The Efficacy of Therapeutic Respiratory Muscle Training Interventions in People with Bronchiectasis: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Methods
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Quality Assessment and Data Extraction
2.4. Statistical Analysis
3. Results
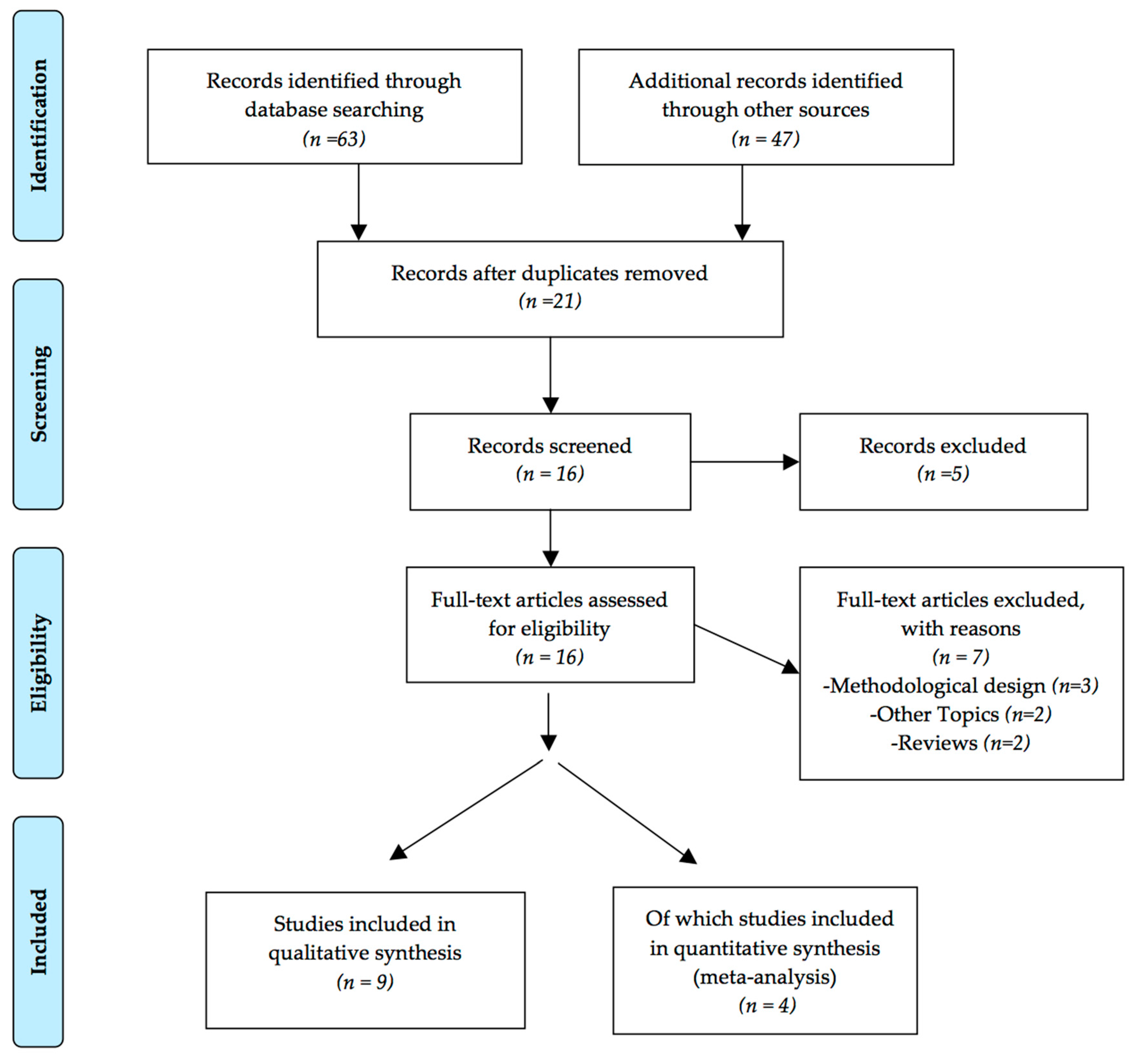
3.1. Study Selection and Methodological Quality Assessment
3.2. Study Design and Population Characteristics
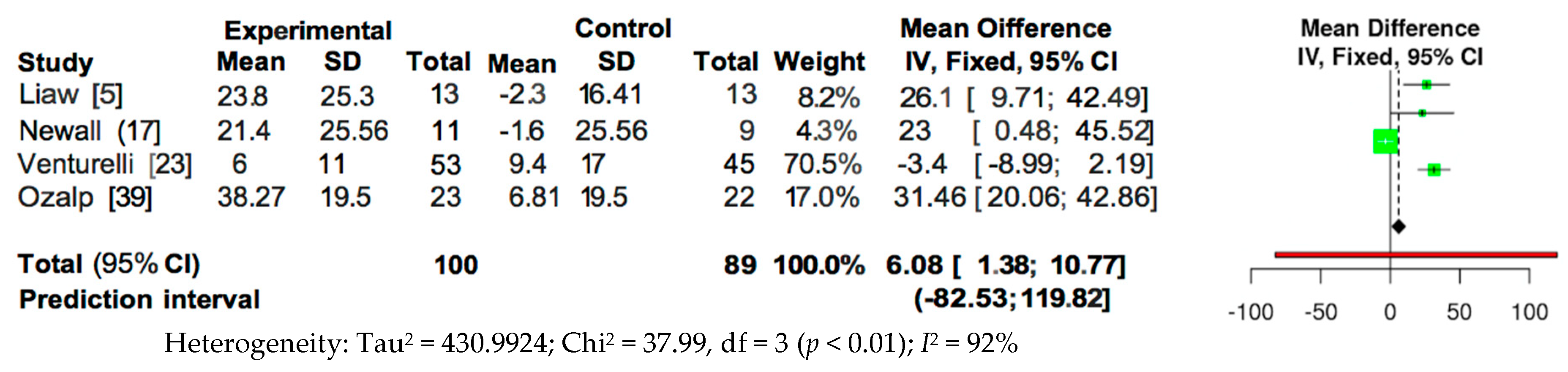
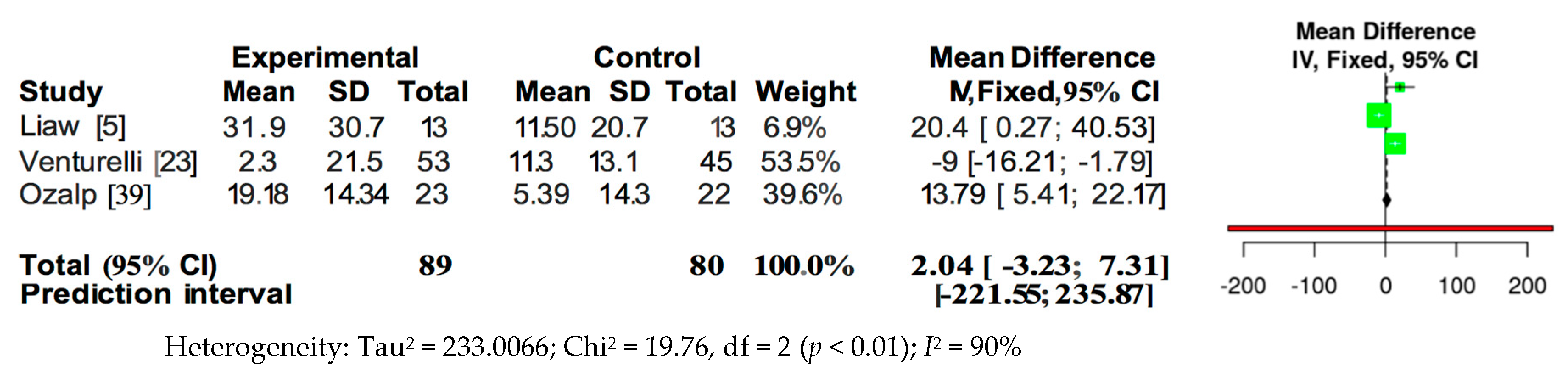
3.3. Meta-Analysis
4. Discussion
5. Limitations
6. Future Research
7. Clinical Implications
8. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
Abbreviations
| BMD | bone mineral density |
| CAM | contact angle measurement |
| CG | control group |
| DR | Degrees of Recommendation |
| EE | endurance exercise |
| FFM | Fat free mass |
| FFMI | Fat free mass index |
| FVC | forced vital capacity |
| FRC | functional residual capacity |
| FSS | Fatigue Severity Scale |
| I | intensity |
| IG | intervention group |
| ISWT | incremental shuttle walking test |
| LCQ | Leicester Cough Questionnaire |
| MBC | maximum breathing capacity |
| PEmax | maximal expiratory pressure |
| MIE | maximal inspiratory effort |
| min | minute |
| PImax | maximal inspiratory pressure |
| OC | outcome |
| OPEP | oscillating positive expiratory pressure |
| PEDro | Physiotherapy Evidence Database |
| PEP | positive expiratory pressure |
| PPS | patient preference scale |
| PRISMA | Preferred Reporting Items for Systematic Reviews and Meta-Analysis |
| PR | pulmonary rehabilitation |
| PR-control | pulmonary rehabilitation control group |
| PR-IMT | pulmonary rehabilitation inspiratory muscle training group |
| PR-sham | pulmonary rehabilitation sham group |
| QOL-B | quality of Life for BC |
| SGRQ | St George’s Respiratory Questionnaire |
| RV | residual volume |
| ss | session |
| SIP | sustainable inspiratory pressure |
| SV | sputum volume |
| TBS | The Borg Scale |
| TIMT | threshold inspiratory muscle trainer |
| TLC | Total Lung Capacity |
| TV | transport velocity |
| VRP1® | type of Flutter |
| 6MWD | 6 Minute-Walking Distance |
Appendix A. PRISMA 2009 Checklist
| Title | |||
| Title | 1 | Identify the report as a systematic review, meta-analysis, or both. | 1 |
| Abstract | |||
| Structured summary | 2 | Provide a structured summary including, as applicable: background; objectives; data sources; study eligibility criteria, participants, and interventions; study appraisal and synthesis methods; results; limitations; conclusions and implications of key findings; systematic review registration number. | Abstract page |
| Introduction | |||
| Rationale | 3 | Describe the rationale for the review in the context of what is already known. | 1–2 |
| Objectives | 4 | Provide an explicit statement of questions being addressed with reference to participants, interventions, comparisons, outcomes, and study design (PICOS). | 3 |
| Methods | |||
| Protocol and registration | 5 | Indicate if a review protocol exists, if and where it can be accessed (e.g., Web address), and, if available, provide registration information including registration number. | 3 |
| Eligibility criteria | 6 | Specify study characteristics (e.g., PICOS, length of follow-up) and report characteristics (e.g., years considered, language, publication status) used as criteria for eligibility, giving rationale. | 3–4 |
| Information sources | 7 | Describe all information sources (e.g., databases with dates of coverage, contact with study authors to identify additional studies) in the search and date last searched. | 3 |
| Search | 8 | Present full electronic search strategy for at least one database, including any limits used, such that it could be repeated. | Appendix B |
| Study selection | 9 | State the process for selecting studies (i.e., screening, eligibility, included in systematic review, and, if applicable, included in the meta-analysis). | 3–4 |
| Data collection process | 10 | Describe method of data extraction from reports (e.g., piloted forms, independently, in duplicate) and any processes for obtaining and confirming data from investigators. | 3 |
| Data items | 11 | List and define all variables for which data were sought (e.g., PICOS, funding sources) and any assumptions and simplifications made. | 4 |
| Risk of bias in individual studies | 12 | Describe methods used for assessing risk of bias of individual studies (including specification of whether this was done at the study or outcome level), and how this information is to be used in any data synthesis. | 5–11 |
| Summary measures | 13 | State the principal summary measures (e.g., risk ratio, difference in means). | 5–11 |
| Synthesis of results | 14 | Describe the methods of handling data and combining results of studies, if done, including measures of consistency (e.g., I2) for each meta-analysis. | 4 |
| Section/Topic | # | Checklist Item | Reported on Page # |
| Risk of bias across studies | 15 | Specify any assessment of risk of bias that may affect the cumulative evidence (e.g., publication bias, selective reporting within studies). | 4 |
| Additional analyses | 16 | Describe methods of additional analyses (e.g., sensitivity or subgroup analyses, meta-regression), if done, indicating which were pre-specified. | Not aplicable |
| Results | |||
| Study selection | 17 | Give numbers of studies screened, assessed for eligibility, and included in the review, with reasons for exclusions at each stage, ideally with a flow diagram. | Page 5, Figure 1 |
| Study characteristics | 18 | For each study, present characteristics for which data were extracted (e.g., study size, PICOS, follow-up period) and provide the citations. | Page 7–9, Table 2 |
| Risk of bias within studies | 19 | Present data on risk of bias of each study and, if available, any outcome level assessment (see item 12). | Table 1 |
| Results of individual studies | 20 | For all outcomes considered (benefits or harms), present, for each study: (a) simple summary data for each intervention group (b) effect estimates and confidence intervals, ideally with a forest plot. | Table 2 Figure 2 and Figure 3 |
| Synthesis of results | 21 | Present results of each meta-analysis done, including confidence intervals and measures of consistency. | Figure 2 and Figure 3 |
| Risk of bias across studies | 22 | Present results of any assessment of risk of bias across studies (see Item 15). | Not aplicable |
| Additional analysis | 23 | Give results of additional analyses, if done (e.g., sensitivity or subgroup analyses, meta-regression [see Item 16]). | Not aplicable |
| Discussion | |||
| Summary of evidence | 24 | Summarize the main findings including the strength of evidence for each main outcome; consider their relevance to key groups (e.g., healthcare providers, users, and policy makers). | 9–11 |
| Limitations | 25 | Discuss limitations at study and outcome level (e.g., risk of bias), and at review-level (e.g., incomplete retrieval of identified research, reporting bias). | 13 |
| Conclusions | 26 | Provide a general interpretation of the results in the context of other evidence, and implications for future research. | 14 |
| Funding | |||
| Funding | 27 | Describe sources of funding for the systematic review and other support (e.g., supply of data); role of funders for the systematic review. | 14 |
Appendix B. Detailed Search Strategy
((((((“respiratory muscle training” [Title/Abstract]) OR “respiratory muscle strength” [Title/Abstract]) OR “maximum inspiratory pressure” [Title/Abstract]) OR “maximum expiratory pressure”[Title/Abstract]) AND “bronchiectasis” [Title/Abstract] Filters: Clinical Trial; Randomized Controlled Trial.
- #1 AND #2AND #5 (1 potential article AND 1 RS)
- #2 AND #5(1 potential article AND the same RS)
- #3 AND #5 (1 potential article AND the same RS)
- #4 AND #5(1 potential article)
- #1 AND #2 AND #5 (1 potential articles)
- (#1 OR #2) AND #5(2 potential articles)
- (#3 OR #4) AND #5 (1 RS)
- #3 AND #4 AND #5 (2 potential articles)
- (#1 OR #2 OR #3) AND #5 (2 potential articles)
- (#1 OR #2 OR #4) AND #5 (2 potential articles)
- (#1 OR #3 OR #4) AND #5 (1 potential article AND 1 RS)
- (#2 OR #3 OR #4) AND #5 (1 potential article)
- #1 AND #5 (10 potential article)
- #5 AND (#1 OR #2) (30 potential articles)
- #3 AND #4 AND #5 (1 potential article)
- #3 AND #5 (1 potential article)
- #4 AND #5 (1 potential article)
References
- Vendrell, M.; De Gracia, J.; Olveira, C.; Martínez, M.Á.; Girón, R.; Máiz, L.; Cantón, R.; Coll, R.; Escribano, A.; Solé, A. Diagnosis and treatment of bronchiectasis. Arch. Bronconeumol. 2008, 44, 629–640. [Google Scholar] [CrossRef] [PubMed]
- Pasteur, M.C.; Bilton, D.; Hill, A.T. British Thoracic Society guideline for non-CF bronchiectasis. Thorax 2010, 65 (Suppl. 1), i1–i58. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Olveira, G.; Olveira, C.; Dorado, A.; Garcia-Fuentes, E.; Rubio, E.; Tinahones, F.; Soriguer, F.; Murri, M. Cellular and plasma oxidative stress biomarkers are raised in adults with bronchiectasis. Clin. Nutr. 2013, 32, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Olveira, G.; Olveira, C.; Gaspar, I.; Porras, N.; Martín-Núñez, G.; Rubio, E.; Colomo, N.; Rojo-Martínez, G.; Soriguer, F. Fat-free mass depletion and inflammation in patients with bronchiectasis. J. Acad. Nutr. Diet. 2012, 112, 1999–2006. [Google Scholar] [CrossRef] [PubMed]
- Liaw, M.Y.; Wang, Y.H.; Tsai, Y.C.; Huang, K.T.; Chang, P.W.; Chen, Y.C.; Lin, M.C. Inspiratory muscle training in bronchiectasis patients: A prospective randomized controlled study. Clin. Rehabil. 2011, 25, 524–536. [Google Scholar] [CrossRef] [PubMed]
- Lima Afonso, J.; Tambascio, J.; Dutra de Souza, H.C.; Jardim, J.R.; Baddini Martinez, J.A.; Gastaldi, A.C. Transport of mucoid mucus in healthy individuals and patients with chronic obstructive pulmonary disease and bronchiectasis. Rev. Port. Pneumol. 2013, 19, 211–216. [Google Scholar] [CrossRef] [Green Version]
- King, P.T.; Holdsworth, S.R.; Freezer, N.J.; Villanueva, E.; Holmes, P.W. Characterisation of the onset and presenting clinical features of adult bronchiectasis. Respir. Med. 2006, 100, 2183–2189. [Google Scholar] [CrossRef] [Green Version]
- Kelly, C.; Grundy, S.; Lynes, D.; Evans, D.J.; Gudur, S.; Milan, S.J.; Spencer, S. Self-management for bronchiectasis. Cochrane Database Syst. Rev. 2018, 2, CD012528. [Google Scholar] [CrossRef] [Green Version]
- Martínez-Garcia, M.A.; de la Rosa, D.; Cantón, R.; Olveira, C.; Máiz-Carro, L.; Girón, R.; Prados, C.; Blanco, M. Bronchiectasis: When the Published Scientific Evidence Proves Insufficient. Arch. Bronconeumol. 2019, 55, 283–285. [Google Scholar] [CrossRef]
- Vogiatzis, I.; Rochester, C.L.; Spruit, M.A.; Troosters, T.; Clini, E.M. Increasing implementation and delivery of pulmonary rehabilitation: Key messages from the new ATS/ERS policy statement. Eur. Respir. J. 2016, 47, 1336–1341. [Google Scholar] [CrossRef] [Green Version]
- Naraparaju, S.; Vaishali, K.; Venkatesan, P.; Acharya, V. A comparison of the Acapella and a threshold inspiratory muscle trainer for sputum clearance in bronchiectasis-A pilot study. Physiother. Theory Pract. 2010, 26, 353–357. [Google Scholar] [CrossRef] [PubMed]
- Murray, M.P.; Pentland, J.L.; Hill, A.T. A randomised crossover trial of chest physiotherapy in non-cystic fibrosis bronchiectasis. Eur. Respir. J. Off. J. Eur. Soc. Clin. Respir. Physiol. 2009, 34, 1086–1092. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.L.; Burge, A.; Holland, A.E. Airway clearance techniques for bronchiectasis. Cochrane Database Syst. Rev. 2013, 5, CD008351. [Google Scholar]
- Illi, S.K.; Held, U.; Frank, I.; Spengler, C.M. Effect of respiratory muscle training on exercise performance in healthy individuals: A systematic review and meta-analysis. Sports Med. 2012, 42, 707–724. [Google Scholar] [CrossRef]
- Bott, J.; Blumenthal, S.; Buxton, M.; Ellum, S.; Falconer, C.; Garrod, R.; Harvey, A.; Hughes, T.; Lincoln, M.; Mikelsons, C.; et al. Guidelines for the physiotherapy management of the adult, medical, spontaneously breathing patient. Thorax 2009, 64 (Suppl. 1), i1–i51. [Google Scholar] [CrossRef] [Green Version]
- Martín-Valero, R.; Rodríguez-Martínez, M.C.; Cantero-Tellez, R.; Villanueva-Calvero, E.; Fernández-Martinez, F. Advances in Comprehensive Pulmonary Rehabilitation for COPD Patients. COPD Clin. Perspect. 2014. [Google Scholar] [CrossRef] [Green Version]
- Newall, C.; Stockley, R.A.; Hill, S.L. Exercise training and inspiratory muscle training in patients with bronchiectasis. Thorax 2005, 60, 943–948. [Google Scholar] [CrossRef] [Green Version]
- Goldstein, R.S. Editorial to Exercise training and inspiratory muscle training in patients with bronchiectasis. Thorax 2005, 60, 889–890. [Google Scholar] [CrossRef] [Green Version]
- Lee, A.L.; Cecins, N.; Hill, C.J.; Holland, A.E.; Rautela, L.; Stirling, R.G.; Thompson, P.J.; McDonald, C.F.; Jenkins, S. The effects of pulmonary rehabilitation in patients with non-cystic fibrosis bronchiectasis: Protocol for a randomised controlled trial. BMC Pulm. Med. 2010, 10, 5. [Google Scholar] [CrossRef] [Green Version]
- Mandal, P.; Sidhu, M.K.; Kope, L.; Pollock, W.; Stevenson, L.M.; Pentland, J.L.; Turnbull, K.; Mac Quarrie, S.; Hill, A.T. A pilot study of pulmonary rehabilitation and chest physiotherapy versus chest physiotherapy alone in bronchiectasis. Respir. Med. 2012, 106, 1647–1654. [Google Scholar] [CrossRef] [Green Version]
- Olveira, G.; Olveira, C.; Doña, E.; Palenque, F.J.; Porras, N.; Dorado, A.; Godoy, A.M.; Rubio-Martínez, E.; Rojo-Martínez, G.; Martín-Valero, R. Oral supplement enriched in HMB combined with pulmonary rehabilitation improves body composition and health related quality of life in patients with bronchiectasis (Prospective, Randomised Study). Clin. Nutr. 2016, 35, 1015–1022. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Venturelli, E.; Crisafulli, E.; DeBiase, A.; Righi, D.; Berrighi, D.; Cavicchioli, P.P.; Vagheggini, G.; Dabrosca, F.; Balbi, B.; Paneroni, M.; et al. Efficacy of temporary positive expiratory pressure (TPEP) in patients with lung diseases and chronic mucus hypersecretion. The UNIKO(R) project: A multicentre randomized controlled trial. Clin. Rehabil. 2013, 27, 336–346. [Google Scholar] [PubMed]
- Patterson, J.E.; Bradley, J.M.; Hewitt, O.; Bradbury, I.; Elborn, J.S. Airway clearance in bronchiectasis: A randomized crossover trial of active cycle of breathing techniques versus Acapella. Respiration 2005, 72, 239–242. [Google Scholar] [CrossRef] [PubMed]
- Patterson, J.E.; Hewitt, O.; Kent, L.; Bradbury, I.; Elborn, J.S.; Bradley, J.M. Acapella versus ‘usual airway clearance’ during acute exacerbation in bronchiectasis: A randomized crossover trial. Chron. Respir. Dis. 2007, 4, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Polverino, E.; Herrero, B.; Romeu, D.M.; Vilarό, J. Efficacy of airway clearance therapy with different autonomy degrees in nonCF-BE: Randomized cross-over trial. Eur. Respir. J. 2011, 38, 2977. [Google Scholar]
- Guimaraes, F.S.; Moco, V.J.; Menezes, S.L.; Dias, C.M.; Salles, R.E.; Lopes, A.J. Effects of ELTGOL and Flutter VRP1® on the dynamic and static pulmonary volumes and on the secretion clearance of patients with bronchiectasis. Rev. Bras. Fisioter. 2012, 16, 108–113. [Google Scholar]
- Kapur, N.; Masters, I.B.; Morris, P.S.; Galligan, J.; Ware, R.; Chang, A.B. Defining pulmonary exacerbation in children with non-cystic fibrosis bronchiectasis. Pediatr. Pulmonol. 2012, 47, 68–75. [Google Scholar] [CrossRef]
- Verhagen, A.P.; de Vet, H.C.; de Bie, R.A.; Kessels, A.G.; Boers, M.; Bouter, L.M.; Knipschild, P.G. The Delphi list: A criteria list for quality assessment of randomized clinical trials for conducting systematic reviews developed by Delphi consensus. J. Clin. Epidemiol. 1998, 51, 1235–1241. [Google Scholar] [CrossRef] [Green Version]
- Foley, N.C.; Bhogal, S.K.; Teasell, R.W.; Bureau, Y.; Speechley, M.R. Estimates of quality and reliability with the physiotherapy evidence-based database scale to assess the methodology of randomized controlled trials of pharmacological and nonpharmacological interventions. Phys. Ther. 2006, 86, 817–824. [Google Scholar] [CrossRef]
- Maher, C.G.; Sherrington, C.; Herbert, R.D.; Moseley, A.M.; Elkins, M. Reliability of the PEDro scale for rating quality of randomized controlled trials. Phys. Ther. 2003, 83, 713–721. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Moseley, A.M.; Herbert, R.D.; Sherrington, C.; Maher, C.G. Evidence for physiotherapy practice: A survey of the Physiotherapy Evidence Database (PEDro). Aust. J. Physiother. 2002, 48, 43–49. [Google Scholar] [CrossRef] [Green Version]
- Figueiredo, P.H.; Zin, W.A.; Guimaraes, F.S. Flutter valve improves respiratory mechanics and sputum production in patients with bronchiectasis. Physiother. Res. Int. 2012, 17, 12–20. [Google Scholar] [CrossRef] [PubMed]
- Ramos, E.M.; Ramos, D.; Iyomasa, D.M.; Moreira, G.L.; Melegati, K.C.; Vanderlei, L.C.; Jardim, J.R.; Oliveira, A.S. Influence that oscillating positive expiratory pressure using predetermined expiratory pressures has on the viscosity and transportability of sputum in patients with bronchiectasis. J. Bras. Pneumol. 2009, 35, 1190–1197. [Google Scholar] [CrossRef] [Green Version]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Lawrence Erlbaum Associates: London, UK, 1988; ISBN 0805802835. [Google Scholar]
- Burgers, J.S.; Grol, R.; Klazinga, N.S.; Makela, M.; Zaat, J.; Collaboration, A. Towards evidence-based clinical practice: An international survey of 18 clinical guideline programs. Int. J. Qual. Health Care 2003, 15, 31–45. [Google Scholar] [CrossRef] [Green Version]
- Guerra, J.A.; Martín Muñoz, P.; Santos Lozano, J.M. Las Revisiones Sistemáticas, Niveles de Evidencia y Grados de Recomendación. Available online: http://www.fisterra.com/mbe/mbe_temas/19/revis_sist.asp (accessed on 1 June 2019).
- Tambascio, J.; de Souza, H.C.; Martinez, J.A.; Afonso, J.L.; Jardim, J.R.; Gastaldi, A.C. The influence of purulence on ciliary and cough transport in bronchiectasis. Respir. Care 2013, 58, 2101–2106. [Google Scholar] [CrossRef] [Green Version]
- Ozalp, O.; Inal-Ince, D.; Cakmak, A.; Calik-Kutukcu, E.; Saglam, M.; Savci, S.; Vardar-Yagli, N.; Arikan, H.; Karakaya, J.; Coplu, L. High-intensity inspiratory muscle training in bronchiectasis: A randomized controlled trial. Respirology 2019, 24, 246–253. [Google Scholar] [CrossRef]
- Tambascio, J.; De Souza, L.T.; Lisboa, R.M.; Passarelli, R.D.C.V.; De Souza, H.C.D.; Gastaldi, A.C. The influence of Flutter VRP1 components on mucus transport of patients with bronchiectasis. Respir. Med. 2011, 105, 1316–1321. [Google Scholar] [CrossRef]
- Martín-Valero, R.; Zamora-Pascual, N.; Armenta-Peinado, J.A. Training of Respiratory Muscles in Patients with Multiple Sclerosis: A Systematic Review. Respir. Care 2014, 59, 1764–1772. [Google Scholar] [CrossRef] [Green Version]
- Charususin, N.; Gosselink, R.; Decramer, M.; McConnell, A.; Saey, D.; Maltais, F.; Derom, E.; Vermeersch, S.; van Helvoort, H.; Heijdra, Y.; et al. Inspiratory muscle training protocol for patients with chronic obstructive pulmonary disease (IMTCO study): A multicentre randomised controlled trial. BMJ Open 2013, 3, e003101. [Google Scholar] [CrossRef] [Green Version]
| Section/Theme | Ozalp [39] | Venture Lli [23] | Liaw [5] | Newall [17] | Olveira [21] | Tambascio [40] | Figueiredo [33] | Mandal [20] | Murray [12] |
|---|---|---|---|---|---|---|---|---|---|
| Eligibility criteria | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Randomly allocated | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Concealed allocation | No | Yes | Yes | Yes | Yes | Yes | Yes | No | No |
| Comparability of base | Yes | Yes | Yes | Yes | Yes | Yes | No | Yes | No |
| Blinding of subjects | Yes | Yes | No | No | No | No | No | No | No |
| Blinding of therapist | No | No | Yes | No | No | No | Yes | No | No |
| Blinding of assessor | Yes | No | Yes | No | No | No | No | No | No |
| Proper Continuation | Yes | Yes | No | Yes | Yes | No | No | Yes | Yes |
| Intention to treat | Yes | Yes | Yes | Yes | Yes | Yes | Yes | No | No |
| Between-group statistical comparison | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Point measure and measures of variability | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes | Yes |
| Total | 8 | 8 | 8 | 7 | 7 | 6 | 6 | 5 | 4 |
| Study, DR | PEDro, Type of Study, Sample Size | Training Protocol | Intra-Group Outcomes | Effect Size (%) Clinical OC Measures | Effect Size (%) Self-Reported OC Measures |
|---|---|---|---|---|---|
| Venturelli, 2013 [23] A | PEDro: 8/10 Randomised controlled trial n = 98 | 10 days twice a day 20-min cycles of manually assisted breathing techniques plus 15 min of temporary PEP | PImax p = 0.541 PEmax p = 0.233 FVC p = 0.495 | PImax + 6% pred PEmax + 2.3% pred FVC + 4.3% pred | |
| Liaw, 2011 [5] A | PEDro: 8/10 Randomised controlled trial n = 26 | 8 week 5 days/week 30 min/day I: 30% MIP increasing 2 cm H2O/week | ↑PImax p = 0.004 ↑PEmax p = 0.004 ↑6MWD p = 0.021 FVC p = 0.309 | PImax + 23.85 cm H2O PEmax + 31.92 cm H2O 6MWD + 61.31 m FVC + 2.51% pred | TBS 1.46 SGRQ 32.46 |
| Ozalp, 2019 [39] A | PEDro: 8/10 Randomised controlled trial n = 45 | 8 week 3 days/week Only 1 ss/week was performed under the supervision I: target workload was selected from 30% (first session) to 70% (third session) of MIP | ↑PImax p = 0.001 ↑PEmax p = 0.233 SIP p < 0.05 ISWT distance | PImax + 2.62 cm H2O PEmax + 1.039 cm H2O | ↓FSS −0.197 p = 0.05 ↑LCQ 0.52 p = 0.05 |
| Newall, 2005 [17] A | PEDro: 7/10 Randomised controlled trial n = 32 | 8 week 3 days/week 2 sets/day 15 min/set I: 30% MIP and increased 5% each week until a training I of 60% MIP | ↑PImax p = 0.003 Vo2 peak p = 0.192 | PImax (cm H2O): PR-sham 12, PR-IMT 21.4; PR-control − 1.6 Vo2 peak(ml/min/kg): PR-sham 1.96; PR-IMT 0.35; PR-control − 1.91 ISWT (m): PR-sham 96.7; PR-IMT 124.5 PR-control 11 EE (m): PR-sham 392.8 PR-IMT 607.3; PR-control − 112.6 | |
| Murray, 2009 [12] A | PEDro: 4/10 Randomised crossover trial n = 20 | 3 months of twice daily, each ss 20–30 min, 3 sets, 10 breath/set | PImax p = 0.2 PEmax p = 0.3 FVC p = 0.6 | PImax +4.5 cm H2O PEmax − 1.5 cm H2O FVC + 0.18 L | ↓ SGRQ 0.7 p = 0.004 |
| Mandal, 2012 [20] C | PEDro: 5/10 RCT n = 30 | 8 weeks, 3sets/ss, 20–30 min/ss Twice a day CG: chest physiotherapy IG: chest physiotherapy plus PR | CG: PImax + 5.9 cm H2O PEmax + 5.3 cm H2O ISWT − 4.6 m IG: PImax + 6.6 cm H2O PEmax + 14.7 cm H2O ISWT + 56.7 m | CG: SGRQ 1.4 IG: ↓ SGRQ 4 p < 0.001 | |
| Tambascio, 2011 [40] B | PEDro: 6/10 RCT crossover n = 18 | 4 weeks with Flutter VRP1® 30 min daily and 1 weeek of a “wash-out” period vs. Flutter therapy | Flutter Therapy ↓CAM: 6.11 ± 0.5° p > 0.05 | ||
| Figueiredo, 2012 [33] B | PEDro: 6/10 RCT crossover n = 8 | Flutter Valve TM vs Sham Flutter (placebo) | 8.4 mL more secretions | ||
| Olveira, 2015 [21] B | PEDro: 7/10 RCT parallel groups n = 30 | 12 weeks PR 45 min +15 min with Orygen-Dual Valve® 3 days/week (one unsupervised ss) | BMD: 0.013 ± 0.002 FFM: 1.1 ± 0.1 p > 0.01 ↑FFMI:0.4 p > 0.01 Maximal Handgrip: 2.2 p > 0.01 | QOL-B: 8.1 ± 4.6 p > 0.05 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martín-Valero, R.; Jimenez-Cebrian, A.M.; Moral-Munoz, J.A.; de-la-Casa-Almeida, M.; Rodriguez-Huguet, M.; Casuso-Holgado, M.J. The Efficacy of Therapeutic Respiratory Muscle Training Interventions in People with Bronchiectasis: A Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 231. https://doi.org/10.3390/jcm9010231
Martín-Valero R, Jimenez-Cebrian AM, Moral-Munoz JA, de-la-Casa-Almeida M, Rodriguez-Huguet M, Casuso-Holgado MJ. The Efficacy of Therapeutic Respiratory Muscle Training Interventions in People with Bronchiectasis: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2020; 9(1):231. https://doi.org/10.3390/jcm9010231
Chicago/Turabian StyleMartín-Valero, Rocio, Ana Maria Jimenez-Cebrian, Jose A Moral-Munoz, Maria de-la-Casa-Almeida, Manuel Rodriguez-Huguet, and Maria Jesus Casuso-Holgado. 2020. "The Efficacy of Therapeutic Respiratory Muscle Training Interventions in People with Bronchiectasis: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 9, no. 1: 231. https://doi.org/10.3390/jcm9010231
APA StyleMartín-Valero, R., Jimenez-Cebrian, A. M., Moral-Munoz, J. A., de-la-Casa-Almeida, M., Rodriguez-Huguet, M., & Casuso-Holgado, M. J. (2020). The Efficacy of Therapeutic Respiratory Muscle Training Interventions in People with Bronchiectasis: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 9(1), 231. https://doi.org/10.3390/jcm9010231








