Photo-Optical Transcutaneous Oxygen Tension Measurement Is of Added Value to Predict Diabetic Foot Ulcer Healing: An Observational Study
Abstract
1. Introduction
2. Methods
2.1. Study Population
2.2. Study Procedure
2.3. Outcome Parameters
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Morbach, S.; Furchert, H.; Groblinghoff, U.; Hoffmeier, H.; Kersten, K.; Klauke, G.T.; Klemp, U.; Roden, T.; Icks, A.; Haastert, B.; et al. Long-term prognosis of diabetic foot patients and their limbs: Amputation and death over the course of a decade. Diabetes Care 2012, 35, 2021–2027. [Google Scholar] [CrossRef] [PubMed]
- Adler, A.I.; Erqou, S.; Lima, T.A.; Robinson, A.H. Association between glycated haemoglobin and the risk of lower extremity amputation in patients with diabetes mellitus-review and meta-analysis. Diabetologia 2010, 53, 840–849. [Google Scholar] [CrossRef] [PubMed]
- Skrepnek, G.H.; Armstrong, D.G.; Mills, J.L. Open bypass and endovascular procedures among diabetic foot ulcer cases in the United States from 2001 to 2010. J. Vasc. Surg. 2014, 60, 1255–1265. [Google Scholar] [CrossRef] [PubMed]
- Edmonds, M. Modern treatment of infection and ischaemia to reduce major amputation in the diabetic foot. Curr. Pharm. Des. 2013, 19, 5008–5015. [Google Scholar] [CrossRef]
- Siersma, V.; Thorsen, H.; Holstein, P.E.; Kars, M.; Apelqvist, J.; Jude, E.B.; Piaggesi, A.; Bakker, K.; Edmonds, M.; Jirkovska, A.; et al. Importance of factors determining the low health-related quality of life in people presenting with a diabetic foot ulcer: The Eurodiale study. Diabet. Med. 2013, 30, 1382–1387. [Google Scholar] [CrossRef]
- Brownrigg, J.R.; Schaper, N.C.; Hinchliffe, R.J. Diagnosis and assessment of peripheral arterial disease in the diabetic foot. Diabet. Med. 2015, 32, 738–747. [Google Scholar] [CrossRef]
- Wang, Z.; Hasan, R.; Firwana, B.; Elraiyah, T.; Tsapas, A.; Prokop, L.; Mills, J.L.; Murad, M.H. A systematic review and meta-analysis of tests to predict wound healing in diabetic foot. J. Vasc. Surg. 2016, 63, 29S–36S.e2. [Google Scholar] [CrossRef]
- Shi, Y.; Vanhoutte, P.M. Macro- and microvascular endothelial dysfunction in diabetes. J. Diabetes 2017, 9, 434–449. [Google Scholar] [CrossRef]
- Vesterager, P. Transcutaneous Po2 electrode. Scand. J. Clin. Lab. Investig. Suppl. 1977, 146, 27–30. [Google Scholar] [CrossRef]
- Urban, M.; Fouasson-Chailloux, A.; Signolet, I.; Colas Ribas, C.; Feuilloy, M.; Abraham, P. Comparison of two devices for measuring exercise transcutaneous oxygen pressures in patients with claudication. Vasa 2015, 44, 355–362. [Google Scholar] [CrossRef]
- Rumsey, W.L.; Vanderkooi, J.M.; Wilson, D.F. Imaging of phosphorescence: A novel method for measuring oxygen distribution in perfused tissue. Science 1988, 241, 1649–1651. [Google Scholar] [CrossRef] [PubMed]
- Mills, J.L.; Conte, M.S.; Armstrong, D.G.; Pomposelli, F.B.; Schanzer, A.; Sidawy, A.N.; Andros, G.; Society for Vascular Surgery Lower Extremity Guidelines Writing Group. The Society for Vascular Surgery Lower Extremity Threatened Limb Classification System: Risk stratification based on wound, ischemia, and foot infection (WIfI). J. Vasc. Surg. 2014, 59, 220–234. [Google Scholar] [CrossRef] [PubMed]
- Mathioudakis, N.; Hicks, C.W.; Canner, J.K.; Sherman, R.L.; Hines, K.F.; Lum, Y.W.; Perler, B.A.; Abularrage, C.J. The Society for Vascular Surgery Wound, Ischemia, and foot Infection (WIfI) classification system predicts wound healing but not major amputation in patients with diabetic foot ulcers treated in a multidisciplinary setting. J. Vasc. Surg. 2017, 65, 1698–1705.e1691. [Google Scholar] [CrossRef] [PubMed]
- Hicks, C.W.; Canner, J.K.; Mathioudakis, N.; Sherman, R.; Malas, M.B.; Black, J.H., 3rd; Abularrage, C.J. The Society for Vascular Surgery Wound, Ischemia, and foot Infection (WIfI) classification independently predicts wound healing in diabetic foot ulcers. J. Vasc. Surg. 2018, 68, 1096–1103. [Google Scholar] [CrossRef]
- Aboyans, V.; Ricco, J.B.; Bartelink, M.L.E.L.; Bjorck, M.; Brodmann, M.; Cohnert, T.; Collet, J.P.; Czerny, M.; De Carlo, M.; Debus, S.; et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur. Heart J. 2018, 39, 763. [Google Scholar] [CrossRef]
- Leenstra, B. Photo-optical transcutaneous oxygen tension measurement in patients with peripheral arterial disease. J. Cardiovasc. Surg. 2019. Submitted. [Google Scholar]
- Ubbink, D.T.; Jacobs, M.J.; Tangelder, G.J.; Slaaf, D.W.; Reneman, R.S. The usefulness of capillary microscopy, transcutaneous oximetry and laser Doppler fluxmetry in the assessment of the severity of lower limb ischaemia. Int. J. Microcirc. Clin. Exp. 1994, 14, 34–44. [Google Scholar] [CrossRef]
- Kalani, M.; Brismar, K.; Fagrell, B.; Ostergren, J.; Jorneskog, G. Transcutaneous oxygen tension and toe blood pressure as predictors for outcome of diabetic foot ulcers. Diabetes Care 1999, 22, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Ballard, J.L.; Eke, C.C.; Bunt, T.J.; Killeen, J.D. A prospective evaluation of transcutaneous oxygen measurements in the management of diabetic foot problems. J. Vasc. Surg. 1995, 22, 485–492. [Google Scholar] [CrossRef]
- Norgren, L.; Hiatt, W.R.; Dormandy, J.A.; Nehler, M.R.; Harris, K.A.; Fowkes, F.G.; Group, T.I.W. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). J. Vasc. Surg. 2007, 45, S5–S67. [Google Scholar] [CrossRef]
- Faglia, E.; Clerici, G.; Caminiti, M.; Quarantiello, A.; Curci, V.; Morabito, A. Predictive values of transcutaneous oxygen tension for above-the-ankle amputation in diabetic patients with critical limb ischemia. Eur. J. Vasc. Endovasc. Surg. 2007, 33, 731–736. [Google Scholar] [CrossRef] [PubMed]
- Ladurner, R.; Kuper, M.; Konigsrainer, I.; Lob, S.; Wichmann, D.; Konigsrainer, A.; Coerper, S.; Beckert, S. Predictive value of routine transcutaneous tissue oxygen tension (tcpO2) measurement for the risk of non-healing and amputation in diabetic foot ulcer patients with non-palpable pedal pulses. Med. Sci. Monit. 2010, 16, CR273–CR277. [Google Scholar] [PubMed]
- Dhatariya, K.K.; Li Ping Wah-Pun Sin, E.; Cheng, J.O.S.; Li, F.Y.N.; Yue, A.W.Y.; Gooday, C.; Nunney, I. The impact of glycaemic variability on wound healing in the diabetic foot-A retrospective study of new ulcers presenting to a specialist multidisciplinary foot clinic. Diabetes Res. Clin. Pract. 2018, 135, 23–29. [Google Scholar] [CrossRef] [PubMed]
- Diabetes Control and Complications Trial Research Group. Effect of intensive diabetes treatment on the development and progression of long-term complications in adolescents with insulin-dependent diabetes mellitus: Diabetes Control and Complications Trial. J. Pediatr. 1994, 125, 177–188. [Google Scholar] [CrossRef]
- Lipsky, B.A.; Berendt, A.R.; Cornia, P.B.; Pile, J.C.; Peters, E.J.; Armstrong, D.G.; Deery, H.G.; Embil, J.M.; Joseph, W.S.; Karchmer, A.W.; et al. 2012 infectious diseases society of america clinical practice guideline for the diagnosis and treatment of diabetic foot infections. J. Am. Podiatr. Med. Assoc. 2013, 103, 2–7. [Google Scholar] [CrossRef] [PubMed]
- Manu, C.; Lacopi, E.; Bouillet, B.; Vouillarmet, J.; Ahluwalia, R.; Ludemann, C.; Garcia-Klepzig, J.L.; Meloni, M.; De Buruaga, V.R.; Sanchez-Rios, J.P.; et al. Delayed referral of patients with diabetic foot ulcers across Europe: Patterns between primary care and specialised units. J. Wound Care 2018, 27, 186–192. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |

| Baseline Characteristics | Healed (n = 68) | Non-Healed (n = 35) | p |
|---|---|---|---|
| Sex (male) (percentage) | 44 (64.7) | 28 (80.0) | 0.109 |
| Age (σ | 71 (12.3) | 69 (12.8) | 0.701 |
| BMI (n, %) | 0.196 | ||
| <25 | 37 (54.4) | 21 (60.0) | |
| 25–30 | 26 (3.2) | 8 (22.9) | |
| 30> | 3 (4.4) | 5 (14.3) | |
| n/a | 2 (2.9) | 1 (2.9) | |
| Smoking history (n, %) | 0.641 | ||
| Active | 12 (21.8) | 9 (31.0) | |
| Former smoker | 22 (40.0) | 12 (41.4) | |
| Non-smoker | 18 (32.7) | 6 (20.7) | |
| n/a | 3 (5.5) | 2 (6.9) | |
| Hypertension (%) | 32 (47.1) | 21 (60.0) | 0.213 |
| Dyslipidemia (%) | 35 (51.5) | 20 (58.8) | 0.482 |
| HBA1c (sd) | 63.0 (15.8) | 62.9 (17.5) | 0.866 |
| Wound Healing Outcome | (Patients, n) |
|---|---|
| Healed | 68 |
| Non-healed | 35 |
| Amputation | 29 |
| Deterioration without amputation | 6 |
| Wound Classification | All (n = 103) | Healed (n = 68) | Non-Healed (n = 35) | p |
|---|---|---|---|---|
| Wound location (n, %) | 0.271 | |||
| Toe | 60 (58.3) | 37 (54.5) | 23 (65.7) | |
| Foot | 43 (41.7) | 31 (45.6) | 12 (34.3) | |
| WIfI classification | ||||
| Wound (n, %) | 0.003 | |||
| 1 | 81 (78.6) | 60 (88.2) | 21 (60.0) | |
| 2 | 21 (20.4) | 8 (11.8) | 13 (37.1) | |
| 3 | 1 (1.0) | 0 (0) | 1 (2.9) | |
| Ischemia (n, %) | 0.231 | |||
| 0 | 43 (41.7) | 32 (47.1) | 11 (31.4) | |
| 1 | 37 (35.9) | 25 (36.8) | 12 (34.3) | |
| 2 | 8 (7.8) | 4 (5.9) | 4 (11.4) | |
| 3 | 6 (5.8) | 2 (2.9) | 4 (11.4) | |
| Not measurable (n, %) | 9 (8.7) | 5 (7.4) | 4 (11.4) | |
| Foot Infection (n, %) | 0.194 | |||
| 0 | 72 (69.9) | 50 (73.5) | 22 (62.9) | |
| 1 | 14 (13.6) | 10 (14.7) | 4 (11.4) | |
| 2 | 17 (16.5) | 8 (11.8) | 9 (25.7) |
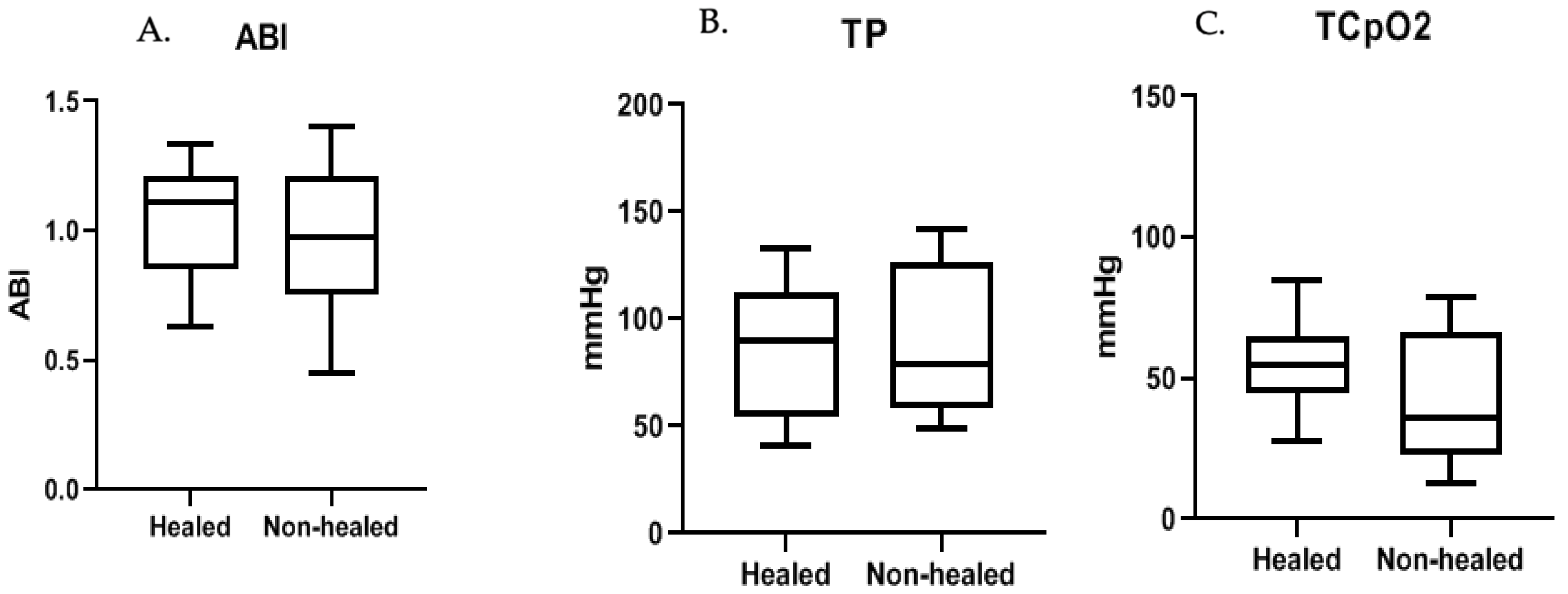
| Measurements | All (n = 103) | Healed (n = 68) | Non-Healed (n = 35) | p |
|---|---|---|---|---|
| Brachial pressure (mmHg, σ) | 152 | 149 (24) | 157 (28) | 0.128 |
| Ankle pressure (mmHg, σ) | 150 | 152 (45) | 145 (54) | 0.531 |
| Toe-pressure (mmHg, σ) | 89 | 88 (36) | 91 (38) | 0.799 |
| TCpO2 reference probe (mmHg, σ) | 72 | 75 (29) | 68 (22) | 0.177 |
| TCpO2 forefoot (mmHg, σ) | 51 | 55 (21) | 41 (24) | 0.005 |
| Ankle-brachial index (σ) | 1.00 | 1.03 (0.28) | 0.96 (0.37) | 0.386 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Leenstra, B.; de Kleijn, R.; Kuppens, G.; Verhoeven, B.A.N.; Hinnen, J.W.; de Borst, G.J. Photo-Optical Transcutaneous Oxygen Tension Measurement Is of Added Value to Predict Diabetic Foot Ulcer Healing: An Observational Study. J. Clin. Med. 2020, 9, 3291. https://doi.org/10.3390/jcm9103291
Leenstra B, de Kleijn R, Kuppens G, Verhoeven BAN, Hinnen JW, de Borst GJ. Photo-Optical Transcutaneous Oxygen Tension Measurement Is of Added Value to Predict Diabetic Foot Ulcer Healing: An Observational Study. Journal of Clinical Medicine. 2020; 9(10):3291. https://doi.org/10.3390/jcm9103291
Chicago/Turabian StyleLeenstra, Bernard, Robert de Kleijn, Geoffrey Kuppens, Bart Arnoldus Nicolaas Verhoeven, Jan Willem Hinnen, and Gert J. de Borst. 2020. "Photo-Optical Transcutaneous Oxygen Tension Measurement Is of Added Value to Predict Diabetic Foot Ulcer Healing: An Observational Study" Journal of Clinical Medicine 9, no. 10: 3291. https://doi.org/10.3390/jcm9103291
APA StyleLeenstra, B., de Kleijn, R., Kuppens, G., Verhoeven, B. A. N., Hinnen, J. W., & de Borst, G. J. (2020). Photo-Optical Transcutaneous Oxygen Tension Measurement Is of Added Value to Predict Diabetic Foot Ulcer Healing: An Observational Study. Journal of Clinical Medicine, 9(10), 3291. https://doi.org/10.3390/jcm9103291






