, pp. 77–94. [Google Scholar]
- Karos, K.; Meulders, A.; Gatzounis, R.; Seelen, H.A.M.; Geers, R.P.G.; Vlaeyen, J.W.S. Fear of pain changes movement: Motor behaviour following the acquisition of pain-related fear. Eur. J. Pain 2017, 21, 1432–1442. [Google Scholar] [CrossRef]
- Malinen, s.; Vartiainena, N.; Hlushchuk, Y.; Koskinen, M.; Ramkumar, P.; Forss, N.; Kalso, E.; Hari, R. Aberrant temporal and spatial brain activity during rest in patients with chronic pain. Proc. Natl. Acad. Sci. USA 2010, 107, 6493–6497. [Google Scholar] [CrossRef]
- Apkarian, A.V.; Hashmi, J.A.; Baliki, M.N. Pain and the brain: Specificity and plasticity of the brain in clinical chronic pain. Pain 2011, 152, S49–S64. [Google Scholar] [CrossRef] [PubMed]
- Kocic, M.; Stankovic, A.; Lazovic, M.; Dimitrijevic, L.; Stankovic, I.; Spalevic, M.; Stojiljkovic, P.; Milenkovic, M.; Stojanovic, Z.; Nikolic, D. Influence of fear of movement on total knee arthroplasty outcome. Ann. Ital. Chir. 2015, 86, 148–155. [Google Scholar] [PubMed]
- Roelofs, J.; Sluiter, J.; Frings-Dresen, M.; Goossens, M.; Thibault, P.; Boersma, K.; Vlaeyen, J.W. Fear of Movement and (re)Injury in Chronic Musculoskeletal Pain: Evidence for an Invariant Two-Factor Model of the Tampa Scale for Kinesiophobia Across Pain Diagnoses and Dutch, Swedish, and Canadian Samples; Elsevier: Amsterdam, The Netherlands, 2007; Volume 131, pp. 181–190. [Google Scholar]
- Miller, R.P.; Kori, S.H.; Todd, D.D. The Tampa Scale: A Measure of Kinisophobia. Clin. J. Pain 1991, 7, 51. [Google Scholar] [CrossRef]
- Priore, L.B.; Azevedo, F.M.; Pazzinatto, M.F.; Ferreira, A.S.; Hart, H.F.; Barton, C.; de Oliveira Silva, D. Influence of kinesiophobia and pain catastrophism on objective function in women with patellofemoral pain. Phys. Ther. Sport 2019, 35, 116–121. [Google Scholar] [CrossRef]
- Palomo-López, P.; Becerro-de-Bengoa-Vallejo, R.; Losa-Iglesias, M.E.; López-López, D.; Rodríguez-Sanz, D.; Romero-Morales, C.; Calvo-Lobo, C.; Mazoteras-Pardo, V. Kinesiophobia and Pain Intensity Are Increased by a Greater Hallux Valgus Deformity Degree-Kinesiophobia and Pain Intensity in Hallux Valgus. Int. J. Environ. Res. Public Health 2020, 17, 626. [Google Scholar] [CrossRef]
- Cai, L.; Liu, Y.; Xu, H.; Xu, Q.; Wang, Y.; Lyu, P. Incidence and Risk Factors of Kinesiophobia After Total Knee Arthroplasty in Zhengzhou, China: A Cross-Sectional Study. J. Arthroplast. 2018, 33, 2858–2862. [Google Scholar] [CrossRef]
- Matsumoto, H.; Okuno, M.; Nakamura, T.; Yamamoto, K.; Hagino, H. Fall incidence and risk factors in patients after total knee arthroplasty. Arch. Orthop. Trauma. Surg. 2012, 132, 555–563. [Google Scholar] [CrossRef]
- Filardo, G.; Merli, G.; Roffi, A.; Marcacci, T.; Berti Ceroni, F.; Raboni, D.; Bortolotti, B.; Kon, E.; Marcacci, M. Kinesiophobia and depression affect total knee arthroplasty outcome in a multivariate analysis of psychological and physical factors on 200 patients. Knee Surg. Sports Traumatol. Arthrosc. 2017, 25, 3417–3423. [Google Scholar] [CrossRef]
- San-Antolín, M.; Rodríguez-Sanz, D.; Vicente-Campos, D.; Palomo-López, P.; Romero-Morales, C.; Benito-de-Pedro, M.; López-López, D.; Calvo-Lobo, C. Fear Avoidance Beliefs and Kinesiophobia Are Presented in Athletes who Suffer from Gastrocnemius Chronic Myofascial Pain. Pain Med. 2020, 87, 1999–2005. [Google Scholar] [CrossRef]
- Sculco, T.P.; Marx, R.G.; Jones, E.C.; Atwan, N.C.; Closkey, R.F.; Salvati, E.A. Measuring improvement following total hip and knee arthroplasty using patient-based measures of outcome. J. Bone Joint Surg. 2005, 87, 1999. [Google Scholar]
- Bean, J.F.; Olveczky, D.D.; Kiely, D.K.; Larose, S.I.; Jette, A.M. Performance- based versus patient- reported physical function: What are the underlying predictors? Phys. Ther. 2011, 91, 1804. [Google Scholar] [CrossRef] [PubMed]
- Beauchamp, M.K.; Jette, A.M.; Ward, R.E.; Kurlinski, L.A.; Kiely, D.; Latham, N.K.; Bean, J.F. Predictive validity and responsiveness of patient-reported and performance-based measures of function in the Boston RISE study. (Research Article)(Clinical report)(Author abstract). J. Gerontol. Ser. A Biomed. Sci. Med Sci. 2015, 70, 616. [Google Scholar] [CrossRef]
- Tinetti, M.E.; Franklin Williams, T.; Mayewski, R. Fall risk index for elderly patients based on number of chronic disabilities. Am. J. Med. 1986, 80, 429–434. [Google Scholar] [CrossRef]
- Barry, E.; Galvin, R.; Keogh, C.; Horgan, F.; Fahey, T. Is the Timed Up and Go test a useful predictor of risk of falls in community dwelling older adults: A systematic review and meta- analysis. BMC Geriatr. 2014, 14, 14. [Google Scholar] [CrossRef] [PubMed]
- Browne, W.; Nair, B.R. The Timed Up and Go test. Med. J. Aust. 2019, 210, 13–14. [Google Scholar] [CrossRef] [PubMed]
- Garber, C.E.; Riebe, D.; Greaney, M.; Burbank, P.; Lees, F.; Clark, P.G. Does The Timed Up And Go Test Reflect Physical Activity And Function In Community Dwelling Older Adults? Results SENIOR Proj. Med. Sci. Sports Exerc. 2005, 37, S257. [Google Scholar]
- Roelofs, J.; van Breukelen, G.; Sluiter, J.; Frings-Dresen, M.H.W.; Goossens, M.; Thibault, P.; Boersma, K.; Vlaeyen, J.W. Norming of the Tampa Scale for Kinesiophobia across pain diagnoses and various countries. Pain 2011, 152, 1090–1095. [Google Scholar] [CrossRef]
- Velthuis, M.J.; Van den Bussche, E.; May, A.M.; Gijsen, B.C.M.; Nijs, S.; Vlaeyen, J.W.S. Fear of Movement in Cancer Survivors: Validation of the Modified Tampa Scale of Kinesiophobia-Fatigue; Wiley: Hoboken, NJ, USA, 2012; Volume 21, pp. 762–770. [Google Scholar]
- Roos, E.M.; Roos, H.P.; Lohmander, L.S.; Ekdahl, C.; Beynnon, B.D. Knee Injury and Osteoarthritis Outcome Score (KOOS)-development of a self-administered outcome measure. J. Orthop. Sports Phys. Ther. 1998, 28, 88. [Google Scholar] [CrossRef]
- Gandek, B.; Ware, J.E., Jr. Validity and Responsiveness of the Knee Injury and Osteoarthritis Outcome Score: A Comparative Study among Total Knee Replacement Patients. Arthritis Care Res. 2017, 69, 817–825. [Google Scholar] [CrossRef]
- Haverkamp, D.; Breugem, S.; Sierevelt, I.; Blankevoort, L.; van Dijk, C. Translation and validation of the Dutch version of the Oxford 12-item knee questionnaire for knee arthroplasty. Acta Orthop. 2005, 76, 347–352. [Google Scholar] [CrossRef] [PubMed]
- Panella, L.; Tinelli, C.; Buizza, A.; Lombardi, R.; Gandolfi, R. Towards objective evaluation of balance in the elderly: Validity and reliability of a measurement instrument applied to the Tinetti test. Int. J. Rehabil. Res. 2008, 31, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Mesquita, R.; Wilke, S.; Smid, D.E.; Janssen, D.J.; Franssen, F.M.E.; Probst, V.S.; Wouters, E.F.; Muris, J.W.; Pitta, F.; Spruit, M.A. Measurement properties of the Timed Up & Go test in patients with COPD. Chronic Respir. Dis. 2016, 13, 344–352. [Google Scholar]
- Vlaeyen, J.W.S.; Crombez, G.; Linton, S.J. The fear- avoidance model of pain. Pain 2016, 157, 1588. [Google Scholar] [CrossRef]
- Crombez, G.; Vlaeyen, J.W.S.; Heuts, P.; Lysens, R. Pain-related fear is more disabling than pain itself: Evidence on the role of pain-related fear in chronic back pain disability. Pain 1999, 80, 329–339. [Google Scholar] [CrossRef]
- Crombez, G.; Eccleston, C.; Van Damme, S.; Vlaeyen, J.W.S.; Karoly, P. Fear-Avoidance Model of Chronic Pain The Next Generation. Pain 2012, 28, 475–483. [Google Scholar]
- Michael Lukas, M.; Philipp, S.; Barry Kim, H.; Andrea, V.; Erich, S.; Petra, S. The impact of pain-related fear on neural pathways of pain modulation in chronic low back pain. PAIN Rep. 2017, 2, e601. [Google Scholar]
- Barke, A.; Preis, M.A.; Schmidt-Samoa, C.; Baudewig, J.; Kröner-Herwig, B.; Dechent, P. Neural Correlates Differ in High and Low Fear-Avoidant Chronic Low Back Pain Patients When Imagining Back-Straining Movements. J. Pain 2016, 17, 930–943. [Google Scholar] [CrossRef]
- Skou, T.S.; Graven-Nielsen, H.T.; Rasmussen, B.S.; Simonsen, B.O.; Laursen, B.M.; Arendt-Nielsen, B.L. Widespread sensitization in patients with chronic pain after revision total knee arthroplasty. Pain 2013, 154, 1588–1594. [Google Scholar] [CrossRef]
- Wylde, D.V.; Hewlett, D.S.; Learmonth, D.I.; Dieppe, D.P. Persistent pain after joint replacement: Prevalence, sensory qualities, and postoperative determinants. Pain 2011, 152, 566–572. [Google Scholar] [CrossRef]
- Noiseux, N.O.; Callaghan, J.J.; Clark, C.R.; Zimmerman, M.B.; Sluka, K.A.; Rakel, B.A. Preoperative Predictors of Pain Following Total Knee Arthroplasty. J. Arthroplast. 2014, 29, 1383–1387. [Google Scholar] [CrossRef] [PubMed]
- Riddle, D.; Wade, J.; Jiranek, W.; Kong, X. Preoperative Pain Catastrophizing Predicts Pain Outcome after Knee Arthroplasty. Clin. Orthop. Relat. Res. 2010, 468, 798–806. [Google Scholar] [CrossRef] [PubMed]
- Hsieh, C.J.; Dominguez, J.; Moser, M.; Indelicato, P.A.; Cicuttini, F.; George, S.; Chmielewski, T.L. Gait Asymmetry after Meniscal Tear Is Associated with Knee Pain Intensity and Fear of Movement/Re-Injury. Osteoarthr. Cartil. 2011, 19, S90–S91. [Google Scholar] [CrossRef][Green Version]
- Heuts, P.H.T.G.; Vlaeyen, J.; Roelofs, J.; de Bie, R.A.; Aretz, K.; van Weel, C.; van Schayck, O.C. Pain-related fear and daily functioning in patients with osteoarthritis. Pain 2004, 110, 228–235. [Google Scholar] [CrossRef]
- Milenković, M.; Kocić, M.; Balov, B.; Stojanović, Z.; Savić, N.; Ivanović, S. Influence of kinesiophobia on activities of daily living of elder institutionalized persons with chronic pain. Prax. Med. 2015, 44, 55–59. [Google Scholar] [CrossRef]
- Hairi, N.N.; Cumming, R.G.; Naganathan, V.; Handelsman, D.J.; Le Couteur, D.G.; Creasey, H.; Waite, L.M.; Seibel, M.J.; Sambrook, P.N. Loss of Muscle Strength, Mass (Sarcopenia), and Quality (Specific Force) and Its Relationship with Functional Limitation and Physical Disability: The Concord Health and Ageing in Men Project. J. Am. Geriatr. Soc. 2010, 58, 2055–2062. [Google Scholar] [CrossRef]
- Cai, L.; Gao, H.; Xu, H.; Wang, Y.; Lyu, P.; Liu, Y. Does a Program Based on Cognitive Behavioral Therapy Affect Kinesiophobia in Patients Following Total Knee Arthroplasty? A Randomized, Controlled Trial with a 6-Month Follow-Up. J. Arthroplast. 2018, 33, 704–710. [Google Scholar] [CrossRef]
- Meulders, W.S.A.; Vlaeyen, W.S.J. Reduction of fear of movement- related pain and pain-related anxiety: An associative learning approach using a voluntary movement paradigm. Pain 2012, 153, 1504–1513. [Google Scholar] [CrossRef]
- Priore, L.B.; Lack, S.; Garcia, C.; Azevedo, F.M.; de Oliveira Silva, D. Two Weeks of Wearing a Knee Brace Compared with Minimal Intervention on Kinesiophobia at 2 and 6 Weeks in People with Patellofemoral Pain: A Randomized Controlled Trial. Arch. Phys. Med. Rehabil. 2019, in press. [Google Scholar] [CrossRef]
- Mogensen, L.; Arendt-Nielsen, L.; Pascal, M. Intensive, personalized multimodal rehabilitation in patients with primary or revision total knee arthroplasty: A retrospective cohort study. BMC Sports Sci. Med. Rehabil. 2020, 12, 1–8. [Google Scholar]
- Van Onsem, S.; Van Der Straeten, C.; Arnout, N.; Deprez, P.; Van Damme, G.; Victor, J. A New Prediction Model for Patient Satisfaction after Total Knee Arthroplasty. J. Arthroplast. 2016, 31, 2660–2667. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | Mean ± SD |
|---|---|
| Sex | M = 24, F = 19 |
| Age (years) | 65.17 ± 7.33 |
| Weight (kg) | 82.25 ± 13.53 |
| BMI (kg/m²) | 27.61 ± 4.79 |
| Arthroplasty type | UKA = 14, TKA = 29 |
| PROMs KOOS | Discharge (3 days) | p-Value | Follow-Up (6 weeks) | p-Value | ||||
|---|---|---|---|---|---|---|---|---|
| Kinesiophobia (n = 24) | No-kinesiophobia (n = 19) | Mean Difference (95% CI) | Kinesiophobia | No-kinesiophobia | Mean Difference (95% CI) | |||
| Pain (%) | 45.89 ± 6.31 | 57.73 ± 5.51 | 11.84 (−8.00, −5.15) | 0.03 | 66.20 ± 8.81 | 75.33 ± 5.73 | 9.13 (−9.82, 3.06) | 0.29 |
| Symptoms (%) | 57.13 ± 5.41 | 60.11 ± 3.66 | 2.98 (−2.63, 2.19) | 0.85 | 67.00 ± 2.84 | 70.72 ± 3.58 | 3.72 (−4.53, 1.39) | 0.41 |
| ADL (%) | 52.95 ± 11.63 | 61.77 ± 9.99 | 8.82 (−13.61, 0.48) | 0.06 | 78.12 ± 10.67 | 81.62 ± 9.41 | 3.49 (−10.58, 4.94) | 0.57 |
| QOL (%) | 40.25 ± 2.78 | 51.13 ± 3.22 | 1.74 (−2.99, 2.67) | 0.07 | 65.13 ± 3.44 | 66.25 ± 3.32 | 1.12 (−3.70, 0.22) | 0.89 |
| OKS (0–48) | 26.04 ± 8.65 | 30.06 ± 7.07 | 4.01 (−1.04, 9.06) | 0.12 | 36.06 ± 7.61 | 38.00 ± 6.55 | 1.94 (−4.07, 7.96) | 0.51 |
| TSK (17–60) | 41.83 ± 3.95 | 30.89 ± 3.53 | 10.95 (−13.35, −8.69) | 0.01 | 36.37 ± 6.78 | 32.90 ± 6.44 | 3.47 (−9.01, 2.06) | 0.21 |
| VAS (0–10) | 4.46 ± 1.88 | 3.94 ± 1.51 | 0.51 (−1.61, 0.59) | 0.35 | 1.89 ± 1.45 | 2.00 ± 1.09 | 0.11 (−0.93, 1.16) | 0.83 |
| PBMs | ||||||||
| Tinetti (0–28) | 16.08 ± 2.09 | 17.78 ± 2.77 | 1.69 (−0.26, 3.65) | 0.05 | 24.00 ± 6.89 | 25.75 ± 4.41 | 1.75 (−0.10, 5.32) | 0.78 |
| Gait (0–12) | 6.30 ± 2.20 | 7.95 ± 2.10 | 1.56 (0.21, 2.93) | 0.01 | 9.40 ± 2.19 | 10.1 ± 2.56 | 0.66 (−1.28, −2.61) | 0.05 |
| Balance (0–16) | 9.70 ± 1.88 | 9.94 ± 1.95 | 0.23 (−0.97, 1.44) | 0.69 | 14.60 ± 2.21 | 14.03 ± 2.20 | 0.56 (−0.77, 2.88) | 0.82 |
| TUG (s) | 25.04 ± 9.39 | 23.59 ± 6.57 | 1.45 (−5.43, 0.27) | 0.58 | 12.18 ± 3.59 | 9.34 ± 2.03 | 2.84 (−5.92, −1.50) | 0.03 |
| r | r² | Standardized β | p-Value | |
|---|---|---|---|---|
| TUG (discharge) | ||||
| Model | 0.234 | 0.530 | - | 0.54 |
| TSK | 0.483 | 0.004 | ||
| VAS pain | 0.157 | 0.341 | ||
| Age | 0.113 | 0.494 | ||
| TUG (follow-up) | ||||
| Model | 0.653 | 0.427 | - | 0.05 |
| TSK | 0.541 | 0.004 | ||
| VAS pain | 0.202 | 0.241 | ||
| Age | 0.122 | 0.439 | ||
| Tinetti (discharge) | ||||
| Model | 0.464 | 0.215 | - | 0.01 |
| TSK | −0.348 | 0.025 | ||
| VAS pain | −0.242 | 0.175 | ||
| Age | −0.145 | 0.332 | ||
| Tinetti (follow-up) | ||||
| Model | 0.490 | 0.274 | - | 0.04 |
| TSK | −0.349 | 0.066 | ||
| VAS pain | −0.242 | 0.193 | ||
| Age | −0.178 | 0.323 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Vroey, H.; Claeys, K.; Shariatmadar, K.; Weygers, I.; Vereecke, E.; Van Damme, G.; Hallez, H.; Staes, F. High Levels of Kinesiophobia at Discharge from the Hospital May Negatively Affect the Short-Term Functional Outcome of Patients Who Have Undergone Knee Replacement Surgery. J. Clin. Med. 2020, 9, 738. https://doi.org/10.3390/jcm9030738
De Vroey H, Claeys K, Shariatmadar K, Weygers I, Vereecke E, Van Damme G, Hallez H, Staes F. High Levels of Kinesiophobia at Discharge from the Hospital May Negatively Affect the Short-Term Functional Outcome of Patients Who Have Undergone Knee Replacement Surgery. Journal of Clinical Medicine. 2020; 9(3):738. https://doi.org/10.3390/jcm9030738
Chicago/Turabian StyleDe Vroey, Henri, Kurt Claeys, Keivan Shariatmadar, Ive Weygers, Evie Vereecke, Geert Van Damme, Hans Hallez, and Filip Staes. 2020. "High Levels of Kinesiophobia at Discharge from the Hospital May Negatively Affect the Short-Term Functional Outcome of Patients Who Have Undergone Knee Replacement Surgery" Journal of Clinical Medicine 9, no. 3: 738. https://doi.org/10.3390/jcm9030738
APA StyleDe Vroey, H., Claeys, K., Shariatmadar, K., Weygers, I., Vereecke, E., Van Damme, G., Hallez, H., & Staes, F. (2020). High Levels of Kinesiophobia at Discharge from the Hospital May Negatively Affect the Short-Term Functional Outcome of Patients Who Have Undergone Knee Replacement Surgery. Journal of Clinical Medicine, 9(3), 738. https://doi.org/10.3390/jcm9030738






