Adult Diabetes and Prediabetes Prevalence in Kuwait: Data from the Cross-Sectional Kuwait Diabetes Epidemiology Program
Abstract
1. Introduction
2. Experimental Section
2.1. Participants and Study Design
2.2. Data Collection
2.3. Definition of Prediabetes and Diabetes
2.4. Statistical Analysis
2.5. Ethical Consideration
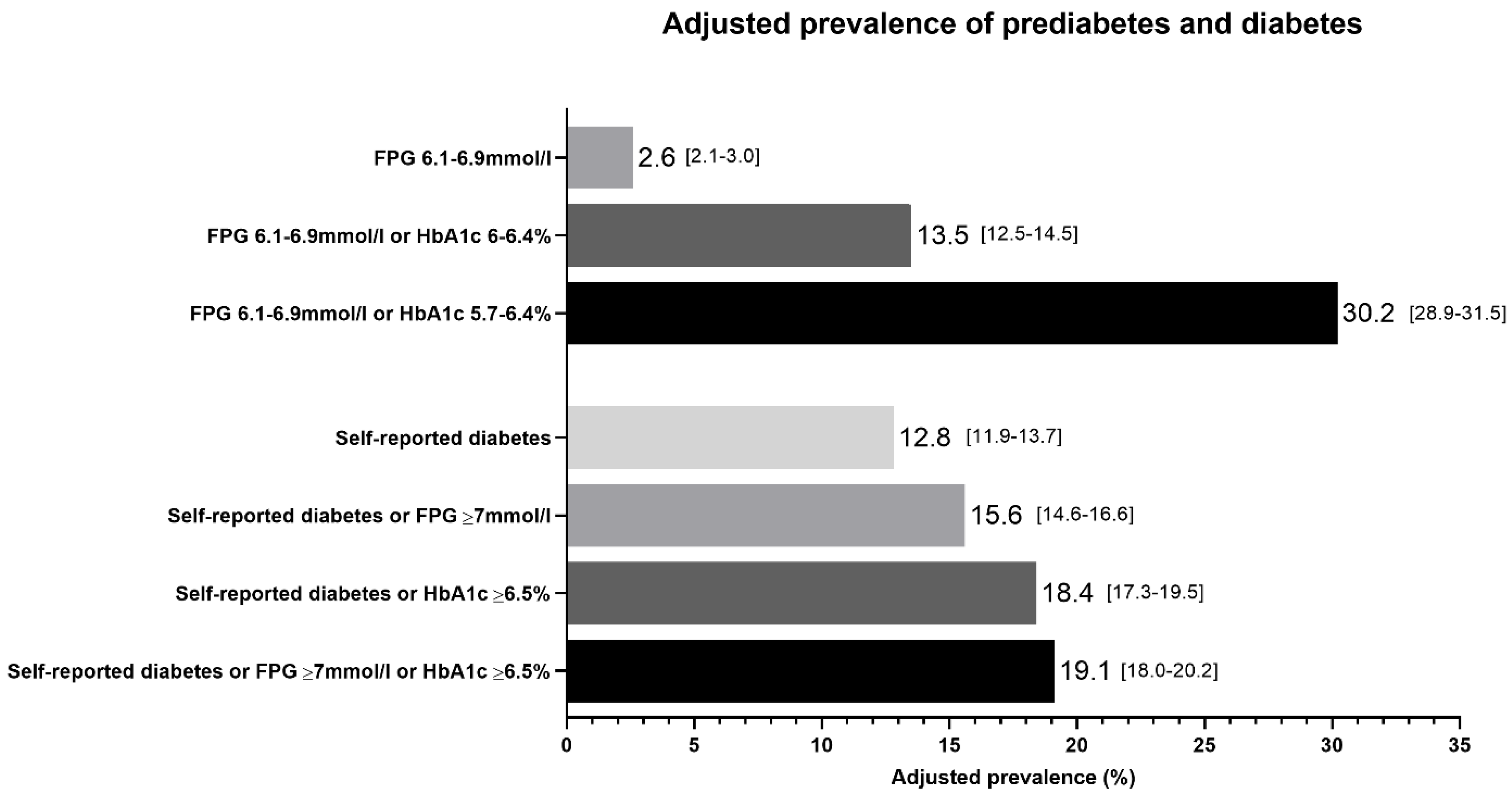
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- International Diabetes Federation. IDF Atlas, 9th ed.; IDF: Brussels, Belgium, 2019. [Google Scholar]
- The Public Authority For Civil Information. Statistical Reports. Available online: https://www.paci.gov.kw/stat (accessed on 31 December 2019).
- Weiderpass, E.; Botteri, E.; Longenecker, J.C.; Alkandari, A.; Al-Wotayan, R.; Al Duwairi, Q.; Tuomilehto, J. The Prevalence of Overweight and Obesity in an Adult Kuwaiti Population in 2014. Front. Endocrinol. 2019, 10, 10. [Google Scholar] [CrossRef] [PubMed]
- Alkandari, A.; Longenecker, J.C.; Barengo, N.C.; Alkhatib, A.; Weiderpass, E.; Al-Wotayan, R.; Al Duwairi, Q.; Tuomilehto, J. The prevalence of pre-diabetes and diabetes in the Kuwaiti adult population in 2014. Diabetes Res. Clin. Pr. 2018, 144, 213–223. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Status Report on Noncommunicable Diseases; WHO: Geneva, Switzerland, 2014. [Google Scholar]
- Elkum, N.; Al-Arouj, M.; Sharifi, M.; Behbehani, K.; Bennakhi, A. Cardiovascular disease risk factors in the South Asian population living in Kuwait: A cross-sectional study. Diabet. Med. 2014, 31, 531–539. [Google Scholar] [CrossRef] [PubMed]
- The World Health Organization. STEPwise Approach to Surveillance (STEPS); WHO: Geneva, Switzerland, 2014. [Google Scholar]
- The World Health Organization. Definition and Diagnosis of Diabetes Mellitus and Intermediate Hyperglycaemia: REPORT of a WHO/IDF Consultation; WHO: Geneva, Switzerland, 2006. [Google Scholar]
- The International Expert Committee International Expert Committee Report on the Role of the A1C Assay in the Diagnosis of Diabetes. Diabetes Care 2009, 32, 1327–1334. [CrossRef]
- Alarouj, M.; Bennakhi, A.; Alnesef, Y.; Sharifi, M.; Elkum, N. Diabetes and associated cardiovascular risk factors in the State of Kuwait: The first national survey. Int. J. Clin. Pr. 2012, 67, 89–96. [Google Scholar] [CrossRef]
- Khalil, S.H.A.; Megallaa, M.H.; Rohoma, K.H.; Ismael, H.; Abouseif, M.; Kharboush, I.; Elkaffash, D.; Hassanein, M.; Wahab, M.M.A.; Malaty, A.; et al. Prevalence of type 2 diabetes mellitus in a sample of the adult population of Alexandria, Egypt. Diabetes Res. Clin. Pr. 2018, 144, 63–73. [Google Scholar] [CrossRef]
- Albache, N.; Al Ali, R.; Rastam, S.; Fouad, F.M.; Mzayek, F.; Maziak, W.; Rastam, S. Epidemiology of Type 2 diabetes mellitus in Aleppo, Syria. J. Diabetes 2009, 2, 85–91. [Google Scholar] [CrossRef]
- Nasrallah, M.P.; Nakhoul, N.F.; Nasreddine, L.; Mouneimne, Y.; Abiad, M.G.; Ismaeel, H.; Tamim, H.M. Prevalence of Diabetes in Greater Beirut Area: Worsening Over Time. Endocr. Pr. 2017, 23, 1091–1100. [Google Scholar] [CrossRef]
- Ajlouni, K.; Khader, Y.; Batieha, A.; Ajlouni, H.; El-Khateeb, M. An increase in prevalence of diabetes mellitus in Jordan over 10 years. J. Diabetes Complicat. 2008, 22, 317–324. [Google Scholar] [CrossRef]
- Tandon, N.; Anjana, R.M.; Mohan, V.; Kaur, T.; Afshin, A.; Ong, K.; Mukhopadhyay, S.; Thomas, N.; Bhatia, E.; Krishnan, A.; et al. The increasing burden of diabetes and variations among the states of India: The Global Burden of Disease Study 1990–2016. Lancet Glob. Heal. 2018, 6, e1352–e1362. [Google Scholar] [CrossRef]
- Katulanda, P.; Constantine, G.R.; Mahesh, J.G.; Sheriff, R.; Seneviratne, R.D.A.; Wijeratne, S.; Wijesuriya, M.; McCarthy, M.I.; Adler, A.I.; Matthews, D.R. Prevalence and projections of diabetes and pre-diabetes in adults in Sri Lanka-Sri Lanka Diabetes, Cardiovascular Study (SLDCS). Diabet. Med. 2008, 25, 1062–1069. [Google Scholar] [CrossRef] [PubMed]
- Akter, S.; Rahman, M.M.; Abe, S.K.; Sultana, P. Prevalence of diabetes and prediabetes and their risk factors among Bangladeshi adults: A nationwide survey. Bull. World Heal. Organ. 2014, 92, 204–213. [Google Scholar] [CrossRef] [PubMed]
- Aamir, A.H.; Ul-Haq, Z.; Mahar, S.A.; Qureshi, F.M.; Ahmad, I.; Jawa, A.; Sheikh, A.; Raza, A.; Fazid, S.; Jadoon, Z.; et al. Diabetes Prevalence Survey of Pakistan (DPS-PAK): Prevalence of type 2 diabetes mellitus and prediabetes using HbA1c: A population-based survey from Pakistan. BMJ Open 2019, 9, e025300. [Google Scholar] [CrossRef] [PubMed]
- Malik, M.; Bakir, A.; Saab, B.A.; Roglic, G.; King, H. Glucose intolerance and associated factors in the multi-ethnic population of the United Arab Emirates: Results of a national survey. Diabetes Res. Clin. Pr. 2005, 69, 188–195. [Google Scholar] [CrossRef]
- Mather, H.M.; Keen, H. The Southall Diabetes Survey: Prevalence of known diabetes in Asians and Europeans. BMJ 1985, 291, 1081–1084. [Google Scholar] [CrossRef]
- Misra, R.; Patel, T.; Kotha, P.; Raji, A.; Ganda, O.; Banerji, M.; Shah, V.; Vijay, K.; Mudaliar, S.; Iyer, D.; et al. Prevalence of diabetes, metabolic syndrome, and cardiovascular risk factors in US Asian Indians: Results from a national study. J. Diabetes Complicat. 2010, 24, 145–153. [Google Scholar] [CrossRef]
- Esteghamati, A.; Etemad, K.; Koohpayehzadeh, J.; Abbasi, M.; Meysamie, A.; Noshad, S.; Asgari, F.; Mousavizadeh, M.; Rafei, A.; Khajeh, E.; et al. Trends in the prevalence of diabetes and impaired fasting glucose in association with obesity in Iran: 2005–2011. Diabetes Res. Clin. Pr. 2014, 103, 319–327. [Google Scholar] [CrossRef]
- Jimeno, C.A. Prevalence of diabetes mellitus and pre-diabetes in the Philippines: A sub-study of the 7th National Nutrition and Health Survey (2008). Philipp J. Int. Med. 2015, 53, 1–8. [Google Scholar]
- Morgan, S.A.; Ali, M.A.M.; Channon, A.A.; Al-Sabahi, S.; Al Suwaidi, H.; Osman, N.; Al Salameen, M.; Khoja, T. Prevalence and correlates of diabetes and its comorbidities in four Gulf Cooperation Council countries: Evidence from the World Health Survey Plus. J. Epidemiol. Community Heal. 2019, 73, 630–636. [Google Scholar] [CrossRef]
- Cheng, Y.J.; Kanaya, A.M.; Araneta, M.R.G.; Saydah, S.H.; Kahn, H.S.; Gregg, E.W.; Fujimoto, W.Y.; Imperatore, G. Prevalence of Diabetes by Race and Ethnicity in the United States, 2011–2016. JAMA 2019, 322, 2389–2398. [Google Scholar] [CrossRef]
- Powers, M.A. Diabetes Self-Management Education and Support in Type 2 Diabetes: A Joint Position Statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics. J. Acad. Nutr. Diet. 2015, 115, 1323–1334. [Google Scholar] [CrossRef] [PubMed]
- Danaei, G.; Fahimi, S.; Lu, Y.; Zhou, B.; Hajifathalian, K.; Di Cesare, M.; Lo, W.-C.; Reis-Santos, B.; Cowan, M.J.; Shaw, J.E.; et al. Effects of diabetes definition on global surveillance of diabetes prevalence and diagnosis: A pooled analysis of 96 population-based studies with 331288 participants. Lancet Diabetes Endocrinol. 2015, 3, 624–637. [Google Scholar] [CrossRef]
- Farmanfarma, K.K.; Ansari-Moghaddam, A.; Zareban, I.; Adineh, H. Prevalence of type 2 diabetes in Middle–East: Systematic review& meta-analysis. Prim. Care Diabetes 2020, 14, 297–304. [Google Scholar]
- Abdella, N.; Khogali, M.; Al-Ali, S.; Gumaa, K.; Bajaj, J. Known type 2 diabetes mellitus among the Kuwaiti population. A prevalence study. Acta Diabetol. 1996, 33, 145–149. [Google Scholar] [CrossRef] [PubMed]
- Chan, J.M.; Rimm, E.B.; Colditz, G.A.; Stampfer, M.J.; Willett, W.C. Obesity, Fat Distribution, and Weight Gain as Risk Factors for Clinical Diabetes in Men. Diabetes Care 1994, 17, 961–969. [Google Scholar] [CrossRef]
- Borrell, L.N.; Dallo, F.J.; White, K. Education and Diabetes in a Racially and Ethnically Diverse Population. Am. J. Public Heal. 2006, 96, 1637–1642. [Google Scholar] [CrossRef] [PubMed]
- Seeman, T.; Merkin, S.S.; Crimmins, E.M.; Koretz, B.; Charette, S.; Karlamangla, A.S. Education, income and ethnic differences in cumulative biological risk profiles in a national sample of US adults: NHANES III (1988–1994). Soc. Sci. Med. 2008, 66, 72–87. [Google Scholar] [CrossRef]
- Vandenheede, H.; Deboosere, P.; Espelt, A.; Bopp, M.; Borrell, C.; Costa, G.; Eikemo, T.A.; Gnavi, R.; Hoffmann, R.; Kulhanova, I.; et al. Educational inequalities in diabetes mortality across Europe in the 2000s: The interaction with gender. Int. J. Public Heal. 2015, 60, 401–410. [Google Scholar] [CrossRef]
- Agardh, E.; Allebeck, P.; Hallqvist, J.; Moradi, T.; Sidorchuk, A. Type 2 diabetes incidence and socio-economic position: A systematic review and meta-analysis. Int. J. Epidemiol. 2011, 40, 804–818. [Google Scholar] [CrossRef]
- Seiglie, J.A.; Marcus, M.-E.; Ebert, C.; Prodromidis, N.; Geldsetzer, P.; Theilmann, M.; Agoudavi, K.; Andall-Brereton, G.; Aryal, K.K.; Bicaba, B.W.; et al. Diabetes Prevalence and Its Relationship with Education, Wealth, and BMI in 29 Low- and Middle-Income Countries. Diabetes Care 2020, 43, 767–775. [Google Scholar] [CrossRef]
- Saeedi, P.; Petersohn, I.; Salpea, P.; Malanda, B.; Karuranga, S.; Unwin, N.; Colagiuri, S.; Guariguata, L.; Motala, A.A.; Ogurtsova, K.; et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas, 9th edition. Diabetes Res. Clin. Pr. 2019, 157, 107843. [Google Scholar] [CrossRef] [PubMed]
- Moussa, M.A.; Alsaeid, M.; Abdella, N.; Refai, T.M.; Al-Sheikh, N.; Gomez, J.E. Prevalence of Type 2 Diabetes Mellitus among Kuwaiti Children and Adolescents. Med. Princ. Pr. 2008, 17, 270–275. [Google Scholar] [CrossRef]
- Elkum, N.; Al-Arouj, M.; Sharifi, M.; Shaltout, A.; Bennakhi, A. Prevalence of childhood obesity in the state of Kuwait. Pediatr. Obes. 2015, 11, e30–e34. [Google Scholar] [CrossRef] [PubMed]
- The DECODE Study Group; European Diabetes Epidemiology Group; Diabetes Epidemiology: Collaborative analysis of Diagnostic criteria in Europe. Glucose tolerance and mortality: Comparison of WHO and American Diabetes Association diagnostic criteria. Lancet 1999, 354, 617–621. [Google Scholar]
- Cowie, C.C.; Rust, K.F.; Byrd-Holt, D.D.; Gregg, E.W.; Ford, E.S.; Geiss, L.S.; Bainbridge, K.E.; Fradkin, J.E. Prevalence of Diabetes and High Risk for Diabetes Using A1C Criteria in the U.S. Population in 1988–2006. Diabetes Care 2010, 33, 562–568. [Google Scholar] [CrossRef]
- Shaltout, A.A.; Wake, D.; Thanaraj, T.A.; Omar, D.M.; Al-Abdulrazzaq, D.; Channanath, A.; Alkandari, H.; Abdulrasoul, M.; Miller, S.; Conway, N.; et al. Incidence of type 1 diabetes has doubled in Kuwaiti children 0–14 years over the last 20 years. Pediatr. Diabetes 2016, 18, 761–766. [Google Scholar] [CrossRef]
- Alsukait, R.; Bleich, S.N.; Wilde, P.; Singh, G.; Folta, S.C. Sugary drink excise tax policy process and implementation: Case study from Saudi Arabia. Food Policy 2020, 90, 101789. [Google Scholar] [CrossRef]
- Magliano, D.J.; Islam, R.M.; Barr, E.L.M.; Gregg, E.W.; Pavkov, M.E.; Harding, J.L.; Tabesh, M.; Koye, D.N.; Shaw, J.E. Trends in incidence of total or type 2 diabetes: Systematic review. BMJ 2019, 366, l5003. [Google Scholar] [CrossRef]
| Sex | Nationality | ||||||
|---|---|---|---|---|---|---|---|
| Characteristic | Total | Male | Female | p | Kuwaiti | Non-Kuwaiti | p |
| n (% total) | 4937 (100) | 2773 (56.2) | 2164 (43.8) | 1684 (34.1) | 3253 (65.9) | ||
| Mean age (years) | 44.1 (10.4) | 44.6 (10.4) | 43.4 (10.3) | <0.0001 | 46.7 (10.7) | 42.7 (9.9) | <0.0001 |
| Mean BMI (kg/m2) | 30.1 (5.8) | 29.5 (5.28) | 30.9 (6.41) | <0.0001 | 31.2 (5.7) | 29.6 (5.8) | <0.0001 |
| Mean HbA1c (%) | 6.16 (1.5) | 6.28 (1.56) | 6.0 (1.4) | <0.0001 | 6.27 (1.54) | 6.1 (1.47) | 0.0001 |
| Mean FPG (mmol/L) | 5.95 (2.29) | 6.17 (2.39) | 5.67 (2.12) | <0.0001 | 6.45 (2.4) | 5.84 (2.22) | <0.0001 |
| Mean systolic BP (mmHg) | 130 (21.1) | 135 (20.9) | 125 (20) | <0.0001 | 126 (18.8) | 132 (22) | <0.0001 |
| Mean diastolic BP (mmHg) | 79 (12.1) | 81 (12.0) | 77 (11.9) | <0.0001 | 77 (11.2) | 81 (12.3) | <0.0001 |
| Mean waist–hip ratio (cm/cm) | 0.91 (0.07) | 0.94 (0.06) | 0.88 (0.07) | <0.0001 | 0.92 (0.06) | 0.91 (0.07) | 0.61 |
| Self-reported hypertension (n) | 1002 (20.9) | 593 (22.1) | 409 (19.3) | 0.02 | 380 (22.6) | 622 (19.9) | 0.027 |
| Self-reported dyslipidaemia (n) | 1046 (22.6) | 624 (24.1) | 422 (20.6) | 0.004 | 409 (24.5) | 637 (21.5) | 0.02 |
| Family history of diabetes (n) | 2807 (61.0) | 1567 (60.1) | 1240 (62.2) | 0.16 | 1178 (78.1) | 1629 (52.7) | <0.0001 |
| University educated (n) | 2807 (56.9) | 1549 (55.9) | 1258 (58.1) | 0.11 | 1166 (69.2) | 1641 (50.5) | <0.0001 |
| >1000 KD monthly household income (n) | 1778 (44.4) | 1001 (42.7) | 777 (46.9) | 0.008 | 1321 (92.4) | 457 (17.8) | <0.0001 |
| Prediabetes Prevalence | Diabetes Prevalence | ||||
|---|---|---|---|---|---|
| Characteristic | n | % [95% CI] | p | % [95% CI] | p |
| Overall | 4937 | 13.5 [12.5–14.5] | 19.1 [18.0–20.2] | ||
| Sex | 0.0008 | <0.0001 | |||
| Men | 2773 | 14.8 [13.5–16.2] | 22.4 [20.9–24.0] | ||
| Women | 2164 | 11.5 [10.2–12.9] | 14.4 [13.0–15.9] | ||
| Nationality | 0.002 | 0.003 | |||
| Kuwaiti | 1684 | 11.1 [9.7–12.7] | 21.8 [19.9–23.8] | ||
| Non-Kuwaiti | 3253 | 14.3 [13.1–15.5] | 18.2 [16.9–19.6] | ||
| Non-Kuwaiti ethnicities | 0.005 | 0.0004 | |||
| Arab | 1615 | 12.5 [11.0–14.2] | 19.1 [17.3–21.1] | ||
| Iranian | 150 | 11.3 [7.1–17.3] | 15.2 [10.4–21.8] | ||
| South Asian | 1051 | 17.2 [15.0–19.6] | 20.2 [17.8–22.7] | ||
| Southeast Asian | 407 | 14.7 [11.6–18.5] | 11.1 [8.4–14.5] | ||
| Age group | 0.001 | <0.0001 | |||
| 20–29 | 370 | 8.4 [6.0–11.6] | 5.4 [3.5–8.2] | ||
| 30–44 | 2282 | 14.3 [12.9–15.8] | 14.2 [12.9–15.7] | ||
| 45–59 | 1889 | 18.6 [16.9–20.4] | 38.7 [36.5–40.9] | ||
| 60+ | 396 | 12.2 [9.3–15.7] | 64.8 [60.0–69.4] | ||
| Obesity category | 0.002 | <0.0001 | |||
| Normal BMI | 825 | 9.7 [7.9–11.9] | 8.4 [6.7–10.5] | ||
| Overweight | 1888 | 14.4 [12.8–16.0] | 17.6 [16.0–19.4] | ||
| Obese | 2219 | 14.8 [13.4–16.3] | 26.7 [24.9–28.6] | ||
| Waist–hip ratio | <0.0001 | <0.0001 | |||
| Normal | 1231 | 9.1 [7.6–10.8] | 7.1 [5.8–8.6] | ||
| Elevated | 3664 | 15.7 [14.6–16.9] | 25.1 [23.7–26.5] | ||
| Self-reported hypertension | 0.63 | <0.0001 | |||
| No | 3800 | 13.3 [12.2–14.4] | 14.1 [13.1–15.3] | ||
| Yes | 1002 | 13.9 [11.9–16.2] | 51.5 [48.4–54.6] | ||
| Self-reported dyslipidaemia | 0.088 | <0.0001 | |||
| No | 3591 | 13.1 [12.1–14.3] | 13.9 [12.8–15.0] | ||
| Yes | 1046 | 15.2 [13.2–17.5] | 47.8 [44.8–50.8] | ||
| Family history of diabetes | 0.62 | <0.0001 | |||
| No | 1795 | 13.3 [11.8–15.0] | 11.9 [10.5–13.4] | ||
| Yes | 2807 | 13.8 [12.6–15.1] | 24.5 [23.0–26.1] | ||
| Education level | 0.92 | <0.0001 | |||
| High school or lower | 2129 | 13.5 [12.1–15.0] | 24.0 [22.2–25.8] | ||
| University | 2807 | 13.4 [12.2–14.7] | 15.6 [14.3–17.0] | ||
| Monthly household income | 0.049 | 0.042 | |||
| ≤1000 KD (≤approx. $3300) | 2223 | 14.2 [12.8–15.7] | 18.3 [16.7–20.0] | ||
| >1000 KD (>approx. $3300) | 1778 | 12.1 [10.7–13.7] | 20.9 [19.0–22.8] | ||
| Kuwaitis | Non-Kuwaitis | ||||
|---|---|---|---|---|---|
| n | Prevalence, % [95% CI] | n | Prevalence, % [95% CI] | p | |
| All | 1684 | 21.8 [19.9–23.8] | 3253 | 18.2 [16.9–19.6] | 0.0025 |
| Sex | |||||
| Men | 863 | 21.9 [19.3–24.8] | 1910 | 22.5 [20.7–24.4] | 0.74 |
| Women | 821 | 21.7 [19.0–24.6] | 1343 | 11.0 [9.5–12.8] | <0.0001 |
| Age | |||||
| 20–29 | 78 | 6.3 [2.7–14.0] | 292 | 5.1 [3.1–8.3] | 0.66 |
| 30–44 | 679 | 12.7 [10.4–15.4] | 1603 | 14.6 [13.0–16.4] | 0.22 |
| 45–59 | 724 | 39.0 [35.5–42.6] | 1165 | 38.6 [35.9–41.5] | 0.89 |
| 60+ | 203 | 69.5 [62.8–75.4] | 193 | 59.3 [52.3–65.9] | 0.04 |
| Obesity category | |||||
| Normal BMI | 173 | 8.1 [4.9–13.1] | 652 | 8.4 [6.5–10.8] | 0.88 |
| Overweight | 600 | 17.2 [14.4–20.4] | 1288 | 17.8 [15.8–20.0] | 0.75 |
| Obese | 909 | 29.9 [27.0–33.0] | 1310 | 25.3 [23.0–27.7] | 0.015 |
| Waist–hip ratio | |||||
| Normal | 338 | 8.6 [6.0–12.0] | 893 | 6.7 [5.3–8.6] | 0.26 |
| Elevated | 1326 | 28.4 [26.0–30.8] | 2338 | 23.9 [22.2–25.7] | 0.003 |
| Self-reported hypertension | |||||
| No | 1299 | 13.9 [12.2–15.9] | 2501 | 14.2 [12.9–15.6] | 0.83 |
| Yes | 380 | 68.2 [63.4–72.7] | 622 | 45.4 [41.6–49.4] | <0.0001 |
| Self-reported dyslipidaemia | |||||
| No | 1263 | 12.7 [10.9–14.6] | 2328 | 14.3 [13.0–15.8] | 0.16 |
| Yes | 409 | 67.7 [63.0–72.1] | 637 | 40.3 [36.5–44.1] | <0.0001 |
| Family history of diabetes | |||||
| No | 331 | 14.2 [10.8–18.4] | 1464 | 11.5 [9.9–13.2] | 0.17 |
| Yes | 1178 | 23.2 [20.9–25.7] | 1629 | 25.2 [23.1–27.3] | 0.22 |
| Education level | |||||
| High school or lower | 518 | 35.5 [31.5–39.7] | 1611 | 21.7 [19.8–23.8] | <0.0001 |
| University | 1166 | 16.7 [14.7–19.0] | 1641 | 15.1 [13.4–16.9] | 0.23 |
| Monthly household income | |||||
| ≤1000 KD (≤approx. $3300) | 109 | 19.3 [13.0–27.7] | 2114 | 18.3 [16.7–20.0] | 0.79 |
| >1000 KD (>approx. $3300) | 1321 | 22.0 [19.9–24.3] | 457 | 18.6 [15.3–22.4] | 0.12 |
| Prediabetes | Diabetes | |||
|---|---|---|---|---|
| Characteristic | OR [95% CI] | p | OR [95% CI] | p |
| Sex | ||||
| Women | 1.00 | 1.00 | ||
| Men | 1.11 [0.91–1.36] | 0.29 | 1.78 [1.47–2.16] | <0.001 |
| Nationality | ||||
| Non-Kuwaiti | 1.00 | 1.00 | ||
| Kuwaiti | 0.84 [0.63–1.12] | 0.23 | 1.10 [0.84–1.44] | 0.48 |
| Age group | ||||
| 20–29 | 1.00 | 1.00 | ||
| 30–44 | 1.47 [0.93–2.33] | 0.10 | 1.08 [0.63–1.85] | 0.78 |
| 45–59 | 1.97 [1.23–3.15] | 0.005 | 2.91 [1.70–4.97] | <0.001 |
| 60+ | 2.03 [1.14–3.62] | 0.016 | 5.00 [2.75–9.10] | <0.001 |
| Obesity category | ||||
| Normal BMI | 1.00 | 1.00 | ||
| Overweight | 1.41 [1.03–1.92] | 0.031 | 1.23 [0.90–1.67] | 0.19 |
| Obese | 1.60 [1.17–2.19] | 0.003 | 1.82 [1.35–2.47] | <0.001 |
| Waist–hip ratio | ||||
| Normal | 1.00 | 1.00 | ||
| Elevated | 1.29 [1.00–1.65] | 0.044 | 2.45 [1.87–3.22] | <0.001 |
| Self-reported hypertension | ||||
| No | 1.00 | 1.00 | ||
| Yes | 0.79 [0.60–1.03] | 0.079 | 2.29 [1.85–2.83] | <0.001 |
| Self-reported dyslipidaemia | ||||
| No | 1.00 | 1.00 | ||
| Yes | 0.91 [0.71–1.17] | 0.48 | 2.58 [2.11–3.16] | <0.001 |
| Family history of diabetes | ||||
| No | 1.00 | 1.00 | ||
| Yes | 0.93 [0.76–1.14] | 0.47 | 2.25 [1.83–2.76] | <0.001 |
| Education level | ||||
| University | 1.00 | 1.00 | ||
| High school or lower | 0.79 [0.64–0.97] | 0.022 | 1.53 [1.27–1.85] | <0.001 |
| Monthly household income | ||||
| >1000 KD (>approx. $3300) | 1.00 | 1.00 | ||
| ≤1000 KD (≤approx. $3300) | 1.24 [0.93–1.63] | 0.14 | 1.30 [0.99–1.69] | 0.058 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Alkandari, A.; Alarouj, M.; Elkum, N.; Sharma, P.; Devarajan, S.; Abu-Farha, M.; Al-Mulla, F.; Tuomilehto, J.; Bennakhi, A. Adult Diabetes and Prediabetes Prevalence in Kuwait: Data from the Cross-Sectional Kuwait Diabetes Epidemiology Program. J. Clin. Med. 2020, 9, 3420. https://doi.org/10.3390/jcm9113420
Alkandari A, Alarouj M, Elkum N, Sharma P, Devarajan S, Abu-Farha M, Al-Mulla F, Tuomilehto J, Bennakhi A. Adult Diabetes and Prediabetes Prevalence in Kuwait: Data from the Cross-Sectional Kuwait Diabetes Epidemiology Program. Journal of Clinical Medicine. 2020; 9(11):3420. https://doi.org/10.3390/jcm9113420
Chicago/Turabian StyleAlkandari, Abdullah, Monira Alarouj, Naser Elkum, Prem Sharma, Sriraman Devarajan, Mohamed Abu-Farha, Fahd Al-Mulla, Jaakko Tuomilehto, and Abdullah Bennakhi. 2020. "Adult Diabetes and Prediabetes Prevalence in Kuwait: Data from the Cross-Sectional Kuwait Diabetes Epidemiology Program" Journal of Clinical Medicine 9, no. 11: 3420. https://doi.org/10.3390/jcm9113420
APA StyleAlkandari, A., Alarouj, M., Elkum, N., Sharma, P., Devarajan, S., Abu-Farha, M., Al-Mulla, F., Tuomilehto, J., & Bennakhi, A. (2020). Adult Diabetes and Prediabetes Prevalence in Kuwait: Data from the Cross-Sectional Kuwait Diabetes Epidemiology Program. Journal of Clinical Medicine, 9(11), 3420. https://doi.org/10.3390/jcm9113420








