Photo-Realistic Interactive Virtual Environments for Neurorehabilitation in Mild Cognitive Impairment (NeuroVRehab.PT): A Participatory Design and Proof-of-Concept Study
Abstract
1. Introduction
2. Experimental Section
2.1. Participatory Design of NeuroVRehab.PT–Shopping Behaviors Questionnaire with Older Adults (Phase 1)
2.1.1. Sample and Recruitment
2.1.2. Instruments and Procedure
2.1.3. Data Analysis
2.1.4. Results
2.1.5. Main Implications for the Development of the NeuroVRehab.PT
2.2. Design and Implementation of the NeuroVRehab.PT (Phase 2)
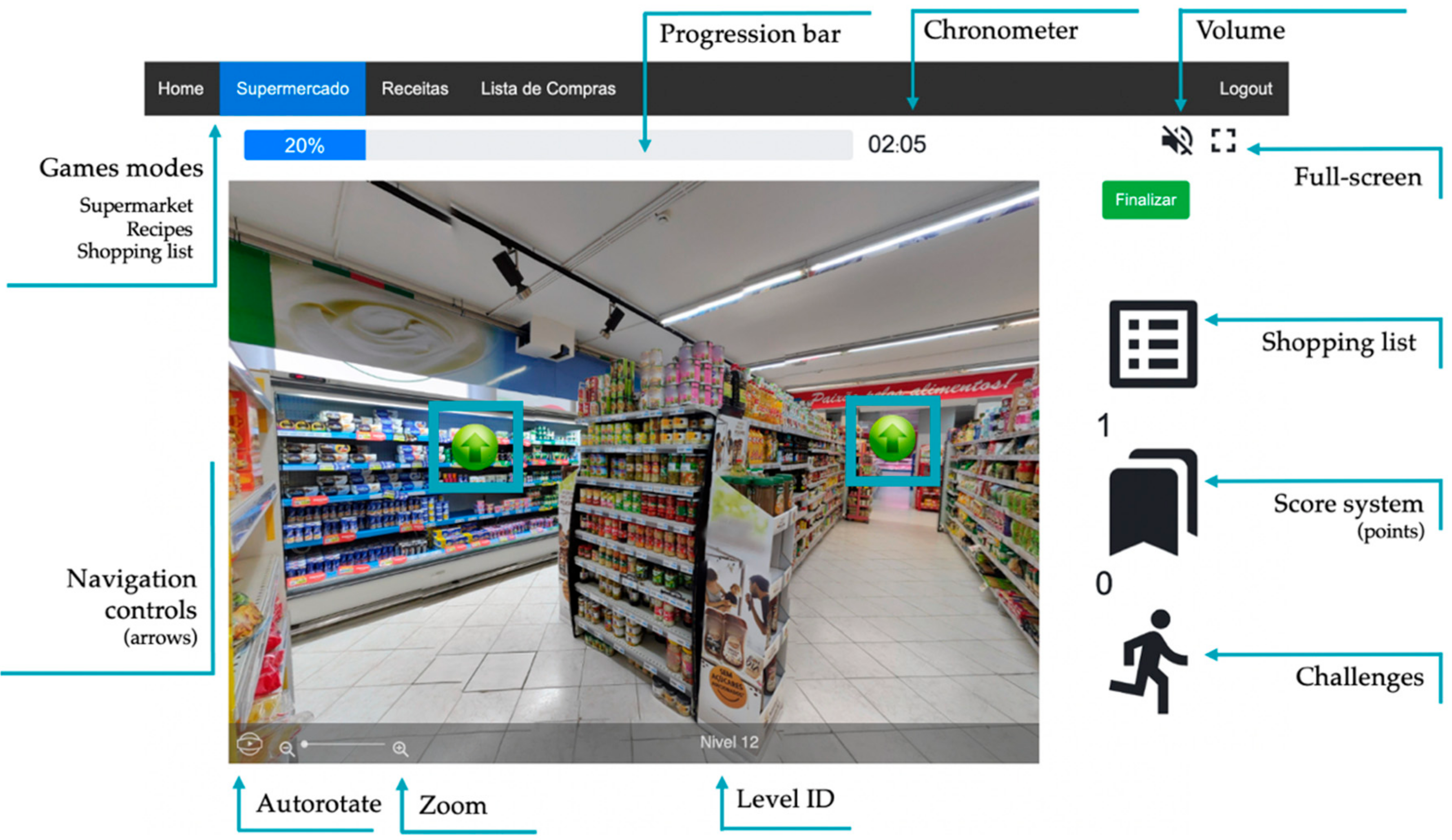
2.2.1. Platform Description
Supermarket Environment Description
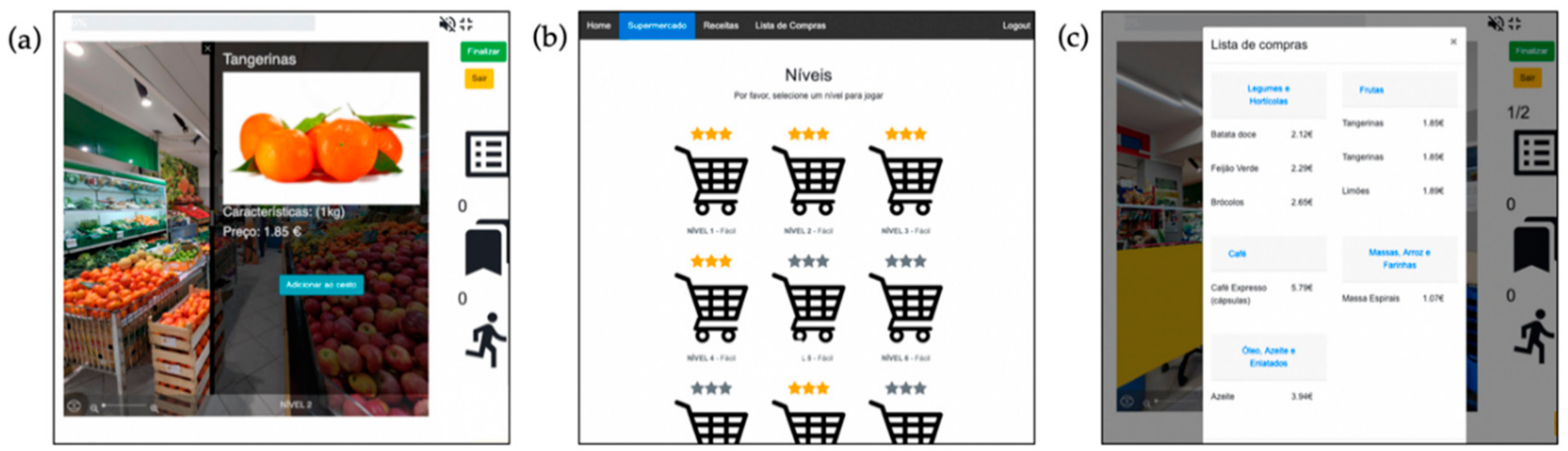
Supermarket Game Mode
Recipe Game Mode
Shopping List Game Mode
2.3. Software Evaluation and User Experience (Phase 3)
2.3.1. Sample and Recruitment
2.3.2. Instruments and Procedure
2.3.3. Data Analysis
3. Results
3.1. Experience with NeuroVRehab.PT
3.1.1. Hedonic Experience and Presence
Participant 1: “I was expecting something more, rudimentary, but not the case, I think it was… the products were clear and colors vivid…”Participant 2: “Well, it is a very appealing image of the supermarket. It makes you want to explore it, doesn’t it? It has beautiful fruits.”Participant 4: “Ah! How cute (…) it really looks like a supermarket (…), maybe this is really a supermarket (…) The products are real, not drawings [as in 3D-modulated scenarios], I think it is good.”Participant 5: “[While performing a task in NeuroVRehab.PT] Ok, hot chocolate. Hot chocolate, now I have to find…. this is really realistic. In fact, it is real, I did not have this expectation.”Participant 6: “It seems very realistic, hyper-realistic.” (line 51) “The locations, the type of products, yes, yes, I think is quite realistic.”Participant 7: “The environment sound is very good; it really puts you inside of a supermarket (…) we know where we are, perfectly.”
3.1.2. Usability
Participant 2: “The arrow appears, I assume this means I need to follow the arrows.”Participant 1: “… the arrow then… means that I need to go back to the fruit section?”
Participant 5: “The arrow helps to orient, doesn’t it? I did not understand if the arrow gives you a hint or if … Does it give you a hint?”
3.2. Rehabilitation Potential
Participant 5: “[regarding another virtual supermarket for IADL rehabilitation] (…) it was prehistoric when compared to this one.”Participant 2 “… a good alternative for cognitive stimulation.”
3.2.1. Cognitive Stimulation
Participant 5 “… working memory, of course, always pumping in my head (…) Manifestly, this also trains orientation….”. […] From an attentional point of view, it is quite demanding”.
Participant 7: “[regarding other CCTP] I think there is not an effort or an intent to be similar to the person’s daily life. Here I notice that effort (…) and that could be more motivating for the person who is doing the training”.
3.2.2. Transfer Capacity
Participant 2: “It has to make much sense [to the patient] to have any impact or transfer to real life. And even with this software, it is either something that meets what the previous life of the person was, and it has any meaning to him/her, or it ends up [just] being an interesting game…”.
3.3. Potential Barriers
Participant 7: “I believe they [the patients] will have some doubts (…) I had someone by my side to explain it to me, and they do not have it”.Participant 3: “I think in some cases, some patients can easily start to get frustrated. And it is advisable not to continue. And I think there will be some situations like that, which is perfectly normal with this type of activity. Therefore, it is necessary to have resources [as therapists] (…) to be you to finish the activity and help the patient to move on …”
3.4. Opportunities
3.4.1. Clinical and Non-Clinical Contexts
3.4.2. Friend Sourcing
3.4.3. Other Environments
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Petersen, R.; Doody, R.; Kurz, A.; Mohs, R.; Morris, J.; Rabins, P.; Ritchie, K.; Rossor, M.; Thal, L.; Winblad, B. Current concepts in Mild Cognitive Impairment. Arch. Neurol. 2001, 58, 1985–1992. [Google Scholar] [CrossRef]
- Tuokko, H.; Morris, C.; Ebert, P. Mild Cognitive Impairment and everyday functioning in older adults. Neurocase 2005, 11, 40–47. [Google Scholar] [CrossRef] [PubMed]
- Jekel, K.; Damian, M.; Wattmo, C.; Hausner, L.; Bullock, R.; Connelly, P.J.; Dubois, B.; Eriksdotter, M.; Ewers, M.; Graessel, E.; et al. Mild Cognitive Impairment and deficits in instrumental activities of daily living: A systematic review. Alzheimer’s Res. Ther. 2015, 7. [Google Scholar] [CrossRef] [PubMed]
- O’Brien, J.T.; Erkinjuntti, T.; Reisberg, B.; Roman, G.; Sawada, T.; Pantoni, L.; Bowler, J.V.; Ballard, C.; DeCarli, C.; Gorelick, P.B.; et al. Vascular cognitive impairment. Lancet Neurol. 2003, 2, 89–98. [Google Scholar] [CrossRef]
- Gorelick, P.B.; Scuteri, A.; Black, S.E.; Decarli, C.; Greenberg, S.M.; Iadecola, C.; Launer, L.J.; Laurent, S.; Lopez, O.L.; Nyenhuis, D.; et al. Vascular contributions to cognitive impairment and dementia: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2011, 42, 2672–2713. [Google Scholar] [CrossRef]
- Pérès, K.; Chrysostome, V.; Fabrigoule, C.; Orgogozo, J.M.; Dartigues, J.F.; Barberger-Gateau, P. Restriction in complex activities of daily living in MCI: Impact on outcome. Neurology 2006, 67, 461–466. [Google Scholar] [CrossRef]
- Freeman, D.; Reeve, S.; Robinson, A.; Ehlers, A.; Clark, D.; Spanlang, B.; Slater, M. Virtual reality in the assessment, understanding, and treatment of mental health disorders. Psychol. Med. 2017, 47, 2393–2400. [Google Scholar] [CrossRef]
- Parsons, T.; Carlew, A.; Magtoto, J.; Stonecipher, K. The potential of function-led virtual environments for ecologically valid measures of executive function in experimental and clinical neuropsychology. Neuropsychol. Rehabil. 2015, 1–31. [Google Scholar] [CrossRef]
- Bombín-González, I.; Cifuentes-Rodríguez, A.; Climent-Martínez, G.; Luna-Lario, P.; Cardas-Iáñez, J.; Tirapu-Ustárroz, J.; Díaz-Orueta, U. Validez ecológica y entornos multitarea en la evaluación de las funciones ejecutivas. Rev. Neurol. 2014, 59, 77–87. [Google Scholar] [CrossRef]
- Jansari, A.S.; Devlin, A.; Agnew, R.; Akesson, K.; Murphy, L.; Leadbetter, T. Ecological assessment of executive functions: A new virtual reality paradigm. Brain Impair. 2014, 15, 71–87. [Google Scholar] [CrossRef]
- Tarnanas, I.; Schlee, W.; Tsolaki, M.; Müri, R.; Mosimann, U.; Nef, T. Ecological validity of virtual reality daily living activities screening for early dementia: Longitudinal study. JMIR Serious Games 2013, 1, e1. [Google Scholar] [CrossRef] [PubMed]
- Renison, B.; Ponsford, J.; Testa, R.; Richardson, B.; Brownfield, K. The ecological and construct validity of a newly developed measure of executive function: The Virtual Library Task. J. Int. Neuropsychol. Soc. 2012, 18, 440–450. [Google Scholar] [CrossRef] [PubMed]
- Manera, V.; Petit, P.D.; Derreumaux, A.; Orvieto, I.; Romagnoli, M.; Lyttle, G.; David, R.; Robert, P. “Kitchen and cooking”, a serious game for Mild Cognitive Impairment and Alzheimer’s disease: A pilot study. Front. Aging Neurosci. 2015, 7, 1–10. [Google Scholar] [CrossRef]
- Klinger, E.; Cao, X.; Douguet, A.S.; Fuchs, P. Designing an ecological and adaptable virtual task in the context of executive functions. Annu. Rev. CyberTherapy Telemed. 2009, 7, 248–252. [Google Scholar] [CrossRef]
- Foreman, N.; Stanton-Fraser, D.; Wilson, P.N.; Duffy, H.; Parnell, R. Transfer of spatial knowledge to a two-level shopping mall in older people, following virtual exploration. Environ. Behav. 2005, 37, 275–292. [Google Scholar] [CrossRef]
- Gamito, P.; Oliveira, J.; Alghazzawi, D.; Fardoun, H.; Rosa, P.; Sousa, T.; Maia, I.; Morais, D.; Lopes, P.; Brito, R. The Art Gallery Test: A preliminary comparison between traditional neuropsychological and ecological VR-based tests. Front. Psychol. 2017, 8, 1–8. [Google Scholar] [CrossRef]
- Gamito, P.; Oliveira, J.; Morais, D.; Coelho, C.; Santos, N.; Alves, C.; Galamba, A.; Soeiro, M.; Yerra, M.; French, H.; et al. Cognitive stimulation of elderly individuals with instrumental virtual reality-based activities of daily life: Pre-post treatment study. Cyberpsychol. Behav. Soc. Netw. 2019, 22, 69–75. [Google Scholar] [CrossRef]
- Oliveira, J.; Gamito, P.; Alghazzawi, D.M.; Fardoun, H.M.; Rosa, P.J.; Sousa, T.; Picareli, L.F.; Morais, D.; Lopes, P. Performance on naturalistic virtual reality tasks depends on global cognitive functioning as assessed via traditional neurocognitive tests. Appl. Neuropsychol. Adult 2018, 25, 555–561. [Google Scholar] [CrossRef]
- Man, D.W.K.; Chung, J.C.C.; Lee, G.Y.Y. Evaluation of a virtual reality-based memory training programme for Hong Kong Chinese older adults with questionable dementia: A pilot study. Int. J. Geriatr. Psychiatry 2012, 27, 513–520. [Google Scholar] [CrossRef]
- Cabinio, M.; Rossetto, F.; Isernia, S.; Saibene, F.L.; Di Cesare, M.; Borgnis, F.; Pazzi, S.; Migliazza, T.; Alberoni, M.; Blasi, V.; et al. The use of a virtual reality platform for the assessment of the memory decline and the hippocampal neural injury in subjects with Mild Cognitive Impairment: The validity of smart aging serious game (SASG). J. Clin. Med. 2020, 9, 1355. [Google Scholar] [CrossRef]
- Aubin, G.; Beliveau, M.-F.; Klinger, E. An exploration of the ecological validity of the Virtual Action Planning-Supermarket (VAP-S) with people with schizophrenia. Neuropsychol. Rehabil. 2018, 28, 689–708. [Google Scholar] [CrossRef] [PubMed]
- Kizony, R.; Korman, M.; Sinoff, G.; Klinger, E.; Josman, N. Using a virtual supermarket as a tool for training executive functions in people with Mild Cognitive Impairment. In Proceedings of the 9th International Conference Disability, Virtual Reality & Associated Technologies, Reading, UK, 10–12 September 2012; pp. 41–46. [Google Scholar]
- Josman, N.; Kizony, R.; Hof, E.; Goldenberg, K.; Weiss, P.L.; Klinger, E. Using the virtual action planning-supermarket for evaluating executive functions in people with stroke. J. Stroke Cerebrovasc. Dis. 2013, 23, 879–887. [Google Scholar] [CrossRef] [PubMed]
- Zygouris, S.; Giakoumis, D.; Votis, K.; Doumpoulakis, S.; Ntovas, K.; Segkouli, S.; Karagiannidis, C.; Tzovaras, D.; Tsolaki, M. Can a virtual reality cognitive training application fulfill a dual role? Using the virtual supermarket cognitive training application as a screening tool for Mild Cognitive Impairment. J. Alzheimer’s Dis. 2015, 44, 1333–1347. [Google Scholar] [CrossRef] [PubMed]
- Erez, N.; Weiss, P.L.; Kizony, R.; Rand, D. Comparing performance within a virtual supermarket of children with traumatic brain injury to typically developing children: A pilot study. OTJR Occup. Particip. Health 2013, 33, 218–227. [Google Scholar] [CrossRef]
- Rand, D.; Rukan, S.B.A.; Weiss, P.L.; Katz, N. Validation of the Virtual MET as an assessment tool for executive functions. Neuropsychol. Rehabil. 2009, 19, 583–602. [Google Scholar] [CrossRef]
- Rand, D.; Katz, N.; Weiss, P.L. Evaluation of virtual shopping in the VMALL: Comparison of post-stroke participants to healthy control groups. Disabil. Rehabil. 2007, 29, 1710–1719. [Google Scholar] [CrossRef]
- Benoit, M.; Guerchouche, R.; Petit, P.D.; Chapoulie, E.; Manera, V.; Chaurasia, G.; Drettakis, G.; Robert, P. Is it possible to use highly realistic virtual reality in the elderly? A feasibility study with image-based rendering. Neuropsychiatr. Dis. Treat. 2015, 11, 557–563. [Google Scholar] [CrossRef]
- Tieri, G.; Morone, G.; Paolucci, S.; Iosa, M. Virtual reality in cognitive and motor rehabilitation: Facts, fiction and fallacies. Expert Rev. Med. Devices 2018, 1–11. [Google Scholar] [CrossRef]
- Manera, V.; Chapoulie, E.; Bourgeois, J.; Guerchouche, R.; David, R.; Ondrej, J.; Drettakis, G.; Robert, P. A feasibility study with image-based rendered virtual reality in patients with Mild Cognitive Impairment and dementia. PLoS ONE 2016, 11, e0151487. [Google Scholar] [CrossRef]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef]
- Bahar-Fuchs, A.; Martyr, A.; Goh, A.; Sabates, J.; Clare, L. Cognitive training for people with mild to moderate dementia. Cochrane Database Syst. Rev. 2019, 2019. [Google Scholar] [CrossRef]
- Bahar-Fuchs, A.; Clare, L.; Woods, B. Cognitive training and cognitive rehabilitation for persons with mild to moderate dementia of the Alzheimer’s or vascular type: A review. Alzheimer’s Res. Ther. 2013, 5. [Google Scholar] [CrossRef]
- Li, H.; Li, J.; Li, N.; Li, B.; Wang, P.; Zhou, T. Cognitive intervention for persons with Mild Cognitive Impairment: A meta-analysis. Ageing Res. Rev. 2011, 10, 285–296. [Google Scholar] [CrossRef] [PubMed]
- Sohlberg, M.M.; Mateer, C.A. Cognitive Rehabilitation: An Integrative Neuropsychological Approach; Guilford Press: New York, NY, USA, 2001; ISBN 9781572306134. [Google Scholar]
- HTML 5.2. Available online: https://www.w3.org/TR/html52/ (accessed on 24 November 2020).
- ECMAScript® 2019 Language Specification. Available online: https://www.ecma-international.org/ecma-262/10.0/index.html (accessed on 24 November 2020).
- Cascading Style Sheets. Available online: https://www.w3.org/Style/CSS/ (accessed on 24 November 2020).
- PHP: Hypertext Preprocessor. Available online: https://www.php.net/ (accessed on 24 November 2020).
- Photo Sphere Viewer. Available online: https://photo-sphere-viewer.js.org/ (accessed on 24 November 2020).
- Blendinger, K. Tablet-Applications for the Elderly: Specific Usability Guidelines; Ulm University: Ulm, Germany, 2015. [Google Scholar]
- Canini, M.; Battista, P.; Della Rosa, P.A.; Catricalà, E.; Salvatore, C.; Gilardi, M.C.; Castiglioni, I. Computerized neuropsychological assessment in aging: Testing efficacy and clinical ecology of different interfaces. Comput. Math. Methods Med. 2014, 2014. [Google Scholar] [CrossRef] [PubMed]
- Shneiderman, B. Touchscreens now offer compelling uses. IEEE Softw. 1991, 8, 93–94. [Google Scholar] [CrossRef]
- Delello, J.A.; McWhorter, R.R. Reducing the digital divide: Connecting older adults to iPad technology. J. Appl. Gerontol. 2015, 1–26. [Google Scholar] [CrossRef]
- Astell, A.J.; Joddrell, P.; Groenewoud, H.; de Lange, J.; Goumans, M.; Cordia, A.; Schikhof, Y. Does familiarity affect the enjoyment of touchscreen games for people with dementia? Int. J. Med. Inform. 2016, 91, e1–e8. [Google Scholar] [CrossRef]
- Alves, S.; Brito, F.; Cordeiro, A.; Carriço, L.; Guerreiro, T. Designing personalized therapy tools for people with dementia. In Proceedings of the 16th Web For All 2019 Personalization-Personalizing the Web, San Francisco, CA, USA, 13–14 May 2019. [Google Scholar] [CrossRef]
- Someren, M.; Barnard, Y.F.; Sandberg, J. The Think Aloud Method: A Practical Guide to Modelling Cognitive Processes; Van Someren, M.W., Barnard, Y.F., Barnard, J.A.C., Eds.; Academic Press: London, UK, 1994; ISBN 0127142703. [Google Scholar]
- McHugh, M.L. Lessons in biostatistics interrater reliability: The kappa statistic. Biochem. Med. 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using thematic analysis in psychology. Qual. Res. Psychol. 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Schultz, D.; Schultz, S.E. Rats, ants, and the animal mind. In A History of Modern Psychology; Wadsworth Cengage Learning: Boston, MA, USA, 2011; pp. 193–195. ISBN 5856420187. [Google Scholar]
- Josman, N.; Hof, E.; Klinger, E.; Marié, R.M.; Goldenberg, K.; Weiss, P.L.; Kizony, R. Performance within a virtual supermarket and its relationship to executive functions in post-stroke patients. In Proceedings of the 2006 International Workshop on Virtual Rehabilitation, New York, NY, USA, 29–30 August 2006; pp. 106–109. [Google Scholar] [CrossRef]
- Werner, P.; Rabinowitz, S.; Klinger, E.; Korczyn, A.D.; Josman, N. Use of the virtual action planning supermarket for the diagnosis of Mild Cognitive Impairment. Dement. Geriatr. Cogn. Disord. 2009, 27, 301–309. [Google Scholar] [CrossRef]
- Chaytor, N.; Schmitter-Edgecombe, M. The ecological validity of neuropsychological tests: A review of the literature on everyday cognitive skills. Neuropsychol. Rev. 2003, 13, 181–197. [Google Scholar] [CrossRef] [PubMed]
- Spooner, D.M.; Pachana, N.A. Ecological validity in neuropsychological assessment: A case for greater consideration in research with neurologically intact populations. Arch. Clin. Neuropsychol. 2006, 21, 327–337. [Google Scholar] [CrossRef] [PubMed]
- Deterding, S.; Dixon, D.; Khaled, R.; Nacke, L. From Game Design Elements to Gamefulness: Defining “Gamification”. In Proceedings of the MindTrek’11, Tampere, Filand, 28–30 September 2011; pp. 28–30. [Google Scholar]
- Deterding, S.; Dixon, D.; Khaled, R.; Nacke, L.; Sicart, M.; O’Hara, K. Gamification: Using game design elements in non-game contexts. In Proceedings of the 2011 Annual Conference Extended Abstracts on Human Factors in Computing Systems (CHI 2011), Vancouver, BC, Canada, 7–12 May 2011; pp. 2425–2428. [Google Scholar] [CrossRef]
- Lumsden, J.; Edwards, E.A.; Lawrence, N.S.; Coyle, D.; Munafò, M.R. Gamification of Cognitive Assessment and Cognitive Training: A Systematic Review of Applications and Efficacy. JMIR Serious Games 2016, 4, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Sardi, L.; Idri, A.; Fernández-Alemán, J.L. A systematic review of gamification in e-Health. J. Biomed. Inform. 2017, 71, 31–48. [Google Scholar] [CrossRef]
- Ferreira-Brito, F.; Fialho, M.; Virgolino, A.; Neves, I.; Miranda, A.C.; Sousa-Santos, N.; Caneiras, C.; Carriço, L.; Verdelho, A.; Santos, O. Game-based interventions for neuropsychological assessment, training and rehabilitation: Which game-elements to use? A systematic review. J. Biomed. Inform. 2019, 98, 103287. [Google Scholar] [CrossRef]
- Sailer, M.; Hense, J.U.; Mayr, S.K.; Mandl, H. How gamification motivates: An experimental study of the effects of specific game design elements on psychological need satisfaction. Comput. Hum. Behav. 2017, 69, 371–380. [Google Scholar] [CrossRef]
- Simons, D.J.; Boot, W.R.; Charness, N.; Gathercole, S.E.; Chabris, C.F.; Hambrick, D.Z.; Stine-Morrow, E.A.L. Do “Brain-Training” programs work? Psychol. Sci. Public Interest Suppl. 2016, 17, 103–186. [Google Scholar] [CrossRef]
- Zhang, H.; Huntley, J.; Bhome, R.; Holmes, B.; Cahill, J.; Gould, R.L.; Wang, H.; Yu, X.; Howard, R. Effect of computerised cognitive training on cognitive outcomes in Mild Cognitive Impairment: A systematic review and meta-analysis. BMJ Open 2019, 9. [Google Scholar] [CrossRef]
- Clare, L.; Woods, B. Cognitive rehabilitation and cognitive training for early-stage Alzheimer’s disease and vascular dementia. Cochrane Database Syst. Rev. 2003, 4. [Google Scholar] [CrossRef]
- De Giglio, L.; De Luca, F.; Prosperini, L.; Borriello, G.; Bianchi, V.; Pantano, P.; Pozzilli, C. A low-cost cognitive rehabilitation with a commercial video game improves sustained attention and executive functions in multiple sclerosis: A pilot study. Neurorehabil. Neural Repair 2015, 29, 453–461. [Google Scholar] [CrossRef]
- Nouchi, R.; Taki, Y.; Takeuchi, H.; Hashizume, H.; Nozawa, T.; Kambara, T.; Sekiguchi, A.; Miyauchi, C.M.; Kotozaki, Y.; Nouchi, H.; et al. Brain training game boosts executive functions, working memory and processing speed in the young adults: A randomized controlled trial. PLoS ONE 2013, 8, e55518. [Google Scholar] [CrossRef] [PubMed]
- López-Martín, O.; Fragoso, A.S.; Hernández, M.R.; Terrer, I.D.; Polonio López, B. Efectividad de un programa de juego basado en realidad virtual para la mejora cognitiva en la esquizofrenia. Gac. Sanit. 2016, 30, 133–136. [Google Scholar] [CrossRef] [PubMed]
- Levine, B.; Robertson, I.H.; Clare, L.; Carter, G.; Hong, J.; Wilson, B.A.; Duncan, J.; Stuss, D.T. Rehabilitation of executive functioning: An experimental-clinical validation of goal management training. J. Int. Neuropsychol. Soc. 2000, 6, 299–312. [Google Scholar] [CrossRef] [PubMed]
- Londos, E.; Boschian, K.; Lindén, A.; Persson, C.; Minthon, L.; Lexell, J. Effects of a Goal-Oriented Rehabilitation program in Mild Cognitive Impairment: A pilot study. Am. J. Alzheimer’s Dis. Other Dement. 2008, 23, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Clare, L.; van Paasschen, J.; Evans, S.J.; Parkinson, C.; Woods, R.T.; Linden, D.E.J. Goal-oriented cognitive rehabilitation for an individual with Mild Cognitive Impairment: Behavioural and neuroimaging outcomes. Neurocase 2009, 15, 318–331. [Google Scholar] [CrossRef] [PubMed]
- Wilson, B.A. Memory Rehabilitation: Integrating Theory and Practice; The Guilford Prss: New York, NY, USA, 2009; Volume 25, ISBN 9781606232873. [Google Scholar]
- De Schutter, B.; Vanden Abeele, V. Designing meaningful play within the psycho-social context of older adults. In Proceedings of the 3rd International Conference on Fun and Games, Leuven, Belgium, 15–17 September 2010; pp. 84–93. [Google Scholar] [CrossRef]
- Barrett, M.; Chua, W.-J.; Crits-Christoph, P.; Gibbons, M.B.; Casiano, D.; Thompson, D. Early withdrawal from mental health treatment: Implications for psychoterapy pratice. Psychotherapy 2008, 45, 247–267. [Google Scholar] [CrossRef] [PubMed]
- Martin, D.J.; Garske, J.P.; Katherine Davis, M. Relation of the therapeutic alliance with outcome and other variables: A meta-analytic review. J. Consult. Clin. Psychol. 2000, 68, 438–450. [Google Scholar] [CrossRef]
- Roos, J.; Werbart, A. Therapist and relationship factors influencing dropout from individual psychotherapy: A literature review. Psychother. Res. 2013, 23, 394–418. [Google Scholar] [CrossRef]
- Werbart, A.; Wang, M. Predictors of not starting and dropping out from psychotherapy in Swedish public service settings. Nord. Psychol. 2012, 64, 128–146. [Google Scholar] [CrossRef]
- Martin, L.; Williams, S.L.; Haskard, K.; DiMatteo, M.R. The challenge of patient adherence. Ther. Clin. Risk Manag. 2005, 1, 189–199. [Google Scholar] [CrossRef]
- Vygotsky, L.S. Interaction between learning and development. In Mind and Society; Harvard University Press: Cambridge, MA, USA, 1978; pp. 79–91. ISBN 9780674576292. [Google Scholar]
- Barnard, Y.; Bradley, M.D.; Hodgson, F.; Lloyd, A.D. Learning to use new technologies by older adults: Perceived difficulties, experimentation behaviour and usability. Comput. Hum. Behav. 2013, 29, 1715–1724. [Google Scholar] [CrossRef]
- WHO. Monitoring and Evaluating Digital Health Interventions. A Pratical Guide to Conducting Research and Assessment; WHO: Geneva, Switzerland, 2016; ISBN 9789241511766. [Google Scholar]

|
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ferreira-Brito, F.; Alves, S.; Santos, O.; Guerreiro, T.; Caneiras, C.; Carriço, L.; Verdelho, A. Photo-Realistic Interactive Virtual Environments for Neurorehabilitation in Mild Cognitive Impairment (NeuroVRehab.PT): A Participatory Design and Proof-of-Concept Study. J. Clin. Med. 2020, 9, 3821. https://doi.org/10.3390/jcm9123821
Ferreira-Brito F, Alves S, Santos O, Guerreiro T, Caneiras C, Carriço L, Verdelho A. Photo-Realistic Interactive Virtual Environments for Neurorehabilitation in Mild Cognitive Impairment (NeuroVRehab.PT): A Participatory Design and Proof-of-Concept Study. Journal of Clinical Medicine. 2020; 9(12):3821. https://doi.org/10.3390/jcm9123821
Chicago/Turabian StyleFerreira-Brito, Filipa, Sérgio Alves, Osvaldo Santos, Tiago Guerreiro, Cátia Caneiras, Luís Carriço, and Ana Verdelho. 2020. "Photo-Realistic Interactive Virtual Environments for Neurorehabilitation in Mild Cognitive Impairment (NeuroVRehab.PT): A Participatory Design and Proof-of-Concept Study" Journal of Clinical Medicine 9, no. 12: 3821. https://doi.org/10.3390/jcm9123821
APA StyleFerreira-Brito, F., Alves, S., Santos, O., Guerreiro, T., Caneiras, C., Carriço, L., & Verdelho, A. (2020). Photo-Realistic Interactive Virtual Environments for Neurorehabilitation in Mild Cognitive Impairment (NeuroVRehab.PT): A Participatory Design and Proof-of-Concept Study. Journal of Clinical Medicine, 9(12), 3821. https://doi.org/10.3390/jcm9123821








