Clinical Significance of ARID1A and ANXA1 in HER-2 Positive Breast Cancer
Abstract
1. Introduction
2. Experimental Section
2.1. Patients and Samples Collection
2.2. Immunohistochemistry (IHC)
2.3. Immunohistochemistry Scoring
2.4. Statistical Analysis
3. Results
3.1. Clinical and Pathological Data
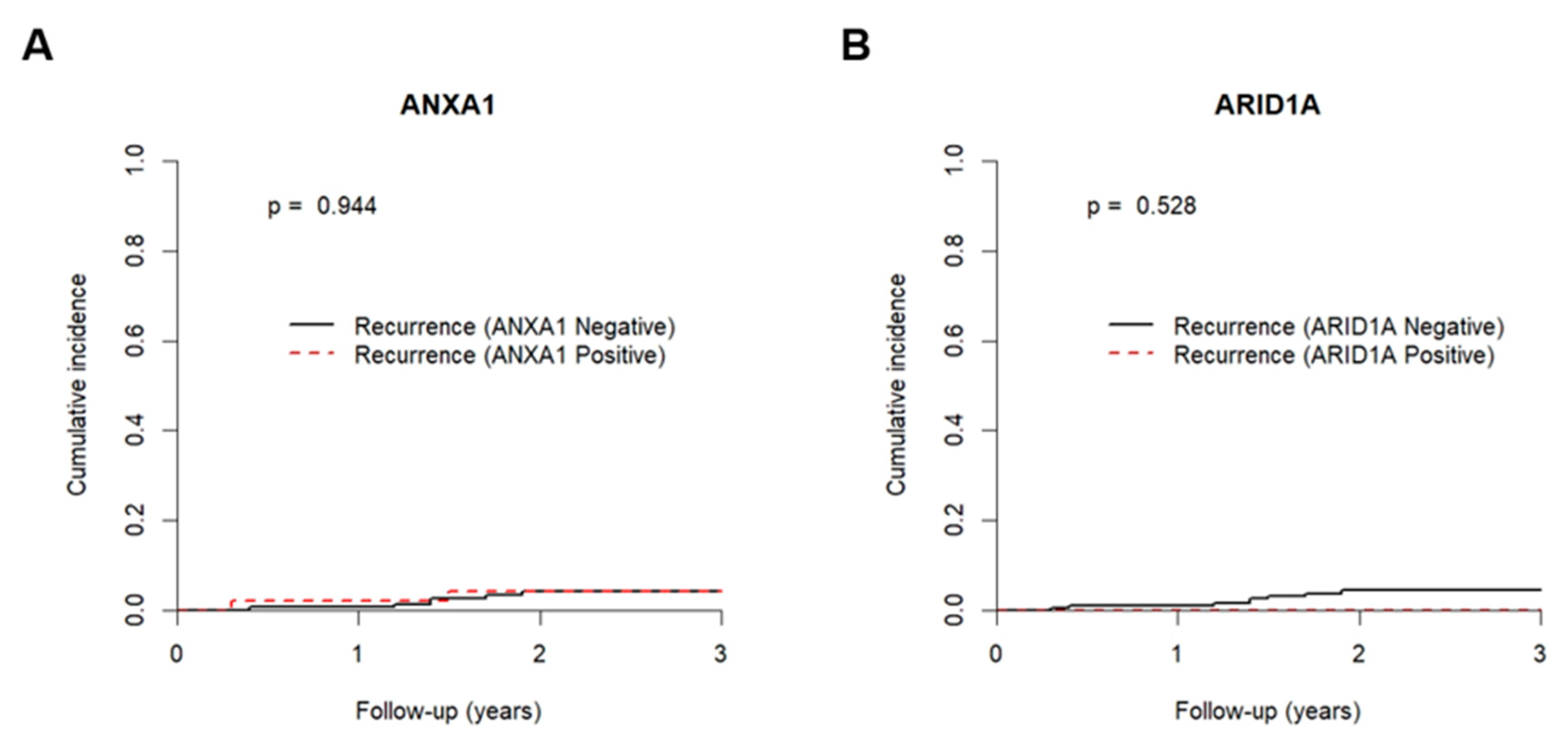
3.2. Resistance to Trastuzumab
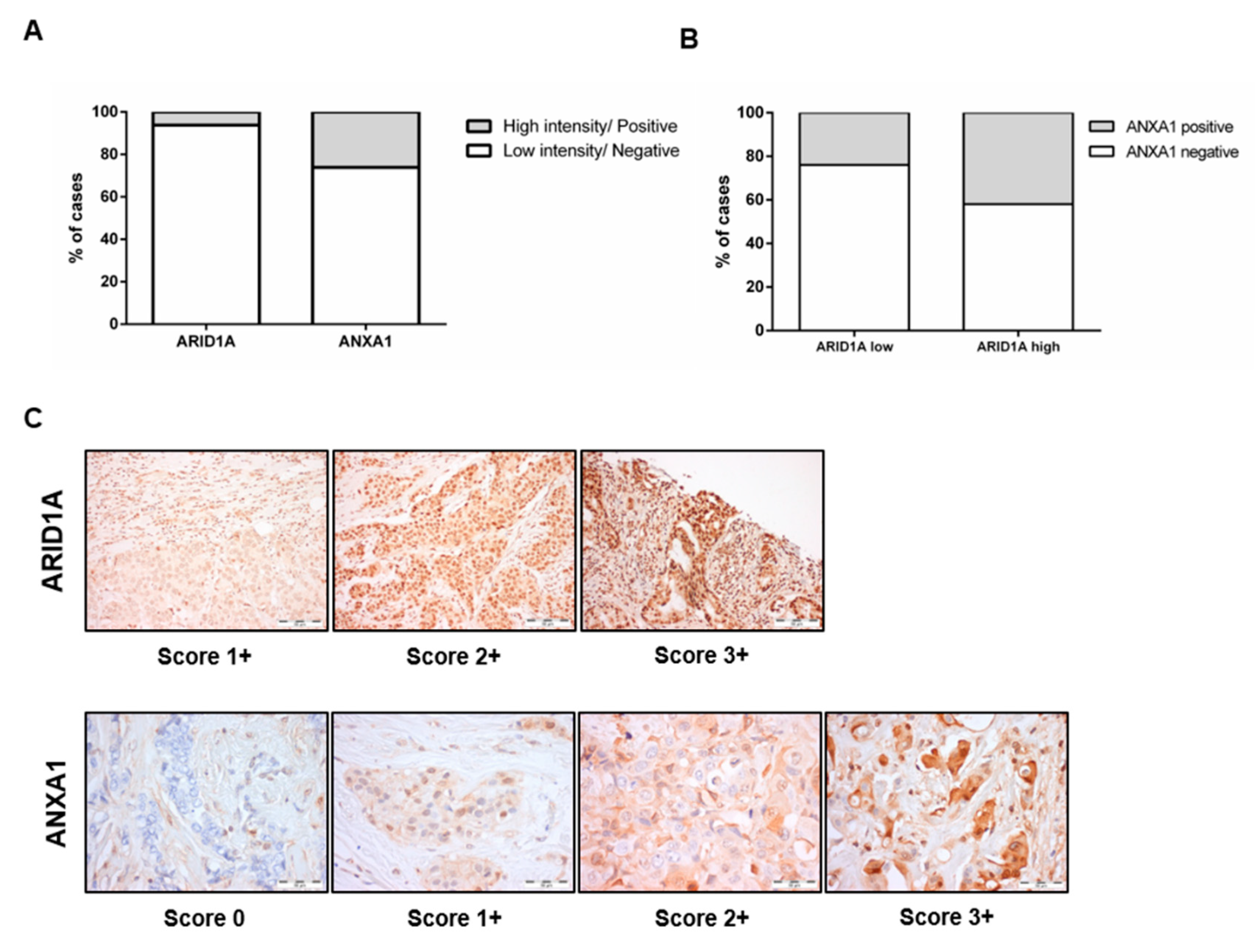
3.3. Relationship between ARID1A and ANXA1
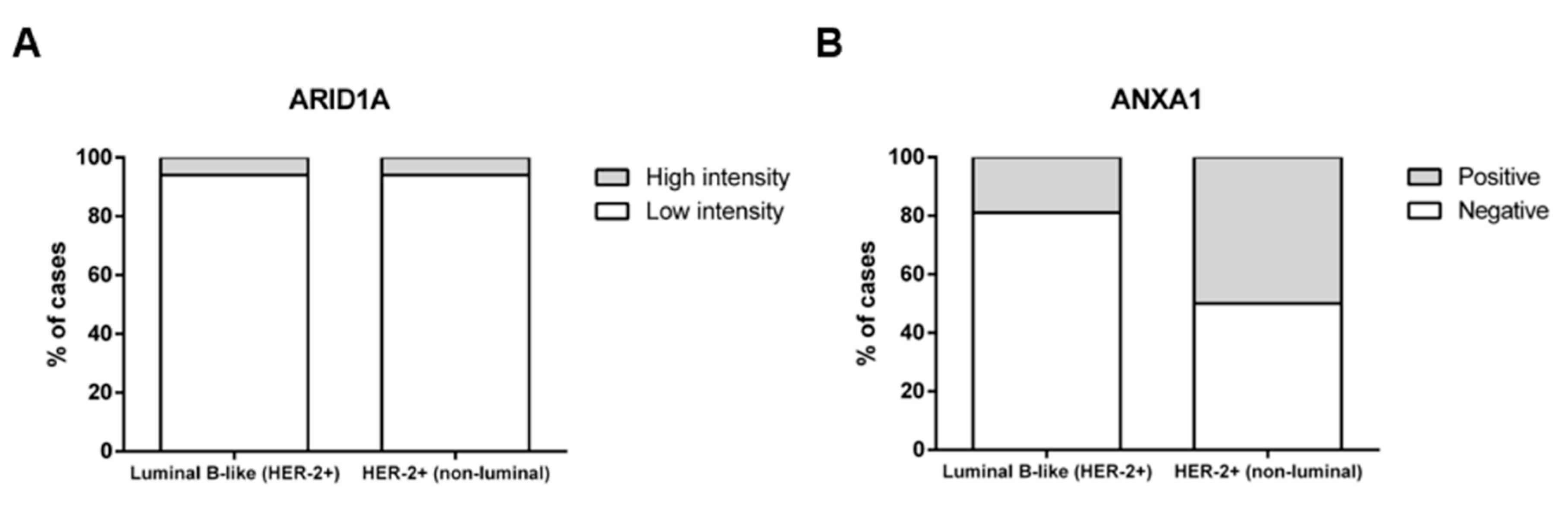
3.4. ANXA1 Expression Is Higher in the HER-2+ (Non-Luminal) Subtype
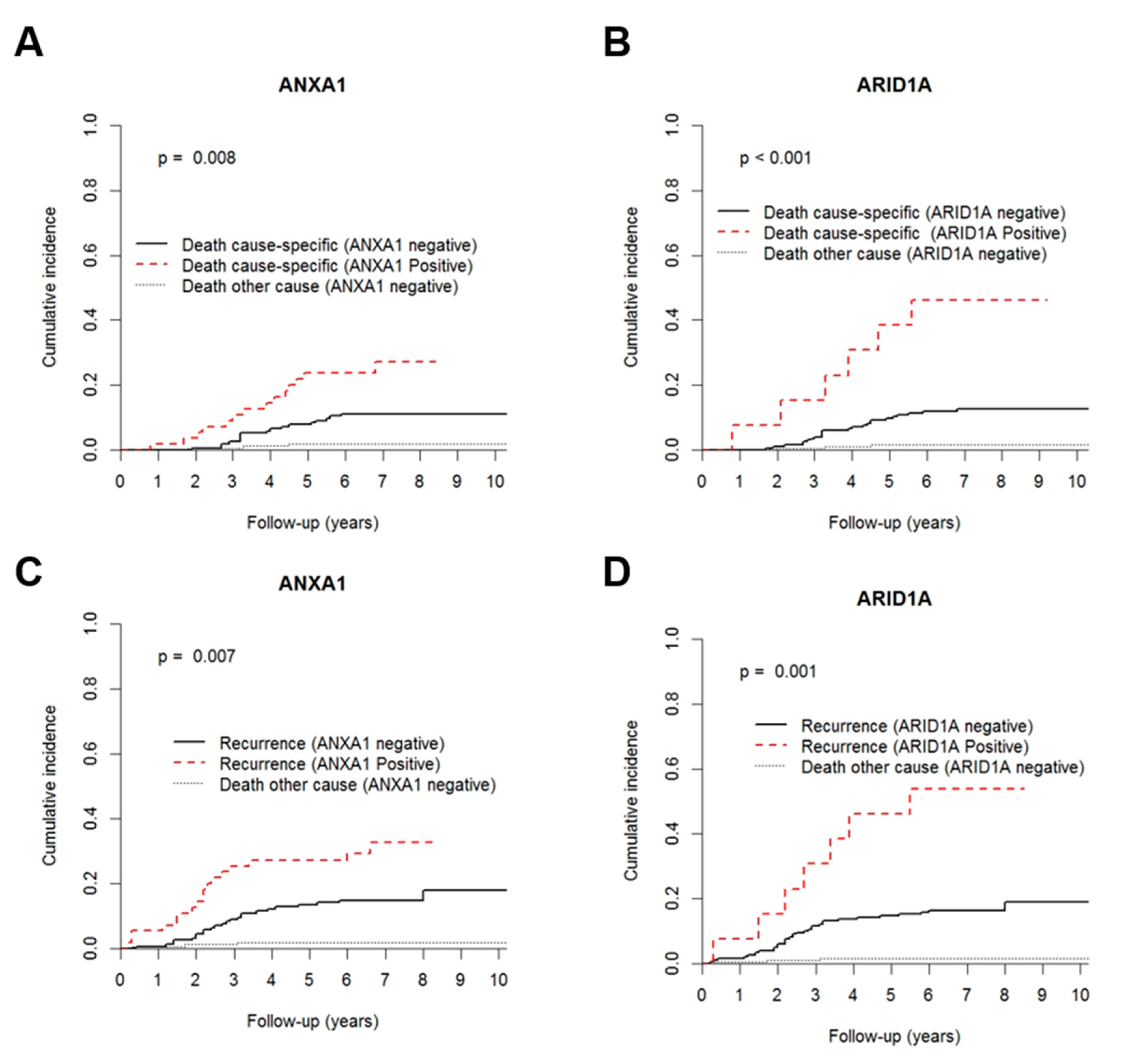
3.5. High ARID1A and ANXA1 Expression Is Associated with Early Recurrence and High Mortality
4. Discussion
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Bray, F.; Ferlay, J.; Soerjomataram, I. Global Cancer Statistics 2018: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2018, 68, 1–31. [Google Scholar] [CrossRef]
- Magnani, L.; Lupien, M. Chromatin landscape and endocrine response in breast cancer R eview. Epigenomics 2012, 4, 675–683. [Google Scholar] [CrossRef]
- Mitri, Z.; Constantine, T.; O’Regan, R. The HER2 Receptor in Breast Cancer: Pathophysiology, Clinical Use, and New Advances in Therapy. Chemother. Res. Pract. 2012, 2012, 1–7. [Google Scholar] [CrossRef]
- Loibl, S.; Gianni, L. HER2-positive breast cancer. Lancet 2016, 6736, 1–15. [Google Scholar] [CrossRef]
- Cardoso, F.; Kyriakides, S.; Ohno, S.; Penault-Llorca, F.; Poortmans, P.; Rubio, I.T.; Zackrisson, S.; Senkus, E. Early breast cancer: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 2019, 30, 1194–1220. [Google Scholar] [CrossRef]
- Hudis, C.A. Trastuzuma—Mechanism of Action and Use in Clinical Practice. N. Engl. J. Med. 2007, 357, 39–51. [Google Scholar] [CrossRef]
- Wilken, J.A.; Maihle, N.J. Primary trastuzumab resistance: New tricks for an old drug. Ann. N. Y. Acad. Sci. 2010, 1210, 53–65. [Google Scholar] [CrossRef]
- Pohlmann, P.R.; Mayer, I.A.; Mernaugh, R. Resistance to Trastuzumab in Breast Cancer. Clin. Cancer Res. 2009, 15, 7479–7491. [Google Scholar] [CrossRef]
- Arteaga, C.L.; Sliwkowski, M.X.; Osborne, C.K.; Perez, E.A.; Puglisi, F.; Gianni, L. Treatment of HER2-positive breast cancer: Current status and future perspectives. Nat. Rev. Clin. Oncol. 2011, 9, 16–32. [Google Scholar] [CrossRef]
- Karina, B.; Hirata, B.; Massayo, J.; Oda, M.; Guembarovski, R.L.; Ariza, C.B.; Eduardo, C.; Oliveira, C.D.; Angelica, M.; Watanabe, E. Molecular Markers for Breast Cancer: Prediction on Tumor Behavior. Dis. Markers 2014, 2014, 1–12. [Google Scholar] [CrossRef]
- Berns, K.; Horlings, H.M.; Hennessy, B.T.; Madiredjo, M.; Hijmans, E.M.; Beelen, K.; Linn, S.C.; Gonzalez-Angulo, A.M.; Stemke-Hale, K.; Hauptmann, M.; et al. A Functional Genetic Approach Identifies the PI3K Pathway as a Major Determinant of Trastuzumab Resistance in Breast Cancer. Cancer Cell 2007, 12, 395–402. [Google Scholar] [CrossRef]
- Gajria, D.; Sarat, C. Her2- amplified breast cancer: Mechanisms of resistance and novel targeted therapies. Expert Rev. Anticancer. Ther. 2011, 11, 263–275. [Google Scholar] [CrossRef]
- Berns, K.; Sonnenblick, A.; Gennissen, A.; Brohée, S.; Hijmans, E.M.; Evers, B.; Fumagalli, D.; Desmedt, C.; Loibl, S.; Denkert, C.; et al. Loss of ARID1A activates ANXA1, which serves as a predictive biomarker for trastuzumab resistance. Clin. Cancer Res. 2016, 22, 5238–5248. [Google Scholar] [CrossRef] [PubMed]
- Zhao, J.; Liu, C.; Zhao, Z. ARID1A: A potential prognostic factor for breast cancer. Tumor Biol. 2014, 35, 4813–4819. [Google Scholar] [CrossRef]
- Cho, H.D.; Lee, J.E.; Jung, H.Y.; Oh, M.-H.; Lee, J.-H.; Jang, S.-H.; Kim, K.-J.; Han, S.W.; Kim, S.Y.; Kim, H.J.; et al. Loss of Tumor Suppressor ARID1A Protein Expression Correlates with Poor Prognosis in Patients with Primary Breast Cancer. J. Breast Cancer 2016, 18, 339–346. [Google Scholar] [CrossRef]
- Samartzis, E.P.; Noske, A.; Dedes, K.J.; Fink, D.; Imesch, P. ARID1A mutations and PI3K/AKT pathway alterations in endometriosis and endometriosis-associated ovarian carcinomas. Int. J. Mol. Sci. 2013, 14, 18824–18849. [Google Scholar] [CrossRef]
- Katagiri, A.; Nakayama, K.; Rahman, M.T.; Rahman, M.; Katagiri, H.; Ishikawa, M.; Ishibashi, T.; Iida, K.; Otsuki, Y.; Nakayama, S.; et al. Frequent loss of tumor suppressor ARID1A protein expression in adenocarcinomas/adenosquamous carcinomas of the uterine cervix. Int. J. Gynecol. Cancer 2012, 22, 208–212. [Google Scholar] [CrossRef]
- Bosse, T.; Ter Haar, N.T.; Seeber, L.M.; Diest, P.J.V.; Hes, F.J.; Vasen, H.F.; Nout, R.A.; Creutzberg, C.L.; Morreau, H.; Smit, V.T. Loss of ARID1A expression and its relationship with PI3K-Akt pathway alterations, TP53 and microsatellite instability in endometrial cancer. Mod. Pathol. 2013, 26, 1525–1535. [Google Scholar] [CrossRef]
- Cho, H.; Kim, J.S.Y.; Chung, H.; Perry, C.; Lee, H.; Kim, J.H. Loss of ARID1A/BAF250a expression is linked to tumor progression and adverse prognosis in cervical cancer. Hum. Pathol. 2013, 44, 1365–1374. [Google Scholar] [CrossRef]
- Ang, X.W.; Agl, N.G.N.; Lowers, S.F.; Weitzig, D.Z.; Allas, P.B.D.; Oran, E.M. Expression of p270 (ARID1A), a component of human SWI/SNF complexes in human tumors. Int. J. Cancer 2004, 112, 636–642. [Google Scholar] [CrossRef]
- Sheikh, M.H.; Solito, E. Annexin A1: Uncovering the Many Talents of an Old Protein. Int. J. Mol. Sci. 2018, 19, 1045. [Google Scholar] [CrossRef]
- Boudhraa, Z.; Bouchon, B.; Viallard, C.; D’Incan, M.; Degoul, F. Annexin A1 localization and its relevance to cancer. Clin. Sci. 2016, 130, 205–220. [Google Scholar] [CrossRef]
- Sun, M.-Z.E.A. Potential role of ANXA1 in cancer. Futur. Oncol. 2013, 9, 1773–1793. [Google Scholar] [CrossRef]
- Sr, L.; Io, E.; Schnitt, S.J.; Al, E. WHO Classification of Tumours, 4th ed.; IARC WHO Classification of Tumours: Lyon, France, 2012; p. 240. [Google Scholar]
- Yom, C.K.; Han, W.; Kim, S.W.; Kim, H.S.; Shin, H.C.; Chang, J.N.; Koo, M.; Noh, D.Y.; Moon, B.I. Clinical signifcance of annexin A1 expression in breast cancer. J. Breast Cancer 2011, 14, 262–268. [Google Scholar] [CrossRef]
- Verma, S.; Miles, D.; Gianni, L.; Krop, I.E.; Welslau, M.; Baselga, J.; Pegram, M.; Oh, D.-Y.; Diéras, V.; Guardino, E.; et al. Trastuzumab emtansine for HER2-positive advanced breast cancer. N. Engl. J. Med. 2012, 367, 1783–1791. [Google Scholar] [CrossRef]
- Sørlie, T.; Perou, C.M.; Tibshirani, R.; Aas, T.; Geisler, S.; Johnsen, H.; Hastie, T.; Eisen, M.B.; Rijn, M.V.D.; Jeffrey, S.S.; et al. Gene expression patterns of breast carcinomas distinguish tumor subclasses with clinical implications. Proc. Natl. Acad. Sci. USA 2001, 98, 10869–10874. [Google Scholar] [CrossRef]
- Eliyatkin, N.; Yalcin, E.; Zengel, B.; Aktaş, S.; Vardar, E. Molecular Classification of Breast Carcinoma: From Traditional, Old-Fashioned Way to A New Age, and A New Way. J. Breast Health 2015, 11, 59–66. [Google Scholar] [CrossRef]
- Nagata, Y.; Lan, K.H.; Zhou, X.; Tan, M.; Esteva, F.J.; Sahin, A.A.; Klos, K.S.; Li, P.; Monia, B.P.; Nguyen, N.T.; et al. PTEN activation contributes to tumor inhibition by trastuzumab, and loss of PTEN predicts trastuzumab resistance in patients. Cancer Cell 2004, 6, 117–127. [Google Scholar] [CrossRef]
- De Graauw, M.; van Miltenburg, M.H.; Schmidt, M.K.; Pont, C.; Lalai, R.; Kartopawiro, J.; Pardali, E.; Le Devedec, S.E.; Smit, V.T.; van der Wal, A.; et al. Annexin A1 regulates TGF- signaling and promotes metastasis formation of basal-like breast cancer cells. Proc. Natl. Acad. Sci. USA 2010, 107, 6340–6345. [Google Scholar] [CrossRef]
- Sonnenblick, A.; Brohée, S.; Fumagalli, D.; Rothé, F.; Vincent, D.; Ignatiadis, M.; Desmedt, C.; Salgado, R.; Sirtaine, N.; Loi, S.; et al. Integrative proteomic and gene expression analysis identify potential biomarkers for adjuvant trastuzumab resistance: Analysis from the Fin-her phase III randomized trial. Oncotarget 2015, 6, 30306–30316. [Google Scholar] [CrossRef]
- Mamo, A.; Cavallone, L.; Tuzmen, S.; Chabot, C.; Ferrario, C.; Hassan, S.; Edgren, H.; Kallioniemi, O.; Aleynikova, O.; Przybytkowski, E.; et al. An integrated genomic approach identifies ARID1A as a candidate tumor-suppressor gene in breast cancer. Oncogene 2011, 31, 2090–2100. [Google Scholar] [CrossRef]
- International, T.; Epidemiology, C.; Zhang, X.; Zhang, Y.; Yang, Y.; Niu, M.; Sun, S.; Ji, H.; Ma, Y. Frequent low expression of chromatin remodeling gene ARID1A in breast cancer and its clinical significance. Cancer Epidemiol. 2012, 36, 288–293. [Google Scholar] [CrossRef]
- Lin, Y.-F.; Tseng, I.-J.; Kuo, C.-J.; Lin, H.-Y.; Chiu, I.J.; Chiu, H.-W. High-level expression of ARID1A predicts a favourable outcome in triple-negative breast cancer patients receiving paclitaxel-based chemotherapy. J. Cell. Mol. Med. 2018, 22, 2458–2468. [Google Scholar] [CrossRef]
- Okano, M.; Kumamoto, K.; Saito, M.; Onozawa, H.; Saito, K.; Abe, N.; Ohtake, T.; Takenoshita, S. Upregulated Annexin A1 promotes cellular invasion in triple-negative breast cancer. Oncol. Rep. 2015, 33, 1064–1070. [Google Scholar] [CrossRef]
- Zóia, M.A.P.; Azevedo, F.V.P.; Vecchi, L.; Mota, S.T.S.; Rodovalho, V.d.R.; Cordeiro, A.O.; Correia, L.I.V.; Silva, A.C.A.; Ávila, V.d.M.R.; de Araújo, T.G.; et al. Inhibition of triple-negative breast cancer cell aggressiveness by cathepsin D blockage: Role of annexin A1. Int. J. Mol. Sci. 2019, 20. [Google Scholar] [CrossRef]
- Bhardwaj, A.; Ganesan, N.; Tachibana, K.; Rajapakshe, K.; Albarracin, C.T.; Gunaratne, P.H.; Coarfa, C.; Bedrosian, I. Annexin A1 Preferentially Predicts Poor Prognosis of Basal-Like Breast Cancer Patients by Activating mTOR-S6 Signaling. PLoS ONE 2015, 10, e0127678. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Yuan, Y.; Kar, S.; Kanchi, M.M.; Arora, S.; Kim, J.E.; Koh, P.F.; Yousef, E.; Samy, R.P.; Shanmugam, M.K.; et al. PPARγ Ligand-induced Annexin A1 Expression Determines Chemotherapy Response via Deubiquitination of Death Domain Kinase RIP in Triple-negative Breast Cancers. Mol. Cancer Ther. 2017, 16, 2528–2542. [Google Scholar] [CrossRef]
- Sobral-Leite, M.; Wesseling, J.; Smit, V.T.H.B.M.; Nevanlinna, H.; van Miltenburg, M.H.; Sanders, J.; Hofland, I.; Blows, F.M.; Coulson, P.; Patrycja, G.; et al. Annexin A1 expression in a pooled breast cancer series: Association with tumor subtypes and prognosis. BMC Med. 2015, 13, 1–11. [Google Scholar] [CrossRef]
- Nahta, R.; Yu, D.; Hung, M.C.; Hortobagyi, G.N.; Esteva, F.J. Mechanisms of disease: Understanding resistance to HER2-targeted therapy in human breast cancer. Nat. Clin. Pr. Oncol. 2006, 3, 269–280. [Google Scholar] [CrossRef]
- Porta, C.; Paglino, C.; Mosca, A. Targeting PI3K / Akt / mTOR signaling in cancer. Front. Oncol. 2014, 4, 1–11. [Google Scholar] [CrossRef]
- Nahta, R.; Shabaya, S.; Ozbay, T.; Rowe, D. Personalizing HER2-Targeted Therapy in Metastatic Breast Cancer Beyond HER2 Status: What We Have Learned from Clinical Specimens. Curr. Pharm. Pers. Med. 2012, 7, 263–274. [Google Scholar] [CrossRef]
- Tang, L.; Long, Z.; Zhao, N.; Feng, G.; Guo, X.; Yu, M. NES1/KLK10 promotes trastuzumab resistance via activation of PI3K/AKT signaling pathway in gastric cancer. J. Cell. Biochem. 2018, 119, 6398–6407. [Google Scholar] [CrossRef]
- Jin, M.H.; Nam, A.-R.; Park, J.E.; Bang, J.-H.; Bang, Y.-J.; Oh, D.-Y. Resistance Mechanism against Trastuzumab in HER2-Positive Cancer Cells and Its Negation by Src Inhibition. Mol. Cancer Ther. 2017, 16, 1145–1154. [Google Scholar] [CrossRef]
- Chen, Y.-C.; Li, H.-Y.; Liang, J.-L.; Ger, L.-P.; Chang, H.-T.; Hsiao, M.; Calkins, M.J.; Cheng, H.-C.; Lu, P.-J.; Lu, P.-J. CTMP, a predictive biomarker for trastuzumab resistance in HER2-enriched breast cancer patient. Oncotarget 2017, 8, 29699–29710. [Google Scholar] [CrossRef]
- Clark, A.S.; West, K.; Streicher, S.; Dennis, P.A. Constitutive and inducible Akt activity promotes resistance to chemotherapy, trastuzumab, or tamoxifen in breast cancer cells. Mol. Cancer Ther. 2002, 1, 707–717. [Google Scholar] [CrossRef]
- Zhang, X.; Sun, Q.; Shan, M.; Niu, M.; Liu, T.; Xia, B.; Liang, X.; Wei, W.; Sun, S.; Zhang, Y.; et al. Promoter Hypermethylation of ARID1A Gene Is Responsible for Its Low mRNA Expression in Many Invasive Breast Cancers. PLoS ONE 2013, 8, e0053931. [Google Scholar] [CrossRef]
- Wu, Y.; Gu, Y.; Guo, S.; Dai, Q.; Zhang, W. Expressing Status and Correlation of ARID1A and Histone H2B on Breast Cancer. BioMed Res. Int. 2016, 2016, 1–9. [Google Scholar] [CrossRef]
- Cao, Y.; Li, Y.; Edelweiss, M.; Arun, B.; Rosen, D.; Resetkova, E.; Wu, Y.; Liu, J.; Sahin, A.; Albarracin, C.T. Loss of annexin A1 expression in breast cancer progression. Appl. Immunohistochem. Mol. Morphol. 2008, 16, 530–534. [Google Scholar] [CrossRef]
| Antibody | Antigen Retrieval Method | Buffer | Dilution | Incubation Time | DAB (min) |
|---|---|---|---|---|---|
| ARID1A(sc-32761) Santa Cruz Biotechnology | Microwave | EDTA | 1:800 | Overnight at 4 °C | 10 |
| ANXA1 (713400) Invitrogen | Water bath | 1:1500 | 1 h at room temperature | 7 |
| Clinicopathological Features | Luminal B-Like (HER-2+) | HER-2+ (Non-Luminal) |
|---|---|---|
| Patients (n) | 167 | 48 |
| Age median (range) | 51 (24–71) | 54.5 (27–69) |
| Histological type (%) | ||
| Invasive Carcinoma, no special type (NST) | 128 (76.6) | 43 (89.6) |
| Invasive lobular carcinoma | 3 (1.8) | 1 (2.1) |
| Other invasive carcinoma subtypes a | 36 (21.7) | 4 (8.5) |
| Lymphovascular invasion (%) | ||
| No | 88 (52.7) | 20 (41.7) |
| Yes | 69 (41.3) | 25 (52.1) |
| Not determined | 10 (6) | 3 (6.7) |
| Grade (%) | ||
| G1 and G2 | 84 (50.3) | 13 (27.1) |
| G3 | 83 (49.7) | 34 (70.8) |
| Not determined | - | 1 (2.1) |
| Oestrogen Receptor Status (%) | ||
| Positive | 167 (100) | - |
| Negative | - | 48 (100) |
| Progesterone Receptor Status (%) | ||
| Positive | 128 (76.6) | - |
| Negative | 39 (23.4) | 48 (100) |
| Primary tumour (T) (%) | ||
| T1 & T2 | 152 (91) | 45 (93.8) |
| T3 & T4 | 13 (7.8) | 3 (6.3) |
| Not determined | 2 (1.2) | |
| Regional lymph node (N) (%) | ||
| N0 | 67 (40.1) | 18 (37.5) |
| N+ | 99 (59.3) | 30 (62.5) |
| Not determined | 1 (0.6) | - |
| Stage (%) | ||
| I/II | 121 (72.5) | 37 (77.1) |
| III | 45 (26.9) | 11 (22.9) |
| Not determined | 1 (0.6) | - |
| Breast Cancer Mortality | Variable | Hazard Ratio (HR) | 95% CI for HR | p-Value |
|---|---|---|---|---|
| Univariable | Stage | 2.415–10.268 | <0.001 | |
| I and II | 1 | |||
| III | 4.980 | |||
| ANXA1 | 1.259–5.189 | 0.009 | ||
| Negative | 1 | |||
| Positive | 2.557 | |||
| Multivariable | Stage | 2.374–10.093 | <0.001 | |
| I and II | 1 | |||
| III | 4.895 | |||
| ANXA1 | 1.309–5.393 | 0.008 | ||
| Negative | 1 | |||
| Positive | 2.658 |
| Relapse | Variable | Hazard Ratio (HR) | 95% CI for HR | p-Value |
|---|---|---|---|---|
| Univariable | Stage | 2.215–7.490 | <0.001 | |
| I and II | 1 | |||
| III | 4.073 | |||
| ANXA1 | 1.239–4.304 | 0.008 | ||
| Negative | 1 | |||
| Positive | 2.309 | |||
| Multivariable | Stage | 2.270–7.817 | <0.001 | |
| I and II | 1 | |||
| III | 4.213 | |||
| ANXA1 | 1.296–4.499 | 0.005 | ||
| Negative | 1 | |||
| Positive | 2.415 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Silva-Oliveira, R.; Pereira, F.F.; Petronilho, S.; Martins, A.T.; Lameirinhas, A.; Constâncio, V.; Caldas-Ribeiro, I.; Salta, S.; Lopes, P.; Antunes, L.; et al. Clinical Significance of ARID1A and ANXA1 in HER-2 Positive Breast Cancer. J. Clin. Med. 2020, 9, 3911. https://doi.org/10.3390/jcm9123911
Silva-Oliveira R, Pereira FF, Petronilho S, Martins AT, Lameirinhas A, Constâncio V, Caldas-Ribeiro I, Salta S, Lopes P, Antunes L, et al. Clinical Significance of ARID1A and ANXA1 in HER-2 Positive Breast Cancer. Journal of Clinical Medicine. 2020; 9(12):3911. https://doi.org/10.3390/jcm9123911
Chicago/Turabian StyleSilva-Oliveira, Rita, Filipa Ferreira Pereira, Sara Petronilho, Ana Teresa Martins, Ana Lameirinhas, Vera Constâncio, Inês Caldas-Ribeiro, Sofia Salta, Paula Lopes, Luís Antunes, and et al. 2020. "Clinical Significance of ARID1A and ANXA1 in HER-2 Positive Breast Cancer" Journal of Clinical Medicine 9, no. 12: 3911. https://doi.org/10.3390/jcm9123911
APA StyleSilva-Oliveira, R., Pereira, F. F., Petronilho, S., Martins, A. T., Lameirinhas, A., Constâncio, V., Caldas-Ribeiro, I., Salta, S., Lopes, P., Antunes, L., Castro, F., de Sousa, S. P., Henrique, R., & Jerónimo, C. (2020). Clinical Significance of ARID1A and ANXA1 in HER-2 Positive Breast Cancer. Journal of Clinical Medicine, 9(12), 3911. https://doi.org/10.3390/jcm9123911









