Effectiveness of Dry Needling for Myofascial Trigger Points Associated with Neck Pain Symptoms: An Updated Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Experimental Section
2.1. Systematic Literature Search
2.2. Selection Criteria
2.3. Screening, Selection Process, and Data Extraction
2.4. Assessment of Methodological Quality and Risk of Bias
2.5. Level of Evidence
2.6. Data Synthesis and Analysis
3. Results
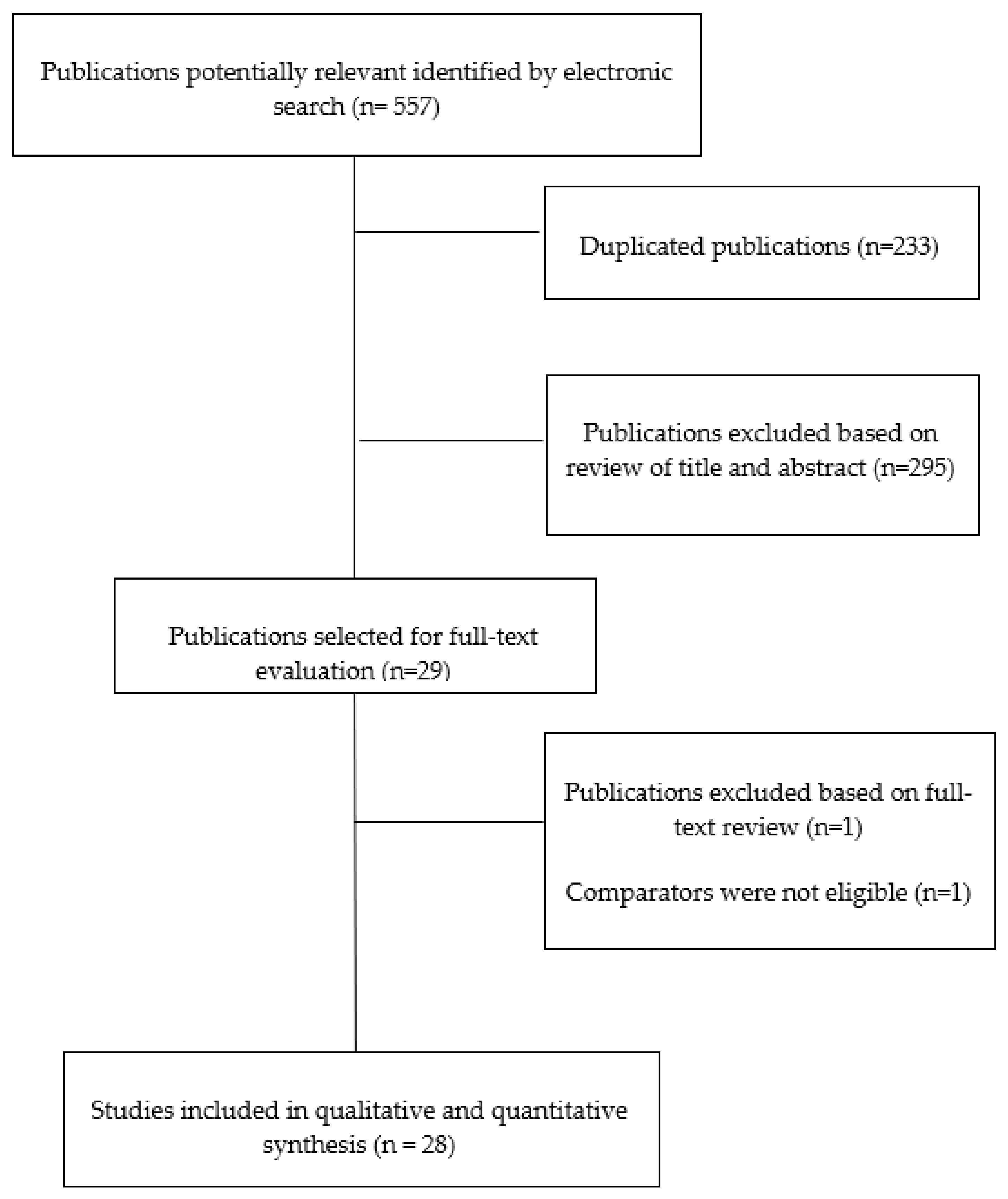
3.1. Study Selection
3.2. Study Characteristics
3.3. Methodological Quality
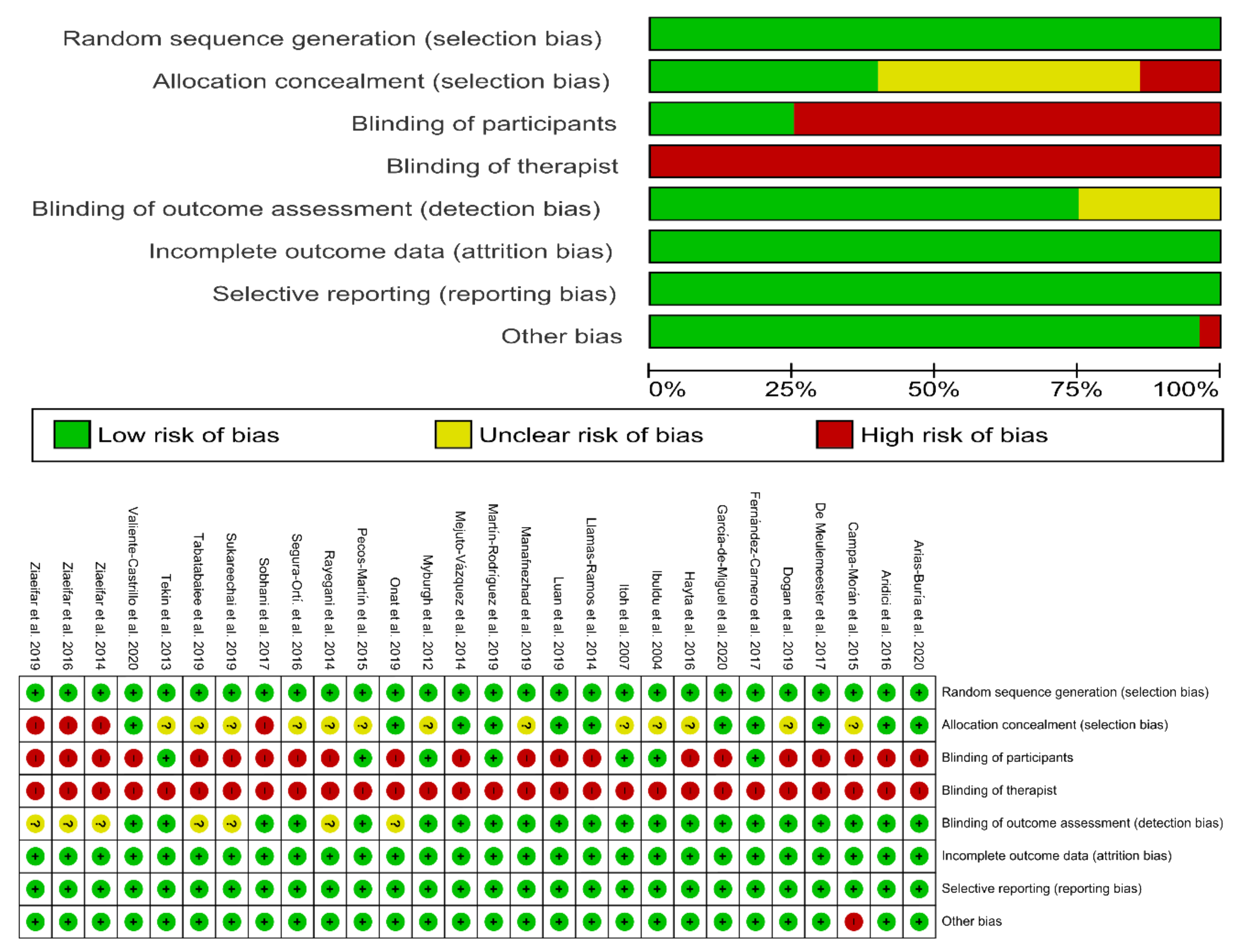
3.4. Risk of Bias
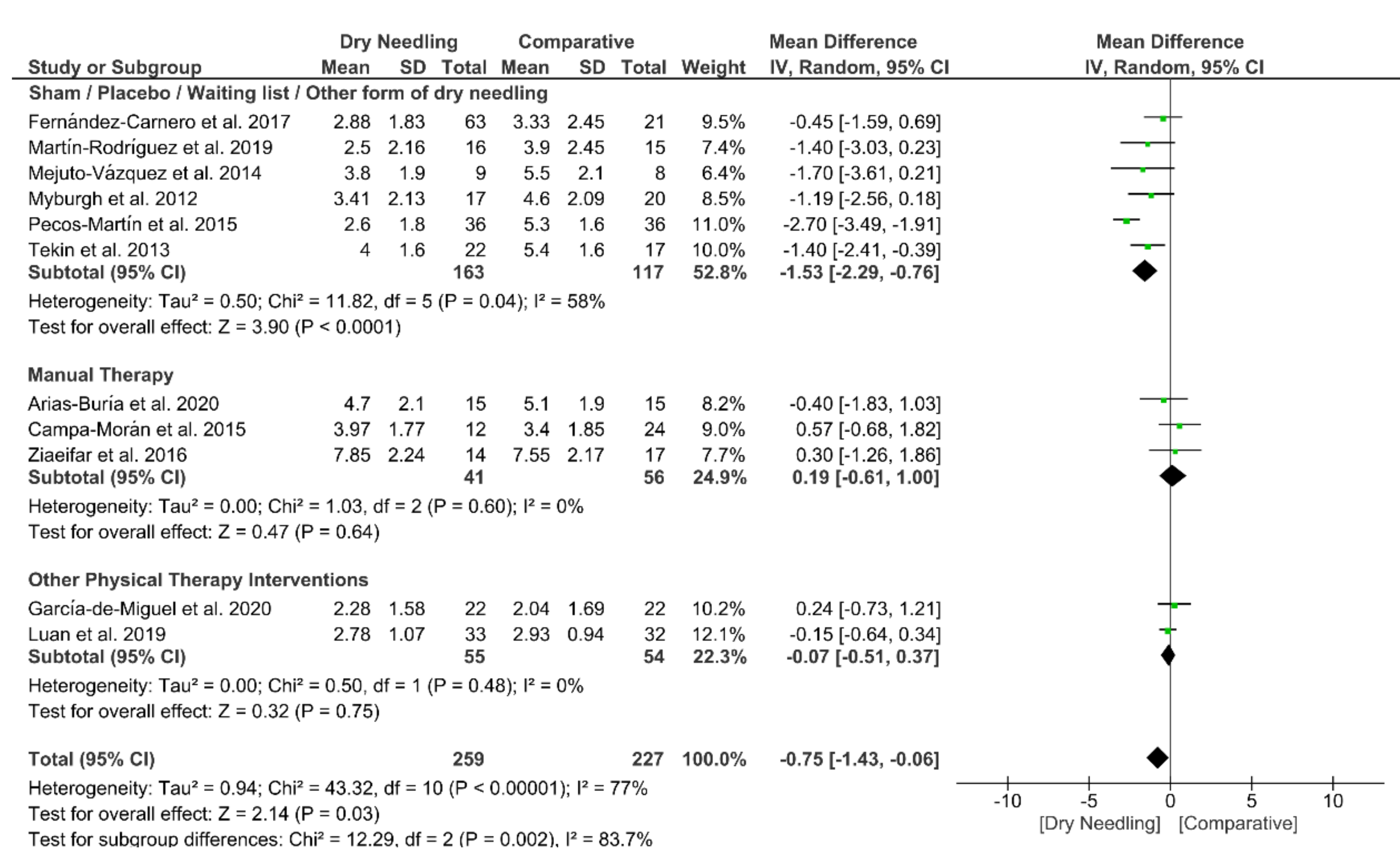
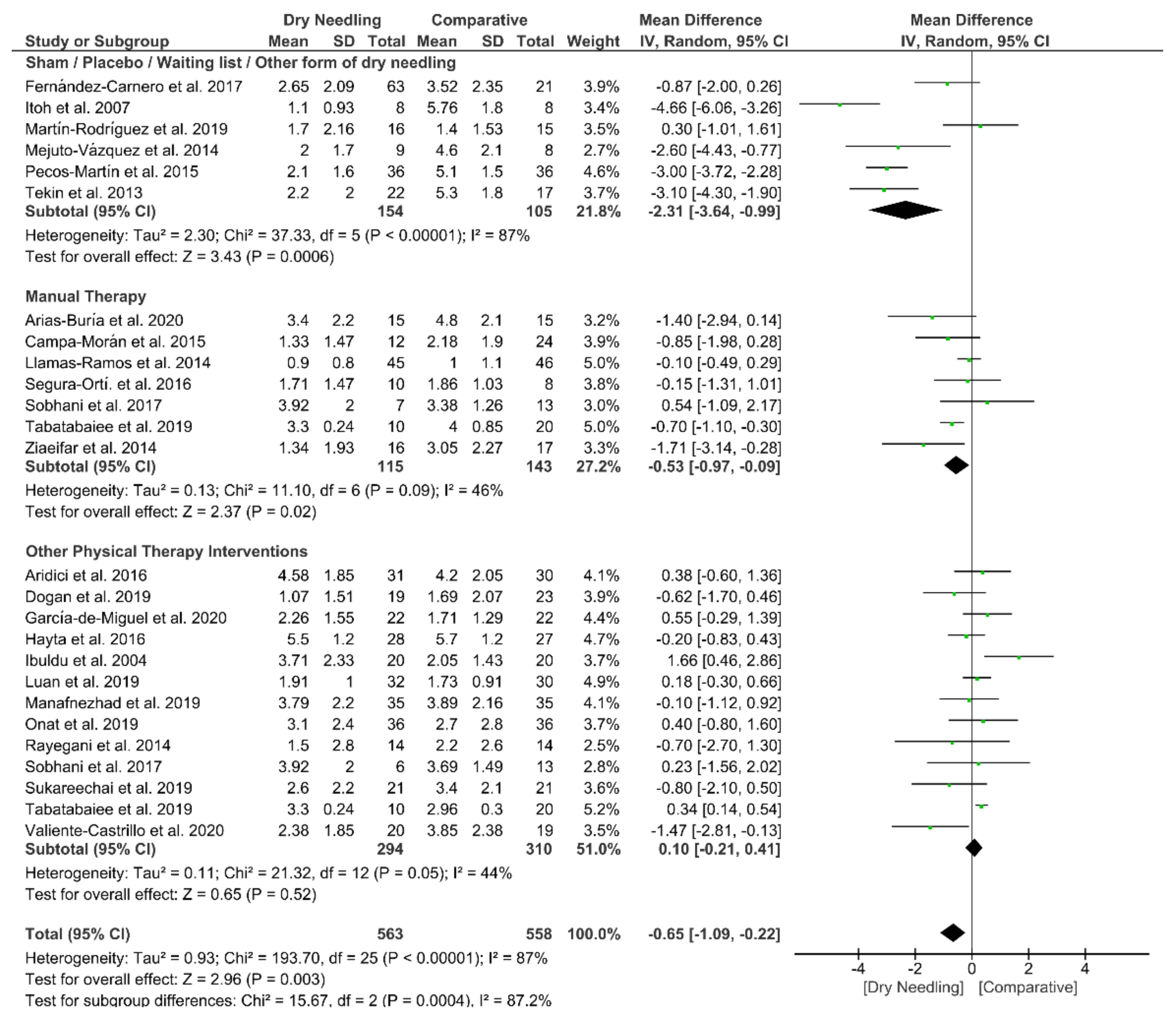
3.5. Dry Needling and Neck Pain Intensity
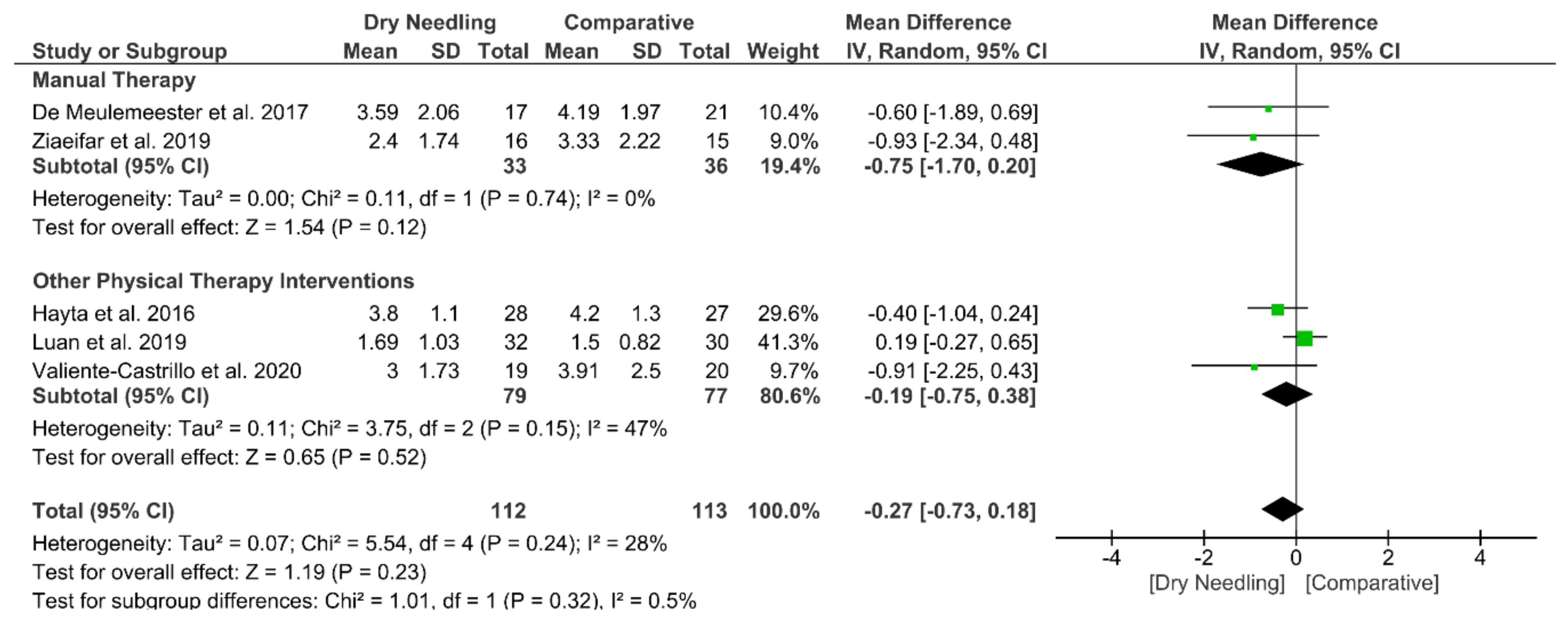
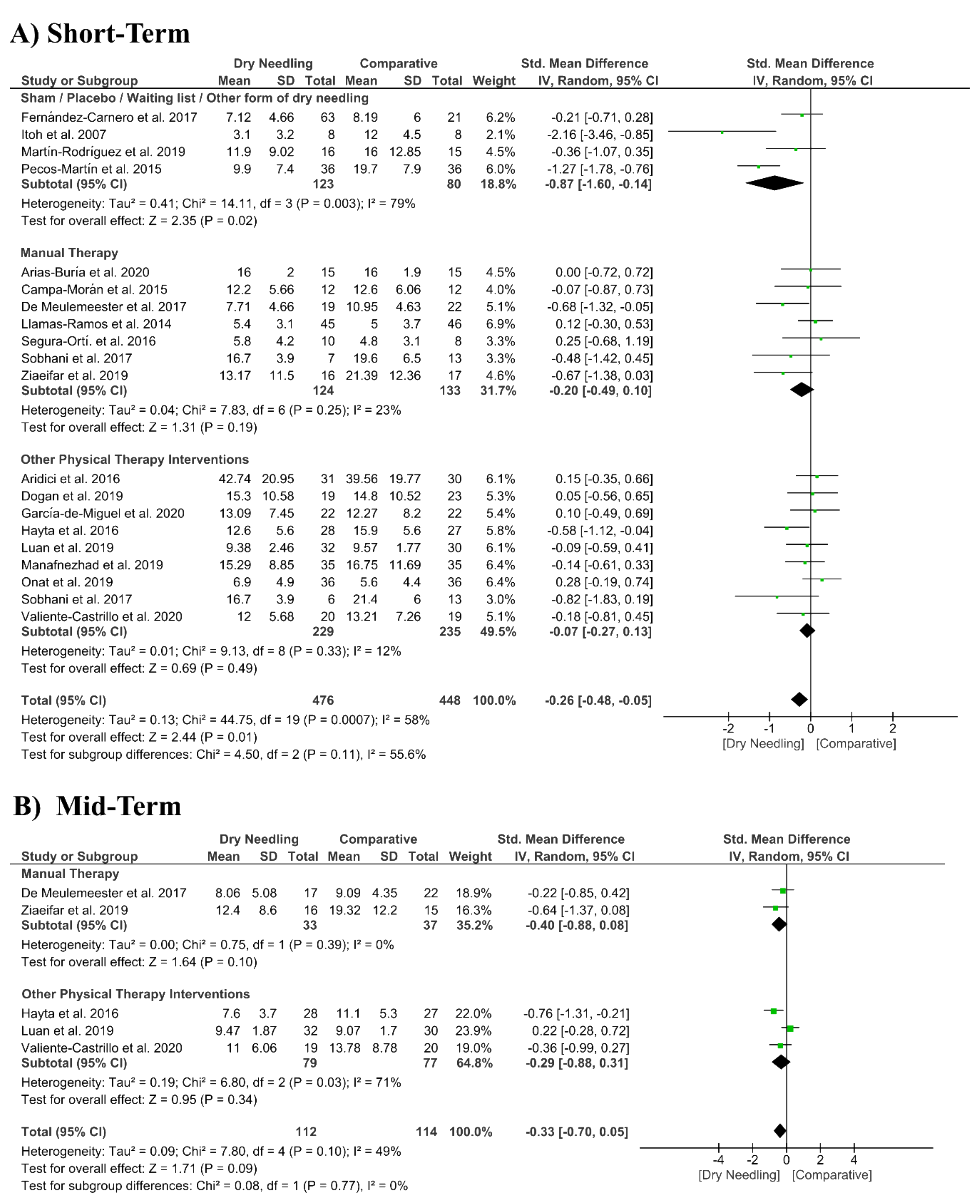
3.6. Dry Needling and Pain-Related Disability
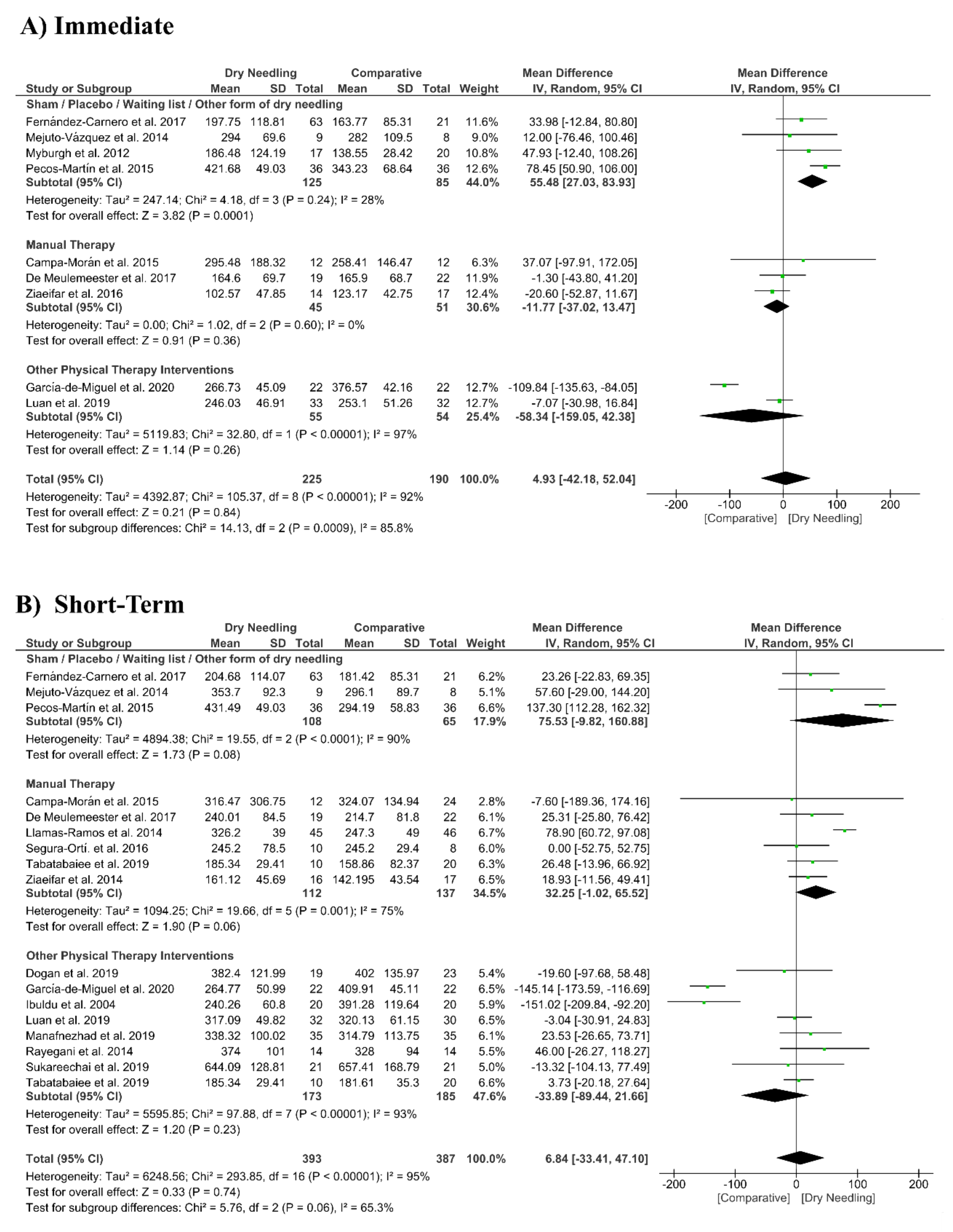
3.7. Dry Needling and Pressure Pain Sensitivity (Pressure Pain Thresholds)
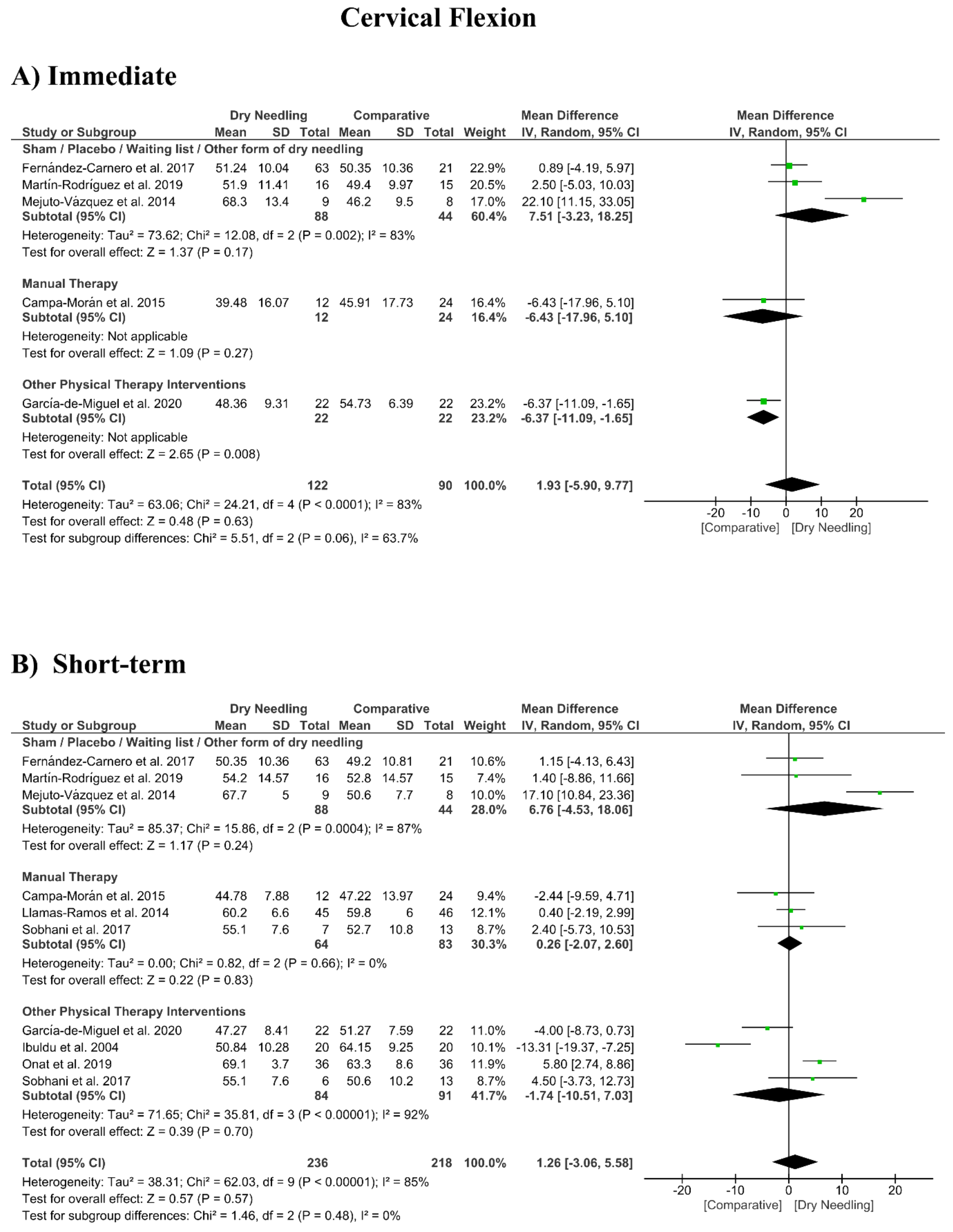
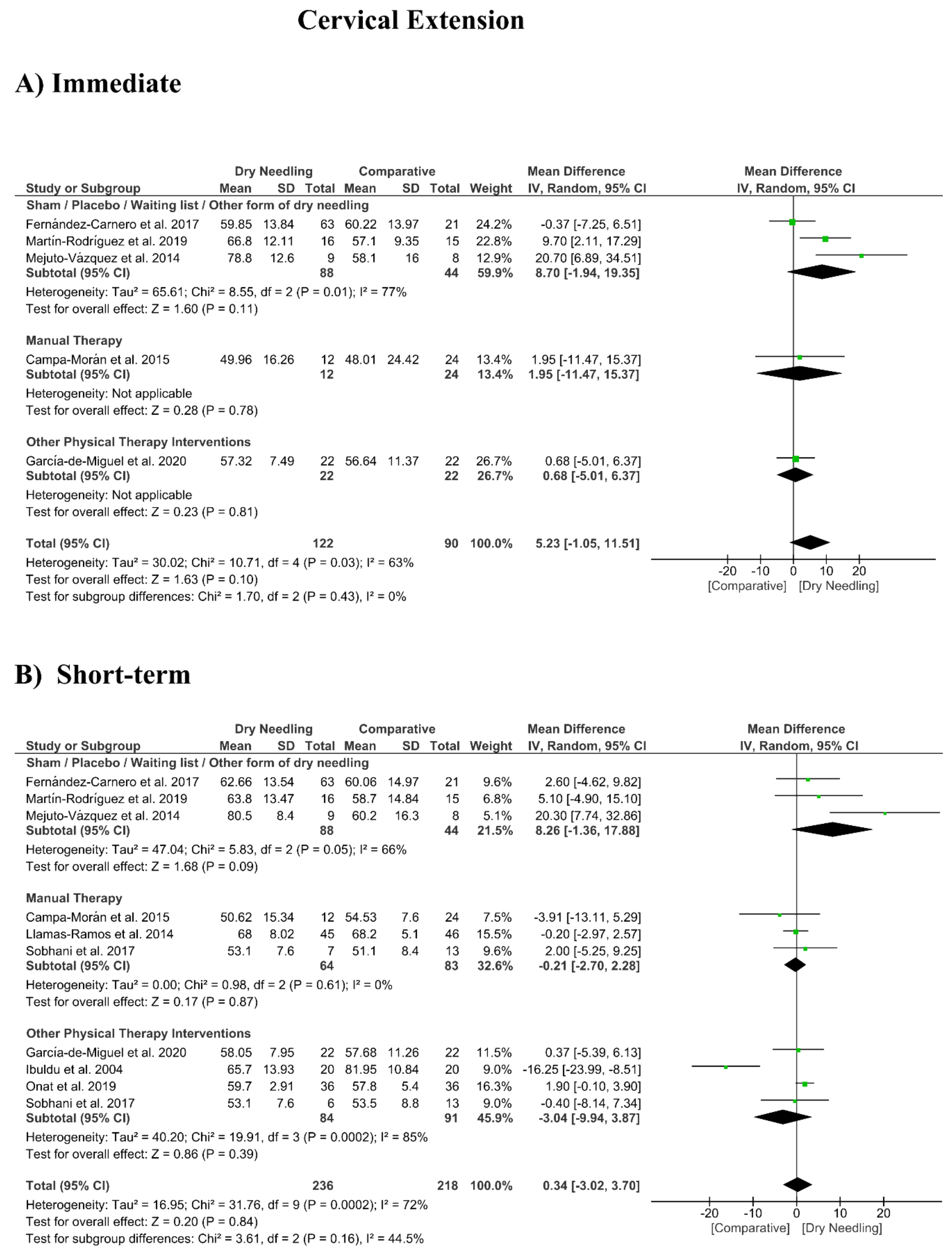
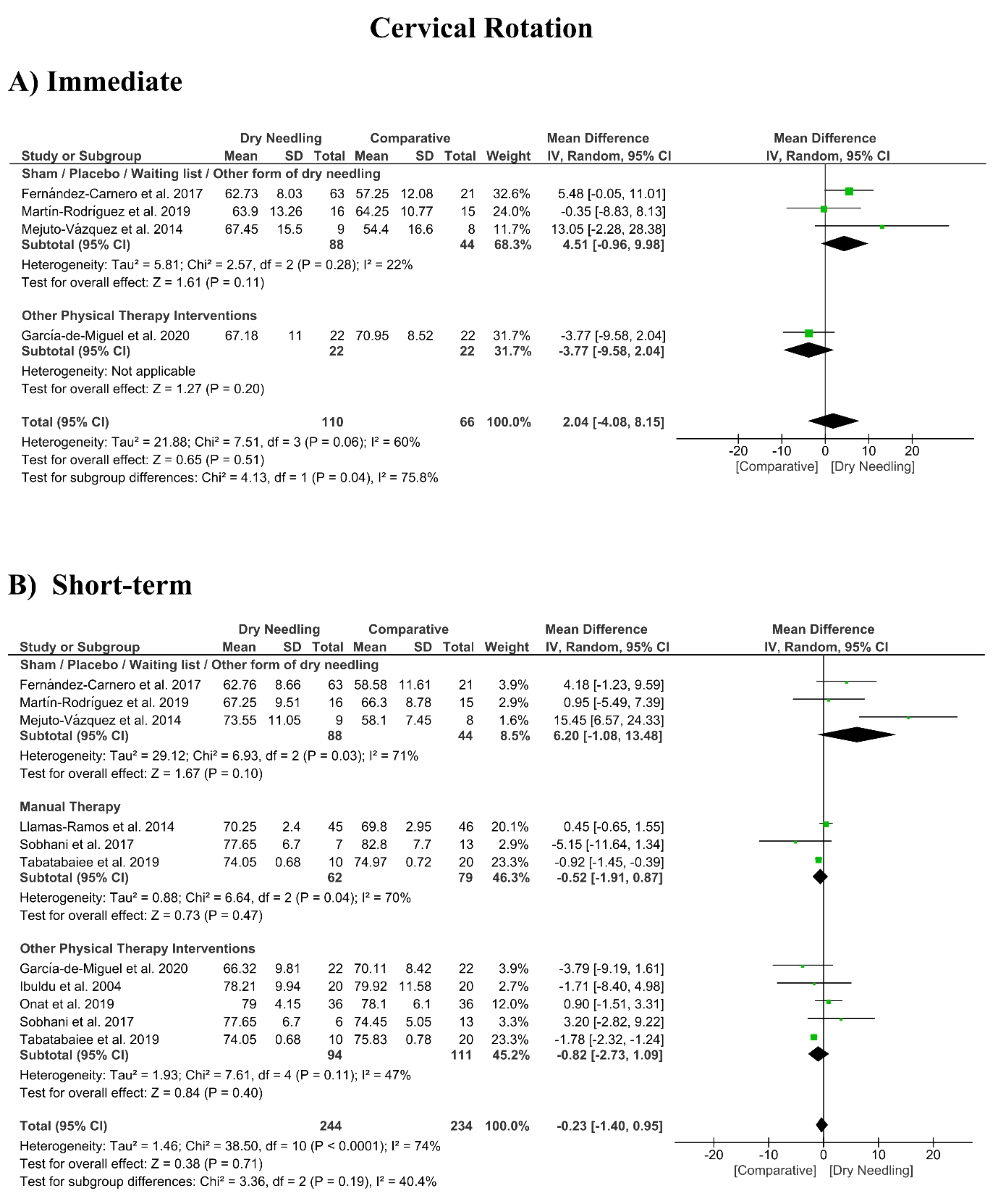
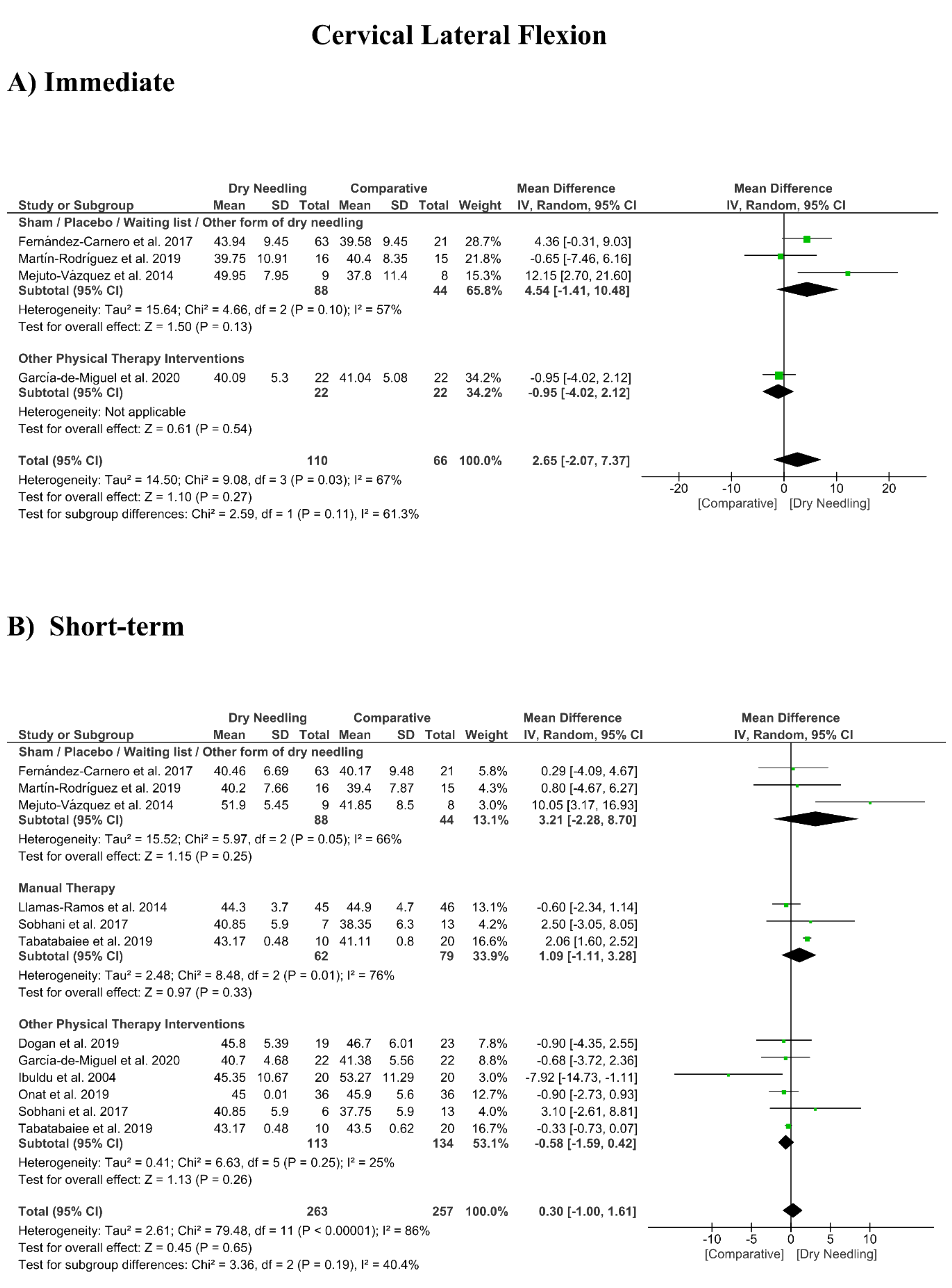
3.8. Dry Needling and Cervical Range of Motion
3.9. Adverse Events
3.10. Quality of Evidence (GRADE)
4. Discussion
4.1. Trigger Point Dry Needling and Neck Pain
4.2. Adverse Events Associated to Trigger Point Dry Needling
4.3. Strengths and Limitations
4.4. Clinical and Research Implications
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Hoy, D.; March, L.; Woolf, A.; Blyth, F.; Brooks, P.; Smith, E. The global burden of neck pain: Estimates from the global burden of disease 2010 study. Ann. Rheum. Dis. 2014, 73, 1309–1315. [Google Scholar] [CrossRef]
- Vos, T.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abdulkader, R.S.; Abdulle, A.M.; Abebo, T.A.; Abera, S.F. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef]
- Gross, A.; Langevin, P.; Burnie, S.J.; Bédard-Brochu, M.; Empey, B.; Dugas, E.; Faber-Dobrescu, M.; Andres, C.; Graham, N.; Goldsmith, C.H. Manipulation and mobilisation for neck pain contrasted against an inactive control or another active treatment. Cochrane Database Syst. Rev. 2015, 9, CD004249. [Google Scholar] [CrossRef]
- Gross, A.; Kay, T.M.; Paquin, J.; Blanchette, S.; Lalonde, P.; Christie, T.; Dupont, G.; Graham, N.; Burnie, S.J.; Gelley, G. Exercises for mechanical neck disorders. Cochrane Database Syst. Rev. 2015, 1, CD004250. [Google Scholar] [CrossRef]
- Gross, A.; Forget, M.; St George, K.; Fraser, M.M.H.; Graham, N.; Perry, L.; Burnie, S.J.; Goldsmith, C.H.; Haines, T.; Brunarski, D. Patient education for neck pain. Cochrane Database Syst. Rev. 2012, 3, CD005106. [Google Scholar] [CrossRef]
- Bier, J.D.; Scholten-Peeters, W.G.M.; Staal, J.B.; Pool, J.; van Tulder, M.W.; Beekman, E.; Knoop, J.; Meerhoff, G.; Verhagen, A.P. Clinical practice guideline for physical therapy assessment and treatment in patients with nonspecific neck pain. Phys. Ther. 2018, 98, 162–171. [Google Scholar] [CrossRef] [PubMed]
- Blanpied, P.R.; Gross, A.R.; Elliott, J.M.; Devaney, L.L.; Clewley, D.; Walton, D.M.; Sparks, C.; Robertson, E.K.; Altman, R.D.; Beattie, P. Neck pain: Revision 2017: Clinical practice guidelines linked to the international classification of functioning, disability and health from the orthopaedic section of the American Physical Therapy Association. J. Orthop. Sport. Phys. Ther. 2017, 47, A1–A83. [Google Scholar] [CrossRef]
- Simons, D.G.; Travell, J.G. Myofascial Pain and Dysfunction: The Trigger Point Manual, 3rd ed.; Wolters Kluwer: Philadelphia, PA, USA, 2019. [Google Scholar]
- Chiarotto, A.; Clijsen, R.; Fernandez-De-Las-Penas, C.; Barbero, M. Prevalence of myofascial trigger points in spinal disorders: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2016, 97, 316–337. [Google Scholar] [CrossRef]
- Dommerholt, J.; Fernandez-de-las Peñas, C. Trigger Point Dry Needling: An Evidence and Clinical-Based Approach, 2nd ed.; Elsevier: London, UK, 2019. [Google Scholar]
- American Physical Therapy Association (APTA). Description of Dry Needling in Clinical Practice: An EducAtional Resource Paper; APTA: Alexandria, VA, USA, 2013. [Google Scholar]
- Cagnie, B.; Castelein, B.; Pollie, F.; Steelant, L.; Verhoeyen, H.; Cools, A. Evidence for the use of ischemic compression and dry needling in the management of trigger points of the upper trapezius in patients with neck pain: A systematic review. Am. J. Phys. Med. Rehabil. 2015, 94, 573–583. [Google Scholar] [CrossRef]
- Liu, L.; Huang, Q.-M.; Liu, Q.-G.; Ye, G.; Bo, C.-Z.; Chen, M.-J.; Li, P. Effectiveness of dry needling for myofascial trigger points associated with neck and shoulder pain: A systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 2015, 96, 944–955. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, T.P. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro Scale for Rating Quality of Randomized. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef]
- Schünemann, H.J.; Oxman, A.D.; Brozek, J.; Glasziou, P.; Bossuyt, P.; Chang, S.; Muti, P.; Jaeschke, R.; Guyatt, G.H. GRADE: Assessing the quality of evidence for diagnostic recommendations. BMJ Evid.-Based Med. 2008, 13, 162–163. [Google Scholar] [CrossRef]
- Austin, T.M.; Richter, R.R.; Sebelski, C.A. Introduction to the GRADE approach for guideline development: Considerations for physical therapist practice. Phys. Ther. 2014, 94, 1652–1659. [Google Scholar] [CrossRef]
- Wan, X.; Wang, W.; Liu, J.; Tong, T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med. Res. Methodol. 2014, 14, 1–13. [Google Scholar] [CrossRef]
- Luo, D.; Wan, X.; Liu, J.; Tong, T. Optimally estimating the sample mean from the sample size, median, mid-range, and/or mid-quartile range. Stat. Methods Med. Res. 2018, 27, 1785–1805. [Google Scholar] [CrossRef]
- Sullivan, G.M.; Feinn, R. Using Effect Size—Or Why the P Value Is Not Enough. J. Grad. Med. Educ. 2012, 4, 279–282. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Churchill, R.; Chandler, J.; Cumpston, M.S. (Eds.) Analyzing data and undertaking metanalyses. In Cochrane Handbook for Systematic Reviews of Interventions Version 5.2.0 (Updated June 2017); Cochrane: London, UK, 2017; Available online: www.training.cochrane.org/handbook (accessed on 1 August 2020).
- Ziaeifar, M.; Arab, A.M.; Nourbakhsh, M.R. Clinical effectiveness of dry needling immediately after application on myofascial trigger point in upper trapezius muscle. J. Chiropr. Med. 2016, 15, 252–258. [Google Scholar] [CrossRef]
- Ziaeifar, M.; Arab, A.M.; Mosallanezhad, Z.; Nourbakhsh, M.R. Dry needling versus trigger point compression of the upper trapezius: A randomized clinical trial with two-week and three-month follow-up. J. Man. Manip. Ther. 2019, 27, 152–161. [Google Scholar] [CrossRef]
- Pecos-Martín, D.; Montañez-Aguilera, F.J.; Gallego-Izquierdo, T.; Urraca-Gesto, A.; Gómez-Conesa, A.; Romero-Franco, N.; Plaza-Manzano, G. Effectiveness of dry needling on the lower trapezius in patients with mechanical neck pain: A randomized controlled trial. Arch. Phys. Med. Rehabil. 2015, 96, 775–781. [Google Scholar] [CrossRef]
- Onat, S.S.; Polat, C.S.; Bicer, S.; Sahin, Z.; Tasoglu, O. Effect of dry needling injection and kinesiotaping on pain and quality of life in patients with mechanical neck pain. Pain Physician 2019, 22, 583–589. [Google Scholar]
- Myburgh, C.; Hartvigsen, J.; Aagaard, P.; Holsgaard-Larsen, A. Skeletal muscle contractility, self-reported pain and tissue sensitivity in females with neck/shoulder pain and upper Trapezius myofascial trigger points- a randomized intervention study. Chiropr. Man. Ther. 2012, 20, 36. [Google Scholar] [CrossRef]
- Mejuto-Vázquez, M.J.; Salom-Moreno, J.; Ortega-Santiago, R.; Truyols-Domínguez, S.; Fernández-De-Las-peñas, C. Short- Term changes in neck pain, widespread pressure pain sensitivity, and cervical range of motion after the application of trigger point dry needling in patients with acute mechanical neck pain: A randomized clinical trial. J. Orthop. Sports Phys. Ther. 2014, 44, 252–260. [Google Scholar] [CrossRef]
- Martín-Rodríguez, A.; Sáez-Olmo, E.; Pecos-Martín, D.; Calvo-Lobo, C. Effects of dry needling in the sternocleidomastoid muscle on cervical motor control in patients with neck pain: A randomised clinical trial. Acupunct. Med. 2019, 37, 151–163. [Google Scholar] [CrossRef]
- Manafnezhad, J.; Salahzadeh, Z.; Salimi, M.; Ghaderi, F.; Ghojazadeh, M. The effects of shock wave and dry needling on active trigger points of upper trapezius muscle in patients with non-specific neck pain: A randomized clinical trial. J. Back Musculoskelet. Rehabil. 2019, 32, 811–818. [Google Scholar] [CrossRef]
- Luan, S.; Zhu, Z.M.; Ruan, J.L.; Lin, C.N.; Ke, S.J.; Xin, W.J.; Liu, C.C.; Wu, S.L.; Ma, C. Randomized Trial on Comparison of the Efficacy of Extracorporeal Shock Wave Therapy and Dry Needling in Myofascial Trigger Points. Am. J. Phys. Med. Rehabil. 2019, 98, 677–684. [Google Scholar] [CrossRef]
- Llamas-Ramos, R.; Pecos-Martín, D.; Gallego-Izquierdo, T.; Llamas-Ramos, I.; Plaza-Manzano, G.; Ortega-Santiago, R.; Cleland, J.; Fernández-de-las-Peñas, C. Comparison of the short-term outcomes between trigger point dry needling and trigger point manual therapy for the management of chronic mechanical neck pain: A randomized clinical trial. J. Orthop. Sports Phys. Ther. 2014, 44, 852–861. [Google Scholar] [CrossRef]
- Itoh, K.; Katsumi, Y.; Hirota, S.; Kitakoji, H. Randomised trial of trigger point acupuncture compared with other acupuncture for treatment of chronic neck pain. Complement. Ther. Med. 2007, 15, 172–179. [Google Scholar] [CrossRef]
- Irnich, D.; Behrens, N.; Gleditsch, J.M.; Stör, W.; Schreiber, M.A.; Schöps, P.; Vickers, A.J.; Beyer, A. Immediate effects of dry needling and acupuncture at distant points in chronic neck pain: Results of a randomized, double-blind, sham-controlled crossover trial. Pain 2002, 99, 83–89. [Google Scholar] [CrossRef]
- Ziaeifar, M.; Arab, A.M.; Karimi, N.; Nourbakhsh, M.R. The effect of dry needling on pain, pressure pain threshold and disability in patients with a myofascial trigger point in the upper trapezius muscle. J. Bodyw. Mov. Ther. 2014, 18, 298–305. [Google Scholar] [CrossRef]
- Ibuldu, E.; Cakmak, A.; Disci, R.; Aydin, R. Comparison of laser, dry needling, and placebo laser treatments in myofascial pain syndrome. Photomed. Laser Surg. 2004, 22, 306–311. [Google Scholar] [CrossRef]
- Hayta, E.; Umdu, N.M. A randomized trial to study the comparison of trigger point dry needling versus Kinesio Taping technique in myofascial pain syndrome during a 3-month follow up. Int. J. Physiother. 2016, 3. [Google Scholar] [CrossRef]
- Fernández-Carnero, J.; Gilarranz-De-Frutos, L.; León-Hernández, J.V.; Pecos-Martin, D.; Alguacil-Diego, I.; Gallego-Izquierdo, T.; Martín-Pintado-Zugasti, A. Effectiveness of different deep dry needling dosages in the treatment of patients with cervical myofascial pain: A pilot RCT. Am. J. Phys. Med. Rehabil. 2017, 96, 726–733. [Google Scholar] [CrossRef] [PubMed]
- Doǧan, N.; Şengül, I.; Akçay-Yalbuzdaǧ, Ş.; Kaya, T. Kinesio taping versus dry needling in the treatment of myofascial pain of the upper trapezius muscle: A randomized, single blind (evaluator), prospective study. J. Back Musculoskelet. Rehabil. 2019, 32, 819–827. [Google Scholar] [CrossRef] [PubMed]
- De Meulemeester, K.E.; Castelein, B.; Coppieters, I.; Barbe, T.; Cools, A.; Cagnie, B. Comparing Trigger Point Dry Needling and Manual Pressure Technique for the Management of Myofascial Neck/Shoulder Pain: A Randomized Clinical Trial. J. Manipulative Physiol. Ther. 2017, 40, 11–20. [Google Scholar] [CrossRef]
- Campa-Moran, I.; Rey-Gudin, E.; Fernández-Carnero, J.; Paris-Alemany, A.; Gil-Martinez, A.; Lerma Lara, S.; Prieto-Baquero, A.; Alonso-Perez, J.L.; La Touche, R. Comparison of Dry Needling versus Orthopedic Manual Therapy in Patients with Myofascial Chronic Neck Pain: A Single-Blind, Randomized Pilot Study. Pain Res. Treat. 2015, 2015, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Aridici, R.; Yetisgin, A.; Boyaci, A.; Tutoglu, A.; Bozdogan, E.; Sen Dokumaci, D.; Kilicaslan, N.; Boyaci, N. Comparison of the Efficacy of Dry Needling and High-Power Pain Threshold Ultrasound Therapy with Clinical Status and Sonoelastography in Myofascial Pain Syndrome. Am. J. Phys. Med. Rehabil. 2016, 95, e149–e158. [Google Scholar] [CrossRef]
- Arias-Buría, J.L.; Monroy-Acevedo, Á.; Fernández-de-las-Peñas, C.; Gallego-Sendarrubias, G.M.; Ortega-Santiago, R.; Plaza-Manzano, G. Effects of dry needling of active trigger points in the scalene muscles in individuals with mechanical neck pain: A randomized clinical trial. Acupunct. Med. 2020. [Google Scholar] [CrossRef]
- García-de-Miguel, S.; Pecos-Martín, D.; Larroca-Sanz, T.; Sanz-de-Vicente, B.; Garcia-Montes, L.; Fernandez-Matias, R.; Gallego-Izquierdo, T. Short-term effects of PENS versus dry needling in subjects with unilateral mechanical neck pain and active myofascial trigger points in levator scapulae muscle: A randomized controlled trial. J. Clin. Med. 2020, 9, 1665. [Google Scholar] [CrossRef]
- Valiente-Castrillo, P.; Martín-Pintado-Zugasti, A.; Calvo-Lobo, C.; Beltran-Alacreu, H.; Fernández-Carnero, J. Effects of pain neuroscience education and dry needling for the management of patients with chronic myofascial neck pain: A randomized clinical trial. Acupunct. Med. 2020. [Google Scholar] [CrossRef]
- Tekin, L.; Akarsu, S.; Durmuş, O.; Çakar, E.; Dinçer, Ü.; Kiralp, M.Z. The effect of dry needling in the treatment of myofascial pain syndrome: A randomized double-blinded placebo-controlled trial. Clin. Rheumatol. 2013, 32, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Tabatabaiee, A.; Ebrahimi-Takamjani, I.; Ahmadi, A.; Sarrafzadeh, J.; Emrani, A. Comparison of pressure release, phonophoresis and dry needling in treatment of latent myofascial trigger point of upper trapezius muscle. J. Back Musculoskelet. Rehabil. 2019, 32, 587–594. [Google Scholar] [CrossRef]
- Sukareechai, C.; Sukareechai, S. Comparison of radial shockwave and dry needling therapies in the treatment of myofascial pain syndrome. Int. J. Ther. Rehabil. 2019, 26, 1–8. [Google Scholar] [CrossRef]
- Sobhani, V.; Shamsoddini, A.; Khatibi-aghda, A.; Mazloum, V.; Hesari, H.; Kazem, M.; Meybodi, E. Differences Among Effectiveness of Dry Needling, Manual Therapy, and Kinesio Taping® Methods for the Management of Patients with Chronic Myofascial Neck Pain: A Single-Blind Clinical Trial. Trauma Mon. 2017, 22, 1–8. [Google Scholar]
- Segura-Ortí, E.; Prades-Vergara, S.; Manzaneda-Piña, L.; Valero-Martínez, R.; Polo-Traverso, J.A. Trigger point dry needling versus strain-counterstrain technique for upper trapezius myofascial trigger points: A randomised controlled trial. Acupunct. Med. 2016, 34, 171–177. [Google Scholar] [CrossRef]
- Rayegani, S.M.; Bayat, M.; Bahrami, M.H.; Raeissadat, S.A.; Kargozar, E. Comparison of dry needling and physiotherapy in treatment of myofascial pain syndrome. Clin. Rheumatol. 2014, 33, 859–864. [Google Scholar] [CrossRef]
- Braithwaite, F.A.; Walters, J.L.; Li, L.S.K.; Moseley, G.L.; Williams, M.T.; McEvoy, M.P. Blinding Strategies in Dry Needling Trials: Systematic Review and Meta-Analysis. Phys. Ther. 2019, 99, 1461–1480. [Google Scholar] [CrossRef]
- Cleland, J.A.; Childs, J.D.; Whitman, J.M. Psychometric properties of the Neck Disability Index and Numeric Pain Rating Scale in patients with mechanical neck pain. Arch. Phys. Med. Rehabil. 2008, 89, 69–74. [Google Scholar] [CrossRef]
- Bijur, P.E.; Latimer, C.T.; Gallagher, E.J. Validation of a verbally administered numerical rating scale of acute pain for use in the emergency department. Acad. Emerg. Med. 2003, 10, 390–392. [Google Scholar] [CrossRef]
- Bialosky, J.E.; Beneciuk, J.M.; Bishop, M.D.; Coronado, R.A.; Penza, C.W.; Simon, C.B.; George, S.Z. Unraveling the Mechanisms of Manual Therapy: Modeling an Approach. J. Orthop. Sport. Phys. Ther. 2017, 48, 1–31. [Google Scholar] [CrossRef]
- Fernández-De-Las-Peñas, C.; Nijs, J. Trigger point dry needling for the treatment of myofascial pain syndrome: Current perspectives within a pain neuroscience paradigm. J. Pain Res. 2019, 12, 1899–1911. [Google Scholar] [CrossRef]
- DiLorenzo, L.; Traballesi, M.; Morelli, D.; Pompa, A.; Brunelli, S.; Buzzi, M.G.; Formisano, R. Hemiparetic shoulder pain syndrome treated with deep dry needling during early rehabilitation: A prospective, open-label, randomized investigation. J. Musculoskelet. Pain 2004, 12, 25–34. [Google Scholar] [CrossRef]
- Carlesso, L.C.; MacDermid, J.C.; Santaguida, L.P. Standardization of adverse event terminology and reporting in orthopaedic physical therapy: Application to the cervical spine. J. Orthop. Sports Phys. Ther. 2010, 40, 455–463. [Google Scholar] [CrossRef]
- Brady, S.; McEvoy, J.; Dommerholt, J.; Doody, C. Adverse events following trigger point dry needling: A prospective survey of chartered physiotherapists. J. Man. Manip. Ther. 2014, 22, 134–140. [Google Scholar] [CrossRef]
- Boyce, D.; Wempe, H.; Campbell, C.; Fuehne, S.; Zylstra, E.; Smith, G.; Wingard, C.; Jones, R. Adverse events aossciated with therapeutic dry needling. Int. J. Sports Phys. Ther. 2020, 15, 103–113. [Google Scholar] [CrossRef]
- Cummings, M.; Ross-Marrs, R.; Gerwin, R. Pneumothorax complication of deep dry needling demonstration. Acupunct. Med. 2014, 32, 517–519. [Google Scholar] [CrossRef]
- Uzar, T.; Turkmen, I.; Menekse, E.B.; Dirican, A.; Ekaterina, P.; Ozkaya, S. A case with iatrogenic pneumothorax due to deep dry needling. Radiol. Case Rep. 2018, 13, 1246–1248. [Google Scholar] [CrossRef]
- Mitchell, U.H.; Johnson, A.W.; Larson, R.E.; Seamons, C.T. Positional changes in distance to the pleura and in muscle thickness for dry needling. Physiotherapy 2019, 105, 362–369. [Google Scholar] [CrossRef]
- Folli, A.; Schneebeli, A.; Ballerini, S.; Mena, F.; Soldini, E.; Fernández-de-las-Peñas, C.; Barbero, M. Enhancing trigger point dry needling safety by ultrasound skin-to-rib measurement: An inter-rater reliability study. J. Clin. Med. 2020, 9, 1958. [Google Scholar] [CrossRef]
- Higgins, J.; Green, S. Cochrane Handbook for Systematic Review Interventions. 2011. Available online: http://handbook.cochrane.org (accessed on 31 July 2020).
- Mansfield, C.J.; Vanetten, L.; Willy, R.; di Stasi, S.; Magnussen, R.; Briggs, M. The Effects of Needling Therapies on Muscle Force Production: A Systematic Review and Meta-analysis. J. Orthop. Sports Phys. Ther. 2019, 49, 154–170. [Google Scholar] [CrossRef]
- Gattie, E.; Cleland, J.A.; Snodgrass, S. The Effectiveness of Trigger Point Dry Needling for Musculoskeletal Conditions by Physical Therapists: A Systematic Review and Meta-analysis. J. Orthop. Sport. Phys. Ther. 2017, 47, 133–149. [Google Scholar] [CrossRef]
| PubMed Search Formula |
| #1 “Dry Needling” (Mesh) OR “Trigger Point Acupuncture” (Title/Abstract) OR “Needling Therapy” (Title/Abstract) OR “Intramuscular Stimulation” (Title/Abstract) |
| #2 “Placebos” (Mesh) OR “Control Groups” (Mesh) OR “Physical Therapy Modalities” (Mesh) |
| OR “Cervical Pain” (Title/Abstract) OR “Mechanical Neck Pain” (Title/Abstract) OR “Myofascial Neck Pain” (Title/Abstract) |
| #4 #1 AND #2 AND #3 |
| CINAHL/Medline (via EBSCO) Search Formula |
| #1 “Dry Needling” OR “Trigger Point Acupuncture” OR “Needling Therapy” OR “Intramuscular Stimulation” |
| #2 “Placebos” OR “Control Groups” OR “Physical Therapy Modalities” |
| #3 “Neck Pain” OR “Non-Specific Neck Pain” OR “Cervicalgia” OR “Cervical Pain” OR “Mechanical Neck Pain” OR “Myofascial Neck Pain” |
| #4 #1 AND #2 AND #3 |
| SCOPUS Search Formula |
| TITLE-ABS-KEY (“Dry Needling” OR “Trigger Point Acupuncture” OR “Needling Therapy” OR “Intramuscular Stimulation”) AND TITLE-ABS-KEY (“Placebos” OR “Control Groups” OR “Physical Therapy Modalities”) AND TITLE-ABS-KEY (“Neck Pain” OR “Non-Specific Neck Pain” OR “Cervicalgia” OR “Cervical Pain” OR “Mechanical Neck Pain” OR “Myofascial Neck Pain”) |
| PEDro Search Formula |
| Abstract & Title: Neck Pain, Myofascial Pain Syndrome |
| Therapy: Dry Needling |
| Method: Clinical trial |
| When Searching: AND |
| WOS Search Formula |
| (“Dry Needling” OR “Trigger Point Acupuncture” OR “Needling Therapy” OR “Intramuscular Stimulation”) AND (“Placebos” OR “Control Groups” OR “Physical Therapy Modalities”) AND (“Neck Pain” OR “Non-Specific Neck Pain” OR “Cervicalgia” OR “Cervical Pain” OR “Mechanical Neck Pain” OR “Myofascial Neck Pain”) |
| Cochrane Library Search Formula |
| #1 Mesh: Dry Needling |
| #2 Mesh: Placebos |
| #3 Mesh: Neck Pain |
| #4 Trigger Point Acupuncture |
| #5 Needling Therapy |
| #6 Intramuscular Stimulation |
| #7 Mesh: Control Groups |
| #8 Mesh: Physical Therapy Modalities |
| #9 Nonspecific Neck Pain |
| #10 Cervicalgia |
| #11 Cervical Pain |
| #12 Mechanical Neck Pain |
| #13 Myofascial Neck Pain |
| #14 #1 OR #4 OR #5 OR #6 |
| #15 #2 OR #7 OR #8 |
| #16 #3 OR #9 OR #10 OR #11 OR #12 OR #13 |
| #17 #14 AND #15 AND #16 |
| Study | Diagnosis | Group | Total (Male/Female) | Age (SD), y | Pain Duration |
|---|---|---|---|---|---|
| Ibuldu et al. 2004 [36] | Myofascial Pain Syndrome | G1: DN + Self-Stretching | 20 | 35.3 (9.2) | 38.5 (31.95) m |
| G2: Laser + Self-Stretching | 20 | 33.9 (10.35) | 32.95 (28.6) m | ||
| G3: Placebo laser + Self-Stretching | 20 | 32.35 (6.9) | 36.95 (33.65) m | ||
| Itoh et al. 2007 [33] | Chronic Neck Pain | G1: TrP-DN | 8 | 62.3 (10.1) | 2.9 (2.7) y |
| G2: Non-TrP-DN | 8 | 65.0 (10.5) | 3.3 (3.9) y | ||
| G3: Sham Acupuncture | 7 | 65.0 (10.5) | 2.3 (1.5) y | ||
| G4: Acupuncture | 8 | 62.3 (11.0) | 3.2 (3.2) y | ||
| Myburgh et al. 2012 [27] | Myofascial Pain Syndrome | G1: TrP-DN | 17 | 46.1 | NR |
| G2: TrP-SDN | 20 | 46.1 | NR | ||
| Tekin et al. 2012 [46] | Myofascial Pain Syndrome | G1: TrP-DN | 22 (5/17) | 42.9 (10.9) | 63.5 (50.7) m |
| G2: TrP-Sham DN | 17 (3/14) | 42.0 (12.0) | 57.9 (48.3) m | ||
| Llamas-Ramos et al. 2014 [32] | Mechanical Neck Pain | G1: TrP-DN | 47 (17/30) | 31 (3) | 7.4 (2.6) m |
| G2: TrP-MT | 47 (15/32) | 31 (2) | 7.1 (2.9) m | ||
| Ziaeifar et al. 2014 [35] | Myofascial Pain Syndrome | G1: TrP-DN | 16 | 30.05 (9.9) | NR |
| G2: TrP-MT | 17 | 26.5 (8.6) | NR | ||
| Mejuto-Vázquez et al. 2014 [28] | Acute Mechanical Neck Pain | G1: TrP-DN | 9 (4/5) | 24 (7) | 3.4 (0.7) d |
| G2: No intervention | 8 (4/4) | 25 (4) | 3.1 (0.8) d | ||
| Rayegani et al. 2014 [51] | Myofascial Pain Syndrome | G1: TrP-DN | 14 | 32 (10) 38.6 | 9.6 (8.4) m 9.8 (9.6) m |
| G2: Physical Therapy | 14 | (4.2) | |||
| Campa-Mran et al. 2015 [41] | Myofascial Chronic Neck Pain | G1: TrP-DN + Passive Stretching | 12 (3/9) | 53.9 (12.7) | 10.0 (2.9) m |
| G2: Soft tissue techniques | 12 (2/10) | 45.8 (15.4) | 11.8 (4.4) m | ||
| G3: MT | 12 (2/10) | 48.7 (10.2) | 14.0 (3.6) m | ||
| Pecos-Martín et al. 2015 [25] | Chronic Mechanical Neck Pain | G1: TrP-DN | 36 (6/30) | 23 (5) | 5.7 (2.6) m |
| G2: Non-TrP-DN (Sham) | 36 (8/28) | 23 (6) | 7 (2.8) m | ||
| Aridici et al. 2016 [42] | Myofascial Pain Syndrome | G1: TrP-DN | 31 (5/26) | 40.5 (10.1) | 7.5 (3.0) |
| G2: High power pain threshold ultrasound therapy | 30 (3/27) | 38.1 (11.4) | 7.75 (3.0) | ||
| Segura-Ortí et al. 2016 [50] | Myofascial Pain Syndrome | G1: TrP-DN | 12 (4/8) | 30.0 (9.5) | NR |
| G2: Strain Counter-strain Technique | 10 (3/7) | 34.1 (11.5) | NR | ||
| G3: Sham Strain Counter-strain | 12 (2/10) | 32.9 (9.5) | NR | ||
| Hayta et al. 2016 [37] | Myofascial Pain Syndrome | G1: TrP-DN | 28 (7/21) | NR | NR |
| G2: Kinesiotaping | 27 (3/24) | NR | NR | ||
| Ziaeifar et al. 2016 [23] | Myofascial Pain Syndrome | G1: TrP-DN | 14 (0/14) | 30.1 (10.4) | NR |
| G2: TrP-MT | 17 (0/17) | 26.6 (9.4) | NR | ||
| Fernández-Carnero et al. 2017 [38] | Cervical Myofascial Pain | G1: 4 LTR DN | 21 (7/14) | 29.7 (11.9) | 9.7 (17.0) m |
| G2: 6 LTR DN | 21 (5/16) | 24.25 (9.4) | 16.85 (38.5) m | ||
| G3: +6 LTR DN | 21 (5/16) | 26.45 (10.7) | 19.2 (22.15) m | ||
| G4: Non-TrP DN | 21 (4/17) | 28.2 (11.4) | 8.4 (15.4) m | ||
| De Meulemeester et al. 2017 [40] | Myofascial Neck/Shoulder Syndrome | G1: TrP-DN | 22 | 40.5 (8.3) | 3: <3m; 19: >3m: |
| G2: TrP-MT | 0 | 36.1 (10.7) | 4: <3m; 16: >3m | ||
| Sobhani et al. 2017 [49] | Chronic Mechanical Neck Pain | G1: DN + Passive stretching | 13 | 34.6 (10.5) | 12.6 (4.4) m |
| G2: MT | 13 | 35.9 (11.4) | 15.1 (7.5) m | ||
| G3: Kinesiotaping | 13 | 34.6 (9.1) | 16.1 (7.6) m | ||
| Luan et al. 2019 [31] | Myofascial Pain Syndrome | G1: DN | 32 (11/21) | 33.1 (12.8) | 8.3 (3.1) m |
| G2: Extracorporeal Shock Wave | 30 (8/22) | 32.5 (10.6) | 8.9 (2.7) m | ||
| Dogan et al. 2019 [39] | Myofascial Pain Syndrome | G1: DN | 19 | 32.4 (12.4) | 12 (4–48) m |
| G2: Kinesiotaping | 23 | 33.6 (9.1) | 12 (4–60) m | ||
| Manafnezhad et al. 2019 [30] | Non-Specific Neck Pain | G1: DN | 35 | 39.2 (7.2) | 12 (3–60) m |
| G2: Extracorporeal Shock Wave | 35 | 37 (9.1) | 12 (3–80) m | ||
| Martín-Rodríguez et al. 2019 [29] | Non-Specific Neck Pain | G1: TrP-DN | 17 (6/11) | 43.6 (12.1) | 88.5 (105.1) m |
| G2: Non-TrP- DN | 14 (4/13) | 42.5 (12.3) | 58.9 (48.5) m | ||
| Tabatabaiee et al. 2019 [47] | Myofascial Pain Syndrome | G1: Latent-TrP DN | 20 | 23.6 (1.8) | NR |
| G2: TrP-MT | 20 | 23.5 (1.6) | NR | ||
| G3: Phonophoresis with betamethasone | 20 | 23.9 (3.1) | NR | ||
| Onat et al. 2019 [26] | Neck Pain | G1: TrP-DN + Home Exercise Program | 36 (7/29) | 44.1 (14.2) | NR |
| G2: Kinesiotaping + Home Exercise Program | 36 (10/26) | 45.1 (12.5) | NR | ||
| Ziaeifar et al. 2019 [24] | Myofascial Pain Syndrome | G1: TrP-DN | 16 | 30.05 (9.9) | NR |
| G2: TrP-MT | 17 | 26.5 (8.6) | NR | ||
| Sukareechai et al. 2019 [48] | Myofascial Pain Syndrome | G1: TrP-DN | 21 (0/21) | 42.7 (12.4) | 36 (3, 120) m |
| G2: Radial Shockwave | 21 (2/19) | 38.2 (11.9) | 24 (1, 120) m | ||
| Arias-Buría et al. 2020 [43] | Mechanical Neck Pain | G1: TrP-DN | 15 (10/5) | 21 (3) | 7.5 (1.3) m |
| G2: TrP-MT | 15 (11/4) | 22 (2) | 8.0 (1.1) m | ||
| Valiente-Castrillo et al. 2020 [45] | Chronic Myofascial Neck Pain | G1: TrP-DN | 20 (4/16) | 40.3 (11.95) | 43.4 (56.55) m |
| G2: TrP-DN + pain neuroscience education | 21 (2/19) | 40.35 (8.0) | 64.95 (62.9) m | ||
| G3: Usual Care | 19 (3/16) | 42.35 (9.4) | 56.3 (67.75) m | ||
| García-de-Miguel et al. 2020 [44] | Unilateral Mechanical Neck Pain | G1: TrP-DN | 22 (9/13) | 25.45 (8.5) | >3 m |
| G2: PENS | 22 (7/15) | 24.15 (9.4) | >3 m |
| Study | Group | TrP criteria | Technique Used | No. Punctures for Patient in Every Intervention | Needle Approach (Targeted Muscles or Tendon) | Gauge (mm) | Depth (mm) | Time of DN | Frequency of Incisions (Hz) | Number of Incisions in Every Needle Intervention | LTR | Therapist that Performed Intervention |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ibuldu et al. 2004 [36] | G1: DN | Yes | NR | 1 | Upper trapezius | 0.25 × 25 | NR | NR | NR | NR | NR | Physician |
| Itoh et al. 2007 [33] | G1: DN-Trp | Yes | “sparrow pecking” technique | NR | Splenius capitis, Upper trapezius, sternocleidomastoid, scalenus, levator scapulae, suboccipital | 0.2 × 0.50 mm | 20 mm | 10 min | 1 | The manipulation was stopped when the LTR was elicited | Yes | Acupuncturist |
| G2: Acupuncture | No | “sparrow pecking” technique | 9 | GB20, GB21, BL10, BL11, S12, S13, TE5, LI4, SI3 | 0.2 × 0.40 mm | 20 mm | 10min | 1 | When the subject felt dull pain or the acupuncture sensation (de qi), the manipulation was stopped | No | Acupuncturist | |
| G3: DN-Non-TrP | Yes | “sparrow pecking” technique | NR | Splenius capitis, upper trapezius, sternocleidomastoid, scalenus, levator scapulae, suboccipital | 0.2 × 0.40 mm | 0 mm | 10 min | 1 | The manipulation was stopped when the LTR was elicited | Yes | Acupuncturis | |
| Myburgh et al. 2012 [27] | G1: DN | Yes | Repeated fanning needling insertion | 1 | Upper trapezius | 32 × 0.25 mm | No less than 10 mm | 90 sg | NR | Elicit and exhaust LTR | Yes | Clinician |
| G2: Superficial DN | Yes | The needle inserted into the epidermis until | 1 | Upper trapezius | 32 × 0.25 mm | 5 mm | 90 sg | 1 | 1 | No | Clinician | |
| Tekin et al. 2012 [46] | G1: DN | Yes | Needle moved forward until the TrP was reached | 6 | Neck and shoulder muscles | 0.25 × 0.25 mm | Until muscle | NR | 1 | 1 | No | Physician |
| G2: Sham-DN | Yes | The blunted needle for sham dry needling | 6 | Neck and shoulder muscles | 0.25 × 0.25 mm | Until skin | NR | 1 | 1 | No | Physician | |
| Llamas-Ramos et al. 2014 [32] | G1: DN | Yes | Hong | 1 | Upper trapezius | 0.30 × 30 mm | 10–15 mm | 20–30 sg | 1 | Once the first LTR was obtained, the needle was moved up and down | Yes | Physiotherapist |
| Mejuto-Vázquez et al. 2014 [28] | G1: DN | Yes | Hong | 1 | Upper trapezius | 0.30 × 30 mm | 10–15 mm | 20–30 sg | 1 | Once the first LTR was obtained, the needle was moved up and down | Yes | Physiotherapist |
| Ziaeifar et al. 2014 [35] | G1: DN | Yes | Hong | 1 | Upper trapezius | NR | NR | NR | NR | Was repeatedly needled forward and backward to the TrP until there were no more LTRs | Yes | Physiotherapist |
| Rayegani et al. 2014 [51] | G1: DN | Yes | NR | 2 | Upper trapezius | 23-gauge needle | NR | NR | NR | NR | No | Physician |
| Campa-Moran et al. 2015 [41] | G1: DN | Yes | Hong | 2 | Levator scapulae and upper trapezius muscles | 0.25 × 25 mm | Until muscle | 2 min | At least 3 times at each point | The needle insertions were repeated to achieve at least three LTR | Yes | Physiotherapist |
| Pecos-Martín et al. 2015 [25] | G1: TrP-DN | Yes | Hong | 1 | Lower trapezius | 0.25 × 25 mm | Until muscle | NR | NR | 8-10 times | No | Physiotherapist |
| G2: Non-TrP-DN | No | Hong | 1 | Lower trapezius | 0.25 × 25 mm | 1.5cm medially from TrP | NR | NR | 8–10 times | No | Physiotherapist | |
| Aridici et al. 2016 [42] | G1: DN | Yes | Hong | 1 | Upper trapezius | 22-gauge needle and 1.5 inch | Until muscle | NR | NR | 8–10 times | Yes | Physician |
| Hayta et al. 2016 [37] | G1: DN | Yes | Manual stimulation was produced (at the TrP) by rotating the needle counterclockwise | 3 | Trapezius | 0.25 × 25 mm | Inside of muscle | 10–20 min | 1 | 1 | No | NR |
| Segura-Ortí et al. 2016 [50] | G1: DN | Yes | Hong | 1 | Upper trapezius | 0.25 × 25 mm | Inside of muscle | NR | NR | Needling at the TrP was continued until the LTR was exhausted | Yes | Physiotherapist |
| Ziaeifar et al. 2016 [23] | G1: DN | Yes | Hong | 1 | Upper trapezius | 0.30 × 50 mm | Inside of muscle | NR | NR | The procedure was repeated until there was no more LTR | Yes | Therapist |
| Fernández-Carnero et al. 2017 [38] | G1: No-LTR-DN | Yes | Hong | 1 | Upper trapezius | 0.32 × 40 mm | Inside of muscle, 1.5 cm away from TrP | NR | NR | 1 | No | Therapist |
| G2: 4-LTR-DN | Ye | Hong | 1 | Upper trapezius | 0.32 × 40 mm | Inside TrP | NR | NR | 10 times | Yes | Therapist | |
| G3: 6-LTr-DN | Ye | Hong | 1 | Upper trapezius | 0.32 × 40 mm | Inside TrP | NR | NR | 10 times | Yes | Therapist | |
| G4: More-6-LTR-DN | Ye | Hong | 1 | Upper trapezius | 0.32 × 40 mm | Inside TrP | NR | NR | 10 times | Yes | Therapist | |
| Sobhani et al. 2017 [49] | G1: DN | Yes | NR | 2 | Upper trapezius and levator scapulae muscles | NR | NR | NR | 20 min | NR | No | Therapist |
| Dogan et al. 2019 [39] | G1: DN | Yes | Hong and the needles were kept in the TrP for ten minutes, after which they were turned counterclockwise several times | 1 | Upper trapezius | 0.20 × 40 mm | Until TrP | 10 min | NR | At least 3 insertions and 1 LTR | Yes | Physician |
| Luan et al. 2019 [31] | G1: DN | Yes | Hong | 1 | Upper trapezius | 0.30 × 50 mm | 30–35 mm | NR | NR | 10 | Yes | Physiotherapist |
| Manafnezhad et al. 2019 [30] | G1: DN | Yes | Hong | 1 | Upper trapezius | 0.30 × 0.50 mm | Until TrP | 1–2 min | NR | Until at least one or two LTR were obtained | Yes | Physiotherapist |
| Martín-Rodríguez et al. 2019 [29] | G1: DN | Yes | Hong | 1 | Sternocleidomastoid muscle | 0.25 × 0.25 mm | Until TrP | NR | NR | 8–10 | No | Physiotherapist |
| G2: DN | Yes | Hong | 1 | Sternocleidomastoid muscle | 0.25 × 0.25 mm | 1.5cm away the TrP | NR | NR | 8–10 | No | Physiotherapist | |
| Onat et al. 2019 [26] | G1: DN | Yes | Hong | 1 | The posterior muscles of the cervical spine | NR | Until TrP | NR | NR | 6–8 | No | Physician |
| Tabatabaiee et al. 2019 [47] | G1: DN | Yes | Hong | 1 | Upper trapezius | 0.25 × 40 mm | Until TrP | NR | 60 sg | Until a LTR was elicited | Yes | Physiotherapist |
| Ziaeifar et al. 2019 [24] | G1: DN | Yes | Hong | 1 | Upper trapezius | 0.30 × 50 mm | Until TrP | NR | NR | After eliciting LTR, needling was stopped. If no twitch was elicited, needling was stopped after 2-3 stellate movements | Yes | Therapist |
| Sukareechai et al. 2019 [48] | G1: DN | Yes | Multiple needle entry technique | NR | Upper trapezius, rhomboid and infraspinatus muscle | 0.25 × 50 mm | NR | NR | NR | NR | No | NR |
| Arias-Buría et al. 2020 [43] | G1: DN | Yes | Hong | 1 | Anterior scalene muscle | 0.30 × 30 mm | Until TrP | 25–30 sg | 1 | Until the first LTR was obtained | Yes | Physiotherapist |
| García-de-Miguel et al. 2020 [44] | G1: DN | Yes | Hong | 1 | Levator scapulae | 0.25 × 25 mm | Until TrP | NR | NR | 8–10 times | No | Physiotherapist |
| G2: PENS | Yes | Hong and electrostimulation asymmetric current at a 2-Hz with a pulse width of 100 us | 2 | Levator scapulae | 0.25 × 25 mm | Until TrP | 20 min | NR | 8–10 times | No | Physiotherapist | |
| Valiente-Castrillo et al. 2020 [45] | G1: DN | Yes | Hong | 4 | Upper trapezius, levator scapulae, cervical multifidus, and splenius cervicis | 032x40 mm | Until TrP | NR | NR | Until to obtain five LTR | Yes | Physiotherapist |
| Study | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | TOTAL |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Ibuldu et al. 2004 [36] | Y | N | Y | Y | N | Y | Y | N | Y | Y | 7/10 |
| Itoh et al. 2007 [33] | Y | N | Y | Y | N | Y | N | N | Y | Y | 6/10 |
| Myburgh et al. 2012 [27] | Y | N | Y | Y | N | Y | Y | N | Y | Y | 7/10 |
| Tekin et al. 2012 [46] | Y | N | Y | Y | N | Y | Y | N | Y | Y | 7/10 |
| Llamas-Ramos et al. 2014 [32] | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 |
| Mejuto-Vázquez et al. 2014 [28] | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7/10 |
| Ziaeifar et al. 2014 [35] | Y | N | Y | N | N | N | Y | N | Y | Y | 5/10 |
| Rayegani et al. 2014 [51] | Y | N | Y | N | N | N | N | N | Y | Y | 4/10 |
| Campa-Moran et al. 2015 [41] | Y | N | N | N | N | Y | Y | Y | Y | Y | 6/10 |
| Pecos-Martín et al. 2015 [25] | Y | N | Y | Y | N | Y | Y | Y | Y | Y | 8/10 |
| Aridici et al. 2016 [42] | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 |
| Hayta et al. 2016 [37] | Y | N | Y | N | N | Y | Y | N | Y | Y | 6/10 |
| Segura-Ortí et al. 2016 [50] | Y | Y | Y | N | N | Y | N | N | Y | Y | 6/10 |
| Ziaeifar et al. 2016 [23] | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
| Fernández-Carnero et al. 2017 [38] | Y | Y | Y | Y | N | Y | Y | N | Y | Y | 8/10 |
| Sobhani et al. 2017 [49] | Y | N | Y | N | N | Y | N | N | Y | Y | 5/10 |
| De Meulemeester et al. 2017 [40] | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7/10 |
| Dogan et al. 2019 [39] | Y | N | Y | N | N | Y | Y | N | Y | Y | 6/10 |
| Luan et al. 2019 [31] | Y | Y | Y | N | N | Y | Y | N | Y | Y | 7/10 |
| Manafnezhad et al. 2019 [30] | Y | N | Y | N | N | Y | Y | N | Y | Y | 6/10 |
| Martín-Rodríguez et al. 2019 [29] | Y | Y | Y | Y | N | Y | Y | N | Y | Y | 8/10 |
| Onat et al. 2019 [26] | Y | Y | Y | N | N | N | Y | Y | Y | Y | 7/10 |
| Tabatabaiee et al. 2019 [47] | Y | N | Y | N | N | N | Y | N | Y | Y | 5/10 |
| Ziaeifar et al. 2019 [24] | Y | N | Y | N | N | N | Y | N | Y | Y | 5/10 |
| Sukareechai et al. 2019 [48] | Y | N | Y | N | N | N | Y | Y | Y | Y | 6/10 |
| Arias-Buría et al. 2020 [43] | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 |
| García-de-Miguel et al. 2020 [44] | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 |
| Valiente-Castrillo et al. 2020 [45] | Y | Y | Y | N | N | Y | Y | Y | Y | Y | 8/10 |
| Ibuldu et al. 2004 [36] | No data about adverse events were provided. |
| Itoh et al. 2007 [33] | One patient in the sham group was excluded due to deterioration of symptoms. No adverse events were observed during treatment. |
| Myburgh et al. 2012 [27] | Within the DN group, 5 patients (29.4%) perceived post-needling soreness, and 8 patients (47.1%) perceived muscle strength soreness (diffuse muscle fatigue) 48 hours postintervention. Within the sham needling group, 9 patients (45%) experienced post-needling soreness. |
| Tekin et al. 2012 [46] | No data about adverse events were provided. |
| Rayegani et al. 2014 [51] | No data about adverse events were provided. |
| Llamas-Ramos et al. 2014 [32] | Twenty-six patients (55%) assigned to DN group experienced post-needling soreness. Eleven patients assigned to manual therapy group experienced muscle fatigue. All minor adverse events resolved spontaneously within 24-48 h without further treatment. |
| Ziaeifar et al. 2014 [35] | No data about adverse events were provided. |
| Mejuto-Vázquez et al. 2014 [28] | Eighty-eight percent (88%) of patients assigned in the DN group experienced post-needling soreness. This minor adverse event resolved spontaneously within 24-36 h without further treatment. |
| Campa-Moran et al. 2015 [41] | No adverse effect was registered after the needling application. |
| Pecos-Martín et al. 2015 [25] | No data about adverse events were provided. |
| Aridici et al. 2016 [42] | No data about adverse events were provided. |
| Segura-Ortí et al. 2016 [50] | Two subjects assigned to the DN group dropped out due to aversion to needles. No other adverse event was observed. |
| Hayta et al. 2016 [37] | No data about adverse events were provided. |
| Ziaeifar et al. 2016 [23] | No data about adverse events were provided. |
| Sobhani et al. 2017 [49] | No data about adverse events were provided. |
| Fernández-Carnero et al. 2017 [38] | Ninety-one percent (91%) of the patients reported post-needling soreness. No other adverse effects were reported |
| De Meulemeester et al. 2017 [40] | Post-needling soreness. No other adverse effects were reported. |
| Luan et al. 2019 [31] | No adverse effects were observed during the study. |
| Dogan et al. 2019 [39] | No adverse effects were observed during the study. |
| Manafnezhad et al. 2019 [30] | No data about adverse events were provided. |
| Martín-Rodríguez et al. 2019 [29] | Within the non-trigger point DN group, three patients (17.6%) experimented contralateral side pain, 4 patients (23.5%) suffered headache, one patient (5.9%) earache, and one (5.9%) hematoma. Within the trigger point DN group, three patients (17.6%) experimented contralateral side pain and one patient (2.9%) post-needling soreness. |
| Tabatabaiee et al. 2019 [47] | No data about adverse events were provided. |
| Onat et al. 2019 [26] | Three patients (8.3%) in the DN group experienced an increase in neck pain after dry needling, and 2 patients (5.5%) in the Kinesiotaping group showed cutaneous irritation. |
| Ziaeifar et al. 2019 [24] | No data about adverse events were provided. |
| Sukareechai et al. 2019 [48] | Some participants experienced soreness after dry needling therapy. |
| Arias-Buría et al. 2020 [43] | Six patients assigned to the DN experienced post-needling soreness, but it resolved spontaneously. |
| Valiente-Castrillo et al. 2020 [45] | Ninety percent (90%) patients presented post-needling soreness after DN, but it resolved spontaneously. |
| García-de-Miguel et al. 2020 [44] | No data about adverse events were provided. |
| Number of Studies | Risk of Bias | Inconsistency | Indirectness of Evidence | Imprecision | Publication Bias | Quality of Evidence | MD or SMD (95% CI) |
|---|---|---|---|---|---|---|---|
| Dry Needling vs. Sham/Control vs. Physical Therapy Modalities on Neck Pain Intensity | |||||||
| Immediate Follow-Up (less than 1 week after single session) | |||||||
| Overall effect (n = 11) | No | Serious (I2 = 77%) | No | No | No | Moderate | MD −0.75 (−1.43 to −0.06) * |
| Sham/Placebo/Waiting list/Other form of Dry Needling (n = 6) | No | Serious (I2 = 58%) | No | Serious | No | Low | MD −1.53 (−2.29 to −0.76) * |
| Manual Therapy (n = 3) | No | No (I2 = 0%) | No | Very Serious | No | Low | MD 0.19 (−0.61 to 1.00) |
| Other Physical Therapy Intervention (n = 2) | No | No (I2 = 0%) | No | Very Serious | No | Low | MD −0.07 (−0.51 to 0.37) |
| Short-term Follow-Up (1 to 12 weeks after intervention) | |||||||
| Overall effect (n = 24) | No | Very Serious (I2 = 87%) | No | No | No | Low | MD −0.65 (−1.09 to −0.22) * |
| Sham/Placebo/waiting list/Other form of Dry Needling (n = 6) | No | Very Serious (I2 = 87%) | No | No | No | Low | MD −2.31 (−3.64 to −0.99) * |
| Manual Therapy (n = 7) | No | Serious (I2 = 46%) | No | No | No | Moderate | MD −0.53 (−0.97 to −0.09) * |
| Other Physical Therapy Intervention (n = 13) | No | Serious (I2 = 44%) | No | No | No | Moderate | MD 0.10 (−0.21 to 0.41) |
| Mid-term Follow-Up (more than 12 weeks after intervention) | |||||||
| Overall effect (n = 5) | No | No (I2 = 28%) | No | Very Serious | No | Low | MD −0.27 (−0.73 to 0.18) |
| Manual Therapy (v = 2) | No | No (I2 = 0%) | No | Very Serious | No | Low | MD −0.75 (−1.70 to 0.20) |
| Other Physical Therapy Intervention (n = 3) | No | Serious (I2 = 47%) | No | Very Serious | No | Very Low | MD −0.19 (−0.75 to 0.38) |
| Dry Needling vs. Sham/Control vs. Physical Therapy Modalities on Pain-Related Disability | |||||||
| Short-term Follow-Up (1 to 12 weeks after intervention) | |||||||
| Overall effect (n = 20) | No | Serious (I2 = 58%) | No | No | Yes | Low | SMD −0.26 (−0.48 to −0.05) * |
| Sham/Placebo/Waiting list/Other form of Dry Needling (n = 5) | No | Serious (I2 = 79%) | No | No | No | Moderate | SMD −0.87 (−1.60 to −0.14) * |
| Manual Therapy (n = 7) | No | No (I2 = 23%) | No | No | No | High | SMD −0.20 (−0.49 to 0.10) |
| Other Physical Therapy Intervention (n = 9) | No | No (I2 = 12%) | No | No | No | High | SMD −0.07 (−0.27 to 0.13) |
| Mid-term Follow-Up (more than 12 weeks after intervention) | |||||||
| Overall effect (n = 5) | No | Serious (I2 = 48%) | No | Very Serious | No | Very Low | SMD −0.33 (−0.70 to 0.05) |
| Manual Therapy (n = 2) | No | No (I2 = 0%) | No | Very Serious | No | Low | SMD −0.40 (−0.88 to 0.08) |
| Other Physical Therapy Intervention (n = 3) | No | Serious (I2 = 71%) | No | Very Serious | No | Very Low | SMD −0.29 (−0.88 to 0.31) |
| Dry Needling vs. Sham/Control vs. Physical Therapy Modalities on Pressure Pain Thresholds | |||||||
| Immediate Follow-Up (less than 1 week after single session) | |||||||
| Overall effect (n = 9) | No | Very Serious (I2 = 92%) | No | No | No | Low | MD 4.93 (−42.18 to 52.04) |
| Sham/Placebo/Waiting list/Other form of dry needling (n = 4) | No | No (I2 = 28%) | No | Serious | No | Moderate | MD 55.48 (27.03 to 83.93) * |
| Manual Therapy (n = 3) | No | No (I2 = 0%) | No | Very Serious | No | Low | MD −11.77 (−37.02 to 13.47) |
| Other Physical Therapy Intervention (n = 2) | No | Very Serious (I2 = 97%) | No | Very Serious | No | Very Low | MD −58.34 (−159.05 to 42.38) |
| Short-term Follow-Up (1 to 12 weeks after intervention) | |||||||
| Overall effect (n = 17) | No | Very Serious (I2 = 95%) | No | No | No | Low | MD 6.84 (−33.41 to 47.12) |
| Sham/Placebo/Waiting list/Other form of dry needling (n = 3) | No | Very Serious (I2 = 90%) | No | Very Serious | No | Very Low | MD 75.53 (−9.82 to 160.88) |
| Manual Therapy (n = 6) | No | Serious (I2 = 75%) | No | No | No | Moderate | MD 32.25 (−1.02 to 65.52) |
| Other Physical Therapy Intervention (n = 8) | No | Very Serious (I2 = 93%) | No | No | No | Low | MD −33.89 (−89.44 to 21.66) |
| Number of studies | Risk of bias | Inconsistency | Indirectness of evidence | Imprecision | Publication bias | Quality of evidence | MD or SMD (95% CI) |
| Dry Needling vs. Sham/Control vs. Physical Therapy Modalities on Cervical Range of Motion | |||||||
| Cervical Flexion (Immediate Follow-Up, less than 1 week after single session) | |||||||
| Overall effect (n = 5) | No | Very Serious (I2 = 83%) | No | Very Serious | No | Very Low | MD 1.93 (−5.90, 9.77) |
| Sham/Placebo/Waiting list/Other form of dry needling (n = 3) | No | Very Serious (I2 = 83%) | No | Very Serious | No | Very Low | MD 7.51 (−3.23, 18.25) |
| Manual Therapy (n = 1) | No | No | No | Very Serious | No | Low | MD −6.43 (−17.96, 5.10) |
| Other Physical Therapy Intervention (n = 1) | No | No | No | Very Serious | No | Low | MD −6.37 (−11.09, −1.65) |
| Cervical Flexion (Short-term Follow-Up, 1 to 12 weeks after intervention) | |||||||
| Overall effect (n = 10) | No | Very Serious (I2 = 85%) | No | No | No | Low | MD 1.26 (−3.06, 5.58) |
| Sham/Placebo/Waiting list/Other form of dry needling (n = 3) | No | Very Serious (I2 = 87%) | No | Very Serious | No | Very Low | MD 6.76 (−4.53, 18.06) |
| Manual Therapy (n = 3) | No | No (I2 = 0%) | No | Very Serious | No | Low | MD 0.26 (−2.07, 2.60) |
| Other Physical Therapy Intervention (n = 4) | No | Very Serious (I2 = 92%) | No | Very Serious | No | Very Low | MD −1.74 (−10.51, 7.03) |
| Cervical Extension (Immediate Follow-Up, less than 1 week after single session) | |||||||
| Overall effect (n = 5) | No | Serious (I2 = 63%) | No | Very Serious | No | Very Low | MD 5.23 (−1.05, 11.51) |
| Sham/Placebo/Waiting list/Other form of dry needling (n = 3) | No | Serious (I2 = 77%) | No | Very Serious | No | Very Low | MD 8.70 (−1.94, 19.35) |
| Manual Therapy (n = 1) | No | No | No | Very Serious | No | Low | MD 1.95 (−11.47, 15.37) |
| Other Physical Therapy Intervention (n = 1) | No | No | No | Very Serious | No | Low | MD 0.68 (−5.01, 6.37) |
| Cervical Extension (Short-term Follow-Up, 1 to 12 weeks after intervention) | |||||||
| Overall effect (n = 10) | No | Serious (I2 = 72%) | No | No | Yes | Low | MD 0.34 (−3.02, 3.70) |
| Sham/Placebo/Waiting list/Other form of dry needling (n = 3) | No | Serious (I2 = 66%) | No | Very Serious | No | Very Low | MD 8.26 (−1.36, 17.88) |
| Manual Therapy (n = 3) | No | No (I2 = 0%) | No | Very Serious | No | Low | MD −0.21 (−2.70, 2.28) |
| Other Physical Therapy Intervention (n = 4) | No | Very Serious (I2 = 85%) | No | Very Serious | No | Very Low | MD −3.04 (−9.94, 3.87) |
| Cervical Lateral-Flexion (Immediate Follow-Up, less than 1 week after single session) | |||||||
| Overall effect (n = 4) | No | Serious (I2 = 67%) | No | Very Serious | No | Very Low | MD 2.65 (−2.07, 7.37) |
| Sham/Placebo/Waiting list/Other form of dry needling (n = 3) | No | Serious (I2 = 57%) | No | Very Serious | No | Very Low | MD 4.54 (−1.41, 10.48) |
| Other Physical Therapy Intervention (n = 1) | No | No | No | Very Serious | No | Low | MD −0.95 (−2.07, 7.37) |
| Cervical Lateral-Flexion (Short-term Follow-Up, 1 to 12 weeks after intervention) | |||||||
| Overall effect (n = 10) | No | Very Serious (I2 = 86%) | No | No | No | Low | MD 0.30 (−1.00, 1.61) |
| Sham/Placebo/Waiting list/Other form of dry needling (n = 3) | No | Serious (I2 = 66%) | No | Very Serious | No | Very Low | MD 3.21 (−2.28, 8.70) |
| Manual Therapy (n = 3) | No | Serious (I2 = 77%) | No | Very Serious | No | Very Low | MD 1.09 (−1.11, 3.28) |
| Other Physical Therapy Intervention (n = 6) | No | No (I2 = 25%) | No | No | No | High | MD −0.58 (−1.59, 0.42) |
| Cervical Rotation (Immediate Follow-Up, less than 1 week after single session) | |||||||
| Overall effect (n = 4) | No | Serious (I2 = 60%) | No | Very Serious | No | Very Low | MD 2.04 (−4.08, 8.15) |
| Sham/Placebo/Waiting list/Other form of dry needling (n = 3) | No | No (I2 = 22%) | No | Very Serious | No | Low | MD 4.51 (−0.96, 9.98) |
| Other Physical Therapy Intervention (n = 1) | No | No | No | Very Serious | No | Low | MD −3.77 (−9.58, 2.04) |
| Cervical Rotation (Short-term Follow-Up, 1 to 12 weeks after intervention) | |||||||
| Overall effect (n = 9) | No | Serious (I2 = 74%) | No | No | Yes | Low | MD −0.23 (−1.40, 1.09) |
| Sham/Placebo/Waiting list/Other form of dry needling (n = 3) | No | Serious (I2 = 71%) | No | Very Serious | No | Very Low | MD 6.20 (−1.08, 13.48) |
| Manual Therapy (n = 3) | No | Serious (I2 = 70%) | No | Very Serious | No | Very Low | MD −0.52 (−1.91, 0.87) |
| Other Physical Therapy Intervention (n = 5) | No | Serious (I2 = 47%) | No | Very Serious | No | Very Low | MD −0.82 (−2.73, 1.09) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Navarro-Santana, M.J.; Sanchez-Infante, J.; Fernández-de-las-Peñas, C.; Cleland, J.A.; Martín-Casas, P.; Plaza-Manzano, G. Effectiveness of Dry Needling for Myofascial Trigger Points Associated with Neck Pain Symptoms: An Updated Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 3300. https://doi.org/10.3390/jcm9103300
Navarro-Santana MJ, Sanchez-Infante J, Fernández-de-las-Peñas C, Cleland JA, Martín-Casas P, Plaza-Manzano G. Effectiveness of Dry Needling for Myofascial Trigger Points Associated with Neck Pain Symptoms: An Updated Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2020; 9(10):3300. https://doi.org/10.3390/jcm9103300
Chicago/Turabian StyleNavarro-Santana, Marcos J., Jorge Sanchez-Infante, César Fernández-de-las-Peñas, Joshua A. Cleland, Patricia Martín-Casas, and Gustavo Plaza-Manzano. 2020. "Effectiveness of Dry Needling for Myofascial Trigger Points Associated with Neck Pain Symptoms: An Updated Systematic Review and Meta-Analysis" Journal of Clinical Medicine 9, no. 10: 3300. https://doi.org/10.3390/jcm9103300
APA StyleNavarro-Santana, M. J., Sanchez-Infante, J., Fernández-de-las-Peñas, C., Cleland, J. A., Martín-Casas, P., & Plaza-Manzano, G. (2020). Effectiveness of Dry Needling for Myofascial Trigger Points Associated with Neck Pain Symptoms: An Updated Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 9(10), 3300. https://doi.org/10.3390/jcm9103300







