Health-Related Quality of Life in Male Patients under Treatment for Substance Use Disorders with and without Major Depressive Disorder: Influence in Clinical Course at One-Year Follow-Up
Abstract
1. Introduction
2. Experimental Section
2.1. Participants
2.2. Procedure
2.3. Measures
2.3.1. Sociodemographic and Clinical Variables
2.3.2. Health-Related Quality of Life
2.3.3. Statistical Analysis
3. Results
3.1. Results in Sociodemographic and Clinical Variables
3.2. Results in Health-Related Quality of Life for the SUD and SUD + MDD Groups
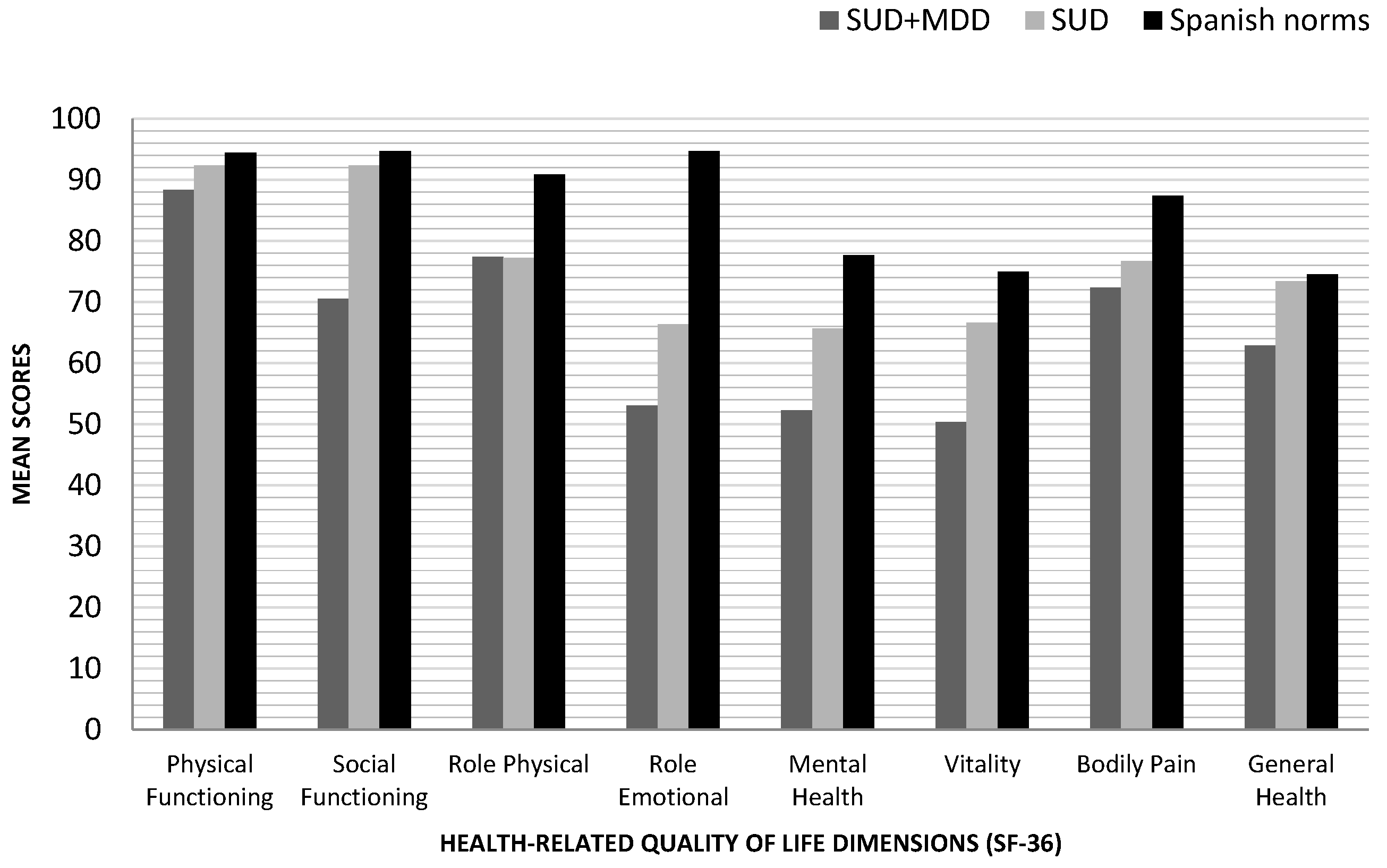
3.3. Population Values in the SF-36 and Scores Obtained in the SUD and SUD + MDD Groups
3.4. Predictive Value of Health-Related Quality of Life Dimensions at 3, 6, and 12 Months of Follow-Up
4. Discussion
Predictive Value of HRQoL Dimensions
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Juel, A.; Kristiansen, C.B.; Madsen, N.J.; Munk-Jørgensen, P.; Hjorth, P. Interventions to improve lifestyle and quality-of-life in patients with concurrent mental illness and substance use. Nord. J. Psychiatry 2016, 41, 1–8. [Google Scholar]
- Abdel-Baki, A.; Ouellet-Plamondon, C.; Salvat, É.; Grar, K.; Potvin, S. Symptomatic and functional outcomes of substance use disorder persistence 2 years after admission to a first-episode psychosis program. Psychiatry Res. 2017, 247, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Worley, J. Recovery in substance use disorders: What to know to inform practice. Issues Ment. Health Nurs. 2016, 2840, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Ibáñez, C.; Cáceresa, J.; Brucher, R.; Seijas, D. Trastornos del ánimo y trastornos por uso de sustancias: Una comorbilidad compleja y frecuente. Rev. Médica Clínica Las Condes 2020, 31, 174–182. [Google Scholar] [CrossRef]
- Daigre, C.; Perea-Ortueta, M.; Berenguer, M.; Esculies, O.; Sorribes-Puertas, M.; Palma-Alvarez, R.; Martínez-Luna, N.; Ramos-Quiroga, J.A.; Grau-López, L. Psychiatric factors affecting recovery after a long term treatment program for substance use disorder. Psychiatry Res. 2019, 276, 283–289. [Google Scholar] [CrossRef]
- Marquez-Arrico, J.E.; Río-Martínez, L.; Navarro, J.; Prat, G.; Forero, D.; Adan, A. Coping strategies in male patients under treatment for substance use disorders and/or severe mental illness: Influence in clinical course at one-year follow-up. J. Clin. Med. 2019, 8, 1972. [Google Scholar] [CrossRef]
- De Moura, A.; Pinto, R.; Ferros, L.; Jongenelen, I.; Negreiros, J. Efficacy indicators of four methods in outpatient addiction treatment. Arch. Clin. Psychiatry 2017, 44, 117–121. [Google Scholar] [CrossRef][Green Version]
- Aguiar, P.; Neto, D.; Lambaz, R.; Chick, J.; Ferrinho, P. Prognostic factors during outpatient treatment for alcohol dependence: Cohort study with 6 months of treatment follow-up. Alcohol Alcohol. 2012, 47, 702–710. [Google Scholar] [CrossRef]
- Laudet, A.B. The case for considering quality of life in addiction research and clinical practice. Addict. Sci. Clin. Pract. 2011, 6, 44–55. [Google Scholar]
- Hansebout, R.R.; Cornacchi, S.D.; Haines, T.; Goldsmith, C. How to use article about prognosis. Contin. Med. Educ. 2009, 52, 328–336. [Google Scholar]
- Croft, P.; Altman, D.G.; Deeks, J.J.; Dunn, K.M.; Hay, A.D.; Hemingway, H.; LeResche, L.; Peat, G.; Perel, P.; Petersen, S.E.; et al. The science of clinical practice: Disease diagnosis or patient prognosis? Evidence about “what is likely to happen” should shape clinical practice. BMC Med. 2015, 13, 20. [Google Scholar] [CrossRef]
- Díaz-Morán, S.; Palma-Álvarez, R.F.; Grau-López, L.; Daigre, C.; Barral, C.; Ros-Cucurull, E.; Casas, M.; Roncero, C. Self-perceived quality of life in cocaine dependents with or without dual diagnosis. Salud Ment. 2015, 38, 397–402. [Google Scholar] [CrossRef]
- Saarijärvi, S.; Salminen, J.K.; Toikka, T.; Raitasalo, R. Health-related quality of life among patients with major depression. Nord. J. Psychiatry 2002, 56, 261–264. [Google Scholar] [CrossRef] [PubMed]
- Lozano, Ó.M.; Rojas, A.J.; Calderón, F.F. Psychiatric comorbidity and severity of dependence on substance users: How it impacts on their health-related quality of life? J. Ment. Health 2017, 26, 119–126. [Google Scholar] [CrossRef] [PubMed]
- Adan, A.; Marquez-Arrico, J.E.; Gilchrist, G. Comparison of health-related quality of life among men with different co-existing severe mental disorders in treatment for substance use. Health Qual. Life Outcomes 2017, 15, 209. [Google Scholar] [CrossRef] [PubMed]
- Marquez-Arrico, J.E.; Río-Martínez, L.; Navarro, J.F.; Prat, G.; Adan, A. Personality profile and clinical correlates of patients with substance use disorder with and without comorbid depression under treatment. Front. Psychiatry 2019, 9, 764. [Google Scholar] [CrossRef]
- Benaiges, I.; Prat, G.; Adan, A. Health-related quality of life in patients with dual diagnosis: Clinical correlates. Health Qual. Life Outcomes 2012, 10, 106. [Google Scholar] [CrossRef]
- Astals, M.; Domingo-salvany, A.; Buenaventura, C.C.; Tato, J.; Vazquez, J.M.; Martín-Santos, R.; Torrens, M. Impact of substance dependence and dual diagnosis on the quality of life of heroin users seeking. Subst. Use Misuse 2009, 43, 612–632. [Google Scholar] [CrossRef]
- Lai, H.M.X.; Cleary, M.; Sitharthan, T.; Hunt, G.E. Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta-analysis. Drug Alcohol Depend. 2015, 154, 1–13. [Google Scholar] [CrossRef]
- Arya, S.; Singh, P.; Gupta, R. Psychiatric comorbidity and quality of life in patients with alcohol dependence syndrome. Indian J. Soc. Psychiatry 2017, 33, 336–341. [Google Scholar] [CrossRef]
- Brook, J.S.; Zhang, C.; Rubenstone, E.; Primack, B.A.; Brook, D.W. Comorbid trajectories of substance use as predictors of antisocial personality disorder, major depressive episode, and generalized anxiety disorder. Addict. Behav. 2016, 62, 114–121. [Google Scholar] [CrossRef] [PubMed]
- Davis, L.; Uezato, A.; Newell, J.M.; Frazier, E. Major depression and comorbid substance use disorders. Curr. Opin. Psychiatry 2008, 21, 14–18. [Google Scholar] [CrossRef]
- Tang, A.L.; Thomas, S.J.; Larkin, T. Cortisol, oxytocin, and quality of life in major depressive disorder. Qual. Life Res. 2019, 28, 2919–2928. [Google Scholar] [CrossRef]
- Giammanco, M.D.; Gitto, L. Coping, uncertainty and health-related quality of life as determinants of anxiety and depression on a sample of hospitalized cardiac patients in Southern Italy. Qual. Life Res. 2016, 25, 2941–2956. [Google Scholar] [CrossRef]
- Kristjánsdóttir, J.; Olsson, G.I.; Sundelin, C.; Naessen, T. Could SF-36 be used as a screening instrument for depression in a Swedish youth population? Scand. J. Caring Sci. 2011, 25, 262–268. [Google Scholar] [CrossRef] [PubMed]
- ten Doesschate, M.C.; Koeter, M.W.J.; Bockting, C.L.H.; Schene, A.H. Health related quality of life in recurrent depression: A comparison with a general population sample. J. Affect. Disord. 2010, 120, 126–132. [Google Scholar] [CrossRef]
- Lin, C.H.; Yen, Y.C.; Chen, M.C.; Chen, C.C. Depression and pain impair daily functioning and quality of life in patients with major depressive disorder. J. Affect. Disord. 2014, 166, 173–178. [Google Scholar] [CrossRef]
- Cho, Y.; Lee, J.K.; Kim, D.H.; Park, J.H.; Choi, M.; Kim, H.J.; Nam, M.J.; Lee, K.U.; Han, K.; Park, Y.G. Factors associated with quality of life in patients with depression: A nationwide population-based study. PLoS ONE 2019, 14, e0219455. [Google Scholar] [CrossRef] [PubMed]
- Shumye, S.; Belayneh, Z.; Mengistu, N. Health related quality of life and its correlates among people with depression attending outpatient department in Ethiopia: A cross sectional study. Health Qual. Life Outcomes 2019, 17, 1–9. [Google Scholar] [CrossRef]
- Torrens, M.; Gilchrist, G.; Domingo-Salvany, A. Psychiatric comorbidity in illicit drug users: Substance-induced versus independent disorders. Drug Alcohol Depend. 2011, 113, 147–156. [Google Scholar] [CrossRef]
- Boschloo, L.; van den Brink, W.; Penninx, B.W.J.H.; Wall, M.M.; Hasin, D.S. Alcohol-use disorder severity predicts first-incidence of depressive disorders. Psychol. Med. 2012, 42, 695–703. [Google Scholar] [CrossRef] [PubMed]
- Aharonovich, E.; Liu, X. Suicide attempts in substance abusers: Effects of major depression in relation to substance use disorders. Am. J. Psychiatry 2002, 159, 1600–1602. [Google Scholar] [CrossRef] [PubMed]
- Samet, S.; Fenton, M.C.; Nunes, E.; Greenstein, E.; Aharonovich, E.; Hasin, D. Effects of independent and substance-induced major depressive disorder on remission and relapse of alcohol, cocaine and heroin dependence. Addiction 2013, 108, 115–123. [Google Scholar] [CrossRef]
- Dagher, R.K.; Green, K.M. Does depression and substance abuse co-morbidity affect socioeconomic status? Evidence from a prospective study of urban African Americans. Psychiatry Res. 2014, 30, 115–121. [Google Scholar] [CrossRef][Green Version]
- Green, C.A.; Yarborough, M.T.; Polen, M.R.; Janoff, S.L.; Yarborough, B.J.H. Dual recovery among people with serious mental illnesses and substance problems: A qualitative analysis. J. Dual Diagn. 2015, 11, 33–41. [Google Scholar] [CrossRef]
- Garner, B.R.; Scott, C.K.; Dennis, M.L.; Funk, R.R. The relationship between recovery and health-related quality of life. J. Subst. Abus. Treat. 2014, 47, 293–298. [Google Scholar] [CrossRef][Green Version]
- Ware, J.E.; Sherbourne, C.D. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med. Care 1992, 30, 473–483. [Google Scholar] [CrossRef]
- Tiffany, S.T.; Friedman, L.; Greenfield, S.F.; Hasin, D.S.; Jackson, R. Beyond drug use: A systematic consideration of other outcomes in evaluations of treatments for substance use disorders. Addiction 2012, 107, 709–718. [Google Scholar] [CrossRef]
- Torrens, M. Quality of life as a means of assessing outcome in opioid dependence treatment. Heroin Addict. Relat. Clin. Probl. 2008, 11, 33–36. [Google Scholar]
- Griffin, M.L.; Bennett, H.E.; Fitzmaurice, G.M.; Hill, K.P.; Provost, S.E.; Weiss, R.D. Health-related quality of life among prescription opioid-dependent patients: Results from a multi-site study. Am. J. Addict. 2015, 24, 308–314. [Google Scholar] [CrossRef]
- Silveira, E.; Taft, C.; Sundh, V.; Waern, M.; Palsson, S.; Steen, B. Performance of the SF-36 Health Survey in screening for depressive and anxiety disorders in an elderly female Swedish population. Qual. Life Res. 2005, 14, 1263–1274. [Google Scholar] [CrossRef] [PubMed]
- Teoh Bing Fei, J.; Yee, A.; Habil, M.H. Bin Psychiatric comorbidity among patients on methadone maintenance therapy and its influence on quality of life. Am. J. Addict. 2016, 25, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Aydemir, O.; Ergün, H.; Soygür, H.; Kesebir, S.; Tulunay, C. Quality of life in major depressive disorder: A cross-sectional study. Turk. J. Psychiatry 2009, 20, 205–212. [Google Scholar] [CrossRef]
- American Psychiatric Association. Manual Diagnóstico y Estadístico de los Trastornos Mentales: DSM-5; Editorial Médica Panamericana: Madrid, Spain, 2014; ISBN 9788498358100. [Google Scholar]
- Gálvez, B.P.; Fernández, L.G. Validación española del drug abuse screening test (DAST-20 y DAST-10). Salud y Drogas 2010, 10, 35–50. [Google Scholar]
- Lobo, A.; Chamorro, L.; Luque, A.; Dal-ré, R.; Badia, X.; Baró, E. Validación de las versiones en español de la Montgomery-Asberg Depression Rating Scale y la Hamilton Anxiety Rating Scale para la evaluación de la depresión y de la ansiedad. Med. Clin. 2002, 118, 493–499. [Google Scholar] [CrossRef]
- Bobes, J.; González, M.P.; Bascarán, M.T.; Corominas, A.; Adan, A.; Sánchez, J.; Such, P. Validación de la versión española de la Escala de Adaptación Social en depresivos. Actas Esp. Psiquiatr. 1999, 27, 71–80. [Google Scholar]
- Alonso, J.; Regidor, E.; Barrio, G.; Prieto, L. Valores poblacionales de referencia de la versión española del Cuestionario de Salud SF-36. Med. Clin. 1998, 36, 1–10. [Google Scholar]
- Boden, J.M.; Fergusson, D.M. Alcohol and depression. Addiction 2011, 106, 906–914. [Google Scholar] [CrossRef]
- Adan, A. A cronobiological approach to addiction. J. Subst. Use 2013, 18, 171–183. [Google Scholar] [CrossRef]
- Mangione, K.K.; Miller, A.H.; Naughton, I.V. Cochrane Review: Improving physical function and training in older adults. Phys. Ther. 2010, 90, 1711–1715. [Google Scholar] [CrossRef]
- Cao, Y.; Li, W.; Shen, J.; Malison, R.T.; Zhang, Y. Health-related quality of life and symptom severity in Chinese patients with major depressive disorder. Asia-Pac. Psychiatry 2013, 5, 276–283. [Google Scholar] [CrossRef] [PubMed]
| SUD + MDD (N = 114) | SUD (N = 123) | Statistical Contrast | |
|---|---|---|---|
| Sociodemographic Data | |||
| Age (years) | 41.55 ± 8.64 | 37.32 ± 8.27 | t(235) = 3.83 *** |
| Marital status | χ2(4) = 9.77 | ||
| Single | 46.4% | 56.6% | |
| Stable partner | 6.3% | 7.4% | |
| Married | 8.9% | 13.9% | |
| Separated/divorced | 35.7% | 22.2% | |
| Widower | 2.7% | 0% | |
| Years of schooling | 11.17 ± 2.84 | 10.75 ± 2.43 | t(235) = 1.23 |
| Economic situation | χ2(4) = 30.02 *** | ||
| Active | 10.7% | 28.7% | |
| Unemployed | 25.9% | 28.7% | |
| Disability pension | 44.6% | 14.8% | |
| Sick leave (due SUD treatment) | 8.9% | 10.7% | |
| No income | 9.8% | 17.2% | |
| Medical and Psychiatric Data | |||
| Medical disease comorbidity a | 50% | 31% | χ2(6) = 14.98 ** |
| Hypercholesterolemia | 9.5% | 2.4% | |
| Respiratory system disease | 10.7% | 8.2% | |
| Hepatitis | 8.0% | 7.4% | |
| Diabetes | 3.6% | 1.6% | |
| Hypertension | 6.3% | 2.5% | |
| HIV | 4.5% | 5.7% | |
| Other | 2.5% | 6.3% | |
| Daily number of medications | 2.94 ± 1.63 | 0.83 ± 1.27 | t(235) = 10.97 *** |
| Type of medication prescribed a | |||
| Antidepressants | 71.0% | 18.9% | χ2(1) = 63.93 *** |
| Anxiolytics | 42.4% | 9.8% | χ2(1) = 33.16 *** |
| Mood Stabilizers | 42.6% | 13.9% | χ2(1) = 25.96 *** |
| Disulfiram | 26.2% | 15.2% | χ2(1) = 4.45 |
| Other | 28.7% | 13.9% | χ2(1) = 25.78 *** |
| History of suicide attempt | 46.4% | 19.0% | χ2(1)=21.72 ** |
| Number of lifetime suicidal attempts | 1.06 ± 2.08 | 0.32 ± 0.77 | t(235) = 3.65 *** |
| SUD-Related Data | |||
| Quantity of substance used a | 2.69 ± 1.48 | 2.56 ± 1.64 | t(235) = 0.66 |
| Substance of use a | |||
| Alcohol | 83.0% | 72.1% | χ2(1) = 3.96 |
| Cocaine | 76.8% | 86.9% | χ2(1) = 5.27 |
| Cannabis | 42.9% | 39.3% | χ2(1) = 0.98 |
| Hallucinogens | 19.6% | 18.9% | χ2(1) = 0.23 |
| Opioids | 18.8% | 16.4% | χ2(1) = 0.22 |
| Sedatives | 14.3% | 6.6% | χ2(1) = 3.78 |
| DAST-20 | 13.10 ± 4.40 | 12.73 ± 3.78 | t(235) = 0.65 |
| Main substance of dependence | χ2(4) = 7.88 | ||
| Alcohol | 12.5% | 10.4% | |
| Cocaine | 11.5% | 12.4% | |
| Alcohol and cocaine | 34.9% | 34.4% | |
| Alcohol and sedatives | 2.7% | 1.8% | |
| Polydrug use | 38.4% | 41.0% | |
| Mean abstinence period (months) | 9.95 ± 5.65 | 7.52 ± 2.93 | t(235) = 1.40 |
| Substance use disorder age onset (years) | 21.56 ± 9.71 | 20.63 ± 7.70 | t(235) = 0.81 |
| Years of substance use disorder | 19.10 ± 10.69 | 15.93 ±9.32 | t(235) = 2.44 |
| Symptomatic SUD + MDD (N = 51) | Asymptomatic SUD + MDD (N = 63) | Statistical Contrast | |
|---|---|---|---|
| Major depressive disorder age onset (years) | 28.65 ± 9.35 | 30.16 ±8.78 | t = 0.865 |
| Years of major depressive disorder | 13.96 ±9.46 | 10.50 ± 7.93 | t = −2.60 |
| Hamilton Depression Rating Scale | 12.39 ± 4.78 | 4.03 ± 3.08 | t = −7.48 *** |
| Social Adaption Self-evaluation Scale | 34.80 ± 8.21 | 38.43 ± 7.51 | t = −1.45 |
| SF-36 Dimensions | SUD + MDD (N = 114) | SUD (N = 123) | F(2,235) | ηp2 |
|---|---|---|---|---|
| Physical Functioning | 88.34 ± 1.35 | 92.36 ± 1.30 | 4.443 * | 0.019 |
| Social Functioning | 70.50 ± 2.50 | 78.65 ± 2.40 | 5.334 * | 0.022 |
| Role Physical | 77.42 ± 3.25 | 77.20 ± 3.12 | 0.002 | 0.001 |
| Role Emotional | 53.07 ± 3.72 | 66.39 ± 3.57 | 6.471 * | 0.027 |
| Mental Health | 52.29 ± 1.59 | 65.65 ± 1.53 | 35.458 *** | 0.133 |
| Vitality | 50.36 ± 1.73 | 66.61 ± 1.66 | 44.550 *** | 0.161 |
| Bodily Pain | 72.34 ± 2.53 | 76.68 ± 2.44 | 1.479 | 0.006 |
| General Health | 62.84 ± 1.75 | 73.42 ± 1.68 | 18.436 *** | 0.074 |
| Health Change item | 77.50 ± 2.21 | 90.64 ± 2.12 | 17.849 *** | 0.071 |
| Physical Composite Scale | 60.19 ± 1.54 | 61.39 ± 1.48 | 0.305 | 0.001 |
| Mental Composite Scale | 42.71 ± 1.63 | 51.60 ± 1.56 | 14.961 *** | 0.061 |
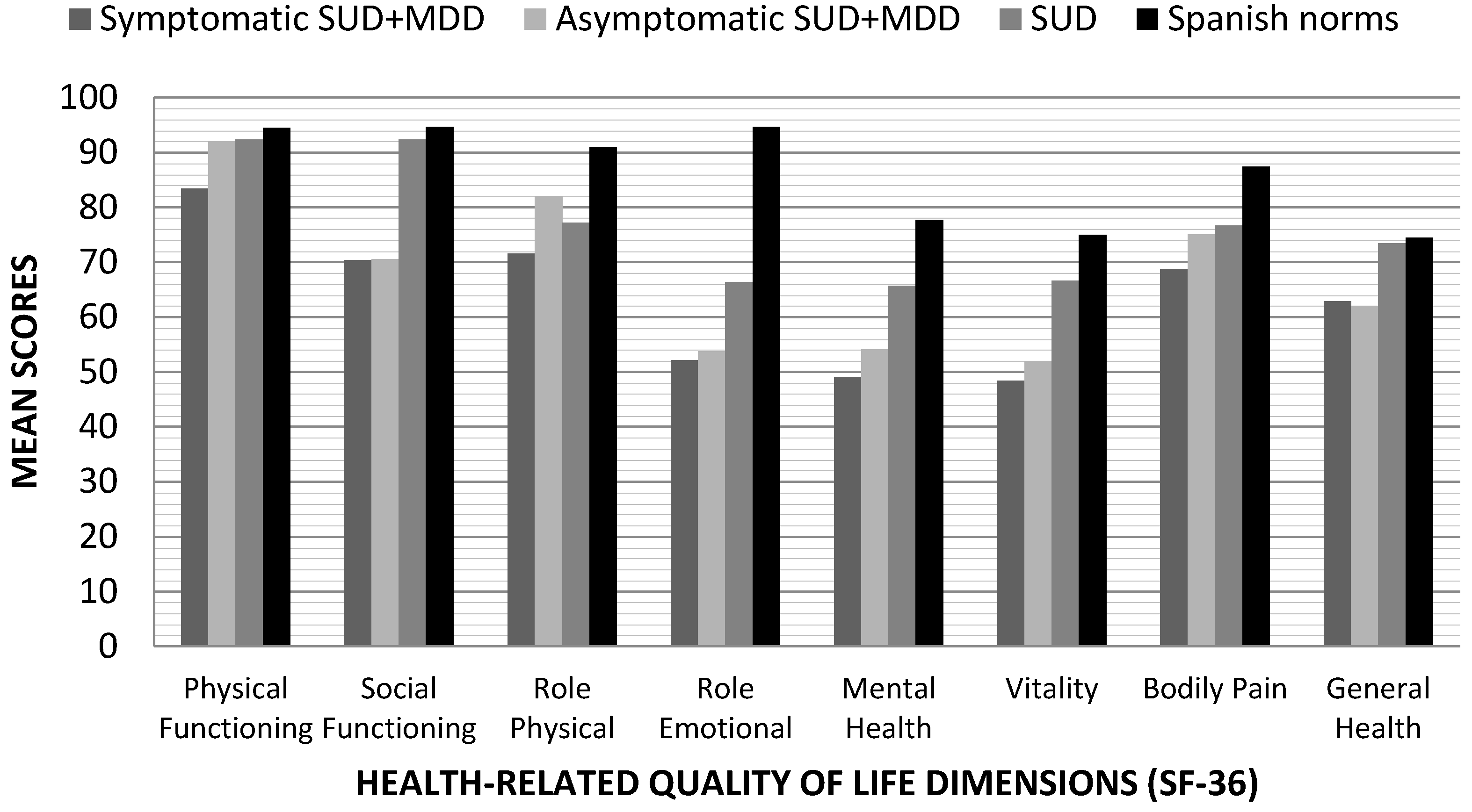
| SF-36 Dimensions | SUD + MDD Symptomatic (N = 51) | SUD + MDD Asymptomatic (N = 63) | SUD (N = 123) | F | ηp2 | Contrasts |
|---|---|---|---|---|---|---|
| Physical Functioning | 83.42 ± 1.98 | 92.02 ± 1.77 | 92.36 ± 1.30 | 7.230 *** | 0.059 | SUD and SUD + MDD asymptomatic > SUD + MDD symptomatic |
| Social Functioning | 70.41 ± 3.74 | 70.58 ± 3.35 | 78.65 ± 2.40 | 2.656 | 0.022 | |
| Role Physical | 71.60 ± 4.81 | 82.07 ± 4.31 | 77.20 ± 3.12 | 1.331 | 0.011 | |
| Role Emotional | 52.18 ± 5.55 | 53.78 ± 4.97 | 66.39 ± 3.57 | 3.246 | 0.027 | |
| Mental Health | 49.03 ± 2.36 | 54.90 ± 2.11 | 65.65 ± 1.53 | 19.662 *** | 0.145 | SUD > SUD + MDD symptomatic/asymptomatic |
| Vitality | 48.42 ± 2.57 | 51.91 ± 2.30 | 66.61 ± 1.66 | 22.800 *** | 0.165 | SUD > SUD + MDD symptomatic/asymptomatic |
| Bodily Pain | 68.63 ± 3.77 | 75.30 ± 3.37 | 76.68 ± 2.44 | 1.625 | 0.014 | |
| General Health | 62.86 ± 2.61 | 62.83 ± 2.34 | 73.42 ± 1.68 | 9.178 *** | 0.074 | SUD > SUD + MDD symptomatic/asymptomatic |
| Health Change item | 83.78 ± 3.25 | 72.49 ± 2.91 | 77.50 ± 2.21 | 12.547 *** | 0.098 | SUD and SUD + MDD asymptomatic > SUD + MDD symptomatic |
| Physical Composite Scale | 59.37 ± 2.30 | 60.84 ± 2.06 | 61.40 ± 1.48 | 0.26 | 0.002 | |
| Mental Composite Scale | 42.77 ± 2.43 | 42.67 ± 2.18 | 51.60 ± 1.57 | 7.449 *** | 0.176 | SUD > SUD + MDD symptomatic/asymptomatic |
| SF-36 Dimensions | Follow-Up Data Variables at 3 Months | SUD + MDD Symptomatic (N = 51) | SUD + MDD Asymptomatic (N = 63) | SUD (N = 123) |
|---|---|---|---|---|
| Role Emotional | Being at treatment | OR = 0.979 * | ||
| β = −0.022 | ||||
| Physical Functioning | Relapses | OR = 0.957 ** | ||
| β = −0.044 | ||||
| General Health | Relapses | OR = 1.028 * | ||
| β = 0.028 | ||||
| Vitality | Quantity of medical consultations | R2 = 0.261 *** | ||
| β = −0.527 | ||||
| Vitality | Need for medical assistance | OR = 0.949 * | ||
| β = −0.052 | ||||
| Follow-up Data Variables at 6 Months | SUD + MDD Symptomatic (N = 51) | SUD + MDD Asymptomatic (N = 63) | SUD (N = 123) | |
| Bodily Pain | Discharge from treatment | OR = 1.023 * | ||
| β = 0.022 | ||||
| Vitality | Being in treatment | OR = 1.046 * | ||
| β = 0.045 | ||||
| Physical Functioning | Relapses | OR = 0.965 * | ||
| β = −0.036 | ||||
| General Health | Quantity of medical consultations | R2 = 0.304 *** | ||
| β = −0.570 | ||||
| Vitality | Need for medical assistance | OR = 0.915 ** | ||
| β = −0.089 | ||||
| Follow-up Data Variables at 12 Months | SUD + MDD Symptomatic (N = 40) | SUD + MDD Asymptomatic (N = 45) | SUD (N = 87) | |
| Role Emotional | Discharge from treatment | OR = 1.014 * | ||
| β = 0.014 | ||||
| Vitality | Being in treatment | OR = 1.064 * | ||
| β = 0.062 | ||||
| Bodily Pain | Drop-out treatment | OR = 0.959 ** | ||
| β = −0.042 | ||||
| Physical Functioning | Relapses | OR = 0.958 * | ||
| β = −0.042 | ||||
| General Health | Relapses | OR = 1.035** | ||
| β = 0.035 | ||||
| General Health | Quantity of medical consultations | R2 = 0.262** | ||
| β = −0.535 |
| With 12-Months Follow-Up Baseline Data (N = 172) | Without 12-Months Follow-Up Baseline Data (N = 65) | Statistical Contrasts | |
|---|---|---|---|
| Sociodemographic Data | |||
| Age (years) | 39.55 ± 8.69 | 38.00 ± 8.74 | t(235) = 0.91 |
| Marital status | χ2(4) = 8.44 | ||
| Single | 57% | 56% | |
| Stable partner | 7.4% | 6.3% | |
| Married | 12.3% | 13.7% | |
| Separated/divorced | 21.8% | 24.0% | |
| Widower | 1.5% | 0% | |
| Years of schooling | 10.92 ± 2.59 | 11.13 ± 2.95 | t(235) = − 0.41 |
| Economic situation | χ2(4) = 6.69 | ||
| Active | 21.6% | 23.3% | |
| Unemployed | 25.0% | 27.0% | |
| Disability pension | 29.4% | 26.7% | |
| Sick leave (due SUD treatment) | 9.3% | 13.3 | |
| No income | 14.7% | 9.7% | |
| Medical and Psychiatric Data | |||
| Medical disease comorbidity a | 33.3% | 30.1% | χ2(6) = 6.18 |
| Hypercholesterolemia | 3.4% | 2.3% | |
| Respiratory system disease | 10.5% | 8.8% | |
| Hepatitis | 8.4% | 10.0% | |
| Diabetes | 2.9% | 1.9% | |
| Hypertension | 4.9% | 6.3% | |
| HIV | 4.9% | 6.7% | |
| Other | 11.3% | 14.2% | |
| Daily number of medications | 1.90 ± 1.84 | 1.21 ± 1.29 | t(235) = 10.97 *** |
| Type of medication prescribed a | |||
| Antidepressants | 43.7% | 39.3% | χ2(1) = 1.78 |
| Anxiolytics | 26.6% | 23.9% | χ2(1) =1.26 |
| Mood Stabilizers | 12.9% | 10.7% | χ2(1) = 5.66 |
| Disulfiram | 10.2% | 12.5% | χ2(1) = 0.99 |
| Other | 13.5% | 14.8% | χ2(1) = 1.69 |
| History of suicide attempt | 32.0% | 33.3% | χ2(1) =2.91 |
| Number of lifetime suicidal attempts | 0.68 ± 1.65 | 0.63 ± 1.00 | t(235) = 0.165 |
| SUD Related Data | |||
| Quantity of substance used a | 2.58 ± 1.55 | 2.90 ± 1.78 | t(235) = − 1.04 |
| Substance of use a | |||
| Alcohol | 80.3% | 83.7% | χ2(1) = 3.14 |
| Cocaine | 82.4% | 80% | χ2(1) = 5.98 |
| Cannabis | 40.1% | 43.3% | χ2(1) = 0.76 |
| Hallucinogens | 19.6% | 16.7% | χ2(1) = 0.14 |
| Opioids | 17.9% | 18.1% | χ2(1) = 0.41 |
| Sedatives | 5.6% | 8.3% | χ2(1) = 4.39 |
| DAST-20 | 13.59 ± 4.16 | 14.48 ± 3.43 | t(235) = 1.20 |
| Main substance of dependence | |||
| Alcohol | 10.3% | 8.7% | |
| Cocaine | 10.8% | 9.3% | |
| Alcohol and cocaine | 29.7% | 33.3% | |
| Alcohol and sedatives | 1.5% | 2.3% | |
| Polydrug use | 39.7% | 40.0% | |
| Mean abstinence period (months) | 8.67 ± 4.41 | 7.20 ± 4.03 | t(235) = 0.68 |
| Substance use disorder age onset (years) | 21.45 ± 9.02 | 18.53 ± 6.08 | t(235) = 1.71 |
| Years of substance use disorder | 17.34 ± 10.16 | 18.26 ± 9.93 | t(235) = − 0.47 |
| SUD + MDD with 12-Months Follow-Up Baseline Data (N = 85) | SUD + MDD without 12-Months Follow-Up Baseline Data (N = 29) | Statistical Contrasts | |
|---|---|---|---|
| Major depressive disorder age onset (years) | 29.77 ± 9.23 | 27.71 ± 7.99 | t = 0.86 |
| Years of major depressive disorder | 12.39 ±8.70 | 10.82 ± 9.59 | t = 0.69 |
| Hamilton Depression Rating Scale | 9.72 ± 5.80 | 10.50 ± 5.82 | t = − 0.47 |
| Social Adaption Self-evaluation Scale | 35.56 ± 7.19 | 36.30 ± 10.87 | t = − 0.286 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Marquez-Arrico, J.E.; Navarro, J.F.; Adan, A. Health-Related Quality of Life in Male Patients under Treatment for Substance Use Disorders with and without Major Depressive Disorder: Influence in Clinical Course at One-Year Follow-Up. J. Clin. Med. 2020, 9, 3110. https://doi.org/10.3390/jcm9103110
Marquez-Arrico JE, Navarro JF, Adan A. Health-Related Quality of Life in Male Patients under Treatment for Substance Use Disorders with and without Major Depressive Disorder: Influence in Clinical Course at One-Year Follow-Up. Journal of Clinical Medicine. 2020; 9(10):3110. https://doi.org/10.3390/jcm9103110
Chicago/Turabian StyleMarquez-Arrico, Julia E., José Francisco Navarro, and Ana Adan. 2020. "Health-Related Quality of Life in Male Patients under Treatment for Substance Use Disorders with and without Major Depressive Disorder: Influence in Clinical Course at One-Year Follow-Up" Journal of Clinical Medicine 9, no. 10: 3110. https://doi.org/10.3390/jcm9103110
APA StyleMarquez-Arrico, J. E., Navarro, J. F., & Adan, A. (2020). Health-Related Quality of Life in Male Patients under Treatment for Substance Use Disorders with and without Major Depressive Disorder: Influence in Clinical Course at One-Year Follow-Up. Journal of Clinical Medicine, 9(10), 3110. https://doi.org/10.3390/jcm9103110






