Predictors of Mental Health Outcomes in Road Traffic Accident Survivors
Abstract
1. Introduction
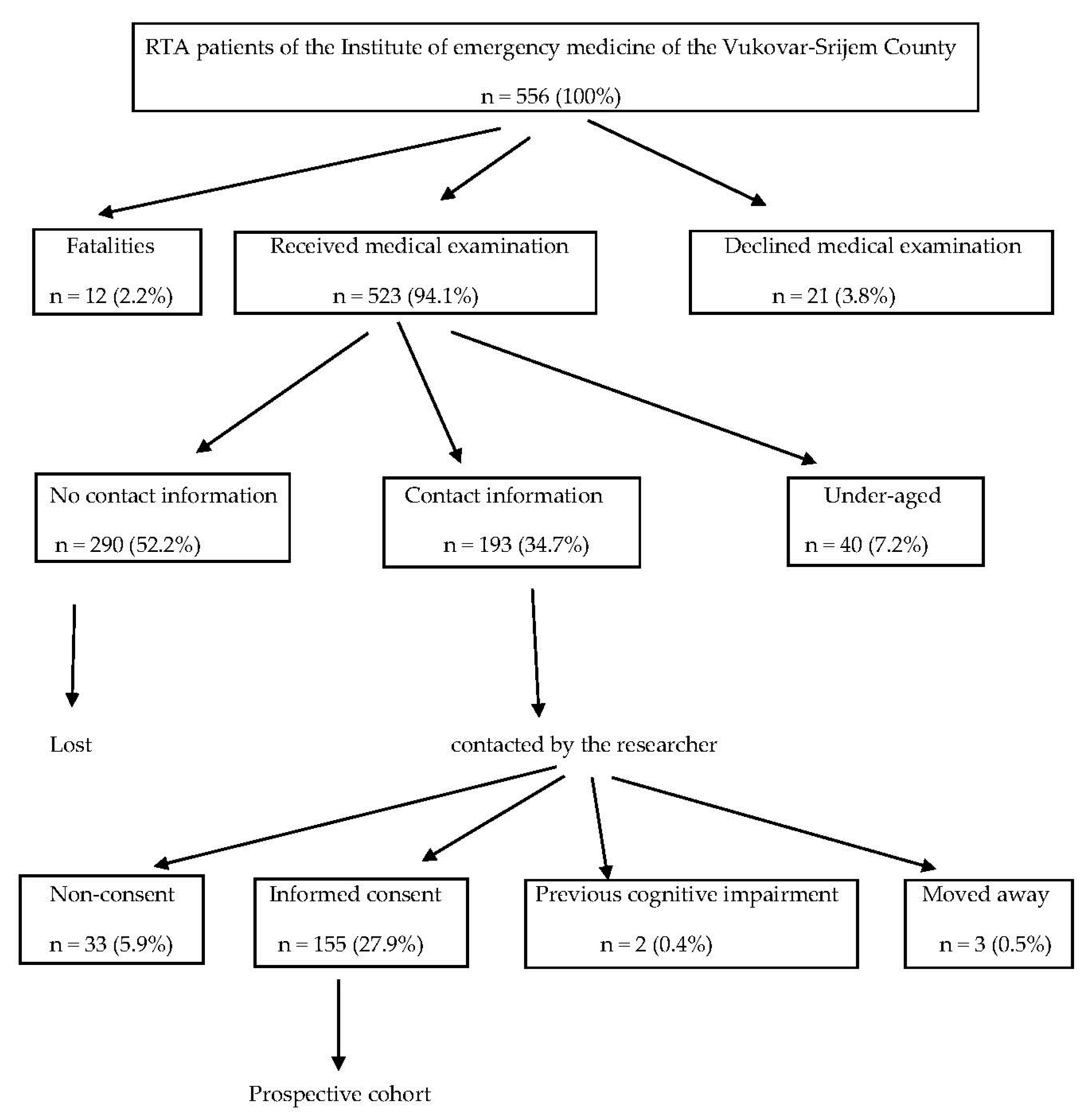
2. Materials and Methods
3. Results
3.1. Sociodemographic Characteristics of the Participants before the RTA
3.2. RTA-Related Characteristics of the Participants
3.3. RTA Injury Characteristics
3.4. Psychological Consequences of the RTA
4. Discussion
Strengths and limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- World Health Organization. Global Status Report on Road Safety 2018; WHO: Geneva, Switzerland, 2018; pp. 1–5. [Google Scholar]
- GBD 2013 DALYs and HALE Collaborators. Global, regional and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: Quantifying the epidemiological transition. Lancet 2015, 386, 2145–2191. [Google Scholar] [CrossRef]
- World Health Organization. Global Status Report on Road Safety 2015; WHO: Geneva, Switzerland, 2015; pp. X–XI. [Google Scholar]
- Croatian Bureau of Statistics. Registered Road Vehicles and Road Traffic Accidents in 2018; Croatian Bureau of Statistics: Zagreb, Croatia, 2019; pp. 1–3. [Google Scholar]
- Republic of Croatia, Ministry of Internal Affairs. Bulletin on Road Traffic Safety in 2017; Republic of Croatia, Ministry of Internal Affairs: Zagreb, Croatia, 2018; pp. 1–2.
- Hours, M.; Chossegros, L.; Charnay, P.; Tardy, H.; Nhac-Vu, H.T.; Boisson, D.; Luaute, J.; Laumon, B. Outcomes one year after a road accident: Results from the ESPARR cohort. Accid. Anal. Prev. 2013, 50, 92–102. [Google Scholar] [CrossRef] [PubMed]
- Chossegros, L.; Hours, M.; Charnay, P.; Bernard, M.; Fort, E.; Boisson, D.; Sancho, P.O.; Yao, S.N.; Laumon, B. Predictive factors of chronic post-traumatic stress disorder 6 months after a road traffic accident. Accident Anal. Prev. 2011, 43, 471–477. [Google Scholar] [CrossRef] [PubMed]
- Copanitsanou, P.; Drakoutos, E.; Kechagias, V. Posttraumatic stress, depressive emotions, and satisfaction with life after a road traffic accident. Otrhop. Nurs. 2018, 37, 43–53. [Google Scholar] [CrossRef] [PubMed]
- Kenardy, J.; Edmed, S.L.; Shourie, S.; Warren, J.; Crothers, A.; Brown, E.A.; Cameron, C.M.; Heron-Delaney, M. Changing patterns in the prevalence of posttraumatic stress disorder, major depressive episode and generalized anxiety disorder over 24 months following a road traffic crash: Results from the UQ SuPPORT study. J. Affect. Disord. 2018, 236, 172–179. [Google Scholar] [CrossRef]
- Ning, L.; Guan, S.; Liu, J. Impact of personality and social support on posttraumatic stress disorder after traffic accidents. Medicine 2017, 96, e7815. [Google Scholar] [CrossRef]
- Khodadadi-Hassankiadeh, N.; Nayeri, N.D.; Shahsavari, H.; Yousefzadeh-Chabok, S.; Haghani, H. Predictors of post-traumatic stress disorder among victims of serious motor vehicle accidents. Int. J. Community Based Nurs. Midwifery 2017, 5, 355–364. [Google Scholar]
- Hruska, B.; Irish, L.A.; Pacella, M.L.; Sledjeski, E.M.; Delahanty, D.L. PTSD symptom severity and psychiatric comorbidity in recent motor vehicle accident victims: A latent class analysis. J. Anxiety Disord. 2014, 28, 644–649. [Google Scholar] [CrossRef]
- Guest, R.; Tran, Y.; Gopinath, B.; Cameron, I.D.; Craig, A. Prevalence and psychometric screening for detection of major depressive disorder and post-traumatic stress disorder in adults injured in a motor vehicle crash who are engaged in compensation. BMC Psychol. 2018, 6, 1–12. [Google Scholar] [CrossRef]
- Yohannes, K.; Gebeyehu, A.; Adera, T.; Ayano, G.; Fekadu, W. Prevalence and correlates of post-traumatic stress disorder among survivors of road traffic accidents in Ethiopia. Int. J. Ment. Health Syst. 2018, 12, 1–8. [Google Scholar] [CrossRef]
- Asuquo, J.E.; Edet, B.E.; Abang, I.E.; Essien, E.A.; Osakwe, O.G.; Aigbomain, E.J.; Chigbundu, K.C. Depression and posttraumatic stress disorder among road traffic accident victims managed in a Tertiary hospital in Southern Nigera. Niger. J. Clin. Pract. 2017, 20, 170–175. [Google Scholar] [CrossRef] [PubMed]
- Dickov, A.; Martinović-Mitrović, S.; Vučković, N.; Siladji-Mladenović, D.; Mitrović, D.; Jovičević, M.; Mišić-Pavkov, G. Psychiatric consequences of stress after a vehicle accident. Psychiat. Danub. 2009, 21, 483–489. [Google Scholar]
- Lin, W.; Gong, L.; Xia, M.; Dai, W. Prevalence of posttraumatic stress disorder among road traffic accident survivors. A PRISMA compliant meta-analysis. Medicine 2018, 97, 1–7. [Google Scholar]
- Craig, A.; Tran, Y.; Guest, R.; Gopinath, B.; Jagnoor, J.; Bryant, R.; Collie, A.; Tate, R.; Kenardy, J.; Middleton, J.W.; et al. Psychological impact of injuries sustained in motor vehicle crashes: Systematic review and meta-analysis. BMJ Open 2016, 6, e011993. [Google Scholar] [CrossRef]
- Craig, A.; Elbers, N.A.; Jagnoor, J.; Gopinath, B.; Kifley, A.; Dinh, M.; Pozzato, I.; Ivers, R.Q.; Nicholas, M.; Cameron, I.D. The psychological impact of traffic injuries sustained in a road crash by bicyclists: A prospective study. Traffic Inj. Prev. 2017, 18, 273–280. [Google Scholar] [CrossRef]
- Papadakaki, M.; Ferraro, O.E.; Orsi, C.; Otte, D.; Tzamalouka, G.; von-der-Geest, M.; Lajunen, T.; Ozkan, T.; Morandi, A.; Sarris, M.; et al. Psychological distress and physical disability in patients sustaining severe injuries in road traffic crashes: Results from a one-year cohort study from three European countries. Injury 2017, 48, 297–306. [Google Scholar] [CrossRef]
- Heron-Delaney, M.; Kenardy, J.; Charlton, E.; Matsuoka, Y. A systematic review of predictors of posttraumatic stress disorder (PTSD) for adult road traffic crash survivors. Injury 2013, 44, 1413–1422. [Google Scholar] [CrossRef]
- Tournier, C.; Charnay, P.; Tardy, H.; Chossegros, L.; Carnis, L.; Hours, M. A few seconds to have an accident, a long time to recover: Consequences for road accident victims from the ESPARR cohort 2 years after the accident. Accid. Anal. Prev. 2014, 72, 422–432. [Google Scholar] [CrossRef]
- Kupchik, M.; Strous, R.D.; Erez, R.; Gonen, N.; Weizman, A.; Spivak, B. Demographic and clinical characteristics of motor vehicle accident victims in the community general health outpatient clinic: A comparison of PTSD and non-PTSD subjects. Depress. Anxiety 2007, 24, 244–250. [Google Scholar] [CrossRef]
- Stein, D.J.; Karam, E.G.; Shahly, V.; Hill, E.D.; King, A.; Petukhova, M.; Atwoli, L.; Bromet, E.J.; Florescu, S.; Haro, J.M.; et al. Post-traumatic stress disorder associated with life-threatening motor vehicle collisions in the WHO World Mental Health Surveys. BMC Psychiatry 2016, 16, 257. [Google Scholar] [CrossRef]
- Littleton, S.M.; Hughes, D.C.; Poustie, S.J.; Robinson, B.J.; Neeman, T.; Smith, P.N.; Cameron, I.D. The influence of fault on health in the immediate post-crash period following road traffic crashes. Injury 2012, 43, 1586–1592. [Google Scholar] [CrossRef]
- Ehring, T.; Ehlers, A.; Gluksman, E. Do cognitive models help in predicting the severity of posttraumatic stress disorder, phobia, and depression after motor vehicle accidents? A prospective longitudinal study. J. Consult. Clin. Psychol. 2008, 76, 219–230. [Google Scholar] [CrossRef]
- Jagnoor, J.; Blyth, F.; Gabbe, B.; Derrett, S.; Boufous, S.; Dinh, M.; Day, R.; Button, G.; Gillet, M.; Joseph, T.; et al. Factors influencing social and health outcomes after motor vehicle crash injury: An inception cohort study protocol. BMC Public Health 2014, 14, 199. [Google Scholar] [CrossRef]
- Civil, I.D.; Schwab, C.W. The Abbreviated Injury Scale, 1985 Revision: A Condensed Chart for Clinical Use. J. Traum. 1988, 28, 87–90. [Google Scholar] [CrossRef]
- Stevenson, M.; Segui-Gomez, M.; Lescohier, I.; Di Scala, C.; McDonald-Smith, G. An overview of the injury severity score and the new injury severity score. Inj. Prev. 2001, 7, 10–13. [Google Scholar] [CrossRef]
- Blanchard, E.B.; Jones-Alexander, J.; Buckley, T.C.; Forneris, C.A. Psychometric properties of the PTSD Checklist (PCL). Behav. Res. Ther. 1996, 34, 669–673. [Google Scholar] [CrossRef]
- National Center for PTSD. Using the PTSD checklist (PCL). Available online: https://sph.umd.edu/sites/default/files/files/PTSDChecklistScoring.pdf (accessed on 19 December 2019).
- Beck, A.T.; Epstein, N.; Brown, G.; Steer, R.A. An inventory for measuring clinical anxiety: Psychometric properties. J. Consult. Clin. Psych. 1988, 56, 893–897. [Google Scholar] [CrossRef]
- Beck, A.T.; Steer, R.A.; Garbin, M.G. Psychometric properties of the Beck Depression Inventory: Twenty-five years of evaluation. Clin. Psychol. Rev. 1988, 8, 77–100. [Google Scholar] [CrossRef]
- Elbers, N.A.; Akkermans, A.J.; Lockwood, K.; Craig, A.; Cameron, I.D. Factors that challenge health for people involved in the compensation process following a motor vehicle crash: A longitudinal study. BMC Public Health 2015, 15, 339. [Google Scholar] [CrossRef]
- European Commission. Mobility and Transport Road Safety. Available online: https://ec.europa.eu/transport/road_safety/specialist/knowledge/safetyratings/changing_design_upgrading_standards_and_reducing_casualties/in_car_safety_en (accessed on 19 December 2019).
- Croatian Centre for vehicles. Technical examination. Statistics. Available online: https://www.cvh.hr/media/3012/s01__pregled_starosti_vozila_prema_vrstama_vozila_2018.pdf (accessed on 19 December 2019).
- Hasselberg, M.; Kirsebom, M.; Backstorm, J.; Berg, H.Y.; Rissanen, R. I did NOT feel like this at all before the accident: Do men and women report different health and life consequences of a road traffic injury? Inj. Prev. 2019, 25, 307–312. [Google Scholar] [CrossRef]
- Giummarra, M.; Black, O.; Smith, P.; Collie, A.; Hassani-Mahmooei, B.; Arnold, C.A.; Gong, J.; Gabbe, B.J. A population-based study of treated mental health and persistent pain conditions after transport injury. Injury 2018, 49, 1787–1795. [Google Scholar] [CrossRef]
- Littleton, S.M.; Cameron, I.D.; Poustie, S.J.; Hughes, D.C.; Robinson, B.J.; Neeman, T.; Smith, P.N. The association of compensation on longer term health status for people with musculosceletal injuries following road traffic crashes: Emergency department inception cohort study. Injury 2011, 42, 927–933. [Google Scholar] [CrossRef]
- Ravn, S.L.; Hartvigsen, J.; Hansen, M.; Sterling, M.; Andresen, T.E. Do post-traumatic pain and post-traumatic stress symptomatology mutually maintain each other? A systematic review of cross-lagged studies. Pain 2018, 159, 2159–2169. [Google Scholar] [CrossRef]
- Jagnoor, J.; De Wolf, A.; Nicholas, M.; Maher, C.G.; Casey, P.; Blyth, F.; Harris, I.A.; Cameron, I.D. Restriction in functioning and quality of life is common in people 2 months after compensable motor vehicle crashes: Prospective cohort study. Inj. Epidemiol. 2015, 2, 8. [Google Scholar] [CrossRef][Green Version]
- Murgatroyd, D.F.; Harris, I.A.; Tran, Y.; Cameron, I.D. The association between seeking financial compensation and injury recovery following motor vehicle related orthopaedic trauma. BMC Musculoskel. Dis. 2016, 17, 282. [Google Scholar] [CrossRef]
- Undavalli, C.; Das, P.; Dutt, T.; Bhoi, S.; Kashyap, R. PTSD in post-traffic accident patients requiring hospitalization in Indian subcontinet: A review on magnitude of the problem and management guidelines. J. Emerg. Trauma Shock 2014, 7, 327–331. [Google Scholar]
| N | % | |
|---|---|---|
| Gender | ||
| Male | 85 | 54.8 |
| Female | 70 | 45.2 |
| Age group (years) | ||
| Younger (18–41) | 77 | 49.7 |
| Older (≥42) | 78 | 50.3 |
| Residence | ||
| Urban | 65 | 41.9 |
| Rural | 90 | 58.1 |
| Education level | ||
| Primary | 28 | 18.1 |
| Secondary | 104 | 67.1 |
| University | 23 | 14.8 |
| Employment | ||
| Employed | 90 | 58.1 |
| Unemployed | 43 | 27.7 |
| Retired | 22 | 14.2 |
| Marital status | ||
| Single | 59 | 38.1 |
| With a partner | 96 | 61.9 |
| Self-perceived economic status | ||
| Below average | 30 | 19.4 |
| Average | 92 | 59.3 |
| Above average | 33 | 21.3 |
| Smoking | ||
| No | 97 | 62.6 |
| Yes | 58 | 37.4 |
| Alcohol use | ||
| No | 76 | 49.0 |
| Yes | 79 | 51.0 |
| Psychoactive substance use | ||
| Never | 154 | 99.4 |
| Sometimes | 1 | 0.6 |
| Religiousness | ||
| No | 16 | 10.3 |
| Yes | 139 | 89.7 |
| Medication use | ||
| No | 75 | 48.4 |
| Yes | 80 | 51.6 |
| Type of medication used | ||
| None | 75 | 48.5 |
| Nonpsychiatric | 63 | 40.6 |
| Psychiatric | 5 | 3.2 |
| Both types | 12 | 7.7 |
| Previous RTA experience | ||
| No | 91 | 58.7 |
| Yes | 64 | 41.3 |
| Previous traumatic experience | ||
| No | 73 | 47.1 |
| Yes | 82 | 52.9 |
| Previous PTSD | ||
| No | 150 | 96.8 |
| Yes | 5 | 3.2 |
| Previous chronic illness | ||
| No | 90 | 58.1 |
| Yes | 65 | 41.9 |
| Previous psychiatric illness | ||
| No | 137 | 88.4 |
| Yes | 18 | 11.6 |
| Previous permanent pain | ||
| No | 140 | 90.3 |
| Yes | 15 | 9.7 |
| N | % | |
|---|---|---|
| Road user type | ||
| Motor vehicle driver | 91 | 58.7 |
| Codriver/passenger | 51 | 32.9 |
| Cyclist/pedestrian | 13 | 8.4 |
| Motor vehicles engaged in the RTA | ||
| None | 1 | 0.6 |
| One | 73 | 47.1 |
| More than one | 81 | 52.3 |
| Total number of injured people in the RTA | ||
| None | 16 | 10.3 |
| One | 67 | 43.3 |
| 2–3 | 58 | 37.4 |
| 4–5 | 14 | 9 |
| Fatalities in the RTA | ||
| No | 153 | 98.7 |
| Yes | 2 | 1.3 |
| Fault in the RTA | ||
| No | 96 | 61.9 |
| Yes | 55 | 35.5 |
| Unknown | 4 | 2.6 |
| Compensation claim after the RTA | ||
| No | 89 | 57.4 |
| Yes | 66 | 42.6 |
| Received compensation after the RTA | ||
| No | 142 | 91.6 |
| Yes | 13 | 8.4 |
| N | % | |
|---|---|---|
| Number of injuries in the RTA | ||
| None | 18 | 11.6 |
| One | 41 | 26.5 |
| Multiple | 96 | 61.9 |
| Location of injuries in the RTA | ||
| None | 18 | 11.6 |
| One: Head | 18 | 11.6 |
| Face | 2 | 1.3 |
| Neck | 7 | 4.5 |
| Thora | 7 | 4.5 |
| Abdomen | 1 | 0.6 |
| Spine | 3 | 1.9 |
| Hands | 3 | 1.9 |
| Legs | 8 | 5.2 |
| Multiple body parts | 88 | 56.9 |
| Primary site of injury | ||
| None | 18 | 11.6 |
| Head | 48 | 31.1 |
| Neck | 29 | 18.7 |
| Thorax | 16 | 10.3 |
| Abdomen | 9 | 5.8 |
| Hands | 14 | 9 |
| Legs | 21 | 13.5 |
| Injury severity | ||
| No injury | 18 | 11.6 |
| Mild | 82 | 52.9 |
| Moderate | 25 | 16.2 |
| Serious | 23 | 14.8 |
| Severe | 5 | 3.2 |
| Critical | 2 | 1.3 |
| Self-perceived threat to life | ||
| No | 88 | 56.8 |
| Yes | 67 | 43.2 |
| Unconsciousness in the RTA | ||
| No | 129 | 83.2 |
| Yes | 26 | 16.8 |
| Post-RTA amnesia | ||
| No | 131 | 84.5 |
| Yes | 24 | 15.5 |
| Hospitalization | ||
| No | 105 | 67.7 |
| Yes | 50 | 32.3 |
| Hospitalization duration | ||
| 0 days | 105 | 67.8 |
| 1–3 days | 21 | 13.5 |
| 4–10 days | 16 | 10.3 |
| Over 10 days | 13 | 8.4 |
| Surgical treatment | ||
| No | 140 | 90.3 |
| Yes | 15 | 9.7 |
| Rehabilitation after RTA | ||
| No | 119 | 76.8 |
| Yes | 36 | 23.2 |
| Pain location after RTA | ||
| No pain | 34 | 21.9 |
| Certain body part | 50 | 32.3 |
| Multiple body parts | 71 | 45.8 |
| Pain frequency after RTA | ||
| Never | 34 | 21.9 |
| Circumstantial | 30 | 19.4 |
| Occasional | 49 | 31.6 |
| Permanent | 42 | 27.1 |
| PTSD symptoms | ||
| No | 105 | 67.7 |
| Yes | 50 | 32.3 |
| Depression symptoms | ||
| Normal mood | 128 | 82.6 |
| Mild mood disturbance | 20 | 12.9 |
| Borderline clinical depression | 7 | 4.5 |
| Anxiety symptoms | ||
| Low | 146 | 94.2 |
| Moderate | 8 | 5.2 |
| Concerning | 1 | 0.6 |
| Injury Affliction (yes/no) | Injury Severity (NISS) | |
|---|---|---|
| Gender | p = 0.623a | p = 0.788a |
| Age | p = 0.453a | p = 0.245a |
| Residency | p = 0.612a | p = 0.069a |
| Education level | p = 0.242b | p = 0.270b |
| Employment status | p = 0.124b | p = 0.092b |
| Self-perceived economic status | p = 0.006b | p = 0.010b |
| Smoking | p > 0.999a | p = 0.937a |
| Alcohol use | p = 0.211a | p = 0.257a |
| Drug use | p > 0.999b | p > 0.999b |
| Religiousness | p = 0.219b | p = 0.047b |
| Medication use | p = 0.318a | p = 0.247a |
| Type of medication used | p = 0.563b | p = 0.600b |
| Previous RTA experience | p = 0.454a | p = 0.708a |
| Previous traumatic experience | p > 0.999a | p = 0.933a |
| Previous PTSD | p > 0.999b | p = 0.697b |
| Previous chronic illness | p = 0.216a | p = 0.403a |
| Previous psychiatric illness | p = 0.697b | p = 0.622b |
| Previous permanent pain | p = 0.687b | p = 0.930b |
| Self-perceived threat to life | p = 0.001a | p = 0.002a |
| Pain after RTA | p < 0.001b | p < 0.001b |
| Road user type | p = 0.088b | p = 0.053b |
| Rehabilitation after RTA | p = 0.014b | p = 0.010b |
| Compensation claim | p = 0.804a | p = 0.860a |
| Received compensation | p = 0.649b | p = 0.138b |
| Depression Symptoms | Anxiety Symptoms | PTSD Symptoms | |
|---|---|---|---|
| Sociodemographic | |||
| Gender | p = 0.525a | p = 0.079b | p = 0.038a |
| Age | p = 0.089a | p = 0.495b | p = 0.864a |
| Residency | p = 0.135a | p > 0.999b | p = 0.862a |
| Education level | p = 0.856b | p = 0.515b | p = 0.439a |
| Employment status | p = 0.407b | p > 0.999b | p = 0.059b |
| Marital status | p = 0.666a | p > 0.999b | p = 0.860a |
| Self-perceived economic status | p = 0.001a | p = 0.441b | p = 0.025a |
| Religiousness | p < 0.001b | p = 0.234b | p = 0.156a |
| Pre-RTA health status | |||
| Smoking | p = 0.669a | p = 0.729b | p = 0.597a |
| Alcohol use | p = 0.833a | p = 0.743b | p = 0.169a |
| Psychoactive substance use | p = 0.174b | p = 0.058b | p = 0.323a |
| Previous RTA experience | p = 0.202a | p = 0.308b | p = 0.226a |
| Previous traumatic experience | p = 0.057a | p = 0.174b | p = 0.395a |
| Previous PTSD | p = 0.588b | p > 0.999b | p = 0.658b |
| Previous chronic illness | p = 0.054a | p = 0.035b | p = 0.169a |
| Previous psychiatric illness | p = 0.999b | p = 0.011b | p = 0.008a |
| Previous permanent pain | p = 0.299b | p < 0.001b | p > 0.999b |
| Medication use | p = 0.001a | p = 0.169b | p = 0.002a |
| Type of medication used | p = 0.002b | p = 0.010b | p < 0.001b |
| Injury-related | |||
| Injury affliction | p = 0.741b | p > 0.999b | p = 0.013a |
| Injury severity | p < 0.001b | p = 0.524b | p = 0.004a |
| Self-perceived threat to life | p = 0.087a | p = 0.040b | p = 0.002a |
| Pain after RTA | p = 0.200a | p = 0.208b | p = 0.006a |
| Hospitalization | p = 0.006a | p = 0.719b | p = 0.358a |
| Surgical treatment | p = 0.001b | p > 0.999b | p = 0.564b |
| Unconsciousness in the RTA | p = 0.020b | p > 0.999b | p = 0.254b |
| Post-RTA amnesia | p = 0.015b | p = 0.356b | p = 0.057a |
| Hospitalization duration | p = 0.009b | p = 0.671b | p = 0.011b |
| RTA-related | |||
| Fault in the RTA | p = 0.278b | p = 0.227b | p = 0.044b |
| Deaths in the RTA | p = 0.319b | p > 0.999b | p = 0.543b |
| Compensation claim | p = 0.284a | p = 0.171b | p < 0.001a |
| Road user type | p = 0.085b | p = 0.094b | p = 0.177b |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kovacevic, J.; Miskulin, M.; Degmecic, D.; Vcev, A.; Leovic, D.; Sisljagic, V.; Simic, I.; Palenkic, H.; Vcev, I.; Miskulin, I. Predictors of Mental Health Outcomes in Road Traffic Accident Survivors. J. Clin. Med. 2020, 9, 309. https://doi.org/10.3390/jcm9020309
Kovacevic J, Miskulin M, Degmecic D, Vcev A, Leovic D, Sisljagic V, Simic I, Palenkic H, Vcev I, Miskulin I. Predictors of Mental Health Outcomes in Road Traffic Accident Survivors. Journal of Clinical Medicine. 2020; 9(2):309. https://doi.org/10.3390/jcm9020309
Chicago/Turabian StyleKovacevic, Jelena, Maja Miskulin, Dunja Degmecic, Aleksandar Vcev, Dinko Leovic, Vladimir Sisljagic, Ivana Simic, Hrvoje Palenkic, Ivan Vcev, and Ivan Miskulin. 2020. "Predictors of Mental Health Outcomes in Road Traffic Accident Survivors" Journal of Clinical Medicine 9, no. 2: 309. https://doi.org/10.3390/jcm9020309
APA StyleKovacevic, J., Miskulin, M., Degmecic, D., Vcev, A., Leovic, D., Sisljagic, V., Simic, I., Palenkic, H., Vcev, I., & Miskulin, I. (2020). Predictors of Mental Health Outcomes in Road Traffic Accident Survivors. Journal of Clinical Medicine, 9(2), 309. https://doi.org/10.3390/jcm9020309







