Comparison of the Effects of Sugammadex, Neostigmine, and Pyridostigmine on Postoperative Nausea and Vomiting: A Propensity Matched Study of Five Hospitals
Abstract
1. Introduction
2. Patients and Methods
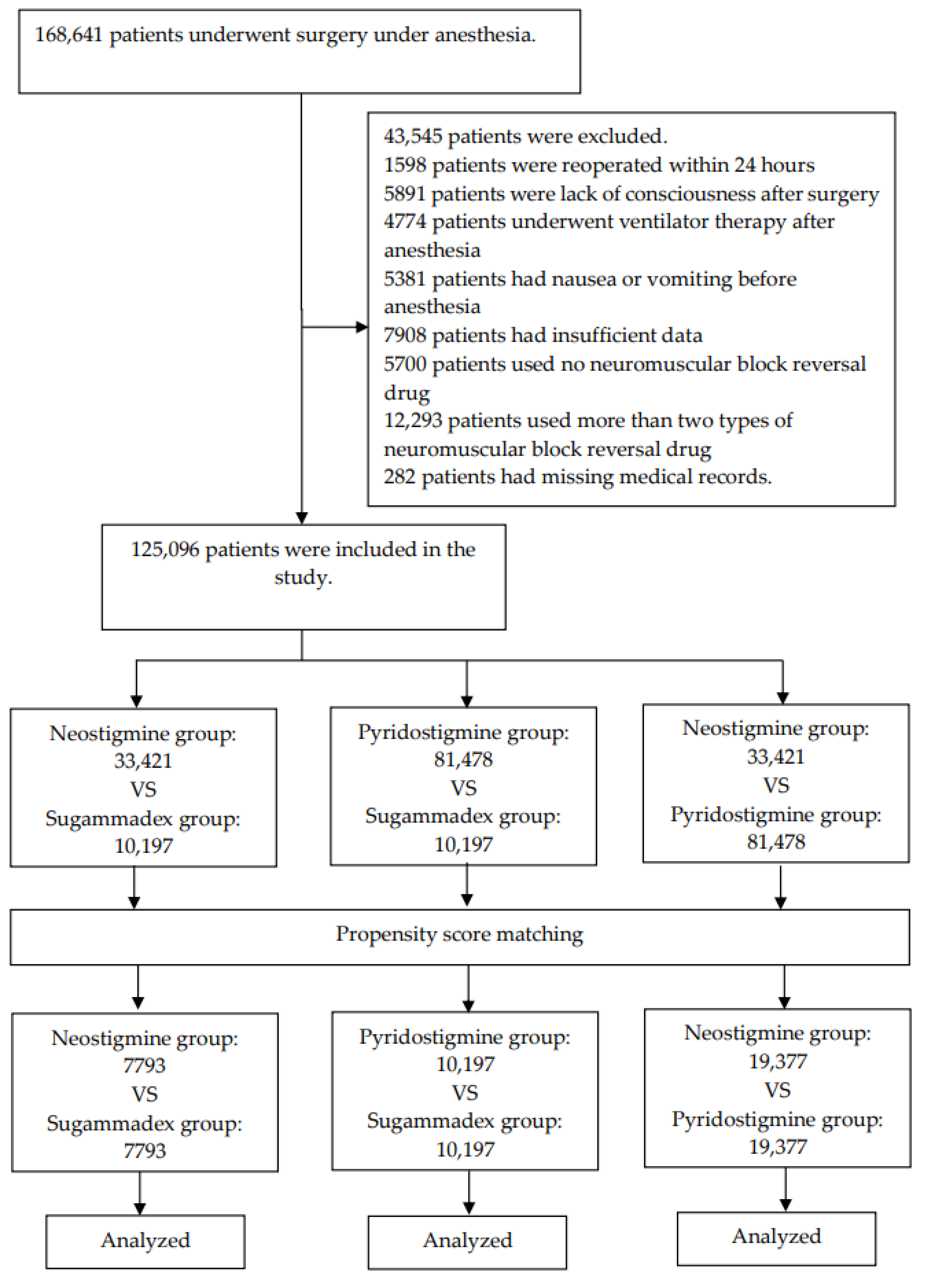
2.1. Patients
- Repeat surgery within 24 h after anesthesia
- Lack of consciousness after surgery
- Ventilator therapy after anesthesia
- Nausea or vomiting before anesthesia
- Insufficient data because the follow-up duration was shorter than 24 h
- Neuromuscular block reversal drugs (NMBRD; sugammadex (Bridion, Kenilworth, NJ, USA), neostigmine (Neostigmine Methylsulfate Injection Daihan, Seoul, Korea), and pyridostigmine (Pyridomine, Seoul, Korea) are not used.
- Two or more types of NMBRD are used.
2.2. PONV, Neuromuscular Block Reversal Drugs and Covariates
2.3. Statistics
3. Results
3.1. Patient Characteristics
3.2. Occurrence and Odds Ratio of PONV
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Macario, A.; Weinger, M.; Carney, S.; Kim, A. Which Clinical Anesthesia Outcomes Are Important to Avoid? The Perspective of Patients. Anesth. Analg. 1999, 89, 652. [Google Scholar] [CrossRef] [PubMed]
- Tramer, M.R. Treatment of postoperative nausea and vomiting. BMJ 2003, 327, 762–763. [Google Scholar] [CrossRef] [PubMed]
- Apfel, C.C.; Kranke, P.; Katz, M.H.; Goepfert, C.; Papenfuss, T.; Rauch, S.; Heineck, R.; Greim, C.A.; Roewer, N. Volatile anaesthetics may be the main cause of early but not delayed postoperative vomiting: A randomized controlled trial of factorial design. Br. J. Anaesth. 2002, 88, 659–668. [Google Scholar] [CrossRef]
- Pierre, S.; Whelan, R. Nausea and vomiting after surgery. Contin. Educ. Anaesth. Crit. Care Pain 2013, 13, 28–32. [Google Scholar] [CrossRef]
- Watcha, M.F.; White, P.F. Postoperative nausea and vomiting. Its etiology, treatment, and prevention. Anesthesiology 1992, 77, 162–184. [Google Scholar] [CrossRef]
- Kwon, Y.S.; Choi, J.W.; Lee, H.S.; Kim, J.H.; Kim, Y.; Lee, J.J. Effect of a Preoperative Proton Pump Inhibitor and Gastroesophageal Reflux Disease on Postoperative Nausea and Vomiting. J. Clin. Med. 2020, 9, 825. [Google Scholar] [CrossRef]
- Kim, J.H.; Hong, M.; Kim, Y.J.; Lee, H.S.; Kwon, Y.S.; Lee, J.J. Effect of Body Mass Index on Postoperative Nausea and Vomiting: Propensity Analysis. J. Clin. Med. 2020, 9, 1612. [Google Scholar] [CrossRef]
- Tramer, M.; Fuchs-Buder, T. Omitting antagonism of neuromuscular block: Effect on postoperative nausea and vomiting and risk of residual paralysis. A systematic review. Br. J. Anaesth. 1999, 82, 379–386. [Google Scholar] [CrossRef] [PubMed]
- Cheng, C.-R.; Sessler, D.I.; Apfel, C.C. Does neostigmine administration produce a clinically important increase in postoperative nausea and vomiting? Anesth. Analg. 2005, 101, 1349–1355. [Google Scholar] [CrossRef] [PubMed]
- Butterworth, J.F.; Mackey, D.C.; Wasnick, J.D. Morgan and Mikhail’s Clinical Anesthesiology, 6th ed.; McGraw-Hill Education: New York, NY, USA, 2018. [Google Scholar]
- Nair, V.P.; Hunter, J.M. Anticholinesterases and anticholinergic drugs. Contin. Educ. Anaesth. Crit. Care Pain 2004, 4, 164–168. [Google Scholar] [CrossRef]
- Yağan, Ö.; Taş, N.; Mutlu, T.; Hancı, V. Comparison of the effects of sugammadex and neostigmine on postoperative nausea and vomiting. Braz. J. Anesthesiol. 2017, 67, 147–152. [Google Scholar] [CrossRef]
- Yang, L.P.H.; Keam, S.J. Sugammadex. Drugs 2009, 69, 919–942. [Google Scholar] [CrossRef]
- Austin, P.C. A critical appraisal of propensity-score matching in the medical literature between 1996 and 2003. Stat. Med. 2008, 27, 2037–2049. [Google Scholar] [CrossRef] [PubMed]
- Joffe, M.M.; Rosenbaum, P.R. Invited commentary: Propensity scores. Am. J. Epidemiol. 1999, 150, 327–333. [Google Scholar] [CrossRef]
- Brookhart, M.A.; Schneeweiss, S.; Rothman, K.J.; Glynn, R.J.; Avorn, J.; Stürmer, T. Variable selection for propensity score models. Am. J. Epidemiol. 2006, 163, 1149–1156. [Google Scholar] [CrossRef]
- Tas Tuna, A.; Palabiyik, O.; Orhan, M.; Sonbahar, T.; Sayhan, H.; Tomak, Y. Does sugammadex administration affect postoperative nausea and vomiting after laparoscopic cholecystectomy: A prospective, double-blind, randomized study. Surg. Laparosc. Endosc. Percutaneous Tech. 2017, 27, 237–240. [Google Scholar] [CrossRef] [PubMed]
- Paech, M.J.; Kaye, R.; Baber, C.; Nathan, E.A. Recovery characteristics of patients receiving either sugammadex or neostigmine and glycopyrrolate for reversal of neuromuscular block: A randomised controlled trial. Anaesthesia 2018, 73, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Lee, O.H.; Choi, G.J.; Kang, H.; Baek, C.W.; Jung, Y.H.; Woo, Y.C.; Oh, J.; Park, Y.H. Effects of sugammadex vs. pyridostigmine-glycopyrrolate on post-operative nausea and vomiting: Propensity score matching. Acta Anaesthesiol. Scand. 2017, 61, 39–45. [Google Scholar] [CrossRef]
- Hristovska, A.M.; Duch, P.; Allingstrup, M.; Afshari, A. Efficacy and safety of sugammadex versus neostigmine in reversing neuromuscular blockade in adults. Cochrane Database Syst. Rev. 2017, 8, Cd012763. [Google Scholar] [CrossRef] [PubMed]
- Gan, T.J.; Belani, K.G.; Bergese, S.; Chung, F.; Diemunsch, P.; Habib, A.S.; Jin, Z.; Kovac, A.L.; Meyer, T.A.; Urman, R.D. Fourth Consensus Guidelines for the Management of Postoperative Nausea and Vomiting. Anesth. Analg. 2020, 131, 411–448. [Google Scholar] [CrossRef]
- Yi, M.S.; Kang, H.; Kim, M.K.; Choi, G.-J.; Park, Y.-H.; Baek, C.W.; Jung, Y.H.; Woo, Y.C. Relationship between the incidence and risk factors of postoperative nausea and vomiting in patients with intravenous patient-controlled analgesia. Asian J. Surg. 2018, 41, 301–306. [Google Scholar] [CrossRef]
- Kang, H.Y.; Park, S.W.; Lee, S.; Jeon, J.-M.; Oh, I.D.; Choi, J.-H. Effect of prophylactic palonosetron and sugammadex on postoperative nausea and vomiting in patients undergoing microvascular decompression under propofol-maintained anesthesia: A retrospective observational study. Medicine 2018, 97, e13237. [Google Scholar] [CrossRef]
- Hovorka, J.; Korttila, K.; Nelskyla, K.; Soikkeli, A.; Sarvela, J.; Paatero, H.; Halonen, P.; Yli-Hankala, A. Reversal of Neuromuscular Blockade with Neostigmine Has No Effect on the Incidence or Severity of Postoperative Nausea and Vomiting. Anesth. Analg. 1997, 85, 1359–1361. [Google Scholar] [CrossRef]
- Nelskylä, K.; Yli-Hankala, A.; Soikkeli, A.; Korttila, K. Neostigmine with glycopyrrolate does not increase the incidence or severity of postoperative nausea and vomiting in outpatients undergoing gynaecological laparoscopy. Br. J. Anaesth. 1998, 81, 757–760. [Google Scholar] [CrossRef][Green Version]
- Løvstad, R.; Thagaard, K.; Berner, N.; Raeder, J. Neostigmine 50 μg/kg with glycopyrrolate increases postoperative nausea in women after laparoscopic gynaecological surgery. Acta Anaesthesiol. Scand. 2001, 45, 495–500. [Google Scholar] [CrossRef] [PubMed]
- Baciarello, M.; Cornini, A.; Zasa, M.; Pedrona, P.; Scrofani, G.; Venuti, F.; Fanelli, G. Intrathecal atropine to prevent postoperative nausea and vomiting after Cesarean section: A randomized, controlled trial. Minerva Anestesiol. 2011, 77, 781. [Google Scholar] [CrossRef]
- Ishida, T.; Tachibana, H.; Ito, A.; Ikeda, S.; Furuta, K.; Nishiyama, A.; Noyama, M.; Tokioka, F.; Yoshioka, H.; Arita, M. Clinical characteristics of pneumonia in bedridden patients receiving home care: A 3-year prospective observational study. J. Infect. Chemother. 2015, 21, 587–591. [Google Scholar] [CrossRef] [PubMed]
- Tokuyasu, H.; Harada, T.; Watanabe, E.; Okazaki, R.; Touge, H.; Kawasaki, Y.; Shimizu, E. Effectiveness of meropenem for the treatment of aspiration pneumonia in elderly patients. Intern. Med. 2009, 48, 129–135. [Google Scholar] [CrossRef]
- Sanivarapu, R.R.; Gibson, J.G. Aspiration Pneumonia; StatPearls Publishing: Treasure Island, FL, USA, 2019. [Google Scholar]
- Bulka, C.M.; Terekhov, M.A.; Martin, B.J.; Dmochowski, R.R.; Hayes, R.M.; Ehrenfeld, J.M. Nondepolarizing neuromuscular blocking agents, reversal, and risk of postoperative pneumonia. J. Am. Soc. Anesthesiol. 2016, 125, 647–655. [Google Scholar] [CrossRef]
- Lawrence, V.A.; Cornell, J.E.; Smetana, G.W. Strategies to reduce postoperative pulmonary complications after noncardiothoracic surgery: Systematic review for the American College of Physicians. Ann. Intern. Med. 2006, 144, 596–608. [Google Scholar] [CrossRef] [PubMed]
- Kheterpal, S.; Vaughn, M.T.; Dubovoy, T.Z.; Shah, N.J.; Bash, L.D.; Colquhoun, D.A.; Shanks, A.M.; Mathis, M.R.; Soto, R.G.; Bardia, A. Sugammadex versus Neostigmine for Reversal of Neuromuscular Blockade and Postoperative Pulmonary Complications (STRONGER) A Multicenter Matched Cohort Analysis. Anesthesiol. J. Am. Soc. Anesthesiol. 2020, 132, 1371–1381. [Google Scholar]
- Apfel, C.C.; Roewer, N.; Korttila, K. How to study postoperative nausea and vomiting. Acta Anaesthesiol. Scand. 2002, 46, 921–928. [Google Scholar] [CrossRef] [PubMed]
- Hornby, P.J. Central neurocircuitry associated with emesis. Am. J. Med. 2001, 111, 106s–112s. [Google Scholar] [CrossRef]
- Gan, T.J. Risk Factors for Postoperative Nausea and Vomiting. Anesth. Analg. 2006, 102, 1884–1898. [Google Scholar] [CrossRef]
| Before Matching | After Matching | ||||||
|---|---|---|---|---|---|---|---|
| Neostigmine (n = 33,421) | Sugammadex (n = 10,197) | ASD | Neostigmine (n = 7793) | Sugammadex (n = 7793) | ASD | ||
| Demographic data | |||||||
| Age (years, median (IQR)) | 64 (39, 52) | 61 (48, 72) | 0.45 | 60 (49, 72) | 62(50, 73) | 0.05 | |
| Female sex (n, %) | 18,079 (54.1) | 4338 (42.5) | 0.23 | 3635 (46.6) | 3471 (44.5) | 0.07 | |
| Obesity (BMI ≥ 30 kg/m2) (n, %) | 2397 (7.2) | 924 (9.1) | 0.07 | 692 (8.9) | 644 (8.3) | 0.04 | |
| Type of surgery | |||||||
| Intraabdominal surgery (n, %) | 8820 (26.4) | 1943 (19.1) | 0.19 | 1647 (21.1) | 1658 (21.3) | 0.00 | |
| GY surgery (n, %) | 2758 (8.3) | 239 (2.3) | 0.39 | 299 (3.8) | 236 (3) | 0.05 | |
| ENT surgery (n, %) | 1351 (4) | 1346 (13.2) | 0.27 | 771 (9.9) | 841 (10.8) | 0.03 | |
| Anesthesia-related factors | |||||||
| ASA PS | 1 | 8534 (25.5) | 1943 (19.1) | 0.14 | 1428 (18.3) | 1156 (15.0) | 0.02 |
| (n, %) | 2 | 16,415 (49.1) | 5517 (54.1) | 3539 (45.4) | 4305 (55.2) | ||
| 3 | 7978 (23.9) | 2362 (23.2) | 2687 (34.5) | 1969 (25.3) | |||
| 4 | 491 (1.5) | 373 (3.7) | 139 (1.8) | 352 (4.5) | |||
| 5 | 3 (0) | 2 (0) | 0 (0) | 1 (0) | |||
| Anesthesia time (hours, median (IQR)) | 1.9 (1.3, 2.9) | 1.9 (1.1, 3.5) | 0.13 | 2.3 (1.5, 3.6) | 2.2 (1.2, 3.9) | 0.01 | |
| Inhalation anesthetics (n, %) | 32,575 (97.5) | 9461 (92.8) | 0.18 | 7312 (93.8) | 7288 (93.5) | 0.01 | |
| N2O (n, %) | 14 (0) | 2009 (19.7) | 0.49 | 14 (0.2) | 16 (0.2) | 0.00 | |
| Opioid (n, %) | 33,325 (99.7) | 9805 (96.2) | 0.19 | 7718 (99) | 7682 (98.6) | 0.02 | |
| Other factors | |||||||
| DM (n, %) | 4289 (12.8) | 1992 (19.5) | 0.17 | 1559 (20) | 1600 (20.5) | 0.01 | |
| Current smoker (n, %) | 5250 (15.7) | 1821 (17.9) | 0.06 | 1265 (16.2) | 1329 (17.1) | 0.02 | |
| Emergency (n, %) | 6508 (19.5) | 1426 (14) | 0.16 | 1109 (14.2) | 1087 (13.9) | 0.02 | |
| Steroid (n, %) | 1150 (3.4) | 916 (9) | 0.19 | 473 (6.1) | 481 (6.2) | 0.00 | |
| Transfusion (n, %) | 1098 (3.3) | 334 (3.3) | 0.00 | 290 (3.7) | 277 (3.6) | 0.01 | |
| Antiemetics (n, %) | 15,426 (46.2) | 6987 (68.5) | 0.48 | 4725 (60.6) | 4729 (60.7) | 0.00 | |
| PCA (n, %) | 14,682 (43.9) | 5568 (54.6) | 0.21 | 4261 (54.7) | 4228 (54.3) | 0.01 | |
| Before Matching | After Matching | ||||||
|---|---|---|---|---|---|---|---|
| Pyridostigmine (n = 81,478) | Sugammadex (n = 10,197) | ASD | Pyridostigmine (n = 10,197) | Sugammadex (n = 10,197) | ASD | ||
| Demographic data | |||||||
| Age (years, median (IQR)) | 49 (36, 61) | 61 (48, 72) | 0.61 | 61 (49, 72) | 61 (48, 72) | 0.00 | |
| Female sex (n, %) | 41,752 (51.2) | 4338 (42.5) | 0.18 | 4340 (42.6) | 4338 (42.5) | 0.01 | |
| Obesity (BMI ≥ 30 kg/m2) (n, %) | 6353 (7.8) | 924 (9.1) | 0.04 | 887 (8.7) | 924 (9.1) | 0.00 | |
| Type of surgery | |||||||
| Intraabdominal surgery (n, %) | 13,670 (16.8) | 1943 (19.1) | 0.06 | 1862 (18.3) | 1943 (19.1) | 0.02 | |
| GY surgery (n, %) | 10,894 (13.4) | 239 (2.3) | 0.73 | 228 (2.2) | 239 (2.3) | 0.01 | |
| ENT surgery (n, %) | 12,077 (14.8) | 1346 (13.2) | 0.05 | 1373 (13.5) | 1346 (13.2) | 0.01 | |
| Anesthesia-related factors | |||||||
| ASA PS | 1 | 36,062 (44.3) | 1943 (19.1) | 0.62 | 1911 (18.7) | 1943 (19.1) | 0.01 |
| (n, %) | 2 | 37,908 (46.5) | 5517 (54.1) | 5513 (54.1) | 5517 (54.1) | ||
| 3 | 7142 (8.8) | 2362 (23.2) | 2564 (25.1) | 2362 (23.2) | |||
| 4 | 366 (0.4) | 373 (3.7) | 209 (2) | 373 (3.7) | |||
| 5 | 0 (0) | 2 (0) | 0 (0) | 2 (0) | |||
| Anesthesia time (hours, median (IQR)) | 1.8 (1.2, 2.6) | 1.9 (1.1, 3.5) | 0.27 | 2.1 (1.3, 3.3) | 1.9 (1.1, 3.5) | 0.01 | |
| Inhalation anesthetics (n, %) | 77,576 (95.2) | 9461 (92.8) | 0.09 | 9413 (92.3) | 9461 (92.8) | 0.02 | |
| N2O (n, %) | 18,431 (22.6) | 2009 (19.7) | 0.07 | 2100 (20.6) | 2009 (19.7) | 0.02 | |
| Opioid (n, %) | 73,008 (89.6) | 9805 (96.2) | 0.34 | 9832 (96.4) | 9805 (96.2) | 0.01 | |
| Other factors | |||||||
| DM (n, %) | 4289 (12.8) | 1992 (19.5) | 0.17 | 1559 (20) | 1600 (20.5) | 0.01 | |
| Current smoker (n, %) | 5250 (15.7) | 1821 (17.9) | 0.06 | 1265 (16.2) | 1329 (17.1) | 0.02 | |
| Emergency (n, %) | 6508 (19.5) | 1426 (14) | 0.16 | 1109 (14.2) | 1087 (13.9) | 0.02 | |
| Steroid (n, %) | 9818 (12) | 1992 (19.5) | 0.19 | 1945 (19.1) | 1992 (19.5) | 0.01 | |
| Transfusion (n, %) | 15,891 (19.5) | 1821 (17.9) | 0.04 | 1748 (17.1) | 1821 (17.9) | 0.02 | |
| Antiemetics (n, %) | 47,313 (58.1) | 6987 (68.5) | 0.23 | 7048 (69.1) | 6987 (68.5) | 0.01 | |
| PCA (n, %) | 37,584 (46.1) | 5568 (54.6) | 0.17 | 5510 (54) | 5568 (54.6) | 0.01 | |
| Before Matching | After Matching | ||||||
|---|---|---|---|---|---|---|---|
| Neostigmine (n = 33,421) | Pyridostigmine (n = 81,478) | ASD | Neostigmine (n = 19,377) | Pyridostigmine (n = 19,377) | ASD | ||
| Demographic data | |||||||
| Age (years, median (IQR)) | 64 (39, 52) | 49 (36, 61) | 0.16 | 51 (38, 62) | 51 (38, 63) | 0.03 | |
| Female sex (n, %) | 18,079 (54.1) | 41,752 (51.2) | 0.06 | 10,205 (52.7) | 10,590 (54.7) | 0.04 | |
| Obesity (BMI ≥ 30 kg/m2) (n, %) | 2397 (7.2) | 6353 (7.8) | 0.05 | 1403 (7.2) | 1544 (8.0) | 0.06 | |
| Type of surgery | |||||||
| Intraabdominal surgery (n, %) | 8820 (26.4) | 13,670 (16.8) | 0.32 | 4256 (22.0) | 4158 (21.5) | 0.02 | |
| GY surgery (n, %) | 2758 (8.3) | 10,894 (13.4) | 0.30 | 2086 (10.8) | 2358 (12.2) | 0.08 | |
| ENT surgery (n, %) | 1351 (4) | 12,077 (14.8) | 0.78 | 1184 (6.1) | 1148 (5.9) | 0.02 | |
| Anesthesia-related factors | |||||||
| ASA PS | 1 | 8534 (25.5) | 36,062 (44.3) | 0.53 | 6188 (3193) | 6073 (31.3) | 0.01 |
| (n, %) | 2 | 16,415 (49.1) | 37,908 (46.5) | 9772 (50.4) | 10,174 (52.5) | ||
| 3 | 7978 (23.9) | 7142 (8.8) | 3245 (16.7) | 2959 (15.3) | |||
| 4 | 491 (1.5) | 366 (0.4) | 172 (0.9) | 171 (0.9) | |||
| 5 | 3 (0) | 0 (0) | 0 (0) | 0 (0) | |||
| Anesthesia time (hours, median (IQR)) | 1.9 (1.3, 2.9) | 1.8 (1.2, 2.6) | 0.20 | 1.9 (1.3, 2.9) | 1.9 (1.3, 2.9) | 0.04 | |
| Inhalation anesthetics (n, %) | 32,575 (97.5) | 77,576 (95.2) | 0.36 | 18,840 (97.2) | 18,994 (98.0) | 0.19 | |
| N2O (n, %) | 14 (0) | 18,431 (22.6) | 3.61 | 14 (0.1) | 12 (0.1) | 0.09 | |
| Opioid (n, %) | 33,325 (99.7) | 73,008 (89.6) | 2.04 | 19,282 (99.5) | 19,294 (99.6) | 0.07 | |
| Other factors | |||||||
| DM (n, %) | 4289 (12.8) | 9818 (12) | 0.04 | 2349 (12.1) | 2496 (12.9) | 0.04 | |
| Current smoker (n, %) | 5250 (15.7) | 15,891 (19.5) | 0.14 | 3424 (16.2) | 3477 (17.9) | 0.01 | |
| Emergency (n, %) | 6508 (19.5) | 14,712 (18.1) | 0.05 | 3739 (19.3) | 3636 (18.2) | 0.02 | |
| Steroid (n, %) | 9818 (12) | 1992 (19.5) | 0.19 | 1945 (19.1) | 1992 (19.5) | 0.01 | |
| Transfusion (n, %) | 1098 (3.3) | 1260 (1.5) | 0.42 | 420 (3.7) | 482 (3.6) | 0.08 | |
| Antiemetics (n, %) | 15,426 (46.2) | 47,313 (58.1) | 0.26 | 9523 (49.1) | 8881 (45.8) | 0.07 | |
| PCA (n, %) | 14,682 (43.9) | 37,584 (46.1) | 0.05 | 4261 (46.2) | 4228 (42.9) | 0.07 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, J.H.; Lim, M.-S.; Choi, J.W.; Kim, H.; Kwon, Y.-S.; Lee, J.J. Comparison of the Effects of Sugammadex, Neostigmine, and Pyridostigmine on Postoperative Nausea and Vomiting: A Propensity Matched Study of Five Hospitals. J. Clin. Med. 2020, 9, 3477. https://doi.org/10.3390/jcm9113477
Kim JH, Lim M-S, Choi JW, Kim H, Kwon Y-S, Lee JJ. Comparison of the Effects of Sugammadex, Neostigmine, and Pyridostigmine on Postoperative Nausea and Vomiting: A Propensity Matched Study of Five Hospitals. Journal of Clinical Medicine. 2020; 9(11):3477. https://doi.org/10.3390/jcm9113477
Chicago/Turabian StyleKim, Jong Ho, Man-Sup Lim, Jun Woo Choi, Haewon Kim, Young-Suk Kwon, and Jae Jun Lee. 2020. "Comparison of the Effects of Sugammadex, Neostigmine, and Pyridostigmine on Postoperative Nausea and Vomiting: A Propensity Matched Study of Five Hospitals" Journal of Clinical Medicine 9, no. 11: 3477. https://doi.org/10.3390/jcm9113477
APA StyleKim, J. H., Lim, M.-S., Choi, J. W., Kim, H., Kwon, Y.-S., & Lee, J. J. (2020). Comparison of the Effects of Sugammadex, Neostigmine, and Pyridostigmine on Postoperative Nausea and Vomiting: A Propensity Matched Study of Five Hospitals. Journal of Clinical Medicine, 9(11), 3477. https://doi.org/10.3390/jcm9113477





