Abstract
Sports activity has many benefits in cancer survivors. A key one is having sport activity contribute to the well-being of the individual. However, there are no guidelines about the intensity and kind of postoperative mobility workouts after hip or knee megaprosthetic treatment. Opinion research about sports after modular bone and joint replacement may provide an understanding of surgeons’ attitudes on sports activity after megaprostheses of the hip and knee joint. A web survey with members of three international professional organizations of orthopedic tumor reconstructive surgeons was conducted between September 2016 and January 2018. Members were invited via personalized emails by the European Musculoskeletal Oncology Society (EMSOS), the International Society of Limb Salvage (ISOLS), and the Musculoskeletal Tumor Society (MSTS). The questionnaire included 26 questions. A total of 149 surgeons started the survey, and 76 finished the entire survey (American Association for Public Opinion Research (AAPOR) second response rate (RR2) EMSOS: 12.3%; ISOLS: 21.9%; MSTS: n/a). More than half of the respondents encourage sarcoma survivors after megaprosthetic treatment to reach an activity level that would allow them to regularly participate in active sporting events of University of California, Los Angeles (UCLA) activity level 7 and higher. Orthopedic tumor reconstructive surgeons do fear a number of complications (periprosthetic fracture, allograft failure/fracture, loosening, prosthetic or bearing failure, and early polyethylene wear) due to sports activity after modular bone–joint replacement, but they actually witness fewer complications than they conceptually anticipated. According to the surgeons’ opinions, between four to seven types of sports after surgery could reasonably be recommended depending on the type of hip or knee procedures. This survey provides insights into opinions on what could be recommended, what could be allowed if surgeons and their patients agree on the potential negative outcome, and which sports should definitely not be allowed after hip and knee megaprostheses.
1. Introduction
Most public authorities perceive sports as an important societal benefit and include sports participation in their policies [1,2,3]. Sports is an important leisure activity with many benefits [4]. According to European community (EU) statistics, 61% of young people regularly participate in sports, and average sports activity is increasing in the general public [5,6]. However, some people are denied active participation in sports for various orthopedic reasons. This applies in particular to patients after orthopedic reconstructive surgery, including megaprosthetic replacement, partly because they are not able to resume or attain their preoperative sports activity levels after accidental or oncologic life events, partly because their physicians do not dare to endanger their orthopedic reconstructions. In this situation, people with physical impairment are often adapting to their loss of function; however, patients who were active in sports before an impairing life event and bound to lower activity level thereafter usually mourn this loss deeply [7].
To avoid patients’ loss of physical sport activity after knee and hip replacement, expert opinions about sports have been defined by knee and hip societies in order to make some sports possible after surgical treatment without harm [8]. Currently, there is scarcely information available about sports activity for the time after megaprosthetic replacement. Several recent case series including patients after bone and joint mega-replacement elucidated the immanent importance of sporting activities for these patients. However, years-long rehabilitation was necessary after an operation of this magnitude to finally reach moderate-to-high levels of sporting activity after replacement in the proximal and distal femur and in the proximal tibia [9,10,11].
There is not a uniform recommendation on whether sporting activity could be allowed after megaprosthetic replacement: while some tumor and adult reconstructive surgeons restrict routine total joint patients from even moderate athletic endeavors, others set the patient-expectations-in-achievement bar quite high [12]. A survey among orthopedic tumor surgeons, who regularly do lower-extremity bone tumor and megaprosthetic replacement in active younger patients, may help to define limits within sports that may be possible for patients after these kinds of treatment. Amongst other issues within this survey, the following questions needed to be raised and answered: What activity level do surgeons encourage sarcoma survivors to eventually reach after megaprosthetic bone–joint replacement? Which complications and failures due to sports activity do surgeons fear and actually witness after modular bone–joint replacement? What sports do surgeons recommend, allow, and not allow to sarcoma survivors after modular hip or knee lower-limb reconstructions?
2. Methods
To answer our research questions, we conducted a web survey with members of three international professional organizations of tumor reconstructive surgeons: the European Musculoskeletal Oncology Society (EMSOS), the International Society of Limb Salvage (ISOLS) and the Musculoskeletal Tumor Society (MSTS) between September 2016 and January 2018. The questionnaire comprised 26 questions and was programmed in Qualtrics Research Core. The target population were the members of the three organizations, and we used the membership lists of these organizations as the sampling frame for our study. At the time of first contact, the membership lists of the three organizations included 155 (EMSOS), 310 (ISOLS, excluding all EMSOS members), and 335 (MSTS) members.
Personalized e-mail invitations were sent to EMSOS members on 14 September 2016, with up to four follow-up reminders to nonrespondents on 21 September, 20 October, and 20 December 2016, as well as on 26 February 2017 (field period: 14 September 2016–6 April 2017). Personalized e-mail invitations were sent to ISOLS members on 4 May 2017, with up to three e-mail reminders for nonrespondents on 23 May, 4 July, and 18 August 2017 (field period: 4 May–30 August 2017). For MSTS members, we did not have access to individual e-mail addresses; thus, invitations were sent as part of the regular MSTS newsletter on 13 December 2017 with 2 reminders (field period: 13 December 2017–17 January 2018). There can be overlap since many members of MSTS and EMSOS are also members of ISOLS, and only a single response was recorded for an individual surgeon.
A total of 149 surgeons started the survey, and 76 completed the entire questionnaire (I = Interviews) with an additional 35 surgeons breaking-off after the demographic information (P = Partial Interviews) about half-way through the questionnaire. All analyses use n = 111 (I + P). Table 1 summarizes the participation behavior for members of the three organizations. The response rate as calculated based on the Standard Definitions by the American Association for Public Opinion Research [13] was 12.3% (AAPOR second response rate (RR2)) for EMSOS members and 21.9% for ISOLS members. We do not know how many MSTS members received the newsletter with the invitation to our survey; thus, we cannot calculate a response rate for this group. Since surgeons could be members in multiple organizations, our response rates are conservative estimates of the true response rate. The sociodemographic as well as regional characteristics of the respondents are presented in Table 2.

Table 1.
Participation behavior and American Association for Public Opinion Research (AAPOR) response rates.

Table 2.
Sociodemographic characteristics of the respondents.
First, respondents were asked to indicate their agreement with two items about the influence of sporting activity on sarcoma survivors’ well-being on a five-point rating scale (strongly disagree–strongly agree) (see Section 3.1).
Second, they were asked about the encouraged activity level after surgery measured by using the 10-point University of California Los Angeles (UCLA) activity scale [14] (see Section 3.2).
Third, respondents were asked which of nine sports-activity-associated complications and failures they fear after modular bone–joint replacement in sarcoma survivors and which of these they had actually witnessed (see Figure 1. The “feared” to the “witnessed” complications were compared conducting McNemar tests and calculating odds ratios (see Section 3.3).
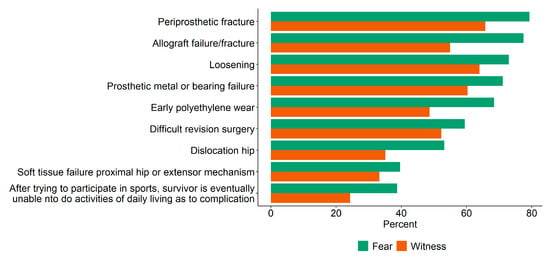
Figure 1.
Percent of respondents who feared and witnessed post-surgery complications due to sports activity.
Fourth, respondents were asked whether they would be more likely to allow a sarcoma survivor to participate in a sport after megaprosthetic replacement surgery if the survivor had prior experience in the particular sport. We then provided respondents a list of 40 different sports and asked the respondents which of the activities they would recommend, which of them they would allow if a survivor asked, and which of them they would not allow sarcoma survivors to do after megaprosthetic replacement surgery. These questions were asked for up to five different modular hip or knee replacement limb salvage procedures based on the surgeons’ experience with the procedure (see Section 3.4).
Finally, the recommendations for sports were compared on whether they differ by experience practicing tumor-orthopedic surgery (15 years or less vs. more than 15 years) using a Mann–Whitney U tests and by region (Europe vs. Americas vs. Asian Pacific) using a Kruskal–Wallis test for the comparisons of median number of sports recommended, allowed, and not allowed as well as chi square tests for the proportion of recommendations for individual sports (see Section 3.5).
All analyses were conducted in R version 3.6.1 [15], Dunn–Šidák correction was used for multiple comparisons. The sequence of the 40 sports corresponds to the average naming by participants according to recommended, recommended if asked, and not allowed (see Table 3).

Table 3.
Sports recommended; allowed, if asked; and not allowed after surgery.
3. Results
3.1. Attitudes toward Sporting Activity after Modular Bone–Joint Replacement
Almost half of the respondents (47%; 95% confidence interval (CI): 37%–57%) strongly agreed and 38% (95% CI: 29%–48%) somewhat agreed with the statement that sport participation is an important contributor to sarcoma survivors’ feelings of well-being after modular bone–joint replacement. Around 9% (95% CI: 5%–16%) neither agreed nor disagreed with the statement, and only 6% (95% CI: 3%–13%) somewhat disagreed or strongly disagreed. Similarly, 44% (95% CI: 35%–54%) of respondents strongly agreed and 44% (95% CI: 35%–54%) somewhat agreed with the statement that sport participation has a positive effect on survivors of bone sarcoma after modular bone–joint replacement. Less than 5% (95% CI: 2%–11%) neither agreed nor disagreed, and around 7% (95% CI: 3%–14%) somewhat or strongly disagreed with the statement.
3.2. Activity Levels Encouraged to Reach after Modular Bone–Joint Replacement
More than half of the respondents encourage sarcoma survivors to reach an activity level that would allow them to regularly participate in active sporting events after modular bone–joint replacement (UCLA activity scale median: 7; range 2–9) (see Figure 2).
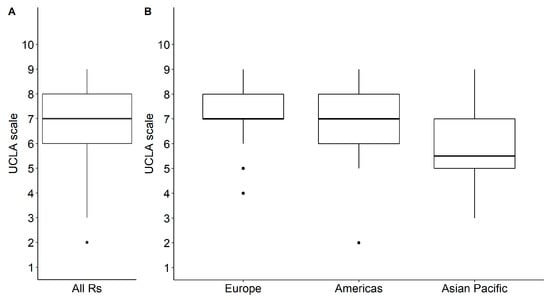
Figure 2.
Box plot of responses to University of California, Los Angeles (UCLA) activity scale: (A) all respondents; (B) by region. UCLA Score: 1: Wholly inactive, dependent on others, and cannot leave residence; 2: Mostly inactive or restricted to minimum activities of daily living; 3: Sometimes participates in mild activities, such as walking, limited housework, and limited shopping; 4: Regularly participates in mild activities; 5: Sometimes participates in moderate activities such as swimming or could do unlimited housework or shopping; 6: Regularly participates in moderate activities; 7: Regularly participates in active events such as bicycling; 8: Regularly participates in active events, such as golf or bowling; 9: Sometimes participates in impact sports such as jogging, tennis, skiing, acrobatics, ballet, heavy labor, or backpacking; 10: Regularly participates in impact sports.
3.3. Feared and Witnessed Post-Surgery Complications Due to Sports Activity
Respondents do fear a number of complications due to sports activity after modular bone–joint replacement, but they actually witness fewer complications (Figure 2). A majority of respondents feared periprosthetic fracture (79%; 95% CI: 70%–86%), allograft failure/fracture (77%; 95% CI: 68%–85%), loosening (73%; 95% CI: 64%–81%), prosthetic or bearing failure (71%; 95% CI: 62%–79%), and early polyethylene wear (69%; 95% CI: 59%–77%) as post-surgery complications from sports activity. The most frequently reported sport-activity-associated complications after surgery were periprosthetic fracture (66%; 95% CI: 56%–74%), loosening (64%; 95% CI: 54%–73%), and prosthetic or bearing failure (60%; 95% CI: 51%–69%). There was a discrepancy between what respondents reported to fear and what they actually witnessed for the four types of complications. Respondents were less likely to witness than to fear early polyethylene wear (odds ratio (OR) = 0.15; 95% CI: 0.03–0.37; p < 0.001), periprosthetic fracture (OR = 0.25; 95% CI: 0.05–0.60; p = 0.04), dislocation of the hip (OR = 0.15; 95% CI: 0.03–0.39; p = 0.02), and allograft failure/fracture (OR = 0.19; 95% CI: 0.06–0.41; p < 0.001).
3.4. Recommended, Allowed, and Not Allowed Sports after Modular Bone–Joint Replacements
Sixty-four percent (95% CI: 51%–74%) of respondents reported being more likely to allow a patient to participate in a sport postoperatively if the patient had prior experience with this sport. Thirty-six percent (95% CI: 26%–49%) of respondents stated that it made no difference in recommendation when prior experience was evident. After proximal femoral replacement hemiarthroplasty, monopolar or bipolar, a median of seven (95% CI: 5–8) different sports were recommended by respondents; 12 (95% CI: 10–15) were allowed, if asked by the patient; and 20 (95% CI: 17–23) were not allowed (Figure 3). After proximal femoral replacement total hip replacement (THR), a median of five (95% CI: 3–7) sports were recommended; 10 (95% CI: 7–14) were allowed, if asked; and 22 (95% CI: 19–26) were not allowed. After distal femoral replacement hinged total knee replacement (TKR), a median of seven (95% CI: 5–8) sports were recommended; 12 (95% CI: 10–14) were allowed, if asked; and 19.5 (95% CI: 16–22) were not allowed, if asked. After proximal tibial replacement hinge TKR with soft tissue extensor reconstruction probable gastrocnemius rotation, a median of four (95% CI: 3–7) sports were recommended; 10 (95% CI: 9–13) were allowed, if asked; and 22 (95% CI: 19–26) were not allowed. After proximal tibial replacement hinge TKR allograft prosthetic composite for extensor reconstruction, a median of five (95% CI: 3–7) sports were recommended; 13 (95% CI: 10–15) were allowed, if asked; and 21.5 (95% CI: 16–26) were not allowed. Walking, swimming, and stationary bicycling were the most often recommended sporting activities after surgery (Table 3).
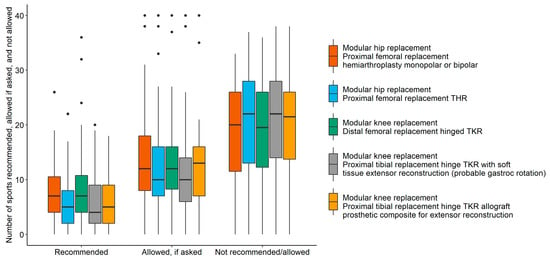
Figure 3.
Number of recommended, allowed, and not allowed sports after surgery by procedure.
3.5. Differences in Recommendations by Regions and Experience
Recommendations about what activity level was encouraged and what sports were recommended, allowed, and not allowed differed by region but not by the years of experience practicing tumor-orthopedic surgery. Respondents from Europe (median = 7; range: 4–9; p = 0.003) and the Americas (median = 7; range: 6–9; p = 0.001) encouraged sarcoma survivors to reach a higher level of activity than did respondents from Asian Pacific region (median = 5.5; range: 5–9; Figure 2B). Only 29% (95% CI: 11%–56%) of respondents from Asian Pacific countries recommended golf after proximal femoral replacement hemiarthroplasty, monopolar or bipolar, compared to 71% (95% CI: 55%–84%; p = 0.008) of respondents from the Americas, and only 24% (95% CI: 8%–50%) of Asian Pacific respondents allowed hunting, if asked by the sarcoma survivor compared to 71% (95% CI: 55%–84%; p = 0.022) from the Americas. Respondents from Asian Pacific countries more often did not allow gymnastics (88%; 95% CI: 60%–98%) compared to European respondents (29%; 95% CI: 12%–52%; p = 0.034) after proximal femoral replacement THR. While only 43% (95% CI: 19%–70%; p = 0.032) of respondents from Asian Pacific countries recommended stationary bicycling, 89% (95% CI: 70%–97%) of respondents from Europe and 88% (95% CI: 72%–95%) of respondents from the Americas did so after distal femoral replacement hinged TKR. For the same procedure, fewer respondents from Asian Pacific countries (7%; 95% CI: 1%–34%) compared to European respondents (59%; 95% CI: 39%–77%; p = 0.047) recommended road bicycling. Finally, fewer European respondents (28%; 95% CI: 13%–50%) than respondents from the Americas (81%; 95% CI: 62%–92%) and Asian Pacific countries (92%; 95% CI: 60%–99%; p = 0.008) did not allow gymnastics after proximal tibial replacement hinge TKR with soft tissue extensor reconstruction with probable gastrocnemius rotation (Table 4).

Table 4.
Proportions (and 95% confidence intervals) of recommended, allowed, and not allowed sports after surgery by regions. Listed sports differed significantly between regions.
4. Discussion
Megaprosthetic replacement is commonly performed in lower-limb reconstruction after tumor resections [16,17,18,19] as well as increasingly after trauma [20,21,22] or failed primary endoprosthetic replacement [23,24]. Despite their high rates of long-term sequelae including infection, mechanical and soft tissue failures, and loosening, patients benefit from surgery by being able to use their lower extremities in activities of daily living. However, once patients enter the rehabilitation phase after megaprosthetic replacement, mobility and function become vaguely described and patients as well as therapists may become confused as to possible mobility restrictions compared to practical endoprosthetic use. A recent systematic review about fitness, function, and exercise training responses after limb salvage with lower-limb megaprostheses concludes that exercise interventions are required. Interestingly, the authors describe the absence of outcome measure items assessing higher-level functioning [25]. Especially for young patients who are faced with a cancer diagnosis early in life, it is important to regain physical performance and mental and social well-being. Currently, sporting activities for handicapped people are facilitated both by creating opportunities such as organized disabled sporting events and by the provision of novel technical developments in exoprosthetics and bionics [26,27]. Of note, the importance of sports activity in oncologic disease has been widely reported with benefits in cancer cohorts [28].
This current survey was therefore assessed in orthopedic tumor societies expecting that surgeons are frequently confronted with requests for sporting activities by younger, active cancer survivors reconstructed with megaprostheses.
Oncologic as well as reconstructive surgeons seem divided over what degree (light activity to strenuous) of sporting activity should be allowed after megaprosthetic limb reconstruction. The most recommended sports were walking, swimming, and playing golf. Only 14% of the respondents allowed some impact-type activities, although nearly 2/3 of the participants were more likely to allow patients to participate in a sport postoperatively when it had been practiced before such as bicycling, ballroom dancing, and bowling, most respondents favored allowing the lower degree of a vigorous activity. Only 15% of the listed sports were recommended, but over 50% of the listed sports were not recommended at all. Most respondents may have considered proximal femoral replacement hemiarthroplasty, monopolar or bipolar, and distal femoral replacement the most stable reconstructions and, therefore, recommended a median of seven different sports. Five different sports were recommended by respondents after proximal femoral replacement THR and after proximal tibial replacement hinge TKR allograft prosthetic composite for extensor reconstruction. Only four different sports were recommended after proximal tibial replacement hinge TKR with soft tissue extensor reconstruction probable gastrocnemius rotation (Table 3). These recommendations may partly reflect the incidence of possible failures in these particular reconstructions (see later), but even more the fear for difficult re-reconstruction, worse functional outcome [29], and higher amputation rate especially after proximal tibia reconstruction [30]. In comparing proximal tibia reconstructions, there may be more stability and confidence in TKA allograft composite for extensor reconstruction than in TKA with soft tissue reconstruction in the respondents´ perception, which goes in line with data published by Müller et al. [31]. Hemiarthroplasty appears to have the lowest risk for instability in the proximal femur reconstruction than THR [32]. However, since recommendations on which sports can safely be done are not available and are often limited to the personal experience of the surgeon, even recommending some of these sporting activities (Table 2) may serve as a possible guideline in postoperative care of these patients.
Healy et al. reported similar sport restrictions in the first consensus expert opinion about sports activity after elective joint arthroplasty of the hip in 1999. In a second consensus paper 2005, several more sports were recommended that had previously been only just allowed [8,33]. The reason for the relaxations in recommendations after primary elective joint replacement might possibly be a change in attitudes of surgeons by observing more vigorous activities in their patients without witnessing any late complications. A more restrictive approach to recommending only some sports contradicts the recommended UCLA level of 7/10 when general activity was requested by the patient. Amstutz et al. defined a UCLA sports activity level of six after elective hip replacement as already high activity [14]. This discrepancy may elucidate once more the uncertainty of surgeons when recommending or allowing a particular sporting activity. There is the fear for a catastrophic event, which often prohibits allowing a more vigorous activity.
Megaprosthetic reconstruction bears the risk for failure in the long term. A comprehensive failure mode classification by the ISOLS serves as the mainstay in describing mechanical (aseptic loosening, soft tissue and structural component failure) but also non-mechanical failures. Authors of this multicenter study reported about 49% mechanical failures out of 534 failures in 2174 primary megaprosthetic replacements. A statistical dependence of anatomic region was found showing a total of 8% percent mechanical failures after proximal femur, 14% after distal femur, and 13% after proximal tibia megaprosthetic reconstruction [34]. According to Grimer et al., the vast majority of patients (82%) will need at least one revision surgery after 30 years following first-generation megaprosthesis [17]. In spite of modern megaprosthetic design changes, aseptic loosening and structural failure exist in 16%–19% of patients [35,36]. Furthermore, in oncologic cases, chemotherapy may affect osseointegration of megaprosthesis in the first 3 years, increasing the risk for aseptic loosening [37]. However, there is no clear evidence in the literature as to which activity levels lead to mechanical prosthetic failure or whether a higher activity level and exercise may control falls and even prevent from consequent prosthetic hardware failure [38]. Furthermore, there is hardly evidence that revision surgery worsens activities of daily living (ADLs) outcome in the long run. According to Biau et al. [18], body weight and activity levels were independent risk factors for early revision after megaprostheses around the knee but did not mention a specific activity loss after revision surgery. Hobusch et al. and Lang et al. reported possible events of loosening or structural failure in association with higher activity levels with proximal femur and around-the-knee megaprostheses. However, the patients’ subsequent activity level was not influenced by revision surgery [9,10,11]. Most surgeons in this current survey (71%–79%) seem more conservative because of fear of a second operation and patients never achieving the original first procedural function if too vigorous of sporting activity is undertaken and failure occurs. Furthermore, the high percentage of fear for sporting-activity-associated complications seem justified considering the high percentage of the reported witness of activity-associated failures. In fact, 60%–66% of the respondents witnessed periprosthetic fracture, loosening, or prosthetic or bearing failure in association with activity, and one quarter of the respondents even witnessed complication episodes in patients who were unable to resume activities of daily living (ADLs). Authors in musculoskeletal oncology literature usually report on Musculoskeletal Tumor Society Score (MSTS) or Toronto Extremity Salvage Score (TESS) outcome data and failure modes without reporting on both together [39]. There is a gap in knowledge about a relationship between sporting activities and failures as well as quality of life following megaprosthetic treatment.
The apparent surgeon expectations were more conservative than what was reported in published case-series unless patients requested to be allowed to do a more vigorous activity. The key point seems to be whether the surgeon is rigid in the initial recommendations or is flexible in allowing a more vigorous activity when the patient makes a request. The “fear” evidence as reported by the respondents suggests that it is appropriate not to encourage patients to overdo sporting activity beyond what is recommended in this current expert respondent review. However, once the patient asks for an increase in vigorous activity level and the surgeon is confronted in possibly modifying their recommendation, a shift of responsibility occurs by counseling the patient about the possible undesirable outcome. Surgeons are the ones who have to take care of the complications and hope to bring the patient back to their best possible ADLs. Interestingly, no respondent wanted to quantitate the recommended number of days of the week or length of the duration of activity in this survey.
This survey ought to help define the conceptual limits between which sporting activities after megaprosthesis may be allowed. The types of sports, defined as recommended in this survey, may be safely done by the patients. Furthermore, the type of sports, defined as allowed if asked, ought to be subject of further investigations in this reconstruction field (see Figure 4).
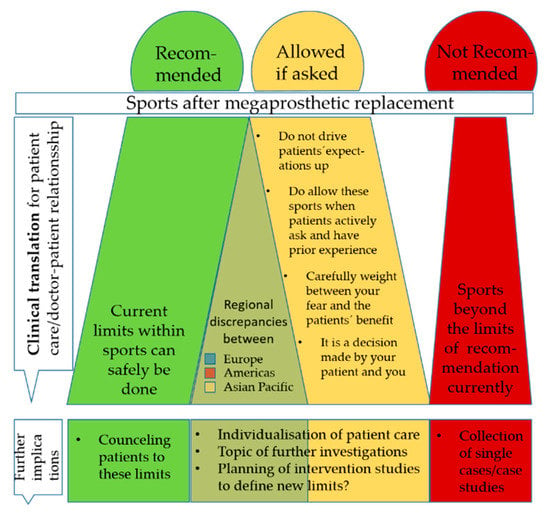
Figure 4.
Graphical summary of sport recommendations after megaprosthetic replacement.
According to the European Sports Charter, “Sports” not only means all forms of physical activity aimed at expressing or improving physical fitness and mental well-being but it is also means forming social relationships [40]. A cross-national study including 33 countries found that nearly 90% of individuals positively perceive sports as an arena for socialization [1]. This influence can also be turned in the other direction as different geographic regions form their specific sports attitudes. It therefore comes as no surprise that expert opinions concerning sports differ between these regions (see Table 4). Cross-continental differences in sporting habits may lead to different perceptions of certain sports and likelihood of allowing them or prohibiting the activity after lower-extremity limb salvage reconstruction. Surgeons may not be concerned about the reconstructed patient playing the most popular sports in their respective country when the surgeon is familiar with the activity. Examples would be playing golf in the United States or riding a road bike in Europe. The level of sporting activity should be balanced as to risks of complications from the level of activity and cultural norms. In some Asian Pacific regions, even regular joint replacement patients are not allowed for higher activity because of a dislike for revision prosthetic replacement surgery or for caution. The international differences in sports activity levels ought to be discussed in international panels to possibly create new approaches and equalities in international future sport recommendations.
Since this current online survey was done in musculoskeletal oncologic societies, issues of quality of life (QOL) were an initial primary focus. This current survey shows a broad agreement of 85% of orthopedic tumor surgeons on sporting activities as a contributor to well-being and even 88% who feel that there are positive effects of sport activity in survivors after bone and joint modular prosthetic replacement. These opinions reflect already existing literature about quality of life (QOL), mobility, and limitations in survivors of bone sarcoma and the obvious need to promote physical activity after bone tumor treatment [41]. Ness et al. reported a relative risk of 2.6–3.2 to develop performance limitations in bone sarcoma patients as well as a relative risk of 5.5–7.0 to develop restricted routine activities [42]. In line with these results, several authors reported the lowest physical functioning item of the Short Form 36 Health Survey Questionaire (SF-36) scores in survivors of bone sarcoma when compared with that in all cancer populations [43]. Furthermore, current preliminary data suggest an underlying association between physical activity and mortality for survivors of different cancers [44].
There are several limitations in this survey. First, the number of participating surgeons is low when measured in terms of orthopedic oncologic practice. The number of surgeons involved based on mean age and mean surgical experience seemed to be a representative group. This survey of surgeons assesses the individual biases of surgeons based on their anecdotal experience, as opposed to being evidence based. This survey does address whether a surgeon has “ever witnessed” the reported complication, which does not address the rate of the complication in the overall population or reconstruction-specific populations. Furthermore, in addition to intercontinental differences of recommendations, there might also be differences between European countries, which because of the low number from single countries are not significant according to this survey.
5. Conclusions
This survey provides insights into the current practice of surgeons counseling their patients toward sporting activities. Based on this knowledge, intervention studies may be planned to further translate current practice into recommendations (see Figure 5).
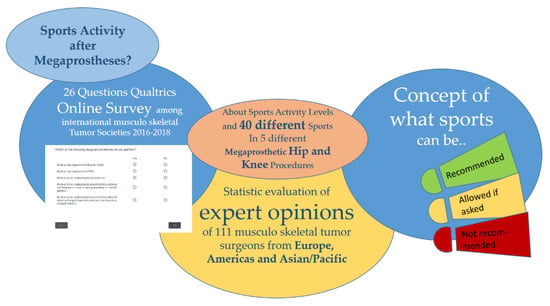
Figure 5.
Graphical abstract of the Mo(dular) Re(placement) Sports Survey.
This survey ought to define the limits between which sporting activities after megaprosthesis may be seen to be safe. The types of sports, defined as recommended in this survey, may be safely done by the patients. There is consensus about the benefits of some light-impact sporting activity after lower-extremity limb salvage reconstructions.
Furthermore, the type of sports, defined as allowed if asked, ought to be the subject of further investigations in this important field. The fear of disaster and need to do another surgery is a realistic concern, and surgeons really have to ask the question as to why they compromise when patients request to do more vigorous sporting activity. It is important that the expectations of patients should not be driven upward to a higher sports activity level to their detriment, e.g., needing a second operation. However, once patients ask for certain activities in the gray area between recommended and not allowed, surgeons can only hope patients accept their “wishes within boundaries.” Individualization of a patient management may also need to include the patients’ personal wishes.
As such, this currently presented survey may represent an understanding of what other surgeons allow for postoperative sports activity after modular megaprostheses implantation. The survey provides some concept of what can be recommended, what can be allowed if surgeons and their patients agree on the potential negative outcome, or which sports should definitely not be allowed. Objective data about the relation of activity levels and prosthetic failure are needed.
Author Contributions
Conceptualization, G.M.H., M.J., and F.K.; methodology, G.M.H., M.J., and F.K.; formal analysis, G.M.H., M.J., and F.K.; programming, F.K.; data curation, G.M.H. and F.K.; writing—original draft preparation, G.M.H., M.J., and F.K.; writing—review and editing, G.M.H., M.J., F.K., H.T., and R.W.; visualization, G.M.H. and F.K.; supervision, G.M.H., M.J., F.K., and R.W.; project administration, G.M.H., M.J., and R.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Acknowledgments
We thank the members of the European Musculoskeletal Oncology Society (EMSOS), the International Society of Limb Salvage (ISOLS), and the Musculoskeletal Tumor Society (MSTS) who supported the survey by responding.
Conflicts of Interest
The authors declare no conflict of interest.
Abbreviations
| AAPOR RR1 | American Association for Public Opinion Research First Response Rate |
| AAPOR RR2 | American Association for Public Opinion Research Second Response Rate |
| dF | Distal femur megaprosthetic replacement |
| EMSOS | European Musculoskeletal Oncology Society |
| EU | European Union |
| ISOLS | International Society of Limb Salvage |
| MoReSports online survey | Modular Replacement Sports Survey |
| MSTS | Musculoskeletal Tumor Society |
| pF/ext.Ap | Proximal tibia megaprosthetic replacement with extensor apparatus reconstruction (e.g., gastrocnemius flap) |
| pF/Hemi | Proximal femur megaprosthesis without acetabular replacement |
| pF/THR | Proximal femur megaprosthesis with acetabular replacement |
| pT/composit | Proximal tibia megaprosthetic replacement with composite allograft prosthesis |
| QOL | Quality of life |
| TKR | Total knee replacement |
| UCLA Score | University of California Los Angeles Sports Activity Score |
References
- Seippel, Ø. Do sports matter to people? A cross-national multilevel study. Sport Soc. 2018, 1–15. [Google Scholar] [CrossRef]
- Breuer, C.; Hoekman, R.; Nagel, S.; van der Werff, H. (Eds.) Sport Clubs in Europe: A Cross-National Comparative Perspective; Sports Economics, Management and Policy; Springer International Publishing: Basel, Switzerland, 2015; ISBN 978-3-319-17634-5. [Google Scholar]
- Bureau of Educational and Cultural Affairs. Sports and Sustainability Initiative. Available online: https://eca.state.gov/sustainability-sports-initiative (accessed on 13 September 2020).
- Tammelin, T.; Näyhä, S.; Hills, A.P.; Järvelin, M.R. Adolescent participation in sports and adult physical activity. Am. J. Prev. Med. 2003, 24, 22–28. [Google Scholar] [CrossRef]
- European Commission—PRESS RELEASES—Press release—Eurobarometer zu Sport und körperlicher Betätigung. Available online: http://europa.eu/rapid/press-release_MEMO-14-207_de.htm (accessed on 28 June 2016).
- Sport and Physical Activity: Report; Publications Office: Luxembourg, 2014.
- Fauske, L.; Bruland, O.S.; Grov, E.K.; Bondevik, H. Cured of primary bone cancer, but at what cost: A qualitative study of functional impairment and lost opportunities. Sarcoma 2015, 2015, 484196. [Google Scholar] [CrossRef]
- Healy, W.L.; Sharma, S.; Schwartz, B.; Iorio, R. Athletic activity after total joint arthroplasty. J. Bone Jt. Surg. Am. 2008, 90, 2245–2252. [Google Scholar] [CrossRef] [PubMed]
- Lang, N.W.; Hobusch, G.M.; Funovics, P.T.; Windhager, R.; Hofstaetter, J.G. What sports activity levels are achieved in patients with modular tumor endoprostheses of osteosarcoma about the knee? Clin. Orthop. Relat. Res. 2015, 473, 847–854. [Google Scholar] [CrossRef] [PubMed]
- Hobusch, G.M.; Lang, N.; Schuh, R.; Windhager, R.; Hofstaetter, J.G. Do patients with ewing’s sarcoma continue with sports activities after limb salvage surgery of the lower extremity? Clin. Orthop. Relat. Res. 2015, 473, 839–846. [Google Scholar] [CrossRef]
- Hobusch, G.M.; Bollmann, J.; Puchner, S.E.; Lang, N.W.; Hofstaetter, J.G.; Funovics, P.T.; Windhager, R. What Sport Activity Levels Are Achieved in Patients After Resection and Endoprosthetic Reconstruction for a Proximal Femur Bone Sarcoma? Clin. Orthop. Relat. Res. 2016. [Google Scholar] [CrossRef]
- Joyce, M.J. CORR Insights®: What sports activity levels are achieved in patients with modular tumor endoprostheses of osteosarcoma about the knee? Clin. Orthop. Relat. Res. 2015, 473, 855–857. [Google Scholar] [CrossRef][Green Version]
- American Association of Public Opinion Research. Standard Definitions Final Dispositions of Case Codes and Outcome Rates for Surveys; Revised 2016; American Association for Public Opinion Research: Washington, DC, USA, 2016. [Google Scholar]
- Amstutz, H.C.; Thomas, B.J.; Jinnah, R.; Kim, W.; Grogan, T.; Yale, C. Treatment of primary osteoarthritis of the hip. A comparison of total joint and surface replacement arthroplasty. J. Bone Jt. Surg. Am. 1984, 66, 228–241. [Google Scholar] [CrossRef]
- R: A Language and Environment for Statistical Computing. Available online: https://www.gbif.org/tool/81287/r-a-language-and-environment-for-statistical-computing (accessed on 7 September 2020).
- Smolle, M.A.; Andreou, D.; Tunn, P.-U.; Leithner, A. Advances in tumour endoprostheses: A systematic review. EFORT Open Rev. 2019, 4, 445–459. [Google Scholar] [CrossRef]
- Grimer, R.J.; Aydin, B.K.; Wafa, H.; Carter, S.R.; Jeys, L.; Abudu, A.; Parry, M. Very long-term outcomes after endoprosthetic replacement for malignant tumours of bone. Bone Jt. J. 2016, 98-B, 857–864. [Google Scholar] [CrossRef] [PubMed]
- Biau, D.; Faure, F.; Katsahian, S.; Jeanrot, C.; Tomeno, B.; Anract, P. Survival of total knee replacement with a megaprosthesis after bone tumor resection. J. Bone Jt. Surg. Am. 2006, 88, 1285–1293. [Google Scholar] [CrossRef]
- Calderón, S.A.L.; Kuechle, J.; Raskin, K.A.; Hornicek, F.J. Lower Extremity Megaprostheses in Orthopaedic Oncology. Available online: https://pubmed.ncbi.nlm.nih.gov/29781818/ (accessed on 16 September 2020).
- Lundh, F.; Sayed-Noor, A.S.; Brosjö, O.; Bauer, H. Megaprosthetic reconstruction for periprosthetic or highly comminuted fractures of the hip and knee. Eur. J. Orthop. Surg. Traumatol. 2014, 24, 553–557. [Google Scholar] [CrossRef] [PubMed]
- Windhager, R.; Schreiner, M.; Staats, K.; Apprich, S. Megaprostheses in the treatment of periprosthetic fractures of the knee joint: Indication, technique, results and review of literature. Int. Orthop. 2016, 40, 935–943. [Google Scholar] [CrossRef] [PubMed]
- Meluzio, M.C.; Oliva, M.S.; Minutillo, F.; Ziranu, A.; Saccomanno, M.F.; Maccauro, G. The use of knee mega-prosthesis for the management of distal femoral fractures: A systematic review. Injury 2019. [Google Scholar] [CrossRef]
- Vertesich, K.; Puchner, S.E.; Staats, K.; Schreiner, M.; Hipfl, C.; Kubista, B.; Holinka, J.; Windhager, R. Distal femoral reconstruction following failed total knee arthroplasty is accompanied with risk for complication and reduced joint function. BMC Musculoskelet. Disord. 2019, 20, 47. [Google Scholar] [CrossRef]
- Savvidou, O.D.; Mavrogenis, A.F.; Sakellariou, V.; Vottis, C.; Christogiannis, I.; Vlasis, K.; Christodoulou, M.; Papagelopoulos, P.J. Salvage of Failed Total Hip Arthroplasty with Proximal Femoral Replacement. Available online: https://pubmed.ncbi.nlm.nih.gov/25275970/ (accessed on 16 September 2020).
- Wilson, P.J.; Steadman, P.; Beckman, E.M.; Connick, M.J.; Carty, C.P.; Tweedy, S.M. Fitness, Function, and Exercise Training Responses after Limb Salvage With a Lower Limb Megaprosthesis: A Systematic Review. Pm R 2019, 11, 533–547. [Google Scholar] [CrossRef]
- Matthews, D.; Sukeik, M.; Haddad, F. Return to sport following amputation. J. Sports Med. Phys. Fit. 2014, 54, 481–486. [Google Scholar]
- Steensma, D.P.; Rayson, D.; Shampo, M.A.; Kyle, R.A. Terry Fox: Canadian Cancer Research Activist Whose “Marathon of Hope” Inspired Millions. Mayo Clin. Proc. 2014, 89, e75–e76. [Google Scholar] [CrossRef] [PubMed]
- Patel, A.V.; Friedenreich, C.M.; Moore, S.C.; Hayes, S.C.; Silver, J.K.; Campbell, K.L.; Winters-Stone, K.; Gerber, L.H.; George, S.M.; Fulton, J.E.; et al. American College of Sports Medicine Roundtable Report on Physical Activity, Sedentary Behavior, and Cancer Prevention and Control. Med. Sci. Sports Exerc. 2019, 51, 2391–2402. [Google Scholar] [CrossRef]
- Petschnig, R.; Baron, R.; Kotz, R.; Ritschl, P.; Engel, A. Muscle function after endoprosthetic replacement of the proximal tibia. Different techniques for extensor reconstruction in 17 tumor patients. Acta Orthop. Scand. 1995, 66, 266–270. [Google Scholar] [CrossRef] [PubMed]
- Lm, J.; Rj, G.; Sr, C.; Rm, T. Risk of Amputation Following Limb Salvage Surgery with Endoprosthetic Replacement, in a Consecutive Series of 1261 Patients. Available online: https://pubmed.ncbi.nlm.nih.gov/12799759/ (accessed on 16 September 2020).
- Müller, D.A.; Beltrami, G.; Scoccianti, G.; Cuomo, P.; Capanna, R. Allograft-prosthetic composite versus megaprosthesis in the proximal tibia-What works best? Injury 2016, 47 (Suppl. 4), S124–S130. [Google Scholar] [CrossRef]
- Henderson, E.R.; Keeney, B.J.; Pala, E.; Funovics, P.T.; Eward, W.C.; Groundland, J.S.; Ehrlichman, L.K.; Puchner, S.S.E.; Brigman, B.E.; Ready, J.E.; et al. The stability of the hip after the use of a proximal femoral endoprosthesis for oncological indications: Analysis of variables relating to the patient and the surgical technique. Bone Jt. J. 2017, 99-B, 531–537. [Google Scholar] [CrossRef] [PubMed]
- Healy, W.L.; Iorio, R.; Lemos, M.J. Athletic activity after joint replacement. Am. J. Sports Med. 2001, 29, 377–388. [Google Scholar] [CrossRef] [PubMed]
- Henderson, E.R.; Groundland, J.S.; Pala, E.; Dennis, J.A.; Wooten, R.; Cheong, D.; Windhager, R.; Kotz, R.I.; Mercuri, M.; Funovics, P.T.; et al. Failure mode classification for tumor endoprostheses: Retrospective review of five institutions and a literature review. J. Bone Jt. Surg. Am. 2011, 93, 418–429. [Google Scholar] [CrossRef]
- Palumbo, B.T.; Henderson, E.R.; Groundland, J.S.; Cheong, D.; Pala, E.; Letson, G.D.; Ruggieri, P. Advances in segmental endoprosthetic reconstruction for extremity tumors: A review of contemporary designs and techniques. Cancer Control 2011, 18, 160–170. [Google Scholar] [CrossRef]
- Shehadeh, A.; Noveau, J.; Malawer, M.; Henshaw, R. Late Complications and Survival of Endoprosthetic Reconstruction after Resection of Bone Tumors. Clin. Orthop. Relat. Res. 2010, 468, 2885–2895. [Google Scholar] [CrossRef]
- Mumith, A.; Coathup, M.; Edwards, T.C.; Gikas, P.; Aston, W.; Blunn, G. Multidrug chemotherapy causes early radiological signs of loosening in distal femoral replacements. Bone Jt. Res. 2020, 9, 333–340. [Google Scholar] [CrossRef]
- Sherrington, C.; Fairhall, N.J.; Wallbank, G.K.; Tiedemann, A.; Michaleff, Z.A.; Howard, K.; Clemson, L.; Hopewell, S.; Lamb, S.E. Exercise for preventing falls in older people living in the community. Cochrane Database Syst. Rev. 2019. [Google Scholar] [CrossRef]
- Pala, E.; Trovarelli, G.; Angelini, A.; Maraldi, M.; Berizzi, A.; Ruggieri, P. Megaprosthesis of the knee in tumor and revision surgery. Acta Biomed. 2017, 88, 129–138. [Google Scholar] [CrossRef]
- European Commission and Directorate-General for Eduction and Culture; White Paper on Sports. 2007. Available online: https://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=COM:2007:0391:FIN:EN:PDF (accessed on 16 September 2020).
- Götte, M.; Taraks, S.; Boos, J. Sports in pediatric oncology: The role(s) of physical activity for children with cancer. J. Pediatr. Hematol. Oncol. 2014, 36, 85–90. [Google Scholar] [CrossRef]
- Ness, K.K.; Mertens, A.C.; Hudson, M.M.; Wall, M.M.; Leisenring, W.M.; Oeffinger, K.C.; Sklar, C.A.; Robison, L.L.; Gurney, J.G. Limitations on physical performance and daily activities among long-term survivors of childhood cancer. Ann. Intern. Med. 2005, 143, 639–647. [Google Scholar] [CrossRef] [PubMed]
- Rueegg, C.S.; Michel, G.; Wengenroth, L.; von der Weid, N.X.; Bergstraesser, E.; Kuehni, C.E. Physical Performance Limitations in Adolescent and Adult Survivors of Childhood Cancer and Their Siblings. PLoS ONE 2012, 7, e47944. [Google Scholar] [CrossRef] [PubMed]
- Ballard-Barbash, R.; Friedenreich, C.M.; Courneya, K.S.; Siddiqi, S.M.; McTiernan, A.; Alfano, C.M. Physical activity, biomarkers, and disease outcomes in cancer survivors: A systematic review. J. Natl. Cancer Inst. 2012, 104, 815–840. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).