Left Ventricular Function and Myocardial Triglyceride Content on 3T Cardiac MR Predict Major Cardiovascular Adverse Events and Readmission in Patients Hospitalized with Acute Heart Failure
Abstract
1. Introduction
2. Methods
2.1. Ethics Approval and Consent to Participate
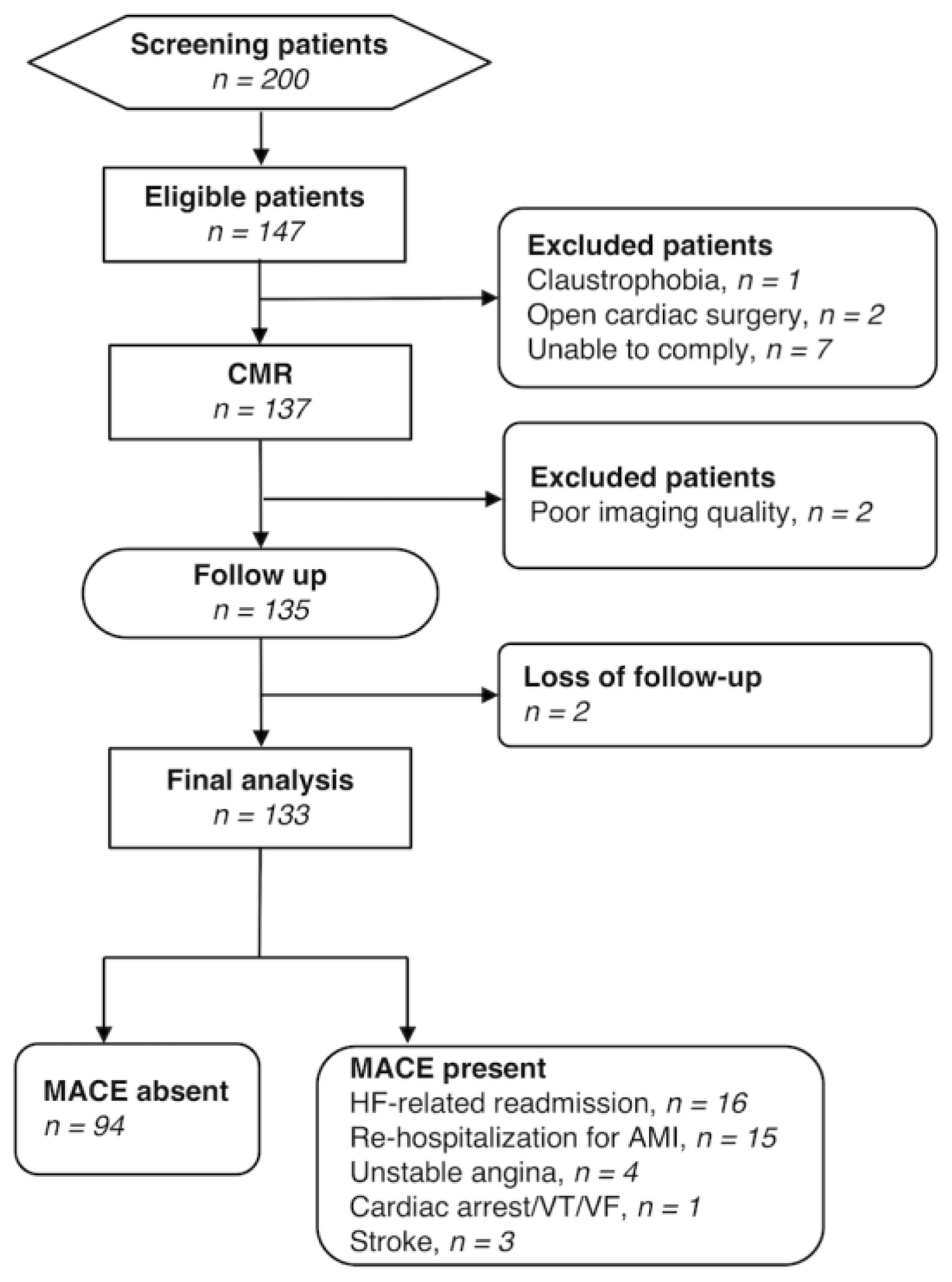
2.2. Study Design and Patient Population
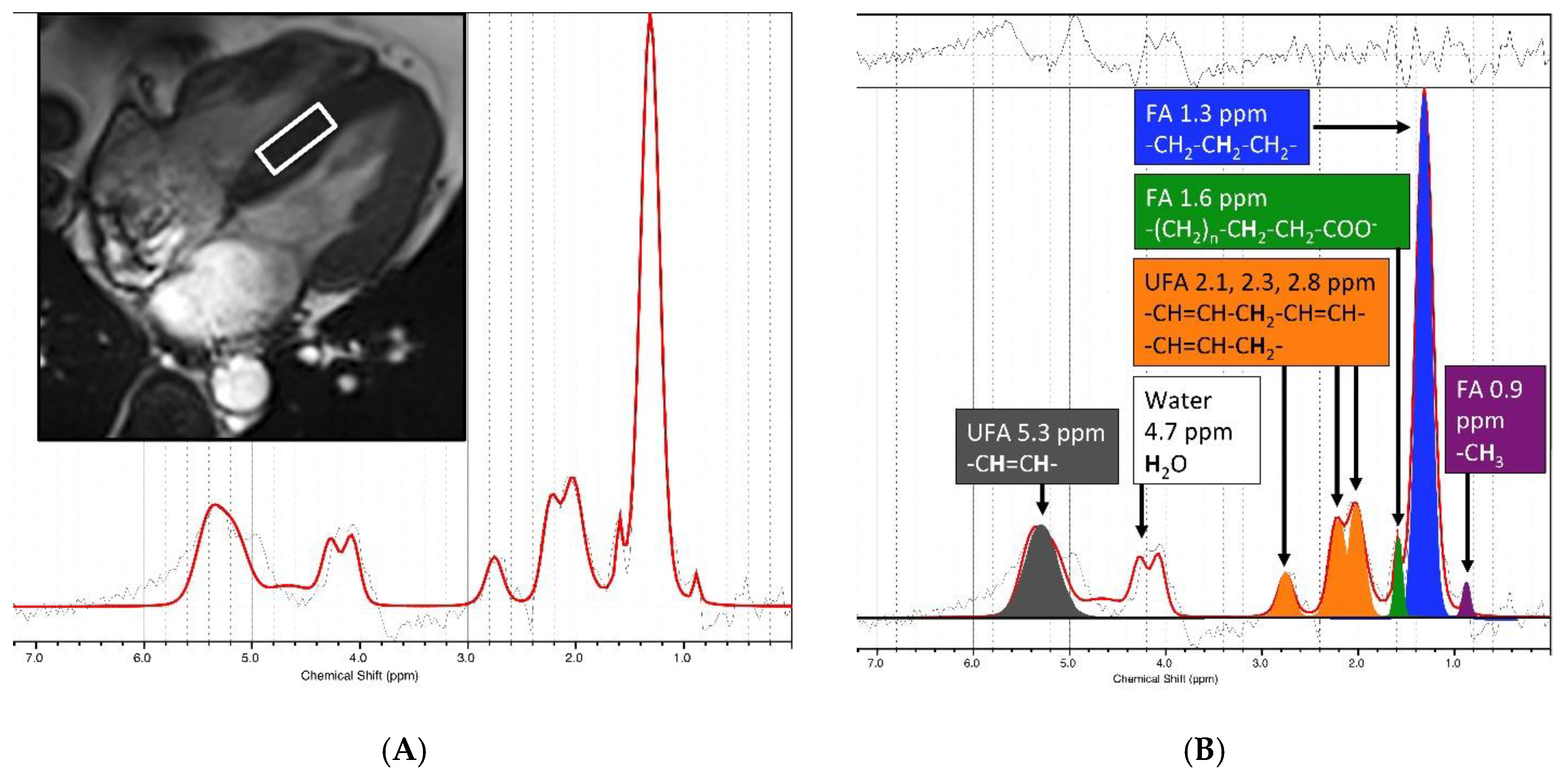
2.3. H-MRS
2.4. CMR Imaging
2.5. Image Analysis
2.6. Treatment and Definition of the Study Outcomes
2.7. Data Analysis
3. Results
3.1. Patient Characteristics
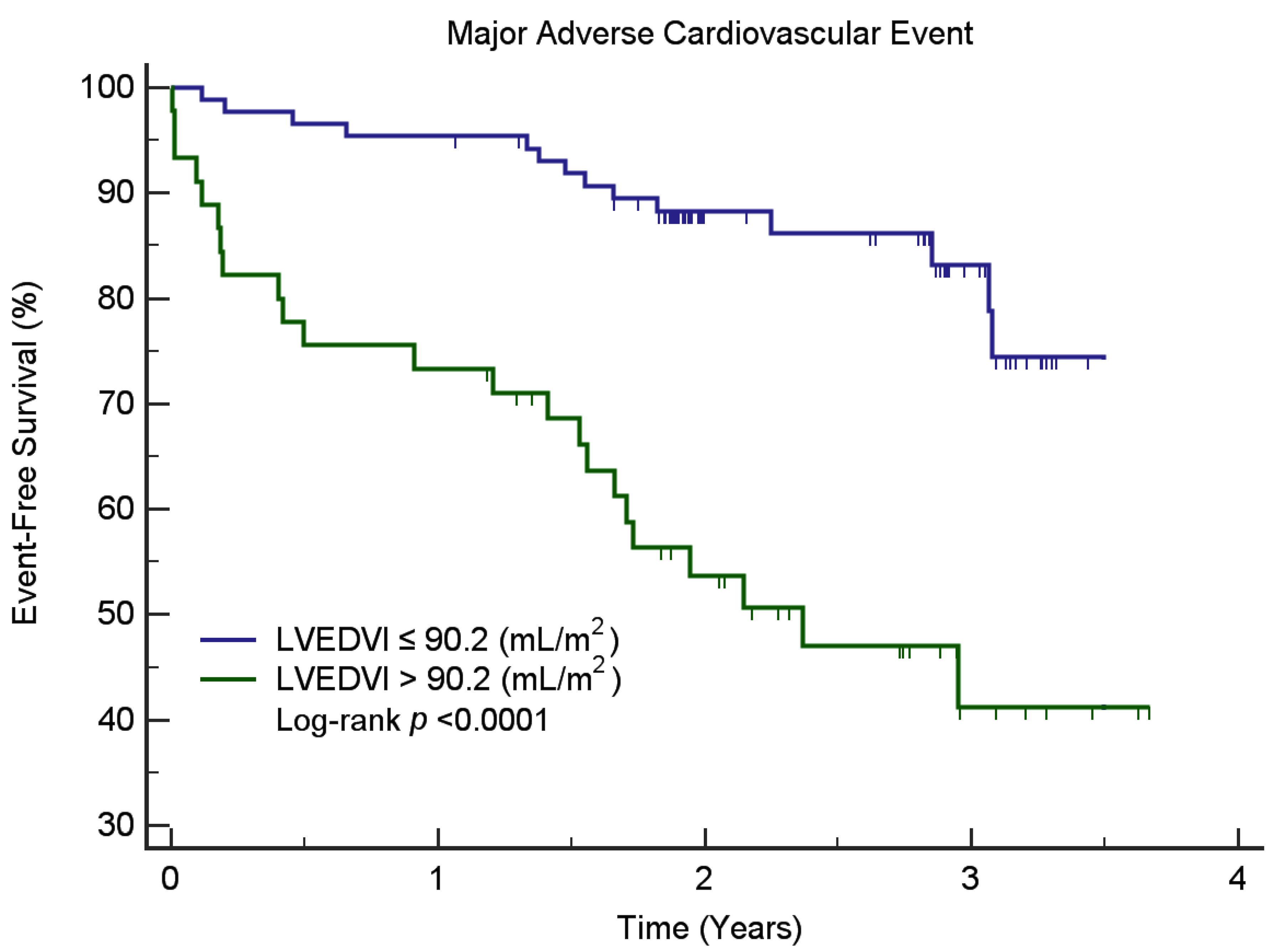
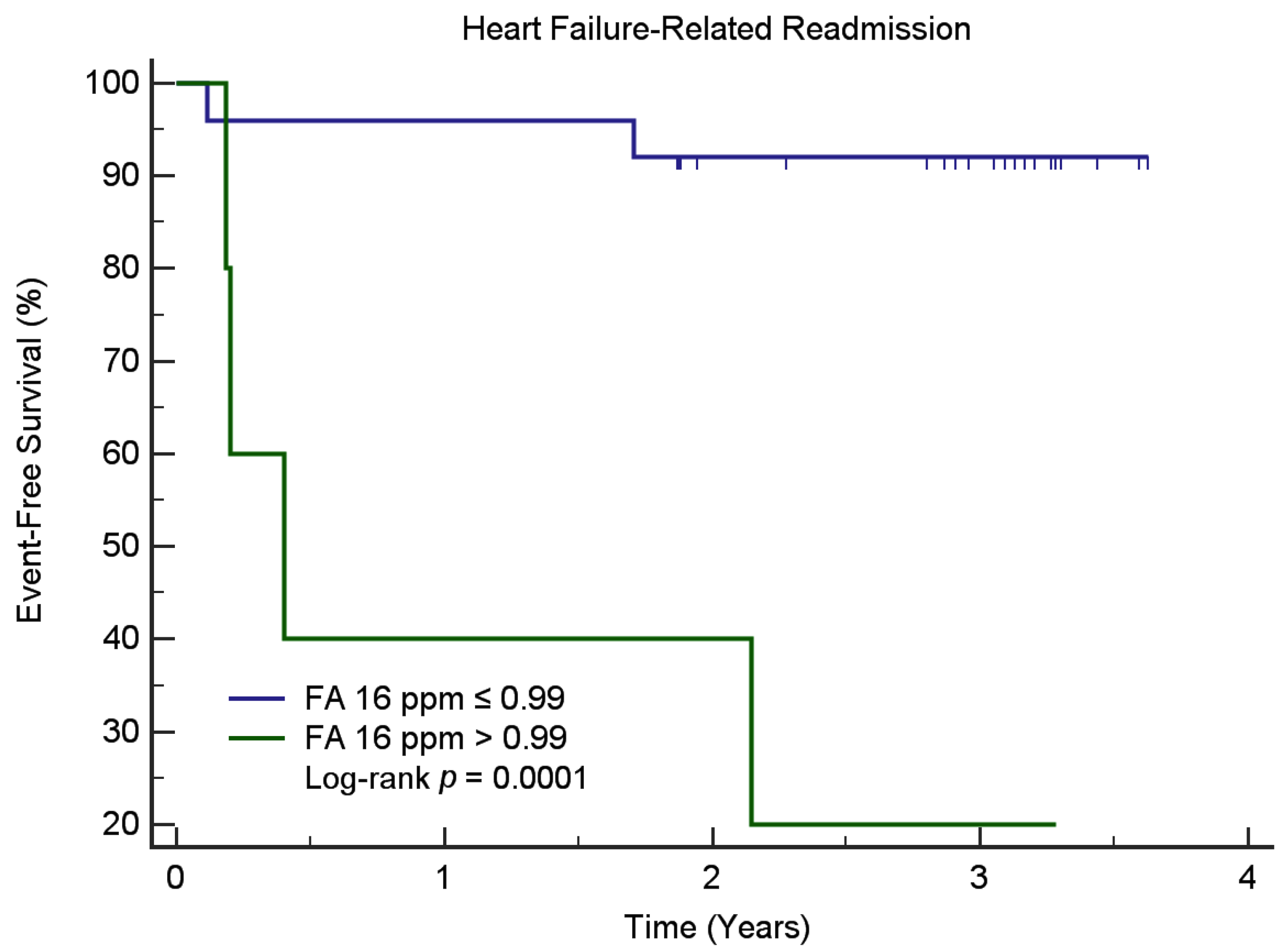
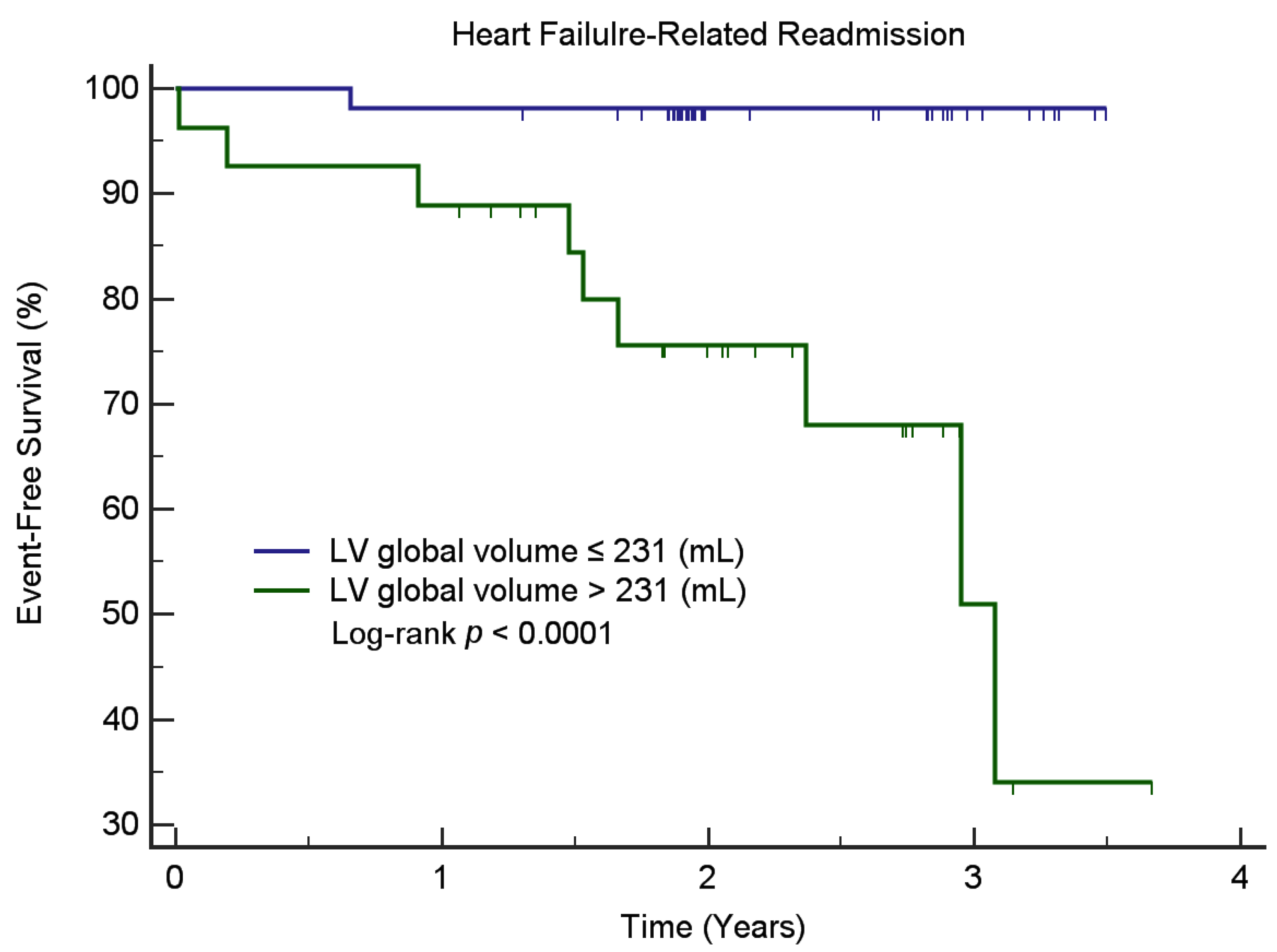
3.2. Associations between CMR, and 1H-MRS Parameters with MACE and HF-Related Readmission
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Ponikowski, P.; Voors, A.A.; Anker, S.D.; Bueno, H.; Cleland, J.G.F.; Coats, A.J.S.; Falk, V.; Gonzalez-Juanatey, J.R.; Harjola, V.P.; Jankowska, E.A.; et al. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur. Heart J. 2016, 37, 2129–2200. [Google Scholar] [PubMed]
- Tsutsui, H.; Tsuchihashi, M.; Takeshita, A. Mortality and readmission of hospitalized patients with congestive heart failure and preserved versus depressed systolic function. Am. J. Cardiol. 2001, 88, 530–533. [Google Scholar] [CrossRef]
- Yancy, C.W.; Jessup, M.; Bozkurt, B.; Butler, J.; Casey, D.E., Jr.; Drazner, M.H.; Fonarow, G.C.; Geraci, S.A.; Horwich, T.; Januzzi, J.L.; et al. 2013 ACCF/AHA guideline for the management of heart failure: Executive summary: A report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation 2013, 128, 1810–1852. [Google Scholar] [CrossRef] [PubMed]
- Hunt, S.A.; Abraham, W.T.; Chin, M.H.; Feldman, A.M.; Francis, G.S.; Ganiats, T.G.; Jessup, M.; Konstam, M.A.; Mancini, D.M.; Michl, K.; et al. ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic Heart Failure in the Adult: A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure): Developed in collaboration with the American College of Chest Physicians and the International Society for Heart and Lung Transplantation: Endorsed by the Heart Rhythm Society. Circulation 2005, 112, e154–e235. [Google Scholar] [PubMed]
- Taegtmeyer, H.; McNulty, P.; Young, M.E. Adaptation and maladaptation of the heart in diabetes: Part I: General concepts. Circulation 2002, 105, 1727–1733. [Google Scholar] [CrossRef]
- Wright, J.J.; Kim, J.; Buchanan, J.; Boudina, S.; Sena, S.; Bakirtzi, K.; Ilkun, O.; Theobald, H.A.; Cooksey, R.C.; Kandror, K.V.; et al. Mechanisms for increased myocardial fatty acid utilization following short-term high-fat feeding. Cardiovasc. Res. 2009, 82, 351–360. [Google Scholar] [CrossRef]
- Turkbey, E.B.; McClelland, R.L.; Kronmal, R.A.; Burke, G.L.; Bild, D.E.; Tracy, R.P.; Arai, A.E.; Lima, J.A.; Bluemke, D.A. The impact of obesity on the left ventricle: The Multi-Ethnic Study of Atherosclerosis (MESA). JACC Cardiovasc. Imaging 2010, 3, 266–274. [Google Scholar] [CrossRef]
- Wende, A.R.; Abel, E.D. Lipotoxicity in the heart. Biochim. Biophys. Acta 2010, 1801, 311–319. [Google Scholar] [CrossRef]
- Vilahur, G.; Casani, L.; Juan-Babot, O.; Guerra, J.M.; Badimon, L. Infiltrated cardiac lipids impair myofibroblast-induced healing of the myocardial scar post-myocardial infarction. Atherosclerosis 2012, 224, 368–376. [Google Scholar] [CrossRef]
- Faller, K.M.; Lygate, C.A.; Neubauer, S.; Schneider, J.E. (1) H-MR spectroscopy for analysis of cardiac lipid and creatine metabolism. Heart Fail. Rev. 2013, 18, 657–668. [Google Scholar] [CrossRef]
- Bizino, M.B.; Hammer, S.; Lamb, H.J. Metabolic imaging of the human heart: Clinical application of magnetic resonance spectroscopy. Heart 2014, 100, 881–890. [Google Scholar] [CrossRef] [PubMed]
- Mahmod, M.; Bull, S.; Suttie, J.J.; Pal, N.; Holloway, C.; Dass, S.; Myerson, S.G.; Schneider, J.E.; De Silva, R.; Petrou, M.; et al. Myocardial steatosis and left ventricular contractile dysfunction in patients with severe aortic stenosis. Circ. Cardiovasc. Imaging 2013, 6, 808–816. [Google Scholar] [CrossRef] [PubMed]
- Liao, P.A.; Lin, G.; Tsai, S.Y.; Wang, C.H.; Juan, Y.H.; Lin, Y.C.; Wu, M.T.; Yang, L.Y.; Liu, M.H.; Chang, T.C.; et al. Myocardial triglyceride content at 3 T cardiovascular magnetic resonance and left ventricular systolic function: A cross-sectional study in patients hospitalized with acute heart failure. J. Cardiovasc. Magn. Reson. 2016, 18, 9. [Google Scholar] [CrossRef] [PubMed]
- Aljizeeri, A.; Sulaiman, A.; Alhulaimi, N.; Alsaileek, A.; Al-Mallah, M.H. Cardiac magnetic resonance imaging in heart failure: Where the alphabet begins! Heart Fail. Rev. 2017, 22, 385–399. [Google Scholar] [CrossRef] [PubMed]
- Todiere, G.; Marzilli, M. Role of cardiac imaging in heart failure. Minerva Cardioangiol. 2012, 60, 347–362. [Google Scholar] [PubMed]
- Partington, S.L.; Cheng, S.; Lima, J.A. Cardiac magnetic resonance imaging for stage B heart failure. Heart Fail. Clin. 2012, 8, 179–190. [Google Scholar] [CrossRef]
- Bottomley, P.A. Spatial localization in NMR spectroscopy in vivo. Ann. N. Y. Acad. Sci. 1987, 508, 333–348. [Google Scholar] [CrossRef]
- Liu, C.Y.; Bluemke, D.A.; Gerstenblith, G.; Zimmerman, S.L.; Li, J.; Zhu, H.; Lai, S.; Lai, H. Myocardial steatosis and its association with obesity and regional ventricular dysfunction: Evaluated by magnetic resonance tagging and 1H spectroscopy in healthy African Americans. Int. J. Cardiol. 2014, 172, 381–387. [Google Scholar] [CrossRef]
- Reingold, J.S.; McGavock, J.M.; Kaka, S.; Tillery, T.; Victor, R.G.; Szczepaniak, L.S. Determination of triglyceride in the human myocardium by magnetic resonance spectroscopy: Reproducibility and sensitivity of the method. Am. J. Physiol. Endocrinol. Metab. 2005, 289, E935–E939. [Google Scholar] [CrossRef]
- van der Meer, R.W.; Doornbos, J.; Kozerke, S.; Schar, M.; Bax, J.J.; Hammer, S.; Smit, J.W.; Romijn, J.A.; Diamant, M.; Rijzewijk, L.J.; et al. Metabolic imaging of myocardial triglyceride content: Reproducibility of 1H MR spectroscopy with respiratory navigator gating in volunteers. Radiology 2007, 245, 251–257. [Google Scholar] [CrossRef]
- O’Connor, R.D.; Xu, J.; Ewald, G.A.; Ackerman, J.J.; Peterson, L.R.; Gropler, R.J.; Bashir, A. Intramyocardial triglyceride quantification by magnetic resonance spectroscopy: In vivo and ex vivo correlation in human subjects. Magn. Reson. Med. 2011, 65, 1234–1238. [Google Scholar] [CrossRef] [PubMed]
- Weiss, K.; Summermatter, S.; Stoeck, C.T.; Kozerke, S. Compensation of signal loss due to cardiac motion in point-resolved spectroscopy of the heart. Magn. Reson. Med. 2014, 72, 1201–1207. [Google Scholar] [CrossRef] [PubMed]
- Kip, K.E.; Hollabaugh, K.; Marroquin, O.C.; Williams, D.O. The problem with composite end points in cardiovascular studies: The story of major adverse cardiac events and percutaneous coronary intervention. J. Am. Coll. Cardiol. 2008, 51, 701–707. [Google Scholar] [CrossRef]
- Cheng, M.L.; Wang, C.H.; Shiao, M.S.; Liu, M.H.; Huang, Y.Y.; Huang, C.Y.; Mao, C.T.; Lin, J.F.; Ho, H.Y.; Yang, N.I. Metabolic disturbances identified in plasma are associated with outcomes in patients with heart failure: Diagnostic and prognostic value of metabolomics. J. Am. Coll. Cardiol. 2015, 65, 1509–1520. [Google Scholar] [CrossRef] [PubMed]
- Minamisawa, M.; Miura, T.; Motoki, H.; Ueki, Y.; Shimizu, K.; Shoin, W.; Harada, M.; Mochidome, T.; Yoshie, K.; Oguchi, Y.; et al. Prognostic Impact of Diastolic Wall Strain in Patients at Risk for Heart Failure. Int. Heart J. 2017, 58, 250–256. [Google Scholar] [CrossRef] [PubMed]
- Mordi, I.; Bezerra, H.; Carrick, D.; Tzemos, N. The Combined Incremental Prognostic Value of LVEF, Late Gadolinium Enhancement, and Global Circumferential Strain Assessed by CMR. JACC. Cardiovasc. Imaging 2015, 8, 540–549. [Google Scholar]
- Mewton, N.; Opdahl, A.; Choi, E.Y.; Almeida, A.L.; Kawel, N.; Wu, C.O.; Burke, G.L.; Liu, S.; Liu, K.; Bluemke, D.A.; et al. Left ventricular global function index by magnetic resonance imaging—A novel marker for assessment of cardiac performance for the prediction of cardiovascular events: The multi-ethnic study of atherosclerosis. Hypertension 2013, 61, 770–778. [Google Scholar] [CrossRef]
- Wei, J.; Nelson, M.D.; Szczepaniak, E.W.; Smith, L.; Mehta, P.K.; Thomson, L.E.; Berman, D.S.; Li, D.; Bairey Merz, C.N.; Szczepaniak, L.S. Myocardial steatosis as a possible mechanistic link between diastolic dysfunction and coronary microvascular dysfunction in women. Am. J. Physiol. Heart Circ. Physiol. 2016, 310, H14–H19. [Google Scholar] [CrossRef]
- Deeka, H.; Skouri, H.; Noureddine, S. Readmission rates and related factors in heart failure patients: A study in Lebanon. Collegian 2016, 23, 61–68. [Google Scholar] [CrossRef]
- Butler, J.; Kalogeropoulos, A. Worsening heart failure hospitalization epidemic we do not know how to prevent and we do not know how to treat! J. Am. Coll. Cardiol. 2008, 52, 435–437. [Google Scholar] [CrossRef][Green Version]
- Desai, A.S.; Stevenson, L.W. Rehospitalization for heart failure: Predict or prevent? Circulation 2012, 126, 501–506. [Google Scholar] [CrossRef] [PubMed]
- Bluemke, D.A.; Kronmal, R.A.; Lima, J.A.; Liu, K.; Olson, J.; Burke, G.L.; Folsom, A.R. The relationship of left ventricular mass and geometry to incident cardiovascular events: The MESA (Multi-Ethnic Study of Atherosclerosis) study. J. Am. Coll. Cardiol. 2008, 52, 2148–2155. [Google Scholar] [CrossRef] [PubMed]
- de Simone, G.; Gottdiener, J.S.; Chinali, M.; Maurer, M.S. Left ventricular mass predicts heart failure not related to previous myocardial infarction: The Cardiovascular Health Study. Eur. Heart J. 2008, 29, 741–747. [Google Scholar] [CrossRef] [PubMed]
| Variable | MACE (n = 39) | Non-MACE (n = 94) | p Value |
|---|---|---|---|
| Clinical profile | |||
| Male sex (%) | 74.2% | 57.5% | 0.088 |
| Age (years) | 52.3 ± 10.0 | 52.7 ± 10.3 | 0.846 |
| Height (m) | 1.7 ± 0.1 | 1.7 ± 0.1 | 0.656 |
| Weight (kg) | 70.5 ± 13.8 | 69.6 ± 15.9 | 0.751 |
| BMI (kg/m2) | 25.7 ± 3.9 | 25.6 ± 5.3 | 0.953 |
| Heart rate | 73.8 ± 14.2 | 71.3 ± 13.2 | 0.350 |
| SBP (mmHg) | 125.3 ± 19.5 | 131.9 ± 21.1 | 0.087 |
| DBP (mmHg) | 73.0 ± 11.7 | 76.4 ± 10.2 | 0.116 |
| Smoking | 53.8% | 42.5% | 0.316 |
| Comorbidities | |||
| Hypertension | 47.3% | 45.0% | 0.956 |
| DM | 23.7% | 20.0% | 0.813 |
| Angina | 36.6% | 32.5% | 0.802 |
| MI | 36.6% | 32.5% | 0.802 |
| DCM | 16.1% | 10.0% | 0.512 |
| Myocarditis | 2.2% | 5.0% | 0.742 |
| CAD | 35.5% | 32.5% | 0.894 |
| Medications | |||
| DM drugs | 16.1% | 20.0% | 0.771 |
| Anti-platelets | 39.8% | 37.5% | 0.957 |
| Statins | 23.7% | 17.5% | 0.576 |
| Thrombolytic agents | 6.5% | 0.0% | 0.235 |
| Antiarrhythmic drugs | 14.0% | 10.0% | 0.729 |
| Diuretics | 39.8% | 30.0% | 0.381 |
| Calcium channel blockers | 10.8% | 7.5% | 0.794 |
| Beta blockers | 68.8% | 62.5% | 0.611 |
| ACEI/ARB | 68.8% | 57.5% | 0.289 |
| Vasodilators | 16.1% | 5.0% | 0.139 |
| Iron supplements | 5.4% | 2.5% | 0.781 |
| Laboratory data | |||
| AST (U/L) | 31.4 ± 28.5 | 27.9 ± 24.3 | 0.556 |
| ALT (U/L) | 28.1 ± 16.5 | 39.8 ± 49.3 | 0.187 |
| HDL (mg/dL) | 43.5 ± 12.4 | 43.5 ± 12.1 | 0.988 |
| VLDL (mg/dL) | 30.3 ± 15.7 | 28.6 ± 13.0 | 0.598 |
| LDL (mg/dL) | 106.2 ± 53.2 | 109.7 ± 38.4 | 0.737 |
| Total cholesterol/HDL | 5.1 ± 5.3 | 4.4 ± 1.1 | 0.449 |
| LDL/HDL | 2.8 ± 1.2 | 2.7 ± 1.0 | 0.663 |
| Total cholesterol (mg/dL) | 189.3 ± 49.4 | 185.2 ± 35.7 | 0.672 |
| Triglyceride (mg/dL) | 165.5 ± 129.1 | 151.2 ± 86.2 | 0.564 |
| Non-HDL (mg/dL) | 145.8 ± 45.0 | 141.7 ± 35.4 | 0.662 |
| Glucose (mg/dL) | 113.2 ± 31.2 | 123.5 ± 51.2 | 0.210 |
| HbA1c (mg/dL) | 6.2 ± 1.2 | 6.4 ± 1.6 | 0.421 |
| TIBC (ug/dL) | 377.9 ± 85.8 | 346.7 ± 52.2 | 0.413 |
| Troponin (ng/mL) | 2.0 ± 8.9 | 0.3 ± 0.7 | 0.428 |
| BNP (pg/mL) | 342.9 ± 583.0 | 450.4 ± 569.7 | 0.470 |
| Neutrophil count (%) | 62.7 ± 12.6 | 57.5 ± 12.4 | 0.078 |
| Hemoglobin (g/dL) | 14.4 ± 3.5 | 13.5 ± 1.5 | 0.129 |
| MCV (fl) | 87.7 ± 6.7 | 86.4 ± 8.0 | 0.322 |
| MCH (pg) | 29.6 ± 2.7 | 29.0 ± 3.1 | 0.240 |
| MCHC (%) | 33.7 ± 1.0 | 41.0 ± 47.5 | 0.337 |
| CMR& MRS Parameters | Overall (n = 133) | Ischemia (n = 50) | Non-Ischemia (n = 83) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate | Stepwise Multivariable | Univariate | Stepwise Multivariable | Univariate | Stepwise Multivariable | |||||||
| Variable | HR | p Value | HR | p Value | HR | p Value | HR | p Value | HR | p Value | HR | p Value |
| EF (%) | 0.97 | <0.001 | 0.99 | 0.456 | 0.95 | 0.001 | ||||||
| LV EDV (mL) | 1.01 | <0.001 | 1.00 | 0.099 | 1.01 | <0.001 | ||||||
| LV EDVI (mL/m2) | 1.01 | <0.001 | 1.01 | <0.001 * | 1.01 | 0.041 | 1.02 | <0.001 | ||||
| LV ESV (mL) | 1.01 | <0.001 | 1.00 | 0.189 | 1.01 | <0.001 | ||||||
| Cardiac output (L/min) | 1.08 | 0.463 | 1.25 | 0.067 | 1.32 | 0.044 | 0.95 | 0.768 | ||||
| Myocardial mass (g) | 1.01 | 0.001 | 1.01 | 0.144 | 1.01 | <0.001 | 1.32 | 0.044 | ||||
| LV stroke volume (mL) | 1.00 | 0.635 | 1.01 | 0.341 | 1.01 | 0.836 | ||||||
| LV mean cavity volume (mL) | 1.01 | <0.001 | 1.00 | 0.132 | 1.01 | <0.001 | ||||||
| LV myocardial volume (mL) | 1.01 | 0.001 | 1.01 | 0.144 | 1.01 | <0.001 | ||||||
| LV global volume (mL) | 1.00 | <0.001 | 1.00 | 0.103 | 1.00 | <0.001 | ||||||
| LVGFI (%) | 0.97 | 0.001 | 0.99 | 0.562 | 0.95 | <0.001 | ||||||
| FA 0.9 ppm | 1.00 | 0.508 | 1.00 | 0.573 | 1.00 | 0.671 | ||||||
| FA 1.3 ppm | 1.00 | 0.599 | 1.00 | 0.697 | 1.00 | 0.764 | ||||||
| FA 1.6 ppm | 1.00 | 0.967 | 1.00 | 0.472 | 1.00 | 0.706 | ||||||
| UFA 2.1 ppm | 1.00 | 0.557 | 1.00 | 0.938 | 1.00 | 0.779 | ||||||
| UFA 2.3 ppm | 1.00 | 0.796 | 1.00 | 0.876 | 0.94 | 0.604 | ||||||
| UFA 2.8 ppm | 1.00 | 0.796 | 1.00 | 0.753 | 0.18 | 0.772 | ||||||
| FA (09,13,16) | 1.00 | 0.617 | 1.00 | 0.701 | 1.00 | 0.748 | ||||||
| UFA (21,23,28,53) | 1.00 | 0.881 | 1.00 | 0.640 | 1.00 | 0.722 | ||||||
| TG (FA+UFA) | 1.00 | 0.592 | 1.00 | 0.643 | 1.00 | 0.740 | ||||||
| FA/TG | 1.68 | 0.219 | 1.89 | 0.292 | 1.60 | 0.605 | ||||||
| UFA/TG | 0.60 | 0.219 | 0.53 | 0.292 | 0.62 | 0.605 | ||||||
| FA/UFA | 1.00 | 0.089 | 1.01 | 0.023 | 1.01 | 0.022 | 0.98 | 0.426 | ||||
| CMR& MRS Parameters | Overall (n = 133) | Ischemia (n = 50) | Non-Ischemia (n = 83) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Univariate | Stepwise Multivariable | Univariate | Stepwise Multivariable | Univariate | Stepwise Multivariable | |||||||
| Variable | HR | p Value | HR | p Value | HR | p Value | HR | p Value | HR | p Value | HR | p Value |
| EF (%) | 0.96 | <0.001 | 0.97 | 0.184 | 0.94 | 0.001 | ||||||
| LV EDV (mL) | 1.01 | <0.001 | 1.01 | 0.152 | 1.01 | <0.001 | ||||||
| LV EDVI (mL/m2) | 1.02 | <0.001 | 1.02 | <0.001 * | 1.02 | 0.106 | 1.02 | 0.001 | 1.01 | <0.001 * | ||
| LV ESV (mL) | 1.01 | <0.001 | 1.01 | 0.119 | 1.01 | <0.001 | ||||||
| Cardiac output (L/min) | 0.85 | 0.348 | 0.92 | 0.781 | 0.81 | 0.326 | ||||||
| Myocardial mass (g) | 1.01 | <0.001 | 1.01 | 0.177 | 1.02 | 0.001 * | 1.01 | 0.001 | ||||
| LV stroke volume (mL) | 0.99 | 0.447 | 0.99 | 0.699 | 0.99 | 0.408 | ||||||
| LV mean cavity volume (mL) | 1.01 | <0.001 | 1.01 | 0.130 | 1.01 | <0.001 | ||||||
| LV myocardial volume (mL) | 1.01 | <0.001 | 1.01 | 0.177 | 1.01 | 0.001 | ||||||
| LV global volume (mL) | 1.01 | <0.001 | 1.01 | <0.001 * | 1.01 | 0.107 | 1.01 | <.001 | 1.01 | 0.002 * | ||
| LVGFI (%) | 0.94 | <0.001 | 0.95 | 0.148 | 0.94 | <0.001 | ||||||
| FA 0.9 ppm | 0.70 | 0.523 | 0.86 | 0.708 | 0.00 | 0.555 | ||||||
| FA 1.3 ppm | 1.00 | 0.746 | 0.96 | 0.832 | 1.00 | 0.769 | ||||||
| FA 1.6 ppm | 0.68 | 0.635 | 0.006 | 0.003 * | 0.22 | 0.735 | ||||||
| UFA 2.1 ppm | 0.34 | 0.629 | 0.50 | 0.723 | 0.16 | 0.766 | ||||||
| UFA 2.3 ppm | 0.65 | 0.718 | 0.82 | 0.737 | 0.24 | 0.770 | ||||||
| UFA 2.8 ppm | 0.04 | 0.619 | 0.71 | 0.780 | 0.487 | |||||||
| FA (09,13,16) | 0.99 | 0.589 | 0.96 | 0.0718 | 1.00 | 0.795 | ||||||
| UFA (21,23,28,53) | 0.93 | 0.581 | 0.77 | 0.708 | 0.96 | 0.635 | ||||||
| TG (FA+UFA) | 0.99 | 0.589 | 0.99 | 0.851 | 0.99 | 0.680 | ||||||
| FA/TG | 2.72 | 0.183 | 56.41 | 0.095 | 1.21 | 0.818 | ||||||
| UFA/TG | 0.37 | 0.183 | 0.02 | 0.095 | 0.83 | 0.818 | ||||||
| FA/UFA | 1.01 | 0.396 | 1.01 | 0.318 | 1.00 | 0.858 | ||||||
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chang, K.-F.; Lin, G.; Huang, P.-C.; Juan, Y.-H.; Wang, C.-H.; Tsai, S.-Y.; Lin, Y.-C.; Wu, M.-T.; Liao, P.-A.; Yang, L.-Y.; et al. Left Ventricular Function and Myocardial Triglyceride Content on 3T Cardiac MR Predict Major Cardiovascular Adverse Events and Readmission in Patients Hospitalized with Acute Heart Failure. J. Clin. Med. 2020, 9, 169. https://doi.org/10.3390/jcm9010169
Chang K-F, Lin G, Huang P-C, Juan Y-H, Wang C-H, Tsai S-Y, Lin Y-C, Wu M-T, Liao P-A, Yang L-Y, et al. Left Ventricular Function and Myocardial Triglyceride Content on 3T Cardiac MR Predict Major Cardiovascular Adverse Events and Readmission in Patients Hospitalized with Acute Heart Failure. Journal of Clinical Medicine. 2020; 9(1):169. https://doi.org/10.3390/jcm9010169
Chicago/Turabian StyleChang, Kuang-Fu, Gigin Lin, Pei-Ching Huang, Yu-Hsiang Juan, Chao-Hung Wang, Shang-Yueh Tsai, Yu-Ching Lin, Ming-Ting Wu, Pen-An Liao, Lan-Yan Yang, and et al. 2020. "Left Ventricular Function and Myocardial Triglyceride Content on 3T Cardiac MR Predict Major Cardiovascular Adverse Events and Readmission in Patients Hospitalized with Acute Heart Failure" Journal of Clinical Medicine 9, no. 1: 169. https://doi.org/10.3390/jcm9010169
APA StyleChang, K.-F., Lin, G., Huang, P.-C., Juan, Y.-H., Wang, C.-H., Tsai, S.-Y., Lin, Y.-C., Wu, M.-T., Liao, P.-A., Yang, L.-Y., Liu, M.-H., Lin, Y.-C., Wang, J.-J., Ng, K.-K., & Ng, S.-H. (2020). Left Ventricular Function and Myocardial Triglyceride Content on 3T Cardiac MR Predict Major Cardiovascular Adverse Events and Readmission in Patients Hospitalized with Acute Heart Failure. Journal of Clinical Medicine, 9(1), 169. https://doi.org/10.3390/jcm9010169






