Revision Arthroscopic Bankart Repair: A Systematic Review of Clinical Outcomes
Abstract
1. Introduction
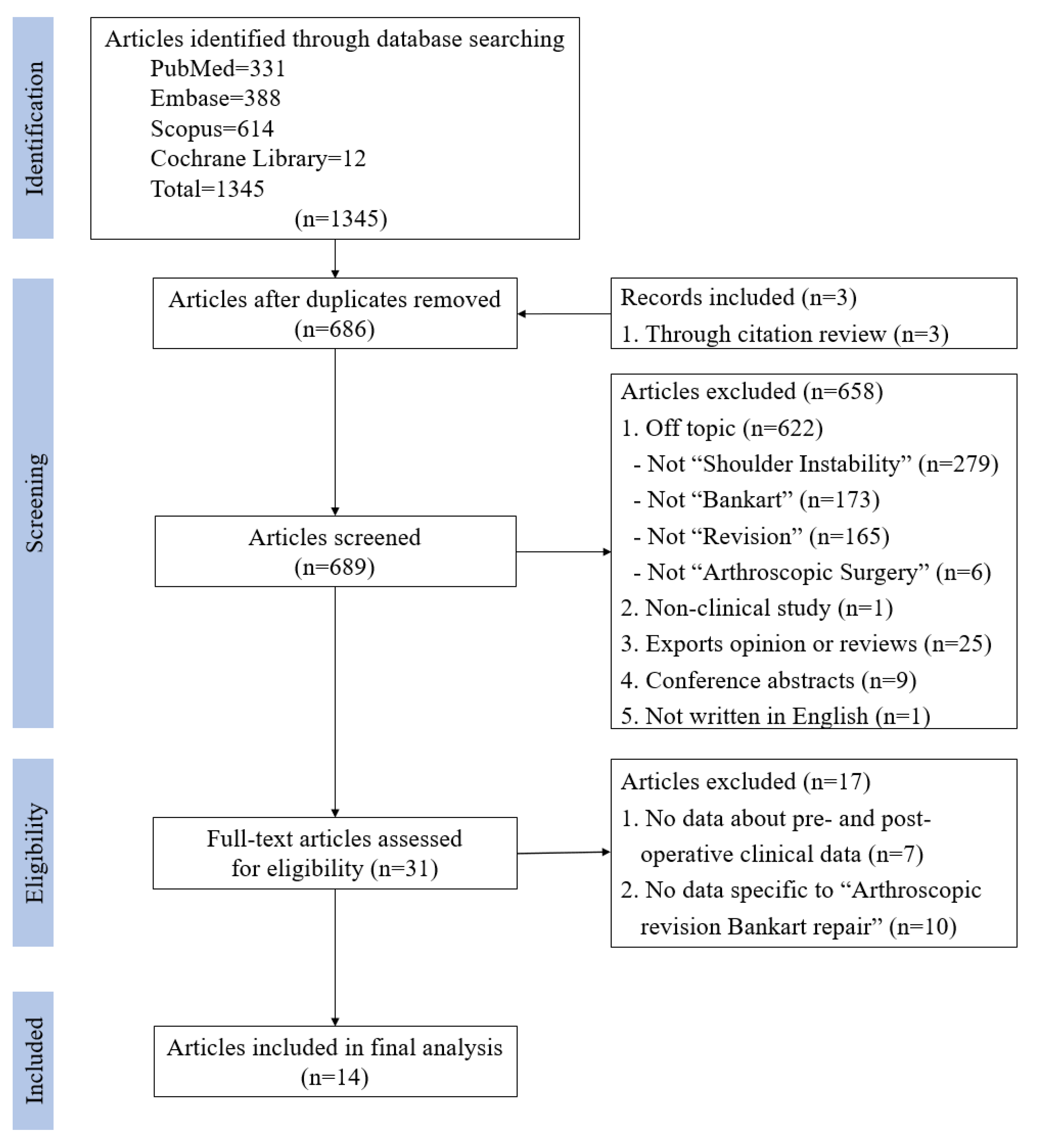
2. Materials and Methods
2.1. Search Strategy
2.2. Eligibility Criteria
2.3. Study Selection
2.4. Quality Assessment and Data Extraction
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Fabbriciani, C.; Milano, G.; Demontis, A.; Fadda, S.; Ziranu, F.; Mulas, P.D. Arthroscopic versus open treatment of Bankart lesion of the shoulder: A prospective randomized study. Arthroscopy 2004, 20, 456–462. [Google Scholar] [CrossRef] [PubMed]
- Hobby, J.; Griffin, D.; Dunbar, M.; Boileau, P. Is arthroscopic surgery for stabilisation of chronic shoulder instability as effective as open surgery? A systematic review and meta-analysis of 62 studies including 3044 arthroscopic operations. J. Bone Joint Surg. Br. 2007, 89, 1188–1196. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Ha, K.I.; Kim, S.H. Bankart repair in traumatic anterior shoulder instability: Open versus arthroscopic technique. Arthroscopy 2002, 18, 755–763. [Google Scholar] [CrossRef] [PubMed]
- Mazzocca, A.D.; Brown, F.M., Jr.; Carreira, D.S.; Hayden, J.; Romeo, A.A. Arthroscopic anterior shoulder stabilization of collision and contact athletes. Am. J. Sports Med. 2005, 33, 52–60. [Google Scholar] [CrossRef]
- On, M.G.; Oh, J.R.; Jang, Y.H.; Kim, D.S. Epidemiologic Study of Shoulder Injuries in the PyeongChang 2018 Winter Olympic Games. Clin. Orthop. Surg. 2019, 11, 187–191. [Google Scholar] [CrossRef]
- Oh, J.H.; Shin, S.J.; Cho, C.H.; Seo, H.J.; Park, J.S.; Rhee, Y.G. Reliability of the Instability Severity Index Score as a Predictor of Recurrence after Arthroscopic Anterior Capsulolabral Reconstruction: A Multicenter Retrospective Study. Clin. Orthop. Surg. 2019, 11, 445–452. [Google Scholar] [CrossRef]
- Ide, J.; Maeda, S.; Takagi, K. Arthroscopic Bankart repair using suture anchors in athletes: Patient selection and postoperative sports activity. Am. J. Sports Med. 2004, 32, 1899–1905. [Google Scholar] [CrossRef]
- Netto, N.A.; Tamaoki, M.J.; Lenza, M.; dos Santos, J.B.; Matsumoto, M.H.; Faloppa, F.; Belloti, J.C. Treatment of Bankart lesions in traumatic anterior instability of the shoulder: A randomized controlled trial comparing arthroscopy and open techniques. Arthroscopy 2012, 28, 900–908. [Google Scholar] [CrossRef]
- Petrera, M.; Patella, V.; Patella, S.; Theodoropoulos, J. A meta-analysis of open versus arthroscopic Bankart repair using suture anchors. Knee Surg. Sports Traumatol. Arthrosc. 2010, 18, 1742–1747. [Google Scholar] [CrossRef]
- Kim, S.H.; Jung, W.; Rhee, S.-M.; Kim, J.U.; Oh, J.H. Outcomes of arthroscopic capsulolabral reconstruction for anterior instability with greater than 20% glenoid bone defects: Are Latarjet procedures absolutely indicated for these patients? Clin. Shoulder Elbow 2020, 23, 62–70. [Google Scholar] [CrossRef]
- Kim, S.H.; Ha, K.I.; Cho, Y.B.; Ryu, B.D.; Oh, I. Arthroscopic anterior stabilization of the shoulder: Two to six-year follow-up. J. Bone Joint Surg. Am. 2003, 85, 1511–1518. [Google Scholar] [CrossRef] [PubMed]
- Boileau, P.; Villalba, M.; Héry, J.Y.; Balg, F.; Ahrens, P.; Neyton, L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J. Bone Joint Surg. Am. 2006, 88, 1755–1763. [Google Scholar] [CrossRef] [PubMed]
- Sugaya, H.; Moriishi, J.; Kanisawa, I.; Tsuchiya, A. Arthroscopic osseous Bankart repair for chronic recurrent traumatic anterior glenohumeral instability. J. Bone Joint Surg. Am. 2005, 87, 1752–1760. [Google Scholar] [CrossRef]
- Garofalo, R.; Mocci, A.; Moretti, B.; Callari, E.; Di Giacomo, G.; Theumann, N.; Cikes, A.; Mouhsine, E. Arthroscopic treatment of anterior shoulder instability using knotless suture anchors. Arthroscopy 2005, 21, 1283–1289. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Arce, G.; Arcuri, F.; Ferro, D.; Pereira, E. Is selective arthroscopic revision beneficial for treating recurrent anterior shoulder instability? Clin. Orthop. Relat. Res. 2012, 470, 965–971. [Google Scholar] [CrossRef]
- Balazs, L.G.C.; Donohue, M.M.A.; Brelin, C.A.M.; Wolfe, C.J.A.; Grimm, C.P.D.; Dworak, L.T.C.; Rue, C.J.H. Outcomes of Revision Arthroscopic Anterior Shoulder Stabilization in a Military Population: A Prospective Cohort Study. J. Surg. Orthop. Adv. 2019, 28, 189–195. [Google Scholar]
- Barnes, C.J.; Getelman, M.H.; Snyder, S.J. Results of arthroscopic revision anterior shoulder reconstruction. Am. J. Sports Med. 2009, 37, 715–719. [Google Scholar] [CrossRef]
- Bartl, C.; Schumann, K.; Paul, J.; Vogt, S.; Imhoff, A.B. Arthroscopic capsulolabral revision repair for recurrent anterior shoulder instability. Am. J. Sports Med. 2011, 39, 511–518. [Google Scholar] [CrossRef]
- Buckup, J.; Welsch, F.; Gramlich, Y.; Hoffmann, R.; Roessler, P.P.; Schüttler, K.F.; Stein, T. Back to Sports After Arthroscopic Revision Bankart Repair. Orthop. J. Sports Med. 2018, 6. [Google Scholar] [CrossRef]
- Creighton, R.A.; Romeo, A.A.; Brown, F.M., Jr.; Hayden, J.K.; Verma, N.N. Revision arthroscopic shoulder instability repair. Arthroscopy 2007, 23, 703–709. [Google Scholar] [CrossRef] [PubMed]
- Franceschi, F.; Longo, U.G.; Ruzzini, L.; Rizzello, G.; Maffulli, N.; Denaro, V. Arthroscopic salvage of failed arthroscopic Bankart repair: A prospective study with a minimum follow-up of 4 years. Am. J. Sports Med. 2008, 36, 1330–1336. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.H.; Ha, K.I.; Kim, Y.M. Arthroscopic revision Bankart repair: A prospective outcome study. Arthroscopy 2002, 18, 469–482. [Google Scholar] [CrossRef] [PubMed]
- Krueger, D.; Kraus, N.; Pauly, S.; Chen, J.; Scheibel, M. Subjective and objective outcome after revision arthroscopic stabilization for recurrent anterior instability versus initial shoulder stabilization. Am. J. Sports Med. 2011, 39, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Millar, N.L.; Murrell, G.A. The effectiveness of arthroscopic stabilisation for failed open shoulder instability surgery. J. Bone Joint Surg. Br. 2008, 90, 745–750. [Google Scholar] [CrossRef]
- Neri, B.R.; Tuckman, D.V.; Bravman, J.T.; Yim, D.; Sahajpal, D.T.; Rokito, A.S. Arthroscopic revision of Bankart repair. J. Shoulder Elbow Surg. 2007, 16, 419–424. [Google Scholar] [CrossRef]
- Patel, R.V.; Apostle, K.; Leith, J.M.; Regan, W.D. Revision arthroscopic capsulolabral reconstruction for recurrent instability of the shoulder. J. Bone Joint Surg. Br. 2008, 90, 1462–1467. [Google Scholar] [CrossRef]
- Ryu, R.K.; Ryu, J.H. Arthroscopic revision Bankart repair: A preliminary evaluation. Orthopedics 2011, 34, 17. [Google Scholar] [CrossRef]
- Shin, J.J.; Mascarenhas, R.; Patel, A.V.; Yanke, A.B.; Nicholson, G.P.; Cole, B.J.; Romeo, A.A.; Verma, N.N. Clinical outcomes following revision anterior shoulder arthroscopic capsulolabral stabilization. Arch. Orthop. Trauma Surg. 2015, 135, 1553–1559. [Google Scholar] [CrossRef]
- Abouali, J.A.; Hatzantoni, K.; Holtby, R.; Veillette, C.; Theodoropoulos, J. Revision arthroscopic Bankart repair. Arthroscopy 2013, 29, 1572–1578. [Google Scholar] [CrossRef]
- Adam, M.; Attia, A.K.; Alhammoud, A.; Aldahamsheh, O.; Al Dosari, M.A.A.; Ahmed, G. Arthroscopic Bankart repair for the acute anterior shoulder dislocation: Systematic review and meta-analysis. Int. Orthop. 2018, 42, 2413–2422. [Google Scholar] [CrossRef] [PubMed]
- Murphy, A.I.; Hurley, E.T.; Hurley, D.J.; Pauzenberger, L.; Mullett, H. Long-term outcomes of the arthroscopic Bankart repair: A systematic review of studies at 10-year follow-up. J. Shoulder Elbow Surg. 2019, 28, 2084–2089. [Google Scholar] [CrossRef] [PubMed]
- Burkhart, S.S.; De Beer, J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: Significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy 2000, 16, 677–694. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.S.; Karadsheh, M.S.; Sekiya, J.K. Failure of operative treatment for glenohumeral instability: Etiology and management. Arthroscopy 2011, 27, 681–694. [Google Scholar] [CrossRef]
- Yamamoto, N.; Itoi, E.; Abe, H.; Kikuchi, K.; Seki, N.; Minagawa, H.; Tuoheti, Y. Effect of an anterior glenoid defect on anterior shoulder stability: A cadaveric study. Am. J. Sports Med. 2009, 37, 949–954. [Google Scholar] [CrossRef]
- Shin, S.J.; Kim, R.G.; Jeon, Y.S.; Kwon, T.H. Critical Value of Anterior Glenoid Bone Loss That Leads to Recurrent Glenohumeral Instability After Arthroscopic Bankart Repair. Am. J. Sports Med. 2017, 45, 1975–1981. [Google Scholar] [CrossRef]
- Di Giacomo, G.; Itoi, E.; Burkhart, S.S. Evolving concept of bipolar bone loss and the Hill-Sachs lesion: From “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy 2014, 30, 90–98. [Google Scholar] [CrossRef] [PubMed]
- Yamamoto, N.; Itoi, E.; Abe, H.; Minagawa, H.; Seki, N.; Shimada, Y.; Okada, K. Contact between the glenoid and the humeral head in abduction, external rotation, and horizontal extension: A new concept of glenoid track. J. Shoulder Elbow Surg. 2007, 16, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Emami, M.J.; Solooki, S.; Meshksari, Z.; Vosoughi, A.R. The effect of open Bristow-Latarjet procedure for anterior shoulder instability: A 10-year study. Musculoskelet Surg. 2011, 95, 231–235. [Google Scholar] [CrossRef] [PubMed]
- Hovelius, L.; Sandström, B.; Olofsson, A.; Svensson, O.; Rahme, H. The effect of capsular repair, bone block healing, and position on the results of the Bristow-Latarjet procedure (study III): Long-term follow-up in 319 shoulders. J. Shoulder Elbow Surg. 2012, 21, 647–660. [Google Scholar] [CrossRef] [PubMed]
- Hurley, E.T.; Jamal, M.S.; Ali, Z.S.; Montgomery, C.; Pauzenberger, L.; Mullett, H. Long-term outcomes of the Latarjet procedure for anterior shoulder instability: A systematic review of studies at 10-year follow-up. J. Shoulder Elbow Surg. 2019, 28, e33–e39. [Google Scholar] [CrossRef]
- Allain, J.; Goutallier, D.; Glorion, C. Long-term results of the Latarjet procedure for the treatment of anterior instability of the shoulder. J. Bone Joint Surg. Am. 1998, 80, 841–852. [Google Scholar] [CrossRef] [PubMed]
- Gordins, V.; Hovelius, L.; Sandström, B.; Rahme, H.; Bergström, U. Risk of arthropathy after the Bristow-Latarjet repair: A radiologic and clinical thirty-three to thirty-five years of follow-up of thirty-one shoulders. J. Shoulder Elbow Surg. 2015, 24, 691–699. [Google Scholar] [CrossRef] [PubMed]
- Hovelius, L.; Vikerfors, O.; Olofsson, A.; Svensson, O.; Rahme, H. Bristow-Latarjet and Bankart: A comparative study of shoulder stabilization in 185 shoulders during a seventeen-year follow-up. J. Shoulder Elbow Surg. 2011, 20, 1095–1101. [Google Scholar] [CrossRef]
- Mizuno, N.; Denard, P.J.; Raiss, P.; Melis, B.; Walch, G. Long-term results of the Latarjet procedure for anterior instability of the shoulder. J. Shoulder Elbow Surg. 2014, 23, 1691–1699. [Google Scholar] [CrossRef]
- Bigliani, L.U.; Pollock, R.G.; Soslowsky, L.J.; Flatow, E.L.; Pawluk, R.J.; Mow, V.C. Tensile properties of the inferior glenohumeral ligament. J. Orthop. Res. 1992, 10, 187–197. [Google Scholar] [CrossRef] [PubMed]
- Randelli, P.; Ragone, V.; Carminati, S.; Cabitza, P. Risk factors for recurrence after Bankart repair a systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2012, 20, 2129–2138. [Google Scholar] [CrossRef]
- Lino, W., Jr.; Belangero, W.D. Labrum repair combined with arthroscopic reduction of capsular volume in shoulder instability. Int. Orthop. 2006, 30, 219–223. [Google Scholar] [CrossRef]
- Westerheide, K.J.; Dopirak, R.M.; Snyder, S.J. Arthroscopic anterior stabilization and posterior capsular plication for anterior glenohumeral instability: A report of 71 cases. Arthroscopy 2006, 22, 539–547. [Google Scholar] [CrossRef]
- Chiang, E.R.; Wang, J.P.; Wang, S.T.; Ma, H.L.; Liu, C.L.; Chen, T.H. Arthroscopic posteroinferior capsular plication and rotator interval closure after Bankart repair in patients with traumatic anterior glenohumeral instability—A minimum follow-up of 5 years. Injury 2010, 41, 1075–1078. [Google Scholar] [CrossRef]
- Park, J.Y.; Chung, S.W.; Kumar, G.; Oh, K.S.; Choi, J.H.; Lee, D.; Park, S. Factors affecting capsular volume changes and association with outcomes after Bankart repair and capsular shift. Am. J. Sports Med. 2015, 43, 428–438. [Google Scholar] [CrossRef] [PubMed]
- Coughlin, R.P.; Bullock, G.S.; Shanmugaraj, A.; Sell, T.C.; Garrigues, G.E.; Ledbetter, L.; Taylor, D.C. Outcomes After Arthroscopic Rotator Interval Closure for Shoulder Instability: A Systematic Review. Arthroscopy 2018, 34, 3098–3108. [Google Scholar] [CrossRef] [PubMed]
- Karovalia, S.; Collett, D.J.; Bokor, D. Rotator interval closure: Inconsistent techniques and its association with anterior instability. A literature review. Orthop. Rev. 2019, 11, 8136. [Google Scholar] [CrossRef] [PubMed]
| Authors | Year | Number of Shoulders | Type of Study | Design | Level of Evidence | MINORS Score |
|---|---|---|---|---|---|---|
| Arce et al. [16] | 2012 | 16 | Case series | Retrospective | IV | 11/16 |
| Balazs et al. [17] | 2019 | 16 | Cohort study | Prospective | II | 14/16 |
| Barnes et al. [18] | 2009 | 17 | Case series | Retrospective | IV | 10/16 |
| Bartl et al. [19] | 2011 | 56 | Case series | Retrospective | IV | 11/16 |
| Buckup et al. [20] | 2018 | 23 | Case series | Retrospective | IV | 11/16 |
| Creighton et al. [21] | 2007 | 18 | Case series | Retrospective | IV | 11/16 |
| Franceschi et al. [22] | 2008 | 10 | Case series | Retrospective | IV | 12/16 |
| Kim et al. [23] | 2002 | 23 | Prospective nonrandomized outcome study | Prospective | IV | 12/16 |
| Krueger et al. [24] | 2011 | 20 | Cohort study | Retrospective Comparative | III | 21/24 |
| Millar et al. [25] | 2008 | 10 | Case series | Retrospective Comparative | III | 18/24 |
| Neri et al. [26] | 2007 | 12 | Case series | Retrospective | IV | 10/16 |
| Patel et al. [27] | 2008 | 40 | Case series | Retrospective | IV | 12/16 |
| Ryu et al. [28] | 2011 | 15 | Case series | Retrospective | IV | 11/16 |
| Shin et al. [29] | 2015 | 63 | Case series | Retrospective | IV | 10/16 |
| Data | |
|---|---|
| No. of patients in the study | 337 |
| No. of shoulders in the study | 339 |
| Mean age (years) | 27.41 |
| Gender | |
| Male | 281 (83.4%) |
| Female | 56 (16.6%) |
| Mean duration of follow-up (months) | 36.7 |
| Dominant extremity | 201 (59.3%) |
| Authors | Primary Surgery | Interval from Initial Surgery to Recurrence or Revision Surgery (Months) | Exclusion Criteria of Revision Surgery | |||
|---|---|---|---|---|---|---|
| Initial Surgery to Recurrence | Between Procedure | Glenoid Loss | Humeral Loss | Hyperlaxity | ||
| Arce et al. [16] | Arthroscopic procedure: 10 Transglenoid: 4 Suture anchors: 6 Open procedure: 6 Staples + Open: 2 Transglenoid + Open: 2 Open: 2 | NA | NA | > 25% excluded | > 33% excluded | Multidirectional instability excluded |
| Balazs et al. [17] | NA | NA | 26.5 (10–62) | NA | NA | NA |
| Barnes et al. [18] | Arthroscopic procedure: 9 Arthroscopic thermal: 2 Arthroscopic suture plication: 1 Arthroscopic suture anchors: 5 2x Arthroscopic (unknown): 1 Open procedure: 8 Open Bankart: 5 Open Magnuson-Stack: 2 Open Magnuson-Stack & Bristow: 1 | 21.5 (4–83) | NA | No exclusion | No exclusion | NA |
| Bartl et al. [19] | Arthroscopic procedure: 34 Arthroscopic Bankart repair (anchors): 20 Arthroscopic Bankart repair (transglenoidal): 4 Arthroscopic Bankart repair (tacks): 8 Capsular plication/Capsular shrinkage: 2 Open procedure: 22 Open Bankart repair (anchors): 13 Open Bankart repair (transosseous): 6 Open capsular shift: 3 | NA | 43 (5–110) | > 20% excluded | Engaging Hill-Sachs excluded | Multidirectional instability excluded |
| Buckup et al. [20] | Arthroscopic Bankart repair: 23 | 28.7 ± 8.45 | 39.55 ± 31.62 | > 20% excluded | > Calandra grade II excluded | More than 1° sulcus sign excluded |
| Creighton et al. [21] | Arthroscopic Bankart repair: 18 with thermal shrinkage: 9 without thermal shrirnage: 9 | 10 (4-20) | NA | > 25% excluded | Engaging Hill-Sachs excluded | Multidirectional or posterior instability Excluded |
| Franceschi et al. [22] | Arthroscopic Bankart repair: 10 Suture anchor: 9 Transglenoid: 1 | 18 (5-73) | 25 (12-49) | > 30% excluded | Engaging Hill-Sachs excluded | Multidirectional instability excluded |
| Kim et al. [23] | Arthroscopic Bankart repair: 15 Transglenoid suture: 10 Suture anchor: 5 Open Bankart repair: 8 Transosseous suture: 5 Suture anchor: 3 | 21 (11-31) | NA | > 30% excluded | NA | Multidirectional or posterior instability or 3° sulcus sign excluded |
| Krueger et al. [24] | Arthroscopic Bankart repair: 15 Open Bankart repair: 5 | NA | NA | > 25% excluded | NA | No Exclusion |
| Millar et al. [25] | Open procedure: 10 Putti-Platt procedure: 5 Open Bankart repair: 3 Open capsular shift: 2 | 97 (28–240) | 121 (18–264) | NA | NA | Multidirectional or posterior instability excluded |
| Neri et al. [26] | Arthroscopic Bankart repair: 6 Suture anchor: 5 Transglenoid: 1 Open Bankart repair: 6 Suture anchor: 5 Staple: 1 | 28 (6–84) | 52.5 (9–204) | > 30% excluded | Engaging Hill-Sachs excluded | Multidirectional instability excluded |
| Patel et al. [27] | Arthroscopic procedure: 21 Arthroscopic Bankart repair: 19 Arthroscopic Bankart repair with posterior labrum repair: 1 Capsular shrinkage: 1 Open procedure: 18 Open Bankart repair: 16 Magnusson-Stack procedure: 2 Unknown: 1 | NA | 72 (5–308) | Inverted-pear Bankart lesion excluded | Engaging Hill-Sachs excluded | NA |
| Ryu et al. [28] | Arthroscopic procedure: 11 Arthroscopic Bankart repair: 11 Open procedure: 4 Open Bankart repair: 3 Capsular shift: 1 | NA | NA | NA | NA | NA |
| Shin et al. [29] | NA | NA | NA | > 25% excluded | NA | NA |
| Total | Arthroscopic procedures: 172/339 (50.7%) Open procedures: 87/339 (25.7%) Unknown: 80/339 (23.6%) | 28.09 | 52.17 | - | - | - |
| Authors | Concomitant Procedure | Recurrence of Instability | Other Complications | Mechanism of Failure | Re-RevisionRate |
|---|---|---|---|---|---|
| Arce et al. [16] | Rotator interval closure: 16/16 Posteroinferior capsular plication: 14/16 | 3/16 (18.8%) | - | 1 T D and 2 NA | 1/3 |
| Balazs et al. [17] | SLAP repair: 1/16 SLAP debridement: 9/16 PASTA debridement: 2/16 | 0/16 (0.0%) | - | 0 | 0/0 |
| Barnes et al. [18] | Rotator interval closure: 1/17 Posterior capsular plication: 13/17 SLAP repair: 3/17 | 4/17 (23.5%) | - | 1 T D and 3 P | 1/4 |
| Bartl et al. [19] | Rotator interval closure: 16/56 | 6/56 (10.7%) | Shoulder stiffness: 2/56 Loosed titanium anchor: 1/56 | 4 T D 2 A S | 4/6 |
| Buckup et al. [20] | NA | 3/23 (13.0%) | - | 3 T D | 3/3 |
| Creighton et al. [21] | Rotator interval closure: 15/18 | 3/18 (16.7%) | - | 1 T D and 2 T S | 1/3 |
| Franceschi et al. [22] | Rotator interval closure: 7/10 | 1/10 (10.0%) | - | 1 P | 0/1 |
| Kim et al. [23] | Rotator interval closure: 15/23 | 5/23 (21.7%) | Transient neurapraxia: 1/23 | 1 T D,2 T S, and 2 P | NA |
| Krueger et al. [24] | Posterior capsular plication: 1/20 | 2/20 (10.0%) | Mild osteoarthritis grade I: 5/20 | 2 P | 0/2 |
| Millar et al. [25] | NA | 2/10 (20.0%) | - | 2 T D | 0/2 |
| Neri et al. [26] | Rotator interval closure: 4/12 | 3/12 (25.0%) | - | 1 T D 1 A D 1 T S | NA |
| Patel et al. [27] | NA | 4/40 (10.0%) | - | 4 T D | 2/4 |
| Ryu et al. [28] | Rotator interval closure: 6/15 | 4/15 (26.7%) | - | 2 T D and 2 A D | 2/4 |
| Shin et al. [29] | Rotator interval closure: 7/63 | 12/63 (19.0%) | - | 7 T D,3 A D, and 2 A S | 8/12 |
| Total | Rotator interval closure: 102 Capsular plication: 28 SLAP repair: 4 SLAP debridement: 9 PASTA debridement: 2 | 52/339 (15.3%) | 9/339 (2.7%) Stiffness: 2 Transient neurapraxia: 1 Metal failure: 1 Arthritic change: 5 | T D: 27/52 (51.9%) T S: 5/52 (9.6%) A D: 6/52 (55.5%) A S: 4/52 (7.7%) P: 8/52 (15.4%) Unknown: 2/52 (3.9%) | 22/339 (6.5%) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yon, C.-J.; Cho, C.-H.; Kim, D.-H. Revision Arthroscopic Bankart Repair: A Systematic Review of Clinical Outcomes. J. Clin. Med. 2020, 9, 3418. https://doi.org/10.3390/jcm9113418
Yon C-J, Cho C-H, Kim D-H. Revision Arthroscopic Bankart Repair: A Systematic Review of Clinical Outcomes. Journal of Clinical Medicine. 2020; 9(11):3418. https://doi.org/10.3390/jcm9113418
Chicago/Turabian StyleYon, Chang-Jin, Chul-Hyun Cho, and Du-Han Kim. 2020. "Revision Arthroscopic Bankart Repair: A Systematic Review of Clinical Outcomes" Journal of Clinical Medicine 9, no. 11: 3418. https://doi.org/10.3390/jcm9113418
APA StyleYon, C.-J., Cho, C.-H., & Kim, D.-H. (2020). Revision Arthroscopic Bankart Repair: A Systematic Review of Clinical Outcomes. Journal of Clinical Medicine, 9(11), 3418. https://doi.org/10.3390/jcm9113418







