The Characteristics of the Favard E4 Glenoid Morphology in Cuff Tear Arthropathy: A CT Study
Abstract
1. Introduction
2. Methods
2.1. Study Cohort
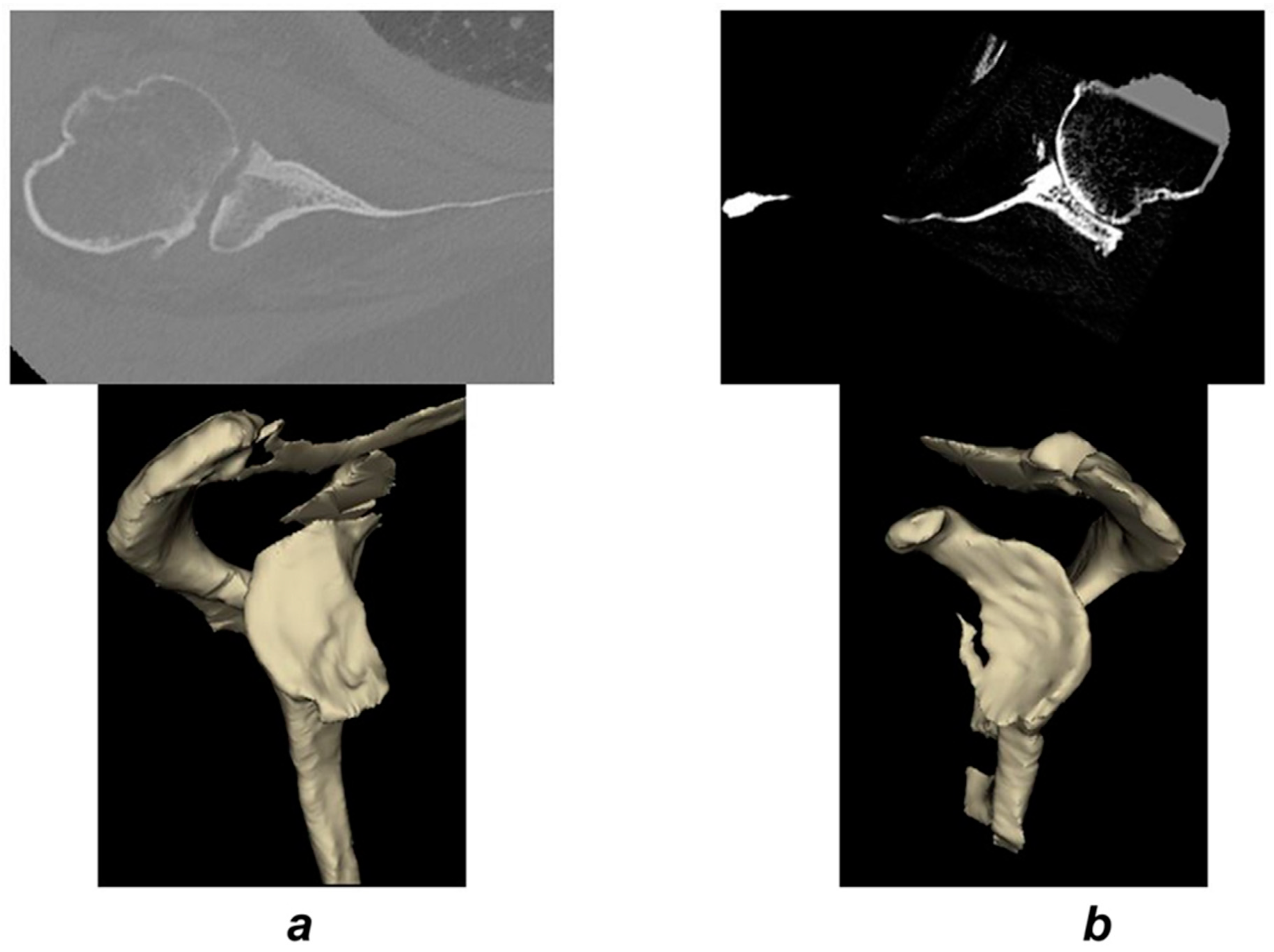
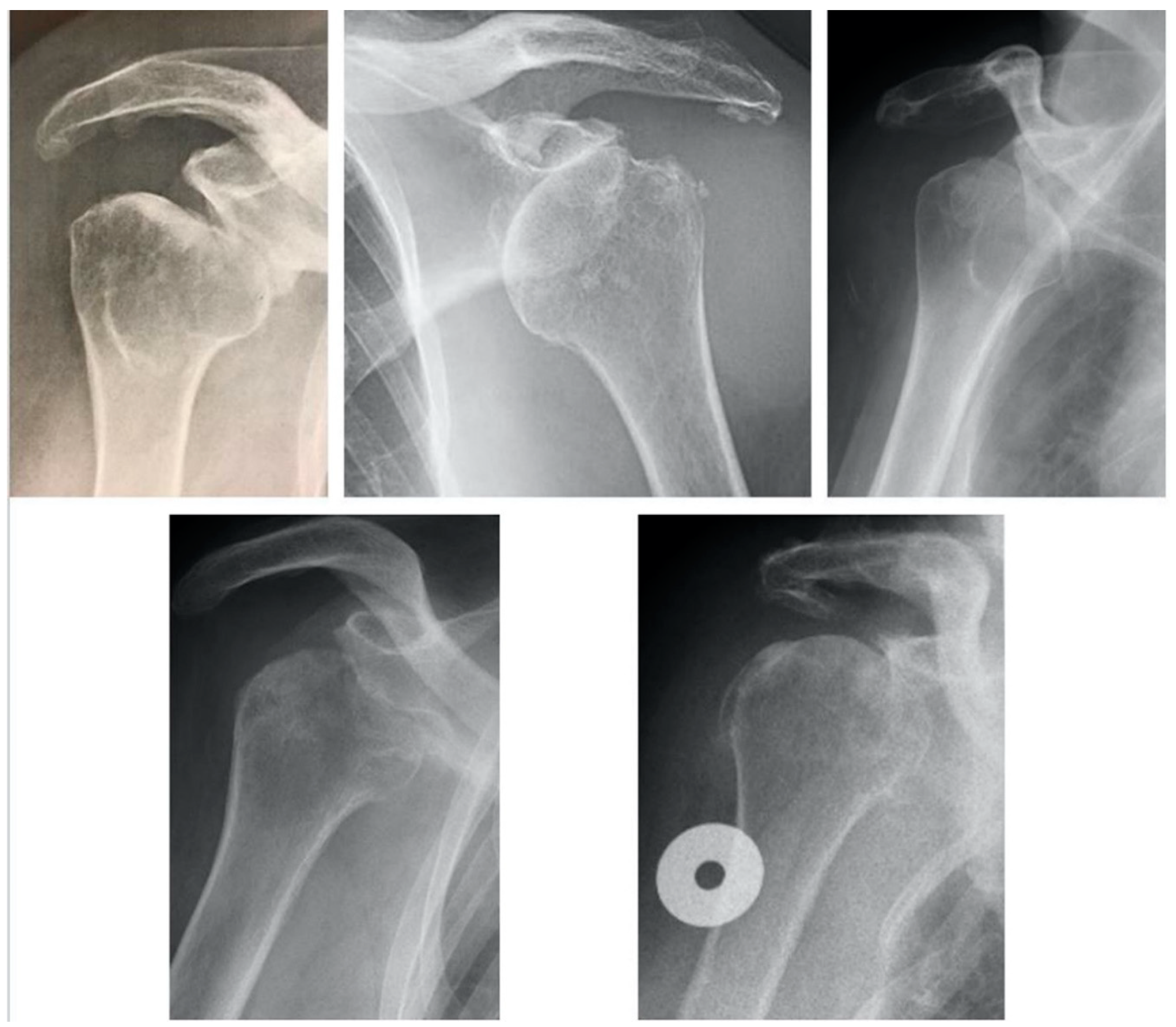
2.2. Imaging Analysis
2.3. Statistics
3. Results
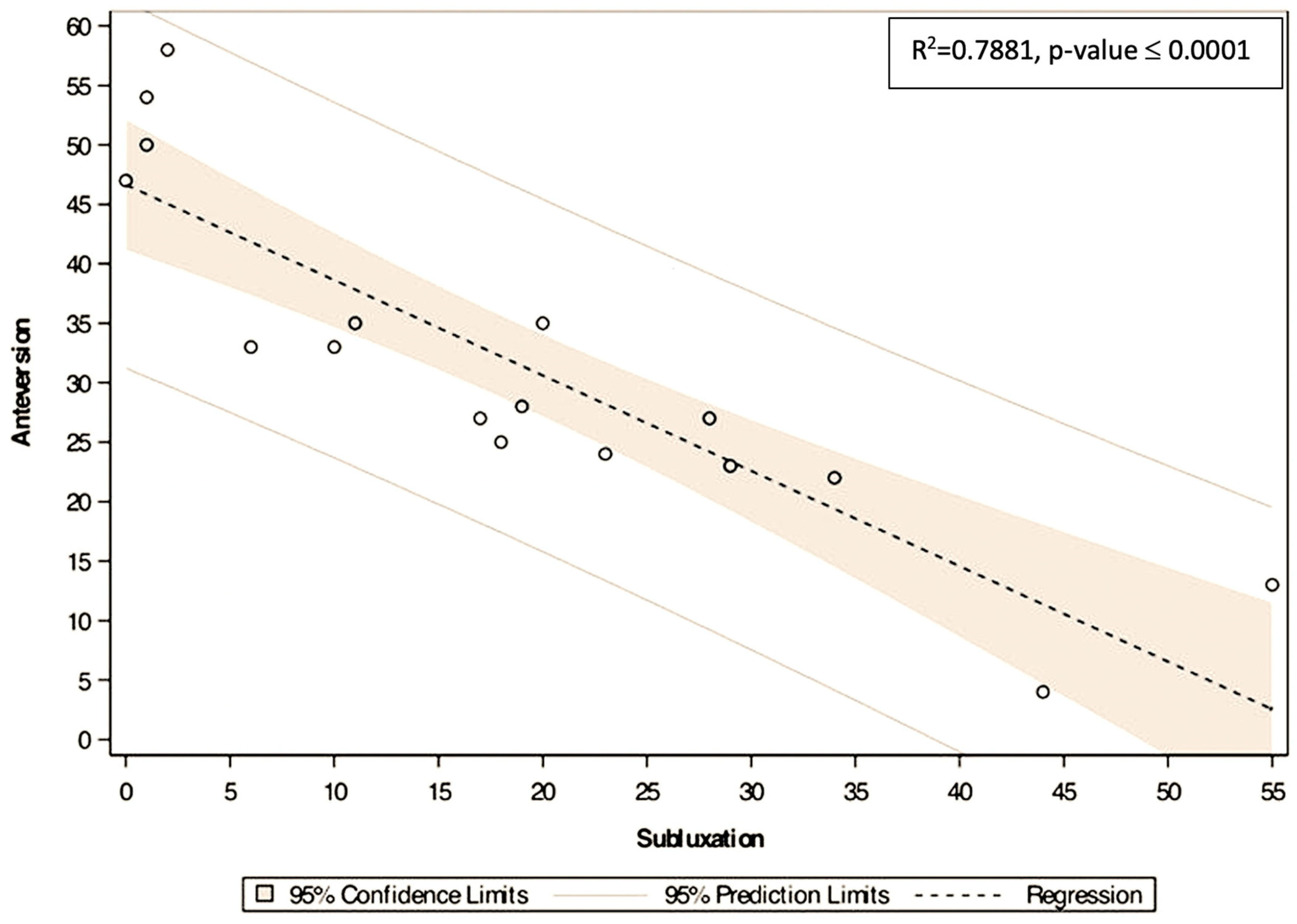
Correlations
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Favard, L.; Lautmann, S.; Sirveaux, F.; Oudet, D.; Kerjean, Y.; Huguet, D. Hemiarthroplasty versus reverse arthroplasty in the treatment of osteoarthritis with massive rotator cuff tear. In 2000 Shoulder Prostheses. Two to Ten Years Follow-Up; Walch, G., Boileau, P., Molé, D., Eds.; Sauramps Medical: Paris, France, 2001; pp. 261–268. [Google Scholar]
- Sirveaux, F.; Favard, L.; Oudet, D.; Huquet, D.; Walch, G.; Molé, D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J. Bone Jt. Surg. Br. 2004, 86, 388–395. [Google Scholar] [CrossRef] [PubMed]
- Lévigne, C.; Garret, J.; Boileau, P.; Alami, G.; Favard, L.; Walch, G. Scapular notching in reverse shoulder arthroplasty: Is it important to avoid it and how? Clin. Orthop. 2011, 469, 2512–2520. [Google Scholar] [CrossRef]
- Badet, R.; Walch, G.; Boulahia, A. Computed tomography in primary glenohumeral osteoarthritis without humeral head elevation. Rev. Rhum. Engl. Ed. 1998, 65, 187–194. [Google Scholar] [PubMed]
- Gerber, C.; Costouros, J.G.; Sukthankar, A.; Fucentese, S.F. Static posterior humeral head subluxation and total shoulder arthroplasty. J. Shoulder Elb. Surg. 2009, 18, 505–510. [Google Scholar] [CrossRef] [PubMed]
- Jacxsens, M.; Karns, M.R.; Henninger, H.B.; Drew, A.J.; Van Tongel, A.; De Wilde, L. Guidelines for humeral subluxation cutoff values: A comparative study between conventional, reoriented, and three-dimensional computed tomography scans of healthy shoulders. J. Shoulder Elb. Surg. 2018, 27, 36–43. [Google Scholar] [CrossRef] [PubMed]
- Jacxsens, M.; Van Tongel, A.; Henninger, H.B.; De Coninck, B.; Mueller, A.M.; De Wilde, L. A three-dimensional comparative study on the scapulohumeral relationship in normal and osteoarthritic shoulders. J. Shoulder Elb. Surg. 2016, 25, 1607–1615. [Google Scholar] [CrossRef]
- Papilion, J.A.; Shall, L.M. Fluoroscopic evaluation for subtle shoulder instability. Am. J. Sports Med. 1992, 20, 548–552. [Google Scholar] [CrossRef] [PubMed]
- Walch, G.; Ascani, C.; Boulahia, A.; Nové-Josserand, L.; Edwards, T.B. Static posterior subluxation of the humeral head: An unrecognized entity responsible for glenohumeral osteoarthritis in the young adult. J. Shoulder Elb. Surg. 2002, 11, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Walch, G.; Boulahia, A.; Boileau, P.; Kempf, J.F. Primary glenohumeral osteoarthritis: Clinical and radiographic classification. The Aequalis Group. Acta Orthop. Belg. 1998, 64 (Suppl. 2), 46–52. [Google Scholar] [PubMed]
- Boileau, P.; Cheval, D.; Gauci, M.-O.; Holzer, N.; Chaoui, J.; Walch, G. Automated Three-Dimensional Measurement of Glenoid Version and Inclination in Arthritic Shoulders. J. Bone Jt. Surg. Am. 2018, 100, 57–65. [Google Scholar] [CrossRef] [PubMed]
- Keener, J.D.; Patterson, B.M.; Orvets, N.; Aleem, A.W.; Chamberlain, A.M. Optimizing reverse shoulder arthroplasty component position in the setting of advanced arthritis with posterior glenoid erosion: A computer-enhanced range of motion analysis. J. Shoulder Elb. Surg. 2018, 27, 339–349. [Google Scholar] [CrossRef] [PubMed]
- Moineau, G.; Levigne, C.; Boileau, P.; Young, A.; Walch, G. French Society for Shoulder & Elbow (SOFEC). Three-dimensional measurement method of arthritic glenoid cavity morphology: Feasibility and reproducibility. Orthop. Traumatol. Surg. Res. OTSR 2012, 98 (Suppl. 6), S139–S145. [Google Scholar] [CrossRef] [PubMed]
- Walch, G.; Vezeridis, P.S.; Boileau, P.; Deransart, P.; Chaoui, J. Three-dimensional planning and use of patient-specific guides improve glenoid component position: An in vitro study. J. Shoulder Elb. Surg. 2015, 24, 302–309. [Google Scholar] [CrossRef] [PubMed]
- Kidder, J.F.; Rouleau, D.M.; Pons-Villanueva, J.; Dynamidis, S.; DeFranco, M.J.; Walch, G. Humeral Head Posterior Subluxation on CT Scan: Validation and Comparison of 2 Methods of Measurement. Tech. Shoulder Elb. Surg. 2010, 11, 72. [Google Scholar] [CrossRef]
- Goutallier, D.; Postel, J.M.; Bernageau, J.; Lavau, L.; Voisin, M.C. Fatty muscle degeneration in cuff ruptures. Pre- and postoperative evaluation by CT scan. Clin. Orthop. 1994, 304, 78–83. [Google Scholar]
- Neer, C.S.; Craig, E.V.; Fukuda, H. Cuff-tear arthropathy. J. Bone Jt. Surg. Am. 1983, 65, 1232–1244. [Google Scholar] [CrossRef] [PubMed]
- Matsoukis, J.; Tabib, W.; Guiffault, P.; Mandelbaum, A.; Walch, G.; Némoz, C.; Cortés, Z.E.; Edwards, T.B. Primary unconstrained shoulder arthroplasty in patients with a fixed anterior glenohumeral dislocation. J. Bone Jt. Surg. Am. 2006, 88, 547–552. [Google Scholar] [CrossRef] [PubMed]
- Raiss, P.; Edwards, T.B.; Bruckner, T.; Loew, M.; Zeifang, F.; Walch, G. Reverse arthroplasty for patients with chronic locked dislocation of the shoulder (type 2 fracture sequela). J. Shoulder Elb. Surg. 2017, 26, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Werner, B.S.; Böhm, D.; Abdelkawi, A.; Gohlke, F. Glenoid bone grafting in reverse shoulder arthroplasty for long-standing anterior shoulder dislocation. J. Shoulder Elb. Surg. 2014, 23, 1655–1661. [Google Scholar] [CrossRef] [PubMed]



| Patient Number | Gender | Age | Side | Anteversion | Inclination | Subluxation | FI SubScap | FI SupraS | FI InfraS | FI Teres Minor | CT Scan Morphology | Coracoid Contact | X-ray Appearance |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 66 | R | 22 | 0 | 34 | 1 | 4 | 4 | 4 | biconcave | - | Ant Inf sublux |
| 2 | M | 80 | L | 35 | −7 | 11 | 4 | 4 | 4 | 4 | monocave | - | Ant Inf sublux |
| 3 | F | 80 | L | 23 | −19 | 29 | 4 | 4 | 4 | 0 | monocave | + | Ant Inf sublux |
| 4 | F | 83 | R | 54 | −35 | 1 | 3 | 4 | 4 | 0 | biconcave | - | Ant Inf sublux |
| 5 | F | 80 | R | 28 | 7 | 19 | 3 | 3 | 3 | 0 | biconcave | - | Ant Inf sublux |
| 6 | F | 78 | R | 27 | 2 | 28 | 4 | 4 | 4 | 0 | biconcave | - | Ant Inf sublux |
| 7 | F | 74 | L | 27 | 31 | 17 | 4 | 4 | 4 | 0 | monocave | + | Ant Inf sublux |
| 8 | F | 70 | R | 35 | −2 | 20 | 4 | 3 | 4 | 0 | biconcave | - | Ant Inf sublux |
| 9 | F | 84 | R | 24 | −6 | 23 | 1 | 2 | 3 | 0 | monocave | - | Ant Inf sublux |
| 10 | F | 83 | R | 47 | −13 | 0 | 2 | 4 | 4 | 0 | biconcave | - | Ant Inf sublux |
| 11 | M | 54 | L | 58 | −43 | 2 | 1 | 4 | 4 | 0 | monocave | + | Ant Inf sublux |
| 12 | F | 76 | R | 4 | 14 | 44 | 1 | 1 | 4 | 0 | monocave | - | Ant Inf sublux |
| 13 | F | 75 | R | 13 | −7 | 44 | 2 | 4 | 4 | 0 | biconcave | - | Ant Inf sublux |
| 14 | F | 75 | R | 25 | −16 | 18 | 4 | 4 | 4 | 0 | biconcave | + | Ant Inf sublux |
| 15 | F | 72 | R | 33 | 18 | 10 | 4 | 4 | 4 | 0 | biconcave | - | Ant Inf sublux |
| 16 | F | 75 | R | 33 | −2 | 6 | 4 | 4 | 4 | 0 | monocave | + | Ant Inf sublux |
| 17 | F | 73 | R | 50 | −3 | 1 | 4 | 4 | 4 | 0 | biconcave | - | Ant Inf sublux |
| SubScap | Supraspinatus | Infraspinatus | Teres Minor | |
|---|---|---|---|---|
| Stage 4 | 9 | 13 | 15 | 2 |
| Stage 3 | 2 | 2 | 2 | - |
| Stage 2 | 2 | 1 | - | - |
| Stage 1 | 4 | 1 | - | - |
| Stage 0 | - | - | - | 15 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Walch, G.; Collotte, P.; Raiss, P.; Athwal, G.S.; Gauci, M.O. The Characteristics of the Favard E4 Glenoid Morphology in Cuff Tear Arthropathy: A CT Study. J. Clin. Med. 2020, 9, 3704. https://doi.org/10.3390/jcm9113704
Walch G, Collotte P, Raiss P, Athwal GS, Gauci MO. The Characteristics of the Favard E4 Glenoid Morphology in Cuff Tear Arthropathy: A CT Study. Journal of Clinical Medicine. 2020; 9(11):3704. https://doi.org/10.3390/jcm9113704
Chicago/Turabian StyleWalch, Gilles, Philippe Collotte, Patric Raiss, George S. Athwal, and Marc Olivier Gauci. 2020. "The Characteristics of the Favard E4 Glenoid Morphology in Cuff Tear Arthropathy: A CT Study" Journal of Clinical Medicine 9, no. 11: 3704. https://doi.org/10.3390/jcm9113704
APA StyleWalch, G., Collotte, P., Raiss, P., Athwal, G. S., & Gauci, M. O. (2020). The Characteristics of the Favard E4 Glenoid Morphology in Cuff Tear Arthropathy: A CT Study. Journal of Clinical Medicine, 9(11), 3704. https://doi.org/10.3390/jcm9113704





