Circulating Biomarkers of Cell Adhesion Predict Clinical Outcome in Patients with Chronic Heart Failure
Abstract
1. Introduction
2. Methods
2.1. Patient Selection
2.2. Study Procedures
2.3. Study Endpoints
2.4. Blood Sample Selection
2.5. Biomarker Measurements
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics and Study Endpoints
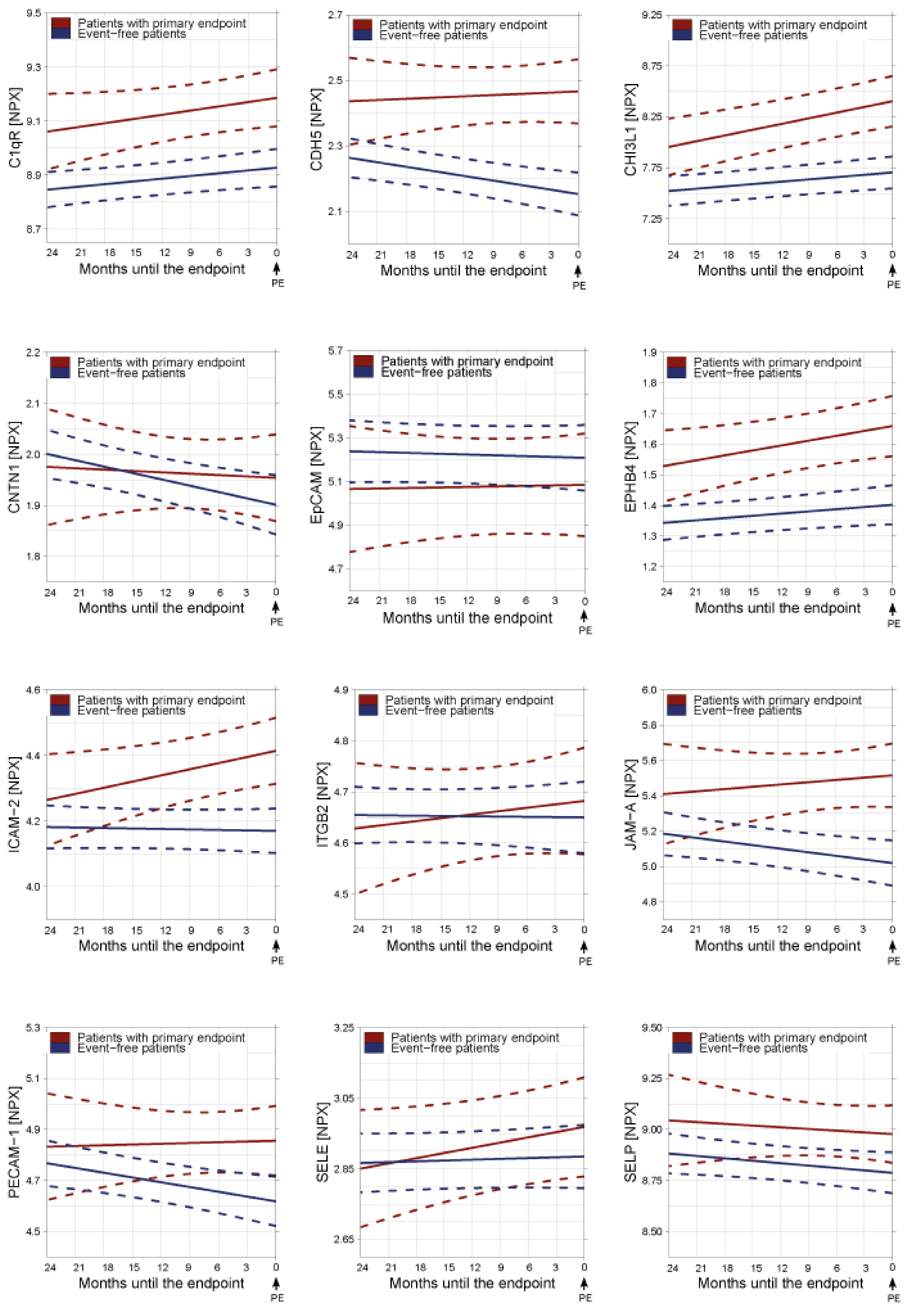
3.2. Temporal Patterns of Circulating Biomarkers of Cell Adhesion in Relation to Study Endpoints
4. Discussion
Author Contributions
Funding
Conflicts of Interest
Appendix A
| Abbreviation | Full Name | Synonyms | Function |
|---|---|---|---|
| C1qR | Complement component C1q receptor | CD93 | Stimulates endothelial expression of adhesion molecules/C1q-mediated endothelial cell adhesion |
| CDH5 | Cadherin 5 | VE cadherin | Major cell–cell adhesion molecule that forms adherens junctions |
| CHI3L1 | Chitinase-3-like protein 1 | YKL-40, HC gp39, brp-39, gp38k, and MGP-40 | Endothelial activation and dysfunction |
| CNTN1 | Contactin-1 | GP130 | Expressed in neuronal tissues, associates with other cell surface proteins and believed to participate in signal transduction pathways and cell functions |
| Ep-CAM | Epithelial cell adhesion molecule | CD326 | Cell–cell adhesion molecule and part of diverse processes such as signaling, cell migration, proliferation, and differentiation |
| EPHB4 | Ephrin type-B receptor 4 | HTK and Tyro11 | Essential role in vascular development |
| ICAM-2 | Intercellular adhesion molecule-2 | CD102 | Adherence and transmigration of leucocytes |
| ITGB2 | Integrin beta-2 | CD18 | Ligands for ICAM-1, and critical for the migration of leucocytes to sites of inflammation |
| JAM-A | Junctional adhesion molecule A | F11R | Involved in the migration of leukocytes through the endothelial cell barrier |
| PECAM-1 | Platelet endothelial cell adhesion molecule 1 | CD31 | Platelet/endothelial interaction, adherence and transmigration of leucocytes |
| SELE | E-selectin | CD62E, ELAM-1, and LECAM2 | Leucocyte rolling |
| SELP | P-selectin | CD154 | Platelet/endothelial interaction and leucocyte rolling |
References
- Doehner, W.; Frenneaux, M.; Anker, S.D. Metabolic impairment in heart failure: The myocardial and systemic perspective. J. Am. Coll. Cardiol. 2014, 64, 1388–1400. [Google Scholar] [CrossRef] [PubMed]
- Yndestad, A.; Damas, J.K.; Oie, E.; Ueland, T.; Gullestad, L.; Aukrust, P. Systemic inflammation in heart failure--the whys and wherefores. Heart Fail. Rev. 2006, 11, 83–92. [Google Scholar] [CrossRef] [PubMed]
- Chong, A.Y.; Blann, A.D.; Lip, G.Y.H. Assessment of endothelial damage and dysfunction: Observations in relation to heart failure. QJM Int. J. Med. 2003, 96, 253–267. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Bauersachs, J.; Langer, H.F. Immune mechanisms in heart failure. Eur. J. Heart Fail. 2017, 19, 1379–1389. [Google Scholar] [CrossRef]
- Yin, W.H.; Chen, J.W.; Young, M.S.; Lin, S.J. Increased endothelial monocyte adhesiveness is related to clinical outcomes in chronic heart failure. Int. J. Cardiol. 2007, 121, 276–283. [Google Scholar] [CrossRef]
- Wilhelmi, M.H.; Leyh, R.G.; Wilhelmi, M.; Haverich, A. Upregulation of endothelial adhesion molecules in hearts with congestive and ischemic cardiomyopathy: Immunohistochemical evaluation of inflammatory endothelial cell activation. Eur. J. Cardiothorac. Surg. 2005, 27, 122–127. [Google Scholar] [CrossRef]
- Juliano, R.L. Signal transduction by cell adhesion receptors and the cytoskeleton: Functions of integrins, cadherins, selectins, and immunoglobulin-superfamily members. Annu. Rev. Pharmacol. Toxicol. 2002, 42, 283–323. [Google Scholar] [CrossRef]
- Anker, S.D.; von Haehling, S. Inflammatory mediators in chronic heart failure: An overview. Heart 2004, 90, 464–470. [Google Scholar] [CrossRef]
- Breviario, F.; Caveda, L.; Corada, M.; Martin-Padura, I.; Navarro, P.; Golay, J.; Introna, M.; Gulino, D.; Lampugnani, M.G.; Dejana, E. Functional properties of human vascular endothelial cadherin (7B4/cadherin-5), an endothelium-specific cadherin. Arterioscler. Thromb. Vasc. Biol. 1995, 15, 1229–1239. [Google Scholar] [CrossRef]
- Granger, D.N.; Senchenkova, E. Inflammation and the Microcirculation. San Rafael (CA): Morgan & Claypool Life Sciences, 2010. Chapter 7, Leukocyte–Endothelial Cell Adhesion. Available online: https://www.ncbi.nlm.nih.gov/books/NBK53380/ (accessed on 2 January 2020).
- Price, D.T.; Loscalzo, J. Cellular adhesion molecules and atherogenesis 1. Am. J. Med. 1999, 107, 85–97. [Google Scholar]
- McMurray, J.J.; Adamopoulos, S.; Anker, S.D.; Auricchio, A.; Bohm, M.; Dickstein, K.; Falk, V.; Filippatos, G.; Fonseca, C.; Gomez-Sanchez, M.A.; et al. ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012: The Task Force for the Diagnosis and Treatment of Acute and Chronic Heart Failure 2012 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2012, 33, 1787–1847. [Google Scholar] [PubMed]
- Paulus, W.J.; Tschope, C.; Sanderson, J.E.; Rusconi, C.; Flachskampf, F.A.; Rademakers, F.E.; Marino, P.; Smiseth, O.A.; De Keulenaer, G.; Leite-Moreira, A.F.; et al. How to diagnose diastolic heart failure: A consensus statement on the diagnosis of heart failure with normal left ventricular ejection fraction by the Heart Failure and Echocardiography Associations of the European Society of Cardiology. Eur. Heart J. 2007, 28, 2539–2550. [Google Scholar] [CrossRef] [PubMed]
- Van Boven, N.; Battes, L.C.; Akkerhuis, K.M.; Rizopoulos, D.; Caliskan, K.; Anroedh, S.S.; Yassi, W.; Manintveld, O.C.; Cornel, J.H.; Constantinescu, A.A.; et al. Toward personalized risk assessment in patients with chronic heart failure: Detailed temporal patterns of NT-proBNP, troponin T, and CRP in the Bio-SHiFT study. Am. Heart J. 2018, 196, 36–48. [Google Scholar] [CrossRef] [PubMed]
- Brankovic, M.; Akkerhuis, K.M.; van Boven, N.; Anroedh, S.; Constantinescu, A.; Caliskan, K.; Manintveld, O.; Cornel, J.H.; Baart, S.; Rizopoulos, D.; et al. Patient-specific evolution of renal function in chronic heart failure patients dynamically predicts clinical outcome in the Bio-SHiFT study. Kidney Int. 2018, 93, 952–960. [Google Scholar] [CrossRef]
- Solier, C.; Langen, H. Antibody-based proteomics and biomarker research—Current status and limitations. Proteomics 2014, 14, 774–783. [Google Scholar] [CrossRef]
- Rizopoulos, D. The R package JMbayes for fitting joint models for longitudinal and time-to-event data using MCMC. arXiv 2014, arXiv:14047625. Available online: http://CRANR-projectorg/package=nlme (accessed on 8 August 2018).
- Rizopoulos, D. Dynamic predictions and prospective accuracy in joint models for longitudinal and time-to-event data. Biometrics 2011, 67, 819–829. [Google Scholar] [CrossRef]
- Rizopoulos, D. Joint Models for Longitudinal and Time-to-Event Data: With Applications in R; Chapman and Hall/CRC: Boca Raton, FL, USA, 2012. [Google Scholar]
- Pinheiro, J.; Bates, D.; DebRoy, S.; Sarkar, D. R Core Team (2014) nlme: Linear and Nonlinear Mixed Effects Models. R Package Version 3.1-117. Available online: http://CRAN.R-project.org/package=nlme (accessed on 8 August 2018).
- Mathiasen, A.B.; Henningsen, K.M.; Harutyunyan, M.J.; Mygind, N.D.; Kastrup, J. YKL-40: A new biomarker in cardiovascular disease? Biomark. Med. 2010, 4, 591–600. [Google Scholar] [CrossRef]
- Harutyunyan, M.; Christiansen, M.; Johansen, J.S.; Kober, L.; Torp-Petersen, C.; Kastrup, J. The inflammatory biomarker YKL-40 as a new prognostic marker for all-cause mortality in patients with heart failure. Immunobiology 2012, 217, 652–656. [Google Scholar] [CrossRef]
- Bilim, O.; Takeishi, Y.; Kitahara, T.; Ishino, M.; Sasaki, T.; Suzuki, S.; Shishido, T.; Kubota, I. Serum YKL-40 predicts adverse clinical outcomes in patients with chronic heart failure. J. Card Fail. 2010, 16, 873–879. [Google Scholar] [CrossRef]
- Arain, F.; Gullestad, L.; Nymo, S.; Kjekshus, J.; Cleland, J.G.; Michelsen, A.; McMurray, J.J.; Wikstrand, J.; Aukrust, P.; Ueland, T. Low YKL-40 in chronic heart failure may predict beneficial effects of statins: Analysis from the controlled rosuvastatin multinational trial in heart failure (CORONA). Biomarkers 2017, 22, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Rathcke, C.N.; Kistorp, C.; Raymond, I.; Hildebrandt, P.; Gustafsson, F.; Lip, G.Y.; Faber, J.; Vestergaard, H. Plasma YKL-40 levels are elevated in patients with chronic heart failure. Scand. Cardiovasc. J. 2010, 44, 92–99. [Google Scholar] [CrossRef] [PubMed]
- Woodfin, A.; Voisin, M.B.; Imhof, B.A.; Dejana, E.; Engelhardt, B.; Nourshargh, S. Endothelial cell activation leads to neutrophil transmigration as supported by the sequential roles of ICAM-2, JAM-A, and PECAM-1. Blood 2009, 113, 6246–6257. [Google Scholar] [CrossRef] [PubMed]
- Reglero-Real, N.; Colom, B.; Bodkin, J.V.; Nourshargh, S. Endothelial Cell Junctional Adhesion Molecules: Role and Regulation of Expression in Inflammation. Arterioscler. Thromb. Vasc. Biol. 2016, 36, 2048–2057. [Google Scholar] [CrossRef]
- Vestweber, D. Adhesion and signaling molecules controlling the transmigration of leukocytes through endothelium. Immunol. Rev. 2007, 218, 178–196. [Google Scholar] [CrossRef]
- Yu, W.K.; McNeil, J.B.; Wickersham, N.E.; Shaver, C.M.; Bastarache, J.A.; Ware, L.B. Vascular endothelial cadherin shedding is more severe in sepsis patients with severe acute kidney injury. Crit Care. 2019, 23, 18. [Google Scholar] [CrossRef]
- Zhang, R.Y.; Liu, Y.Y.; Li, L.; Cui, W.; Zhao, K.J.; Huang, W.C.; Gu, X.W.; Liu, W.; Wu, J.; Min, D.; et al. Increased levels of soluble vascular endothelial cadherin are associated with poor outcome in severe sepsis. J. Int. Med. Res. 2010, 38, 1497–1506. [Google Scholar] [CrossRef]
- Soeki, T.; Tamura, Y.; Shinohara, H.; Sakabe, K.; Onose, Y.; Fukuda, N. Elevated concentration of soluble vascular endothelial cadherin is associated with coronary atherosclerosis. Circ. J. 2004, 68, 1–5. [Google Scholar] [CrossRef]
- Luissint, A.C.; Nusrat, A.; Parkos, C.A. JAM-related proteins in mucosal homeostasis and inflammation. Semin. Immunopathol. 2014, 36, 211–226. [Google Scholar] [CrossRef]
- Nourshargh, S.; Krombach, F.; Dejana, E. The role of JAM-A and PECAM-1 in modulating leukocyte infiltration in inflamed and ischemic tissues. J. Leukoc. Biol. 2006, 80, 714–718. [Google Scholar] [CrossRef]
- Curaj, A.; Wu, Z.; Rix, A.; Gresch, O.; Sternkopf, M.; Alampour-Rajabi, S.; Lammers, T.; van Zandvoort, M.; Weber, C.; Koenen, R.R.; et al. Molecular Ultrasound Imaging of Junctional Adhesion Molecule A Depicts Acute Alterations in Blood Flow and Early Endothelial Dysregulation. Arterioscler Thromb Vasc Biol. 2018, 38, 40–48. [Google Scholar] [CrossRef] [PubMed]
- Newman, P.J.; Newman, D.K. Signal transduction pathways mediated by PECAM-1: New roles for an old molecule in platelet and vascular cell biology. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 953–964. [Google Scholar] [CrossRef] [PubMed]
- Soeki, T.; Tamura, Y.; Shinohara, H.; Sakabe, K.; Onose, Y.; Fukuda, N. Increased soluble platelet/endothelial cell adhesion molecule-1 in the early stages of acute coronary syndromes. Int. J. Cardiol. 2003, 90, 261–268. [Google Scholar] [CrossRef]
- Serebruany, V.L.; Murugesan, S.R.; Pothula, A.; Atar, D.; Lowry, D.R.; O’Connor, C.M.; Gurbel, P.A. Increased soluble platelet/endothelial cellular adhesion molecule-1 and osteonectin levels in patients with severe congestive heart failure. Independence of disease etiology, and antecedent aspirin therapy. Eur. J. Heart Fail 1999, 1, 243–249. [Google Scholar] [CrossRef]
- Blann, A.D.; Nadar, S.K.; Lip, G.Y. The adhesion molecule P-selectin and cardiovascular disease. Eur. Heart J. 2003, 24, 2166–2179. [Google Scholar] [CrossRef] [PubMed]
- O’Connor, C.M.; Gurbel, P.A.; Serebruany, V.L. Usefulness of soluble and surface-bound P-selectin in detecting heightened platelet activity in patients with congestive heart failure. Am. J. Cardiol. 1999, 83, 1345–1349. [Google Scholar] [CrossRef]
- Stumpf, C.; Lehner, C.; Eskafi, S.; Raaz, D.; Yilmaz, A.; Ropers, S.; Schmeisser, A.; Ludwig, J.; Daniel, W.G.; Garlichs, C.D. Enhanced levels of CD154 (CD40 ligand) on platelets in patients with chronic heart failure. Eur. J. Heart Fail. 2003, 5, 629–637. [Google Scholar] [CrossRef]
- Gibbs, C.R.; Blann, A.D.; Watson, R.D.; Lip, G.Y. Abnormalities of hemorheological, endothelial, and platelet function in patients with chronic heart failure in sinus rhythm: Effects of angiotensin-converting enzyme inhibitor and beta-blocker therapy. Circulation 2001, 103, 1746–1751. [Google Scholar] [CrossRef]
- Chung, I.; Choudhury, A.; Patel, J.; Lip, G.Y. Soluble, platelet-bound, and total P-selectin as indices of platelet activation in congestive heart failure. Ann. Med. 2009, 41, 45–51. [Google Scholar] [CrossRef]
- Ghebrehiwet, B.; Feng, X.; Kumar, R.; Peerschke, E.I. Complement component C1q induces endothelial cell adhesion and spreading through a docking/signaling partnership of C1q receptors and integrins. Int. Immunopharmacol. 2003, 3, 299–310. [Google Scholar] [CrossRef]
- Guo, W.X.; Ghebrehiwet, B.; Weksler, B.; Schweitzer, K.; Peerschke, E.I. Up-regulation of endothelial cell binding proteins/receptors for complement component C1q by inflammatory cytokines. J. Lab. Clin. Med. 1999, 133, 541–550. [Google Scholar] [CrossRef]
- Hamada, K.; Oike, Y.; Ito, Y.; Maekawa, H.; Miyata, K.; Shimomura, T.; Suda, T. Distinct roles of ephrin-B2 forward and EphB4 reverse signaling in endothelial cells. Arterioscler. Thromb. Vasc. Biol. 2003, 23, 190–197. [Google Scholar] [CrossRef] [PubMed]
- Severino, P.; Mariani, M.V.; Fedele, F. Futility in cardiology: The need for a change in perspectives. Eur. J. Heart Fail. 2019, 21, 1483–1484. [Google Scholar] [CrossRef] [PubMed]
- Severino, P.; Maestrini, V.; Mariani, M.V.; Birtolo, L.I.; Scarpati, R.; Mancone, M.; Fedele, F. Structural and myocardial dysfunction in heart failure beyond ejection fraction. Heart Fail. Rev. 2019. [Google Scholar] [CrossRef]
- Severino, P.; Mather, P.J.; Pucci, M.; D’Amato, A.; Mariani, M.V.; Infusino, F.; Birtolo, L.I.; Maestrini, V.; Mancone, M.; Fedele, F. Advanced Heart Failure and End-Stage Heart Failure: Does a Difference Exist. Diagnostics 2019, 9, 170. [Google Scholar] [CrossRef]
- Severino, P.; D’Amato, A.; Netti, L.; Pucci, M.; Infusino, F.; Maestrini, V.; Mancone, M.; Fedele, F. Myocardial Ischemia and Diabetes Mellitus: Role of Oxidative Stress in the Connection between Cardiac Metabolism and Coronary Blood Flow. J. Diabetes Res. 2019, 2019, 9489826. [Google Scholar] [CrossRef]
- Fedele, F.; Severino, P.; Calcagno, S.; Mancone, M. Heart failure: TNM-like classification. J. Am. Coll. Cardiol. 2014, 63, 1959–1960. [Google Scholar] [CrossRef]
- Bouwens, E.; Brankovic, M.; Mouthaan, H.; Baart, S.; Rizopoulos, D.; van Boven, N.; Caliskan, K.; Manintveld, O.; Germans, T.; van Ramshorst, J.; et al. Temporal Patterns of 14 Blood Biomarker candidates of Cardiac Remodeling in Relation to Prognosis of Patients With Chronic Heart Failure-The Bio- SH i FT Study. J. Am. Heart Assoc. 2019, 8, e009555. [Google Scholar] [CrossRef]
| Variable | Total | PE Reached during Follow-Up | p-Value | |
|---|---|---|---|---|
| Yes | No | |||
| 263 (100) | 70 (27) | 193 (73) | ||
| Demographics | ||||
| Age—years | 68 (59–76) | 72 (60–80) | 67 (58–75) | 0.021 * |
| Men | 189 (72) | 53 (76) | 136 (71) | 0.40 |
| Clinical characteristics | ||||
| Body Mass Index (kg/m2) | 26 (24–30) | 27 (24–30) | 26 (24–30) | 0.80 |
| Heart rate (eats/min) | 67 ± 12 | 69 ± 13 | 67 ± 11 | 0.22 |
| Systolic blood pressure (mmHg) | 122 ± 20 | 117 ± 17 | 124 ± 21 | 0.020 * |
| Diastolic blood pressure (mmHg) | 72 ± 11 | 70 ± 10 | 73 ± 11 | 0.06 |
| Features of heart failure | ||||
| Duration of HF (years) | 4.6 (1.7–9.9) | 6.8 (2.8–12.5) | 3.8 (1.1–8.2) | 0.002 * |
| NYHA class III or IV | 69 (26) | 31 (44) | 38 (20) | <0.001 * |
| HF with reduced ejection fraction | 250 (95) | 66 (94) | 184 (95) | 0.75 |
| HF with preserved ejection fraction | 13 (5) | 4 (6) | 9 (5) | |
| Left ventricular ejection fraction | 31 ± 11 | 28 ± 11 | 31 ± 11 | 0.108 |
| Established biomarkers | ||||
| NT-proBNP (pmol/L) | 137 (52–273) | 282 (176–517) | 95 (32–208) | <0.001 * |
| HsTnT (ng/L) | 18 (10–33) | 32 (21–50) | 14 (8–27) | <0.001 * |
| eGFR (mL/min per 1.73m2) | 58 (43–76) | 53 (40–73) | 59 (44–77) | 0.20 |
| Etiology of heart failure | ||||
| Ischemic | 117 (45) | 36 (51) | 81 (42) | 0.17 |
| Hypertension | 34 (13) | 10 (14) | 24 (12) | 0.69 |
| Secondary to valvular disease | 12 (5) | 5 (7) | 7 (4) | 0.31 |
| Cardiomyopathy | 68 (26) | 15 (21) | 53 (28) | 0.32 |
| Unknown or Others | 32 (12) | 4 (6) | 28 (15) | |
| Medical history | ||||
| Prior Myocardial infarction | 96 (37) | 32 (46) | 64 (33) | 0.060 |
| Prior Percutaneous coronary intervention | 82 (31) | 27 (39) | 55 (29) | 0.12 |
| Prior Coronary artery bypass grafting | 43 (16) | 13 (19) | 30 (16) | 0.56 |
| Prior CVA/TIA | 42 (16) | 15 (21) | 27 (14) | 0.15 |
| Atrial fibrillation | 106 (40) | 36 (51) | 70 (36) | 0.027 * |
| Diabetes Mellitus | 81 (31) | 32 (46) | 49 (25) | 0.002 * |
| Hypercholesterolemia | 96 (37) | 30 (43) | 66 (34) | 0.20 |
| Hypertension | 120 (46) | 38 (54) | 82 (43) | 0.090 |
| COPD | 31 (12) | 12 (17) | 19 (10) | 0.11 |
| Medication use | ||||
| Beta-blocker | 236 (90) | 61 (87) | 175 (91) | 0.40 |
| ACE-I or ARB | 245 (93) | 63 (90) | 182 (94) | 0.22 |
| Diuretics | 237 (90) | 68 (97) | 169 (88) | 0.021 * |
| Loop diuretics | 236 (90) | 68 (97) | 168 (87) | 0.017 * |
| Thiazides | 7 (3) | 3 (4) | 4 (2) | 0.39 |
| Aldosterone antagonist | 179 (68) | 53 (76) | 126 (65) | 0.11 |
| Biomarker level at baseline in arbitrary unit (NPX values) | ||||
| C1qR | 8.88 (8.56–9.27) | 9.16 (8.78–9.50) | 8.78 (8.50–9.20) | <0.001 * |
| CDH5 | 2.29 (2.00–2.67) | 2.36 (2.12–2.84) | 2.27 (1.96–2.60) | 0.010 * |
| CHI3L1 | 7.68 (6.88–8.39) | 8.08 (7.53–8.72) | 7.47 (6.68–8.20) | <0.001 * |
| CNTN1 | 2.01 (1.72–2.25) | 2.00 (1.68–2.22) | 2.01 (1.75–2.27) | 0.58 |
| EpCAM | 5.11 (4.38–5.82) | 4.91 (4.40–5.71) | 5.18 (4.36–5.90) | 0.41 |
| EPHB4 | 1.35 (1.08–1.66) | 1.55 (1.19–1.95) | 1.31 (1.05–1.58) | <0.001 * |
| ICAM-2 | 4.20 (3.88–4.59) | 4.35 (4.00–4.64) | 4.18 (3.85–4.51) | 0.061 |
| ITGB2 | 4.65 (4.39–4.90) | 4.64 (4.41–4.96) | 4.67 (4.39–4.89) | 0.86 |
| JAM-A | 5.22 (4.64–5.80) | 5.41 (4.79–6.02) | 5.08 (4.56–5.71) | 0.024 * |
| PECAM-1 | 4.74 (4.36–5.17) | 4.77 (4.36–5.39) | 4.70 (4.35–5.10) | 0.32 |
| SELE | 2.89 (2.46–3.28) | 3.06 (2.51–3.32) | 2.84 (2.45–3.28) | 0.40 |
| SELP | 8.84 (8.46–9.38) | 8.98 (8.54–9.58) | 8.78 (8.42–9.28) | 0.087 |
| Crude Model | Clinical Model | Biomarker Model | ||||
|---|---|---|---|---|---|---|
| Biomarker | HR (95% CI) | p-Value | HR (95% CI) | p-Value | HR (95% CI) | p-Value |
| C1qR | 2.22 (1.62–3.10) | <0.001 * | 1.90 (1.36–2.72) | <0.001 * | 1.47 (1.04–2.14) | 0.028 |
| CDH5 | 2.01 (1.47–2.77) | <0.001 * | 1.79 (1.30–2.50) | <0.001 * | 1.56 (1.14–2.14) | 0.004 |
| CHI3L1 | 2.11 (1.60–2.84) | <0.001 * | 2.27 (1.66–3.16) | <0.001 * | 1.68 (1.23–2.35) | 0.002 * |
| CNTN1 | 0.93 (0.66–1.32) | 0.70 | 0.98 (0.67–1.45) | 0.92 | 0.93 (0.66–1.31) | 0.66 |
| EpCAM | 0.86 (0.66–1.11) | 0.27 | 0.90 (0.67–1.20) | 0.46 | 0.90 (0.69–1.17) | 0.46 |
| EPHB4 | 1.90 (1.48–2.44) | <0.001 * | 1.77 (1.35–2.33) | <0.001 * | 1.37 (1.03–1.80) | 0.031 |
| ICAM2 | 2.08 (1.51–2.94) | <0.001 * | 1.79 (1.29–2.53) | 0.001 * | 1.53 (1.12–2.12) | 0.005 |
| ITGB2 | 1.07 (0.77–1.47) | 0.70 | 0.95 (0.65–1.37) | 0.77 | 1.04 (0.75–1.42) | 0.83 |
| JAM-A | 1.86 (1.34–2.63) | <0.001 * | 2.10 (1.42–3.23) | <0.001 * | 1.75 (1.25–2.49) | 0.001 * |
| PECAM-1 | 1.39 (1.00–1.94) | 0.050 | 1.60 (1.10–2.35) | 0.013 | 1.47 (1.04–2.08) | 0.031 |
| SELE | 1.11 (0.86–1.44) | 0.43 | 1.07 (0.81–1.40) | 0,66 | 1.11 (0.86–1.44) | 0.43 |
| SELP | 1.34 (0.98–1.86) | 0.071 | 1.45 (1.01–2.10) | 0.044 | 1.49 (1.08–2.06) | 0.018 |
| Crude Model | Clinical Model | Biomarker Model | ||||
|---|---|---|---|---|---|---|
| Biomarker | HR (95% CI) | p-Value | HR (95% CI) | p-Value | HR (95% CI) | p-Value |
| C1qR | 1.34 (1.16–1.56) | <0.001 * | 1.43 (1.13–1.92) | 0.002 * | 1.12 (1.02–1.24) | 0.019 |
| CDH5 | 1.36 (1.18–1.60) | <0.001 * | 1.47 (1.17–2.00) | <0.001 * | 1.16 (1.07–1.27) | <0.001 * |
| CHI3L1 | 1.41 (1.29–1.57) | <0.001 * | 1.58 (1.36–1.93) | <0.001 * | 1.27 (1.18–1.39) | <0.001 * |
| CNTN1 | 1.04 (0.94–1.17) | 0.45 | 1.04 (0.92–1.18) | 0.53 | 1.06 (0.98–1.15) | 0.13 |
| EpCAM | 1.01 (0.88–1.16) | 0.92 | 1.01 (0.88–1.17) | 0.88 | 1.01 (0.92–1.11) | 0.83 |
| EPHB4 | 1.33 (1.19–1.51) | <0.001 * | 1.34 (1.15–1.68) | <0.001 * | 1.14 (1.04–1.25) | 0.005 |
| ICAM2 | 1.32 (1.22–1.45) | <0.001 * | 1.44 (1.27–1.72) | <0.001 * | 1.22 (1.15–1.31) | <0.001 * |
| ITGB2 | 1.07 (0.94–1.21) | 0.32 | 0.99 (0.83–1.16) | 0.90 | 1.05 (0.97–1.15) | 0.23 |
| JAM-A | 1.34 (1.12–1.62) | 0.002 * | 1.64 (1.23–2.24) | 0.001 * | 1.10 (0.99–1.24) | 0.085 |
| PECAM-1 | 1.15 (0.98–1.40) | 0.088 | 1.09 (0.86–1.72) | 0.80 | 1.06 (0.97–1.18) | 0.21 |
| SELE | 1.21 (1.05–1.41) | 0.015 | 1.19 (0.99–1.41) | 0.060 | 1.10 (0.96–1.23) | 0.15 |
| SELP | 1.29 (1.13–1.49) | 0.020 | 1.45 (1.22–1.84) | <0.001 * | 1.12 (0.94–1.27) | 0.15 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bouwens, E.; van den Berg, V.J.; Akkerhuis, K.M.; Baart, S.J.; Caliskan, K.; Brugts, J.J.; Mouthaan, H.; van Ramshorst, J.; Germans, T.; Umans, V.A.W.M.; et al. Circulating Biomarkers of Cell Adhesion Predict Clinical Outcome in Patients with Chronic Heart Failure. J. Clin. Med. 2020, 9, 195. https://doi.org/10.3390/jcm9010195
Bouwens E, van den Berg VJ, Akkerhuis KM, Baart SJ, Caliskan K, Brugts JJ, Mouthaan H, van Ramshorst J, Germans T, Umans VAWM, et al. Circulating Biomarkers of Cell Adhesion Predict Clinical Outcome in Patients with Chronic Heart Failure. Journal of Clinical Medicine. 2020; 9(1):195. https://doi.org/10.3390/jcm9010195
Chicago/Turabian StyleBouwens, Elke, Victor J. van den Berg, K. Martijn Akkerhuis, Sara J. Baart, Kadir Caliskan, Jasper J. Brugts, Henk Mouthaan, Jan van Ramshorst, Tjeerd Germans, Victor A. W. M. Umans, and et al. 2020. "Circulating Biomarkers of Cell Adhesion Predict Clinical Outcome in Patients with Chronic Heart Failure" Journal of Clinical Medicine 9, no. 1: 195. https://doi.org/10.3390/jcm9010195
APA StyleBouwens, E., van den Berg, V. J., Akkerhuis, K. M., Baart, S. J., Caliskan, K., Brugts, J. J., Mouthaan, H., van Ramshorst, J., Germans, T., Umans, V. A. W. M., Boersma, E., & Kardys, I. (2020). Circulating Biomarkers of Cell Adhesion Predict Clinical Outcome in Patients with Chronic Heart Failure. Journal of Clinical Medicine, 9(1), 195. https://doi.org/10.3390/jcm9010195





